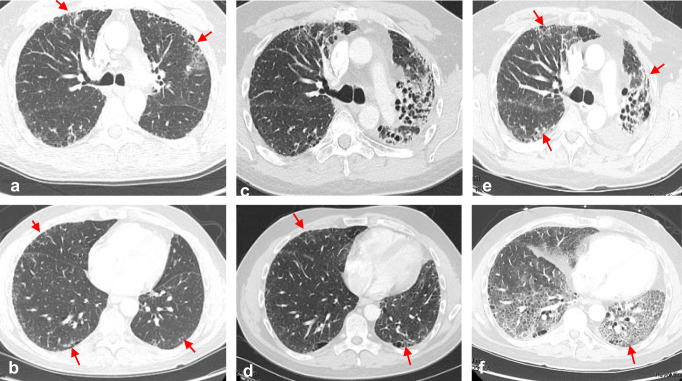
Fig. 1.
Accelerated lung injury following sequential ICI therapy. A 60-year-old man with metastatic urothelial carcinoma was treated with Pembrolizumab after failing standard chemotherapy. Pembrolizumab was interrupted after cycle 2 due to increased shortness of breath. Baseline CT imaging showed bilateral subpleural reticulations over the upper and lower lobes, consistent with his known history of idiopathic pulmonary fibrosis (a, b). Repeat CT imaging after cycle 2 of Pembrolizumab showed marked increase in diffuse upper and lower lobe and bilateral ground glass opacities (c, d). Symptoms and ground glass findings on CT nearly completely resolved with drug withdrawal and systemic corticosteroids. The PD-L1 inhibitor, durvalumab, given as monotherapy, was subsequently initiated. Three weeks after cycle 1 of durvalumab, severe and progressive symptoms of dyspnea, dry cough and hypoxia developed, resulting in admission and intubation for hypoxemic respiratory failure. All cultures were negative and no malignant cells were seen on BAL fluid. The patient continued to deteriorate despite high-dose steroids, antibiotics, and aggressive supportive care and later expired. An autopsy report confirmed diffuse alveolar damage with pulmonary fibrosis felt to be related to ICI therapy