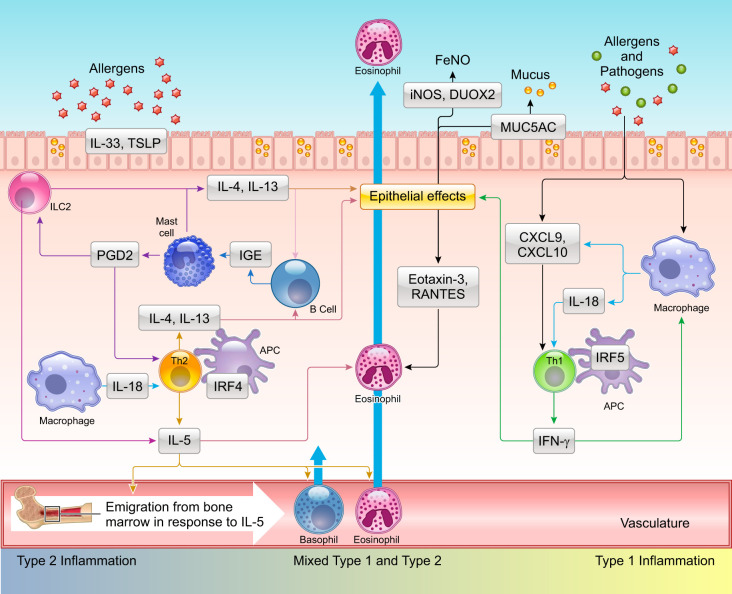
FIGURE 2.
Complex interplay between type 1 and type 2 immune pathways contributes to differing asthma phenotypes. Repeated exposure to allergens in genetically susceptible individuals induces the development of Th2 cells, which produce interleukin (IL)-4, IL-5, and IL-13. These type 2 cytokines can be also produced by alternate mechanisms involving cells of the innate immune system. In this regard, pathogens including bacteria, viruses, and fungi as well as allergens can cause epithelial damage in which proteases encoded by these agents play a prominent role. Epithelial damage leads to increased expression and release of IL-33 and thymic stromal lymphopoietin (TSLP), which stimulate ILC2 cells to produce IL-5 and IL-13. Tissue resident mast cells and basophils recruited from the periphery or generated from in situ differentiation of progenitors can also generate these cytokines. IL-5 released from circulating Th2 cells and other growth factors such as IL-3 and granulocyte-macrophage colony stimulating factor (GM-CSF) stimulate eosinophil differentiation, proliferation in the bone marrow, which are then recruited to the airways under the influence eosinophilic chemokines. Mast cells also produce prostaglandin D2 (PGD2) that binds its cognate receptor CRTH2 on Th2, ILC2 cells, triggering cytokine release. IL-4 and IL-13 produced by these different cell types augment mucus production via expression of mucin genes including MUC5AC. In certain individuals, gene-environment interactions also promote a type 1/interferon (IFN)-γ response with or without IL-17 production from T cells (not shown). IFN-γ in turn stimulates production of the chemokines CXCL9 and CXCL10 from both airway epithelial cells and resident macrophages with the potential to create a positive feedback loop promoting recruitment of Th1 cells and eosinophils via interaction with the receptor CXCR3. Increased expression of the cytokine IL-18 in macrophages can also promote development of Th1 and Th2 cells. Synergism between T1 (IFN-γ) and T2 (IL-13) cytokines augments expression of the enzymes inducible nitric oxide synthase (iNOS) and dual oxidase 2 (DUOX2) in the airway epithelial cells driving production of nitric oxide (NO) and H2O2, respectively, with increases in nitrative and oxidative stress. APC, antigen presenting cell; FeNO, fraction exhaled nitric oxide.