Abstract
In Australia and internationally, there are increasing calls for the use of strengths-based methodologies, to counter the dominant deficit discourse that pervades research, policy, and media relating to Indigenous health and wellbeing. However, there is an absence of literature on the practical application of strengths-based approaches to quantitative research. This paper describes and empirically evaluates a set of strategies to support strengths-based quantitative analysis.
A case study about Aboriginal and Torres Strait Islander child wellbeing was used to demonstrate approaches to support strengths-based quantitative analysis, in comparison to the dominant deficit approach of identifying risk factors associated with a negative outcome. Data from Wave 8 (2015) of the Australian Longitudinal Study of Indigenous Children were analysed. The Protective Factors Approach is intended to enable identification of factors protective against a negative outcome, and the Positive Outcome Approach is intended to enable identification of factors associated with a positive health outcome. We compared exposure-outcome associations (prevalence ratios and 95% confidence intervals (CIs), calculated using Poisson regression with robust variance) between the strengths-based and deficit approaches.
In this case study, application of the strengths-based approaches retains the identification of statistically significant exposure-outcome associations seen with the standard deficit approach. Strengths-based approaches can enable a more positive story to be told, without altering statistical rigour. For Indigenous research, a strengths-based approach better reflects community values and principles, and it is more likely to support positive change than standard pathogenic models. Further research is required to explore the generalisability of these findings.
Keywords: Strengths-based analysis, Decolonizing methodologies, Indigenous methodologies, Deficit discourse, Protective factors, Health resources, Australia
Highlights
-
•
To our knowledge, this is the first paper to outline and compare pragmatic analytic approaches to implementing strengths-based approaches in quantitative research.
-
•
For Indigenous research, a strengths-based approach is consistent with community values and principles.
-
•
Strengths-based approaches support the generation of research findings that are focused on strengths in order to reward and reinforce positive change, without altering statistical rigour.
-
•
In this case study, application of the strengths-based approaches retains the identification of statistically significant exposure-outcome associations seen with the standard deficit approach
1. Introduction
There have been substantial improvements in Aboriginal and Torres Strait Islander health and wellbeing in recent decades, including a 43% decrease in cardiovascular disease mortality from 1998 to 2015 (Australian Health Ministers' Advisory Council, 2017). Despite these improvements, a deficit discourse pervades research, policy, and media relating to Aboriginal and Torres Strait Islander health and wellbeing (Fogarty, Bulloch, McDonnell, & Davis, 2018; Stoneham, Goodman, & Daube, 2014; Sweet, 2009), with an enduring focus on Aboriginal and Torres Strait Islander identity in terms of negativity, deficiency, and disempowerment (Fforde, Bamblett, Lovett, Gorringe, & Fogarty, 2013; Walter & Andersen, 2013; Fogarty, Lovell, Langenberg, & Heron, 2018). A fallacious focus on Indigeneity as a ‘cause’ of poor health masks the contributions of systemic, covert, and overt racism to inequity. This focus is then used to ‘blame’ Indigenous people themselves for the circumstances of this inequity. This is demonstrated through a review of media articles in Western Australia in 2012 that found 74% of media stories about Aboriginal and Torres Strait Islander peoples were negative, focusing on topics such as alcohol use, child abuse, petrol sniffing, violence, and suicide (Stoneham et al., 2014). Deficit discourse forms part of a broader trend of blaming Indigenous culture for inequality (Bulloch & Fogarty, 2018).
Australia's overarching Aboriginal and Torres Strait Islander health strategy is centred around ‘Closing the Gap’ in health compared to the non-Indigenous population. Accordingly, much research and reporting describes Aboriginal and Torres Strait Islander health in relation to the health of non-Indigenous Australians, with the size of the gap the primary focus. Annual national policy documents focus on the extent to which aggregate Aboriginal and Torres Strait Islander indicators fall short of non-Indigenous outcomes (Fogarty, Bulloch, et al., 2018). Quantifying the magnitude of inequality can be important; however, it homogenises the population into a single metric, hiding diversity within the population, and provides limited information on where to focus and how to improve health and wellbeing (Walter & Andersen, 2013). Further, the focus on the gap can mask improvements occurring within the Aboriginal and Torres Strait Islander population. For example, a previous report identified that the gap in smoking prevalence between the Aboriginal and Torres Strait Islander population and the non-Indigenous population has remained stable, or even widened, in the past decade (Australian Institute of Health and Welfare, 2016). While this is technically accurate, examination of trends within the Aboriginal and Torres Strait Islander population demonstrates a significant and substantial decrease in smoking prevalence from 2004 to 15 (from 50% to 41%, absolute decrease of 9%), matching if not exceeding the decrease (in absolute terms) observed in the non-Indigenous population (Lovett, Thurber, Wright, Maddox, & Banks, 2017). This analysis also identified that young adults aged 18–44 years and people living in urban settings experienced particularly notable reductions in smoking prevalence. Exploring variation in outcomes within the Aboriginal and Torres Strait Islander population, rather than focusing on the gap alone, can identify meaningful progress, and provide valuable information on groups that are doing well or where targeted attention is required.
An important consequence of the dominant deficit discourse is that services, communities, and individuals are not getting an accurate reflection of progress that is occurring. Seeing progress is part of reinforcing improvement, serving to create a virtuous cycle (Bulloch, Fogarty, & Bellchambers, 2019; Cohen & Sherman, 2014). Aboriginal and Torres Strait Islander people are being denied this cycle, even in the circumstances where improvement is substantial; this is unjust. Hence, the current deficit focus does not make the most of progress pragmatically to reinforce and build on positive change, and is not appropriate from a social justice point of view.
Further, the continual repetition of negative discourses around Aboriginal and Torres Straits Islander people can stigmatise and problematise the Aboriginal and Torres Strait Islander population, that is, ingraining failure and deficiency as part of Aboriginal and Torres Strait Islander identity (Bond, 2005; Fforde et al., 2013; Fogarty, Bulloch, et al., 2018; Pyett, Waples-Crowe, & van der Sterren, 2008; Sweet, 2009). This negative discourse can fuel racist beliefs about Aboriginal and Torres Strait Islander peoples; it can also contribute to internalised racism, and a sense of fatalism, among Aboriginal and Torres Strait Islander peoples (Bond, 2005; Fogarty, Bulloch, et al., 2018; Jones, 2001; Stoneham et al., 2014). These can, in turn, contribute to poorer health and wellbeing outcomes, including through delays in taking health actions. For example, a United States study found that African-American adults exposed to messaging about colon cancer in a disparity frame (Blacks are doing worse than Whites, or Blacks are improving, but less than Whites), compared to those receiving the message in a progress frame (Blacks are improving over time), had a more negative emotional response and were less likely to pursue colon cancer screening (Nicholson et al., 2008).
In Australia and internationally, community members, researchers, and increasingly governments have advocated for the use of strengths-based approaches, to counter the dominant deficit discourse in Indigenous health (Durie, 2004; Fogarty, Lovell, Langenberg, & Heron, 2018; Foley & Schubert, 2013; Gray & Oprescu, 2015; Haswell-Elkins, Sebasio, Hunter, & Mar 2007; Laliberté, Haswell-Elkins, & Reilly, 2009; National Health and Medical Research Council, 2002; Smylie, Lofters, Firestone, & O'Campo, 2011; Wand & Eades, 2008). The intention of strengths-based approaches is not to ‘problem deflate’, misconstrue results, or deny inequities, but to refocus research and policy on identifying assets and strengths within individuals and communities and ‘avenues for action’ (Bond, 2009; Fogarty, Lovell, et al., 2018; Foley & Schubert, 2013; Haswell-Elkins et al., 2007; Salmon et al., 2018; Wand & Eades, 2008). A 2018 review identified a typology of strengths-based approaches described in national and international literature about Indigenous peoples' health and wellbeing (Fogarty, Lovell, et al., 2018). These strengths-based approaches are underpinned by decolonising methodologies, which aim to shift power to the Indigenous community; to centre research on Indigenous concerns; and, to respect Indigenous ways of knowing and worldviews, including holistic and multidimensional views of health/wellbeing, and interconnectivity (Fogarty, Lovell, et al., 2018; Pyett et al., 2008). Strengths-based approaches fit within the framework of salutogenesis, which focuses on the assets and origins of health, identifying individual and community strengths and resources that move an individual towards optimum wellbeing (Antonovsky, 1996; Becker, Glascoff, & Felts, 2010; Foley & Schubert, 2013). Salutogenesis contrasts pathogenesis, which is focused on the causes and origins of disease (Antonovsky, 1996; Becker et al., 2010).
While the literature documents strengths-based approaches for various stages of the research cycle (Bond, 2009; Foley & Schubert, 2013; Haswell-Elkins et al., 2007; Holmes, Stewart, Garrow, Anderson, & Thorpe, 2002; Pyett et al., 2008; Rossingh & Yunupingu, 2016; Wand & Eades, 2008), there is an absence of literature on the practical application of strengths-based approaches to quantitative research. Given increasing demands for strengths-based approaches, there is a need for practical guidance on the application of these methods. The aim of this paper is to describe and empirically evaluate a set of strategies to support strengths-based quantitative analysis, through application to a case study about Aboriginal and Torres Strait Islander child wellbeing.
1.1. Proposed strengths-based quantitative analytical approaches
Informed by the literature on strengths-based methodologies, and by approaches used in published studies, we developed approaches to support strengths-based quantitative analysis. As a starting point, the approaches require the research to be focused primarily on the Aboriginal and Torres Strait Islander population, rather than solely on comparisons to the non-Indigenous population.
A substantial body of literature has identified a higher prevalence of poor social and emotional wellbeing (SEWB) and mental health-related outcomes in the Aboriginal and Torres Strait Islander compared to non-Indigenous population (Jorm, Bourchier, Cvetkovski, & Stewart, 2012; Priest, Baxter, & Hayes, 2012). In contrast to this between-population approach, we focused on the examination of factors associated with mental health within a sample of Aboriginal and Torres Strait Islander children.
1.1.1. Protective Factors Approach
Bio-medical focused research tends to quantify individual risk factors and determinants of disease (pathogenesis). Across Indigenous worldviews internationally, there are many factors believed to contribute to health beyond biology and biomedicine (Durie, 2004; Gray & Oprescu, 2015; Haswell-Elkins et al., 2007; Holmes et al., 2002; Penman, 2006; Smith, 2005; Smylie & Anderson, 2006; Wand & Eades, 2008). Indigenous perspectives of health tend to be holistic (Durie, 2004). For example, Aboriginal and Torres Strait Islander health has been defined as ‘not just the physical wellbeing of the individual, but the social, emotional and cultural wellbeing of the whole community … [and] a matter of determining all aspects of their life, including control over their physical environment, of dignity, of community self-esteem and of justice. It is not merely a matter of the provision of doctors, hospitals, medicines or the absence of disease and incapacity’ (National Aboriginal Health Strategy Working Party, 1989 p. X). Conducting research based on a narrow view of biology alone can have detrimental impacts, including the devaluation of Indigenous culture and the generation of research findings that are not meaningful to participants.
It is therefore critical to adopt a holistic approach, including broader factors in analyses, beyond individual-focused measures and standard indicators of risk (Pyett et al., 2008). This may encompass social determinants of health (such as employment, income, housing, community, and structural factors) and other health resources that may promote wellbeing (such as cultural connection, identity, resilience, and empowerment) (Fogarty, Lovell, et al., 2018; Foley & Schubert, 2013). These protective factors can contribute to health-promoting behaviours and/or positive health and wellbeing outcomes, even when standard risk factors are present (Henson, Sabo, Trujillo, & Teufel-Shone, 2017). In addition, where standard risk factors are examined, it is possible to reframe this, by focusing on the absence of risk. This can be done by simply changing which exposure category is defined as the reference group in the analysis, enabling identification of protective factors rather than risk factors.
1.1.2. Positive Outcome Approach
Salutogenic theory calls for data to be examined differently, to ‘look at those who are succeeding and try to find out why they are doing well’, rather than looking at those with disease to find out why they are unwell. In addition to exploring health resources (rather than risk factors), this requires shifting from a pathogenically-oriented outcome (i.e. disease) to a health-oriented outcome (i.e. wellbeing) (Antonovsky, 1996; Becker et al., 2010; Lindström & Eriksson, 2005; Mittelmark & Bauer, 2017; Mittelmark & Bull, 2013).
The Positive Outcome Approach builds upon the Protective Factors Approach, in that it retains as the reference category the group most likely to experience adverse outcomes, so that the analyses identify exposures likely to be protective. It then incorporates an outcome that is along the spectrum towards optimum health. In the absence of a robust measure of positive wellbeing, this can be achieved through using an outcome that represents the absence of ill-health, which may simply require reversing the coding for the outcome variable (i.e. disease = = 0, non-disease = = 1 instead of non-disease = = 0, disease = = 1).
2. Case study: application of strengths-based approaches to quantitative data analysis
To empirically evaluate the two approaches described above, we conducted a case study, applying these approaches and the standard Deficit Approach to the same data about the wellbeing of Aboriginal and Torres Strait Islander children. We conducted a statistical assessment of the quantitative analytical approaches, considering their strengths and limitations compared to the standard Deficit Approach.
2.1. Data source
This case study analyses data from Footprints in Time, the Longitudinal Study of Indigenous Children (LSIC). LSIC is an ongoing national longitudinal study of Aboriginal and Torres Strait Islander children and their families, funded and managed by the Australian Government Department of Social Services (Thurber, Banks, & Banwell, 2014). The study collects data on a broad range of social, cultural, and environmental factors through annual face-to-face interviews with the study child and their caregiver(s). We analysed data from families participating in the 8th wave of the study, collected in 2015 when children were aged 7–13 years.
2.2. Variables
All variables included in this study are collected via primary caregiver (P1) self-report.
We were interested in examining a measure of social and emotional wellbeing (SEWB). In the absence of an Indigenous-specific robust measure of child SEWB or mental health, the Strengths and Difficulties Questionnaire (SDQ) (Goodman, 1994, 1997, 2001) is routinely used with Aboriginal and Torres Strait Islander youth, including in national data collections (Australian Government Department of Health, 2016) and in multiple cohort studies (Gubhaju et al., 2019; The SEARCH Investigators; Thurber et al., 2014). The SDQ is designed to capture risk of emotional and behavioural difficulties. There are evidenced concerns about the validity of SDQ for use with Aboriginal and Torres Strait Islander children; however, it demonstrates some value as an indicator of psychological distress (Thurber et al., 2019; Williamson et al., 2010, 2014; Zubrick, Lawrence, De Maio, & Biddle, 2006). Therefore, in this case study, we examined children's caregiver-reported (SDQ) Total Difficulties Score as a proxy measure of psychological distress. SDQ responses were summed and categorised according to the SDQ scoring guide, using the three-band classification. Scores of 0–13 were defined as reflecting low, 14–16 moderate, and 17–40 high levels of psychological distress. For the primary analysis, we defined ‘good mental health’ as SDQ scores in the low category (67.3%), and ‘poor-moderate mental health’ as SDQ scores in the moderate or high category (32.7%). Children missing data on SDQ were excluded from analysis (n = 5/1255).
We selected 15 exposure variables for analysis, chosen to represent standard factors commonly used in analysis (age group, sex, general health, parental mental health); social determinants of health often included in health research (financial security, housing security, stressful events); and potential salutogenic factors or health assets that are rarely explored in quantitative health research (family cohesion, living on country, language, safety at school, positive peer relationships at school, parental trust in the school, and parental connection to community). The selection of variables for inclusion was informed by the findings of the literature review (Fogarty, Lovell, et al., 2018), but was limited to the variables available in the LSIC dataset. The variables selected were diverse in terms of distribution across exposure categories; the distribution of the exposure variables overall and in relation to the outcome are presented in Table A1.
2.3. Statistical methods
To illustrate the different approaches, we ran a series of analyses with variations to the analytical strategy. Across all approaches, we calculated prevalence ratios (PRs, using Poisson regression) rather than odds ratios because the outcome was common (Cummings, 2009).
All models were restricted to children with data on the variables of interest (n = 998–1250). Models were unadjusted. LSIC employs a clustered sampling design and therefore adjustment for geographic cluster is recommended for analysis (Hewitt, 2012). However, we did not adjust for cluster in this analysis as it was most transparent to assess the three approaches using crude models, where estimates could be directly calculated from the PR formula. The purpose of this paper is to develop and compare strengths-based and standard approaches; the study findings are not intended to provide an accurate representation of the exposure-outcome associations. We note that findings were not materially different when analysis was re-run adjusted for clustering (data not shown).
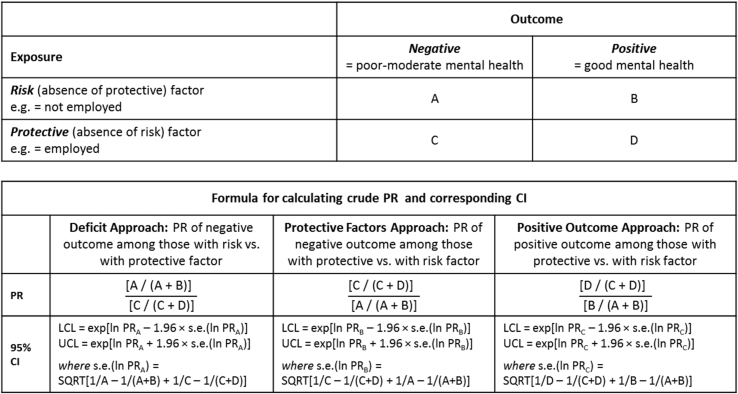
The broad strategy for comparing the approaches was to compare the Deficit Approach with the Protective Factors Approach and the Positive Outcomes Approach, as follows (Fig. 1):
Fig. 1.
Formula for calculating crude PRs and CIs in the Deficit Approach, Protective Factors Approach, and Positive Outcome Approach.
2.3.1. Deficit approach
We first modelled the associations using the standard pathogenic approach, to identify risk factors for a ‘disease’ outcome in the cohort. Our outcome was poor-moderate mental health; we defined the reference group as the category with the highest prevalence of the outcome.
2.3.2. Protective Factors Approach
We repeated the first Approach, with the single change of switching the reference group to the category with the lowest prevalence of the outcome.
2.3.3. Positive Outcome Approach
This approach extends the second Approach, retaining the exposure categorisation, and switching the outcome to be good mental health.
We compared each exposure-outcome association across the three approaches. Analyses were conducted in Stata 15.
2.4. Sensitivity analyses
-
(1)
We conducted a sensitivity analysis using an alternate categorisation of the outcome, to test the robustness of our strategies to different outcome prevalences (Table A2, Table A3
-
(2)
To test the robustness of our strategies to different statistical methods, we conducted a sensitivity analysis across all approaches calculating PRs using log-binomial, instead of Poisson, models (Petersen & Deddens, 2008) (Table A4).
3. Results
3.1. Comparison of findings across approaches
Fig. 1 summarises the calculation of crude PRs with their respective CIs across the three approaches. The results of these analyses is presented in Table 1, and a plain-language interpretation is included in Table A5.
Table 1.
Associations between exposures and child mental health, according to the Deficit Approach, Protective Factors Approach, and Positive Outcome Approach.
| Deficit Approach: PR of poor-moderate vs. good mental health |
Protective Factors Approach: PR of poor-moderate vs. good mental health |
Positive Outcome Approach: PR of good vs. poor-moderate mental health |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Main analysis (Poisson) | PR | 95%CI | P-value | PR | 95%CI | P-value | PR | 95%CI | P-value |
| Child age | |||||||||
| 7–8 years | 1.18 | (1.00,1.38) | 0.04 | 1 | (ref) | 1 | (ref) | ||
| 9–13 years | 1 | (ref) | 0.85 | (0.72,0.99) | 0.04 | 1.08 | (1.00,1.17) | 0.04 | |
| Child gender | |||||||||
| Male | 1.21 | (1.03,1.42) | 0.02 | 1 | (ref) | 1 | (ref) | ||
| Female | 1 | (ref) | 0.82 | (0.70,0.97) | 0.02 | 1.10 | (1.02,1.19) | 0.02 | |
| Child general health | |||||||||
| Excellent or very good | 1 | (ref) | 0.7 | (0.58,0.83) | <0.01 | 1.23 | (1.09,1.39) | <0.01 | |
| Good, fair, or poor | 1.44 | (1.20,1.71) | <0.01 | 1 | (ref) | 1 | (ref) | ||
| Caregiver mental health | |||||||||
| Good | 1 | (ref) | 0.46 | (0.40,0.54) | <0.01 | 1.65 | (1.45,1.88) | <0.01 | |
| Poor | 2.16 | (1.86,2.51) | <0.01 | 1 | (ref) | 1 | (ref) | ||
| Caregiver employment | |||||||||
| Employed | 1 | (ref) | 0.78 | (0.66,0.92) | <0.01 | 1.13 | (1.04,1.22) | <0.01 | |
| Not employed | 1.29 | (1.09,1.52) | <0.01 | 1 | (ref) | 1 | (ref) | ||
| Worries about money | |||||||||
| No worries | 1 | (ref) | 0.69 | (0.59,0.81) | <0.01 | 1.22 | (1.11,1.34) | <0.01 | |
| Yes worries | 1.45 | (1.23,1.69) | <0.01 | 1 | (ref) | 1 | (ref) | ||
| Housing problems | |||||||||
| No problems | 1 | (ref) | 0.83 | (0.70,0.98) | 0.02 | 1.10 | (1.01,1.20) | 0.03 | |
| Yes problems | 1.21 | (1.03,1.42) | 0.02 | 1 | (ref) | 1 | (ref) | ||
| Negative major life events | |||||||||
| 0-1 events | 1 | (ref) | 0.76 | (0.64,0.89) | <0.01 | 1.14 | (1.06,1.23) | <0.01 | |
| 2-9 events | 1.32 | (1.12,1.56) | <0.01 | 1 | (ref) | 1 | (ref) | ||
| Family cohesion | |||||||||
| Always or most times | 1 | (ref) | 0.65 | (0.52,0.81) | <0.01 | 1.33 | (1.10,1.62) | <0.01 | |
| Sometimes, or not really | 1.55 | (1.24,1.93) | <0.01 | 1 | (ref) | 1 | (ref) | ||
| Living on country | |||||||||
| Live on country | 1.18 | (0.99,1.40) | 0.07 | 1 | (ref) | 1 | (ref) | ||
| Do not live on country | 1 | (ref) | 0.85 | (0.72,1.01) | 0.07 | 1.09 | (0.99,1.19) | 0.07 | |
| Child speaks an Indigenous language | |||||||||
| Yes does speak | 1 | (ref) | 0.88 | (0.73,1.08) | 0.22 | 1.06 | (0.97,1.15) | 0.20 | |
| No does not speak | 1.13 | (0.93,1.38) | 0.22 | 1 | (ref) | 1 | (ref) | ||
| Child feels safe at school | |||||||||
| Yes | 1 | (ref) | 0.54 | (0.46,0.63) | <0.01 | 1.51 | (1.31,1.75) | <0.01 | |
| Sometimes or no | 1.87 | (1.59,2.20) | <0.01 | 1 | (ref) | 1 | (ref) | ||
| Child positive peer relationships | |||||||||
| Not bullied at school | 1 | (ref) | 0.52 | (0.44,0.61) | <0.01 | 1.47 | (1.31,1.64) | <0.01 | |
| Bullied at school | 1.92 | (1.65,2.25) | <0.01 | 1 | (ref) | 1 | (ref) | ||
| Caregiver trusts local school | |||||||||
| Strongly agree or agree | 1 | (ref) | 0.64 | (0.54,0.77) | <0.01 | 1.30 | (1.14,1.48) | <0.01 | |
| Neutral to disagree | 1.55 | (1.30,1.85) | <0.01 | 1 | (ref) | 1 | (ref) | ||
| Caregiver feels connected to community | |||||||||
| Yes connected | 1 | (ref) | 0.76 | (0.64,0.91) | <0.01 | 1.16 | (1.04,1.30) | 0.01 | |
| Sometimes or not connected | 1.31 | (1.09,1.57) | <0.01 | 1 | (ref) | 1 | (ref) | ||
Age, gender, general health, bullying at school, caregiver mental health, caregiver employment, family worries about money, housing problems, negative major life events, family cohesion, safety at school, caregiver trust in the school, and caregiver connection to community were significantly associated with child mental health across all Approaches (p-value <0.05). We did not observe a significant association between child mental health and living on country or speaking Indigenous language(s) in any of the three approaches.
Although all Approaches describe the same exposure-outcome association, the interpretation varies across the three approaches. For example, findings on employment could be interpreted as follows:
-
•
Deficit Approach: Poor-moderate mental health is significantly more common among children whose caregivers are not employed versus employed.
-
•
Protective Factors Approach: Poor-moderate mental health is significantly less common among children whose caregivers are employed versus not employed.
-
•
Positive Outcome Approach: Good mental health is significantly more common among children whose caregivers are employed versus not employed.
Risk ratios have symmetry with respect to exposure definition (Fig. 1) (Cummings, 2009). Therefore, results for the Deficit Approach and Protective Factors Approach will be equivalent – though inverse – where the only change was flipping the exposure's reference category. For example, in Deficit Approach, we found that the PR for poor-moderate mental health was 1.29 (95%CI:1.09,1.52) for children whose caregiver was not employed versus employed; in Protective Factors Approach, the PR for poor-moderate mental health was 0.78 (1/1.29 = 0.78) (95%CI:0.66,0.92) for children whose caregiver was employed versus not employed. The bounds of the CIs are also inverse (0.92 = 1/1.09; 0.66 = 1/1.52).
However, PRs are not symmetrical with respect to the definition of the outcome, so the PR for the outcome of good mental health (Positive Outcome Approach) is not the inverse of the PR for the outcome of poor-moderate mental health (Protective Factors Approach). The PRs tend to appear somewhat attenuated (reduced magnitude of effect) when comparing the Positive Outcome Approach to the Deficit Approach.
3.2. Sensitivity analyses
Use of the alternative outcome definition decreased the outcome prevalence in the Protective Factors Approach (from 32.7% ‘poor-moderate’ mental health to 17.3% ‘poor’ mental health), and increased the outcome prevalence in the Positive Outcome Approach (from 67.3% ‘good’ mental health to 82.7% ‘good-moderate’ mental health) (Table A2). The significance and direction of exposure-outcome associations remained consistent across the two outcome definitions (Table A3).
In general, in the sensitivity analysis compared to the main analysis, the magnitude of PRs (effect size) increased for the Protective Factors Approach and decreased for the Positive Outcome Approach. For the Protective Factors Approach, in all cases, the CIs were wider in the sensitivity analysis compared to the main analysis, resulting from the lower outcome prevalence and larger standard error. In contrast, for the Positive Outcome Approach, the CIs were narrower in the sensitivity analysis compared to the main analysis, given the higher outcome prevalence and smaller standard error.
Findings were not materially different when using log-binomial regression versus Poisson regression (Table A3).
4. Discussion
Our results demonstrate that the application of strengths-based approaches changes the framing of results while retaining identification of statistically significant exposure-outcome associations seen with the standard Deficit Approach. Rather than identifying risk factors for disease, strengths-based approaches enable identification of factors that promote wellbeing. This can enable a more positive story to be told, without altering statistical rigour. This, in turn, is likely to support health-promoting actions.
To our knowledge, this is the first paper to outline and compare pragmatic analytic approaches to implementing a salutogenic stance for quantitative research. This paper contributes new knowledge about approaches that can be implemented in practice to support strengths-based quantitative analysis, with the intention of supporting the generation of research findings focused on strengths in order to reinforce positive change. Achieving these positive health impacts requires the maintenance of the strengths-based approach in the dissemination of findings, including through the media. It is well established that disparities and negative outcomes are generally considered more ‘newsworthy’ and ‘attention grabbing’ than positive stories (Haskins & Miller, 1984; Hinnant, Oh, Caburnay, & Kreuter, 2011). Educating the media may be an important component of supporting a positive cycle of change through strengths-based research (Hinnant et al., 2011).
While we argue for increased use of strengths-based approaches broadly, we acknowledge that there may be circumstances in which it may be beneficial to adopt a deficit frame. For example, a deficit frame may be employed to attract policy or public attention to a problem, where required (Hinnant et al., 2011). Policy is generally designed to address problems; therefore, a deficit frame may be required to define the policy problem, and then strengths-based approaches could be used for monitoring and evaluation. The use of strengths-based or other approaches should be fit for purpose.
This analysis is a case study, intended to demonstrate the application of strengths-based approaches in one example. While there are elements of our findings that are likely to be generalisable, they may not be reproduced across all analyses. The initial research proposed here is exploratory, and can form the foundation for future research in this area. There are potential challenges and limitations to using these strengths-based approaches, as described below.
4.1. Potential challenges with these approaches
Within-population comparisons rather than between-population comparisons: The focus on the gap between Aboriginal and Torres Strait Islander and non-Indigenous health is ingrained in research, policy, and reporting, which defaults to comparing the Aboriginal and Torres Strait Islander population to the non-Indigenous benchmark. Policy often requires a single summary statistic, rather than multiple within-population statistics, as proposed here. Benchmarking against another population (or ideally, against an achievable target that is not based on Indigeneity) can be useful. While between-population comparisons can yield useful information, they too require the application of methods that avoid the deficit discourse; the development of such methods will be addressed in subsequent work and is not covered in the current paper. In any case, a between-population comparison should not be the only metric examined and reported. Where between-population comparisons are required (i.e. to demonstrate the magnitude of, or assess trends in, inequity), these should be secondary to within-population analysis to identify areas for targeted attention and to provide insight into what underlies areas of success.
Protective Factors Approach: Focusing on salutogenic factors requires considering factors both within and outside of the biomedical/pathogenesis space. Some of these factors may be unknown and may require identification. Qualitative research can provide insight into potential salutogenic factors, and these can be examined in exploratory quantitative research (Henson et al., 2017).
When examining standard measures of risk, shifting the focus from risk to the absence of risk exposure can be perceived as cumbersome. For example, it might be more direct to interpret the finding that ‘experiencing bullying is associated with an increased prevalence of poor-moderate mental health’ than ‘the absence of bullying is associated with a decreased prevalence of poor-moderate mental health’. Calculating Floating Absolute Risks (FAR) alongside main results could help alleviate this potential concern by allowing readers the flexibility to make the desired comparison for their purposes (Easton, Peto, & Babiker, 1991; Plummer, 2004).
By nature, examination of a disease-oriented outcome in relation to a protective factor will result in a PR less than one, rather than a PR greater than one as occurs in standard risk factor-disease associations. There is a perception that it is generally more difficult to interpret PRs less than one (cognitive bias). This is alleviated through focusing on a positive (health-oriented) rather than negative (disease-oriented) outcome; quantifying the association between a salutogenic factor and a wellbeing outcome will result in a PR greater than one.
Positive Outcome Approach: The focus on positive outcomes contrasts the standard biomedical, pathogenesis approach. While there are many robust measures of disease and ill-health, we lack robust measures of optimum health and wellbeing. For example, when applying a strengths-based approach in this case study, we wanted to focus on a health-oriented outcome (i.e. SEWB). However, it is well established that we lack a holistic, health-oriented measure of SEWB for Aboriginal and Torres Strait Islander peoples (Le Grande et al., 2017). We were limited by the variables available in the LSIC dataset (Marmor & Harley, 2018), and thus used SDQ as a proxy measure of mental health, which is just one component of SEWB, and suffers from limitations to validity (Thurber et al., 2019; Williamson et al., 2010, 2014; Zubrick et al., 2006). Even though we focused on children with good mental health, this was still based on a pathogenically-oriented outcome (SDQ), which is designed to identify children's risk of social and emotional difficulties. There is a clear need for valid and relevant measures of wellbeing. Identifying factors associated with positive SEWB may provide additional insight beyond what is learned through examining factors associated with low SDQ risk. In any case, this analysis demonstrates ways to enhance the analysis of routinely collected measures (such as the SDQ) to enable a more strengths-based analysis even of a deficit-based measure.
PRs, as a ratio of percentages, are subject to a ceiling effect. The maximum possible value of a PR depends upon the outcome prevalence in the base category. For example, if the prevalence of good mental health is 50% in the unexposed group, the maximum PR for the exposed group would be 2.0, with a 100% outcome prevalence in the exposed category. The maximum possible PR magnitude decreases as the base prevalence increases; for example, the maximum possible PR is reduced to 1.25 if the outcome prevalence is 80% in the unexposed group. Given that a positive wellbeing outcome is likely to be more common than an outcome representing disease or ill-health, this ceiling effect is likely to constrain the magnitude of effect observed. As such, the association between a protective factor and a positive wellbeing outcome may appear to be attenuated (i.e. smaller magnitude of effect) compared to the corresponding association between the same risk factor and negative wellbeing outcome. Readers may need to be informed of this, and different criteria may need to be developed to assist with the interpretation of results. Nevertheless, the CIs around a PR will be narrower for a higher versus lower prevalence outcome. As a result, a high prevalence outcome and the associated ceiling effect do not necessarily preclude identification of significant exposure-outcome associations. While this may not be true for all studies, in this case study, we were able to detect the same significant associations, regardless of our choice of exposure/outcome categorisation.
5. Conclusion
The population focus of research, and the approach to within- and between-population comparisons, have profound effects on the framing of results. For Indigenous research, a strengths-based approach better reflects community values and principles, and it is more likely to support positive change than standard pathogenic models. Although the development of appropriate methods is in its infancy, these findings demonstrate the practicability of applying such methods and the need for developments in understanding of and policy demand for salutogenic framing, in parallel with methods development.
Data statement
LSIC is a shared resource; its data are readily accessible (through application) via the Australian Data Archive: https://dataverse.ada.edu.au/dataverse/lsic.
Financial Support
This project was funded by the Lowitja Institute [Grant No: 017-G-052], including support for JT, KD, and MS; KT, RL, and EB are supported by the National Health and Medical Research Council of Australia [KT: 1156276, RL:1122273, EB:1136128].
Ethics approval
This research paper used data collected by The Footprints in Time Study (the Longitudinal Study of Indigenous Children, LSIC) which is conducted with ethics approval from the Departmental Ethics Committee of the Australian Commonwealth Department of Health, and from Ethics Committees in each state and territory, including relevant Aboriginal and Torres Strait Islander organisations. The Australian National University's Human Research Ethics Committee granted ethics approval for the current analysis of data from LSIC (Protocol No. 2016/534).
CRediT authorship contribution statement
Katherine A. Thurber: Conceptualization, Methodology, Formal analysis, Data curation, Writing - original draft, Funding acquisition. Joanne Thandrayen: Methodology, Formal analysis, Writing - review & editing. Emily Banks: Methodology, Writing - review & editing. Kate Doery: Writing - review & editing, Visualization. Mikala Sedgwick: Writing - review & editing, Visualization. Raymond Lovett: Conceptualization, Methodology, Writing - review & editing, Supervision, Funding acquisition.
Declaration of competing interest
No potential conflict of interest was reported by the author.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ssmph.2020.100637.
Appendix
Table A1.
Characteristics of the sample, overall and in relation to child mental health (good mental health vs. poor-moderate mental health)
| Total |
Good mental health |
Poor-moderate mental health |
||||
|---|---|---|---|---|---|---|
| % | N | % | n | % | n | |
| Overall | 100 | 1250 | 67.3 | 841 | 32.7 | 409 |
| Child age | ||||||
| 7–8 years | 47.7 | 596 | 64.4 | 384 | 35.6 | 212 |
| 9–13 years | 52.3 | 654 | 69.9 | 457 | 30.1 | 197 |
| Child gender | ||||||
| Male | 49.4 | 618 | 64.1 | 396 | 35.9 | 222 |
| Female | 50.6 | 632 | 70.4 | 445 | 29.6 | 187 |
| Child general health | ||||||
| Excellent or very good | 82.0 | 1025 | 69.7 | 714 | 30.3 | 311 |
| Good, fair, or poor | 18.0 | 225 | 56.4 | 127 | 43.6 | 98 |
| Caregiver mental health | ||||||
| Good | 73.0 | 912 | 74.7 | 681 | 25.3 | 231 |
| Poor | 24.4 | 305 | 45.3 | 138 | 54.8 | 167 |
| Missing | 2.6 | 33 | 66.7 | 22 | 33.3 | 11 |
| Caregiver employment | ||||||
| Employed | 43.4 | 542 | 71.8 | 389 | 28.2 | 153 |
| Not employed | 56.4 | 705 | 63.7 | 449 | 36.3 | 256 |
| Missing | 0.2 | 3 | 100.0 | 3 | 0.0 | 0 |
| Worries about money | ||||||
| No worries | 68.8 | 860 | 71.3 | 613 | 28.7 | 247 |
| Yes worries | 30.6 | 383 | 58.5 | 224 | 41.5 | 159 |
| Missing | 0.6 | 7 | 57.1 | 4 | 42.9 | 3 |
| Housing problems | ||||||
| No problems | 68.3 | 854 | 69.3 | 592 | 30.7 | 262 |
| Yes problems | 31.5 | 394 | 62.9 | 248 | 37.1 | 146 |
| Missing | 0.2 | 2 | 50.0 | 1 | 50.0 | 1 |
| Negative major life events | ||||||
| 0-1 events | 44.7 | 559 | 72.3 | 404 | 27.7 | 155 |
| 2-9 events | 52.2 | 652 | 63.3 | 413 | 36.7 | 239 |
| Missing | 3.1 | 39 | 61.5 | 24 | 38.5 | 15 |
| Family cohesion | ||||||
| Always or most times | 92.1 | 1151 | 68.6 | 790 | 31.4 | 361 |
| Sometimes to never | 7.9 | 99 | 51.5 | 51 | 48.5 | 48 |
| Living on country | ||||||
| Live on country | 37.3 | 466 | 63.1 | 294 | 36.9 | 172 |
| Do not live on country | 42.6 | 532 | 68.6 | 365 | 31.4 | 167 |
| Missing | 20.2 | 252 | 72.2 | 182 | 27.8 | 70 |
| Child speaks an Indigenous language | ||||||
| Yes does speak | 24.2 | 302 | 70.5 | 213 | 29.5 | 89 |
| No does not speak | 73.4 | 918 | 66.7 | 612 | 33.3 | 306 |
| Missing | 2.4 | 30 | 53.3 | 16 | 46.7 | 14 |
| Child feels safe at school | ||||||
| Yes | 79.4 | 992 | 72.0 | 714 | 28.0 | 278 |
| Sometimes or no | 17.1 | 214 | 47.7 | 102 | 52.3 | 112 |
| Missing | 3.5 | 44 | 56.8 | 25 | 43.2 | 19 |
| Child positive peer relationships | ||||||
| Not bullied at school | 69.7 | 871 | 74.4 | 648 | 25.6 | 223 |
| Bullied at school | 27.4 | 343 | 50.7 | 174 | 49.3 | 169 |
| Missing | 2.9 | 36 | 52.8 | 19 | 47.2 | 17 |
| Caregiver trusts local school | ||||||
| Strongly agree or agree | 82.2 | 1027 | 70.4 | 723 | 29.6 | 304 |
| Neutral to disagree | 16.9 | 211 | 54.0 | 114 | 46.0 | 97 |
| Missing | 1.0 | 12 | 33.3 | 4 | 66.7 | 8 |
| Caregiver feels connected to community | ||||||
| Yes connected | 76.7 | 959 | 68.7 | 659 | 31.3 | 300 |
| Sometimes or not connected | 19.0 | 237 | 59.1 | 140 | 40.9 | 97 |
| Missing | 4.3 | 54 | 77.8 | 42 | 22.2 | 12 |
Table A2.
Characteristics of the sample, overall and in relation to child mental health (alternate categorisation: good-moderate mental health vs. poor mental health)
| Total |
Good-moderate mental health |
Poor mental health |
||||
|---|---|---|---|---|---|---|
| % | N | % | n | % | n | |
| Overall | 100 | 1250 | 82.7 | 1034 | 17.3 | 216 |
| Child age | ||||||
| 7–8 years | 47.7 | 596 | 80.4 | 479 | 19.6 | 117 |
| 9–13 years | 52.3 | 654 | 84.9 | 555 | 15.1 | 99 |
| Child gender | ||||||
| Male | 49.4 | 618 | 80.3 | 496 | 19.7 | 122 |
| Female | 50.6 | 632 | 85.1 | 538 | 14.9 | 94 |
| Child general health | ||||||
| Excellent or very good | 82.0 | 1025 | 83.9 | 860 | 16.1 | 165 |
| Good, fair, or poor | 18.0 | 225 | 77.3 | 174 | 22.7 | 51 |
| Caregiver mental health | ||||||
| Good | 73.0 | 912 | 87.4 | 797 | 12.6 | 115 |
| Poor | 24.4 | 305 | 68.9 | 210 | 31.2 | 95 |
| Missing | 2.6 | 33 | 81.8 | 27 | 18.2 | 6 |
| Caregiver employment | ||||||
| Employed | 43.4 | 542 | 86.7 | 470 | 13.3 | 72 |
| Not employed | 56.4 | 705 | 79.6 | 561 | 20.4 | 144 |
| Missing | 0.2 | 3 | 100.0 | 3 | 0.0 | 0 |
| Worries about money | ||||||
| No worries | 68.8 | 860 | 85.6 | 736 | 14.4 | 124 |
| Yes worries | 30.6 | 383 | 76.2 | 292 | 23.8 | 91 |
| Missing | 0.6 | 7 | 85.7 | 6 | 14.3 | 1 |
| Housing problems | ||||||
| No problems | 68.3 | 854 | 85.0 | 726 | 15.0 | 128 |
| Yes problems | 31.5 | 394 | 77.7 | 306 | 22.3 | 88 |
| Missing | 0.2 | 2 | 100.0 | 2 | 0.0 | 0 |
| Negative major life events | ||||||
| 0-1 events | 44.7 | 559 | 86.6 | 484 | 13.4 | 75 |
| 2-9 events | 52.2 | 652 | 80.1 | 522 | 19.9 | 130 |
| Missing | 3.1 | 39 | 71.8 | 28 | 28.2 | 11 |
| Family cohesion | ||||||
| Always or most times get along | 92.1 | 1151 | 83.7 | 963 | 16.3 | 188 |
| Sometimes to never get along | 7.9 | 99 | 71.7 | 71 | 28.3 | 28 |
| Living on country | ||||||
| Live on country | 37.3 | 466 | 80.0 | 373 | 20.0 | 93 |
| Do not live on country | 42.6 | 532 | 82.9 | 441 | 17.1 | 91 |
| Missing | 20.2 | 252 | 87.3 | 220 | 12.7 | 32 |
| Child speaks an Indigenous language | ||||||
| Yes does speak | 24.2 | 302 | 84.4 | 255 | 15.6 | 47 |
| No does not speak | 73.4 | 918 | 82.6 | 758 | 17.4 | 160 |
| Missing | 2.4 | 30 | 70.0 | 21 | 30.0 | 9 |
| Child feels safe at school | ||||||
| Yes | 79.4 | 992 | 86.2 | 855 | 13.8 | 137 |
| Sometimes or no | 17.1 | 214 | 70.1 | 150 | 29.9 | 64 |
| Missing | 3.5 | 44 | 65.9 | 29 | 34.1 | 15 |
| Child positive peer relationships | ||||||
| Not bullied at school | 69.7 | 871 | 87.3 | 760 | 12.7 | 111 |
| Bullied at school | 27.4 | 343 | 72.9 | 250 | 27.1 | 93 |
| Missing | 2.9 | 36 | 66.7 | 24 | 33.3 | 12 |
| Caregiver trusts local school | ||||||
| Strongly agree or agree | 82.2 | 1027 | 84.4 | 867 | 15.6 | 160 |
| Neutral to disagree | 16.9 | 211 | 75.4 | 159 | 24.6 | 52 |
| Missing | 1.0 | 12 | 66.7 | 8 | 33.3 | 4 |
| Caregiver feels connected to community | ||||||
| Yes connected | 76.7 | 959 | 84.2 | 807 | 15.9 | 152 |
| Sometimes or not connected | 19.0 | 237 | 76.8 | 182 | 23.2 | 55 |
| Missing | 4.3 | 54 | 83.3 | 45 | 16.7 | 9 |
Table A3.
Associations between exposures and alternate categorisation of child mental health, according to the Deficit Approach, Protective Factors Approach, and Positive Outcome Approach
| SENSITIVITY ANALYSIS 1: Alternate categorisation of mental health |
Deficit Approach: PR of poor vs. good-moderate mental health |
Protective Factors Approach: PR of poor vs. good-moderate mental health |
Positive Outcome Approach: PR of good-moderate vs. poor mental health |
||||||
|---|---|---|---|---|---|---|---|---|---|
| PR | 95%CI | P-value | PR | 95%CI | P-value | PR | 95%CI | P-value | |
| Child age | |||||||||
| 7–8 years | 1.30 | (1.02,1.65) | 0.04 | 1 | (ref) | 1 | (ref) | ||
| 9–13 years | 1 | (ref) | 0.77 | (0.60,0.98) | 0.04 | 1.06 | (1.00,1.11) | 0.04 | |
| Child gender | |||||||||
| Male | 1.33 | (1.04,1.70) | 0.02 | 1 | (ref) | ||||
| Female | 1 | (ref) | 0.75 | (0.59,0.96) | 0.02 | 1.06 | (1.01,1.12) | 0.02 | |
| Child general health | |||||||||
| Excellent or very good | 1 | (ref) | 0.71 | (0.54,0.94) | 0.02 | 1.08 | (1.01,1.17) | 0.04 | |
| Good, fair, or poor | 1.41 | (1.07,1.86) | 0.02 | 1 | (ref) | 1 | (ref) | ||
| Caregiver mental health | |||||||||
| Good | 1 | (ref) | 0.4 | (0.32,0.51) | <0.01 | 1.27 | (1.17,1.37) | <0.01 | |
| Poor | 2.47 | (1.95,3.14) | <0.01 | 1 | (ref) | 1 | (ref) | ||
| Caregiver employment | |||||||||
| Employed | 1 | (ref) | 0.65 | (0.50,0.84) | <0.01 | 1.09 | (1.04,1.15) | <0.01 | |
| Not employed | 1.54 | (1.19,1.99) | <0.01 | 1 | (ref) | 1 | (ref) | ||
| Worries about money | |||||||||
| No worries | 1 | (ref) | 0.61 | (0.48,0.77) | <0.01 | 1.12 | (1.05,1.19) | <0.01 | |
| Yes worries | 1.65 | (1.29,2.10) | <0.01 | 1 | (ref) | 1 | (ref) | ||
| Housing problems | |||||||||
| No problems | 1 | (ref) | 0.67 | (0.53,0.86) | <0.01 | 1.09 | (1.03,1.16) | <0.01 | |
| Yes problems | 1.49 | (1.17,1.90) | <0.01 | 1 | (ref) | 1 | (ref) | ||
| Negative major life events | |||||||||
| 0-1 events | 1 | (ref) | 0.67 | (0.52,0.87) | <0.01 | 1.08 | (1.03,1.14) | <0.01 | |
| 2-9 events | 1.49 | (1.14,1.93) | <0.01 | 1 | (ref) | 1 | (ref) | ||
| Family cohesion | |||||||||
| Always or most times | 1 | (ref) | 0.58 | (0.41,0.81) | <0.01 | 1.17 | (1.03,1.32) | 0.02 | |
| Sometimes, or not really | 1.73 | (1.23,2.43) | <0.01 | 1 | (ref) | 1 | (ref) | ||
| Living on country | |||||||||
| Live on country | 1.17 | (0.90,1.51) | 0.25 | 1 | (ref) | 1 | (ref) | ||
| Do not live on country | 1 | (ref) | 0.86 | (0.66,1.11) | 0.25 | 1.04 | (0.98,1.10) | 0.25 | |
| Child speaks an Indigenous language | |||||||||
| Yes does speak | 1 | (ref) | 0.89 | (0.66,1.20) | 0.46 | 1.02 | (0.97,1.08) | 0.44 | |
| No does not speak | 1.12 | (0.83,1.51) | 0.46 | 1 | (ref) | 1 | (ref) | ||
| Child feels safe at school | |||||||||
| Yes | 1 | (ref) | <0.01 | 0.46 | (0.36,0.60) | <0.01 | 1.23 | (1.12,1.35) | <0.01 |
| Sometimes or no | 2.17 | (1.67,2.80) | 1 | (ref) | 1 | (ref) | |||
| Child positive peer relationships | |||||||||
| Not bullied at school | 1 | (ref) | <0.01 | 0.47 | (0.37,0.60) | <0.01 | 1.2 | (1.12,1.28) | <0.01 |
| Bullied at school | 2.13 | (1.66,2.72) | 1 | (ref) | 1 | (ref) | |||
| Caregiver trusts local school | |||||||||
| Strongly agree or agree | 1 | (ref) | <0.01 | 0.63 | (0.48,0.83) | <0.01 | 1.12 | (1.03,1.22) | 0.01 |
| Neutral to disagree | 1.58 | (1.20,2.08) | 1 | (ref) | 1 | (ref) | |||
| Caregiver feels connected to community | |||||||||
| Yes connected | 1 | (ref) | 0.01 | 0.68 | (0.52,0.90) | 0.01 | 1.1 | (1.02,1.18) | 0.02 |
| Sometimes or not connected | 1.46 | (1.11,1.93) | 1 | (ref) | 1 | (ref) | |||
Table A4.
Associations between exposures and child mental health using log-binomial models, according to the Deficit Approach, Protective Factors Approach, and Positive Outcome Approach
| SENSITIVITY ANALYSIS 2: Log-Binomial models |
Deficit Approach: PR of poor-moderate vs. good mental health |
Protective Factors Approach: PR of poor-moderate vs. good mental health |
Positive Outcome Approach: PR of good vs. poor-moderate mental health |
|||||||
|---|---|---|---|---|---|---|---|---|---|---|
| PR | 95%CI | P-value | PR | 95%CI | P-value | PR | 95%CI | P-value | ||
| Child age | ||||||||||
| 7–8 years | 1.18 | (1.01,1.38) | 0.04 | 1 | (ref) | 1 | (ref) | |||
| 9–13 years | 1 | (ref) | 0.85 | (0.72,0.99) | 0.04 | 0.85 | (0.72,0.99) | 0.04 | ||
| Child gender | ||||||||||
| Male | 1.21 | (1.03,1.42) | 0.02 | 1 | (ref) | 1 | (ref) | |||
| Female | 1 | (ref) | 0.82 | (0.70,0.97) | 0.02 | 0.82 | (0.70,0.97) | 0.02 | ||
| Child general health | ||||||||||
| Excellent or very good | 1 | (ref) | 0.7 | (0.58,0.83) | <0.01 | 0.7 | (0.58,0.83) | <0.01 | ||
| Good, fair, or poor | 1.44 | (1.20,1.71) | <0.01 | 1 | (ref) | 1 | (ref) | |||
| Caregiver mental health | ||||||||||
| Good | 1 | (ref) | 0.46 | (0.40,0.54) | <0.01 | 0.46 | (0.40,0.54) | <0.01 | ||
| Poor | 2.16 | (1.86,2.51) | <0.01 | 1 | (ref) | 1 | (ref) | |||
| Caregiver employment | ||||||||||
| Employed | 1 | (ref) | 0.78 | (0.66,0.92) | <0.01 | 0.78 | (0.66,0.92) | <0.01 | ||
| Not employed | 1.29 | (1.09,1.52) | <0.01 | 1 | (ref) | 1 | (ref) | |||
| Worries about money | ||||||||||
| No worries | 1 | (ref) | 0.69 | (0.59,0.81) | <0.01 | 0.69 | (0.59,0.81) | <0.01 | ||
| Yes worries | 1.45 | (1.23,1.69) | <0.01 | 1 | (ref) | 1 | (ref) | |||
| Housing problems | ||||||||||
| No problems | 1 | (ref) | 0.83 | (0.70,0.97) | 0.02 | 0.83 | (0.70,0.97) | 0.02 | ||
| Yes problems | 1.21 | (1.03,1.42) | 0.02 | 1 | (ref) | 1 | (ref) | |||
| Negative major life events | ||||||||||
| 0-1 events | 1 | (ref) | 0.76 | (0.64,0.89) | <0.01 | 0.76 | (0.64,0.89) | <0.01 | ||
| 2-9 events | 1.32 | (1.12,1.56) | <0.01 | 1 | (ref) | 1 | (ref) | |||
| Family cohesion | ||||||||||
| Always or most times | 1 | (ref) | 0.65 | (0.52,0.81) | <0.01 | 0.65 | (0.52,0.81) | <0.01 | ||
| Sometimes, or not really | 1.55 | (1.24,1.93) | <0.01 | 1 | (ref) | 1 | (ref) | |||
| Living on country | ||||||||||
| Live on country | 1.18 | (0.72,1.01) | 0.07 | 1 | (ref) | 1 | (ref) | |||
| Do not live on country | 1 | (ref) | 0.85 | (0.72,1.01) | 0.07 | 0.85 | (0.72,1.01) | 0.07 | ||
| Child speaks an Indigenous language | ||||||||||
| Yes does speak | 1 | (ref) | 0.88 | (0.73,1.08) | 0.22 | 0.88 | (0.73,1.08) | 0.22 | ||
| No does not speak | 1.13 | (0.93,1.38) | 0.22 | 1 | (ref) | 1 | (ref) | |||
| Child feels safe at school | ||||||||||
| Yes | 1 | (ref) | 0.54 | (0.46,0.63) | <0.01 | 0.54 | (0.46,0.63) | <0.01 | ||
| Sometimes or no | 1.87 | (1.59,2.20) | <0.01 | 1 | (ref) | 1 | (ref) | |||
| Child bullied at school | ||||||||||
| Not bullied | 1 | (ref) | 0.52 | (0.44,0.61) | <0.01 | 0.52 | (0.44,0.61) | <0.01 | ||
| Yes bullied | 1.92 | (1.65,2.25) | <0.01 | 1 | (ref) | 1 | (ref) | |||
| Caregiver trusts local school | ||||||||||
| Strongly agree or agree | 1 | (ref) | 0.64 | (0.54,0.77) | <0.01 | 0.64 | (0.54,0.77) | <0.01 | ||
| Neutral to disagree | 1.55 | (1.30,1.85) | <0.01 | 1 | (ref) | 1 | (ref) | |||
| Caregiver feels connected to community | ||||||||||
| Yes connected | 1 | (ref) | 0.76 | (0.64,0.91) | <0.01 | 0.76 | (0.64,0.91) | <0.01 | ||
| Sometimes or not connected | 1.31 | (1.09,1.57) | <0.01 | 1 | (ref) | 1 | (ref) | |||
Table A5.
Interpretation of findings, according to the Deficit Approach, Protective Factors Approach, and Positive Outcome Approach
| Deficit Approach: PR of poor-moderate vs. good mental health | Protective Factors Approach: PR of poor-moderate vs. good mental health | Positive Outcome Approach: PR of good vs. poor-moderate mental health | |
|---|---|---|---|
| Child general health *†‡t | Poor-moderate mental health is significantly more common among children whose health is good, fair, or poor compared to excellent or very good. | Poor-moderate mental health is significantly less common among children whose health is excellent or very good compared to good, fair, or poor. | Good mental health is significantly more common among children whose health is excellent or very good compared to good, fair, or poor. |
| Caregiver mental health *†‡ | Poor-moderate mental health is significantly more common among children whose caregivers have poor mental health compared to good mental health. | Poor-moderate mental health is significantly less common among children whose caregivers have good mental health compared to poor mental health. | Good mental health is significantly more common among children whose caregivers have good mental health compared to those whose caregivers have poor mental health. |
| Caregiver employment *†‡ | Poor-moderate mental health is significantly more common among children whose caregivers are not employed compared to those who are employed. | Poor-moderate mental health is significantly less common among children whose caregivers are employed compared to those who are not employed. | Good mental health is significantly more common among children whose caregivers are employed compared to those who are not employed. |
| Worries about money *†‡ | Poor-moderate mental health is significantly more common among children whose families have worries about money compared to children whose families do not have worries about money. | Poor-moderate mental health is significantly less common among children whose families do not have worries about money compared to children whose families do have worries about money. | Good mental health is significantly more common among children whose families do not have worries about money compared to children whose families do have worries about money. |
| Housing problems *†‡ | Poor-moderate mental health is significantly more common among children whose families have housing problems compared to children whose families do not have housing problems. | Poor-moderate mental health is significantly less common among children whose families do not have housing problems compared to children whose families do have housing problems. | Good mental health is significantly more common among children whose families do not have housing problems compared to children whose families do have housing problems. |
| Negative major life events *†‡ | Poor-moderate mental health is significantly more common among children whose families have 2 to 9 negative major life events, compared to 0 to 1, negative major life events. | Poor-moderate mental health is significantly less common among children whose families have 0 to 1 negative major life events, compared to 2 to 9, negative major life events. | Good mental health is significantly more common among children whose families have 0 to 1 negative major life events, compared to 2 to 9, negative major life events. |
| Family cohesion *†‡ | Poor-moderate mental health is significantly more common among children whose families don't get along well, compared to children whose families do get along well. | Poor-moderate mental health is significantly less common among children whose families do get along well, compared to children whose families don't get along well. | Good mental health is significantly more common among children whose families do get along well, compared to children whose families don't get along well. |
| Living on country | There is no significant difference in the prevalence of poor mental health between children whose caregivers do not live on country compared to those who do live on country. | There is no significant difference in the prevalence of poor mental health between children whose caregivers do live on country compared to those who do not live on country. | There is no significant difference in the prevalence of good mental health between children whose caregiver lives on country compared to those who do not live on country. |
| Child speaks an Indigenous language | There is no significant difference in the prevalence of poor mental health between children who do not speak an Indigenous language, compared to speak an Indigenous language. | There is no significant difference in the prevalence of poor mental health between children who not speak an Indigenous language, compared to do not speak an Indigenous language. | There is no significant difference in the prevalence of poor mental health between children who do not speak an Indigenous language, compared to those who do not speak an Indigenous language. |
| Child feels safe at school *†‡ | Poor-moderate mental health is significantly more common among children who do not feel safe at school, compared to those who feel safe at school. | Poor-moderate mental health is significantly less common among children who feel safe at school, compared to those who do not feel safe at school. | Good mental health is significantly more common among children who feel safe at school, compared to those who do not feel safe at school. |
| Child positive peer relationships at school *†‡ | Poor-moderate mental health is significantly more common among children who are bullied at school, compared to not bullied. | Poor-moderate mental health is significantly less common among children who are not bullied at school, compared to bullied. | Good mental health is significantly more common among children who are not bullied at school, compared to bullied. |
| Caregiver trusts local school *†‡ | Poor-moderate mental health is significantly more common among children whose caregiver does not trust the school, compared to those who do trust the school. | Poor-moderate mental health is significantly less common among children whose caregiver does trust the school, compared to those who do not trust the school. | Good mental health is significantly more common among children whose caregiver does trust the school, compared to those who do not trust the school. |
| Caregiver feels connected to community*†‡ | Poor-moderate mental health is significantly more common among children whose caregiver does not feel connected to community, compared to those who feel connected. | Poor-moderate mental health is significantly less common among children whose caregiver does feel connected to community, compared to those who do not feel connected. | Good mental health is significantly more common among children whose caregiver does feel connected to community, compared to those who do not feel connected. |
* Association is significant in the Deficit Approach.
† Association is significant in the Protective Factors Approach. ‡ Association is significant in the Positive Outcome Approach.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- Antonovsky A. The salutogenic model as a theory to guide health promotion. Health Promotion International. 1996;11(1):11–18. doi: 10.1093/heapro/11.1.11. [DOI] [Google Scholar]
- Australian Government Department of Health . Department of Health; Canberra, Australia: 2016. Primary mental health care minimum data set: Overview of purpose, design, scope and key decision issues. [Google Scholar]
- Australian Health Ministers' Advisory Council . Australian Health Ministers’ Advisory Council; Canberra, Australia: 2017. Aboriginal and Torres Strait islander health performance framework 2017 report.http://www.health.gov.au/indigenous-hpf/ Retrieved from. [Google Scholar]
- Australian Institute of Health and Welfare . Australian Institute of Health and Welfare; Canberra, Australia: 2016. Tobacco indicators: Measuring midpoint progress—reporting under the national tobacco strategy 2012–2018. Drug statistics series no. 30. PHE 210. (1742491480. [Google Scholar]
- Becker C.M., Glascoff M.A., Felts W.M. Salutogenesis 30 Years later: Where do we go from here? The International Electronic Journal of Health Education. 2010;13:25–32. [Google Scholar]
- Bond C. A culture of ill health: Public health or aboriginality? Medical Journal of Australia. 2005;183(1):39–41. doi: 10.5694/j.1326-5377.2005.tb06891.x. [DOI] [PubMed] [Google Scholar]
- Bond C. Starting at strengths... An indigenous early years intervention. Medical Journal Australia. 2009;191(3):175–177. doi: 10.5694/j.1326-5377.2009.tb02733.x. [DOI] [PubMed] [Google Scholar]
- Bulloch H., Fogarty W. Aboriginal and Torres Strait islander health: Watching our words. 2018. https://www.doctorportal.com.au/mjainsight/2018/46/aboriginal-and-torres-strait-islander-health-watching-our-words/ 26 November. Retrieved from.
- Bulloch H., Fogarty W., Bellchambers K. The Lowitja Institute; Melbourne, Australia: 2019. Aboriginal health and wellbeing services: Putting community-driven strengths-based approaches into practice. [Google Scholar]
- Cohen G.L., Sherman D.K. The Psychology of Change: Self-affirmation and social psychological intervention. Annual Review of Psychology. 2014;65:333–371. doi: 10.1146/annurev-psych-010213-115137. [DOI] [PubMed] [Google Scholar]
- Cummings P. The relative merits of risk ratios and odds ratios. Archives of Pediatrics & Adolescent Medicine. 2009;163(5):438–445. doi: 10.1001/archpediatrics.2009.31. [DOI] [PubMed] [Google Scholar]
- Durie M. Understanding Health and Illness: Research at the interface between science and indigenous knowledge. International Journal of Epidemiology. 2004;33(5):1138–1143. doi: 10.1093/ije/dyh250. [DOI] [PubMed] [Google Scholar]
- Fforde C., Bamblett L., Lovett R., Gorringe S., Fogarty W. Discourse, Deficit and Identity: Aboriginality, the race paradigm and the language of representation in contemporary Australia. Media International Australia. 2013;149(1):162–173. doi: 10.1177/1329878X1314900117. [DOI] [Google Scholar]
- Fogarty W., Bulloch H., McDonnell S., Davis M. The Lowitja Institute; Melbourne, Australia: 2018. Deficit discourse and indigenous health: How narrative framings of aboriginal and Torres Strait islander people are reproduced in policy.https://www.lowitja.org.au/lowitja-publishing/l056 Retrieved from. [Google Scholar]
- Fogarty W., Lovell M., Langenberg J., Heron M.-J. The Lowitja Institute; Melbourne, Australia: 2018. Deficit discourse and strengths-based approaches: Changing the narrative of Aboriginal and Torres Strait Islander health and wellbeing. [Google Scholar]
- Foley W., Schubert L. Applying strengths-based approaches to nutrition research and interventions in indigenous Australian communities. Journal of Critical Dietetics. 2013;1(3):15–25. [Google Scholar]
- Goodman R. A modified version of the rutter parent Questionnaire including extra items on children's strengths: A research note. Journal of Child Psychology and Psychiatry. 1994;35(8):1483–1494. doi: 10.1111/j.1469-7610.1994.tb01289.x. [DOI] [PubMed] [Google Scholar]
- Goodman R. The strengths and Difficulties Questionnaire: A research note. Journal of Child Psychology and Psychiatry. 1997;38(5):581–586. doi: 10.1111/j.1469-7610.1997.tb01545.x. [DOI] [PubMed] [Google Scholar]
- Goodman R. Psychometric properties of the strengths and Difficulties Questionnaire. Journal of the American Academy of Child & Adolescent Psychiatry. 2001;40(11):1337–1345. doi: 10.1097/00004583-200111000-00015. [DOI] [PubMed] [Google Scholar]
- Gray M.A., Oprescu F.I. Role of non-indigenous researchers in indigenous health research in Australia: A review of the literature. Australian Health Review. 2015;40:459–465. doi: 10.1071/AH15103. [DOI] [PubMed] [Google Scholar]
- Gubhaju L., Banks E., Ward J., D'Este C., Ivers R., Roseby R.…Liu B. ‘Next generation youth well-being Study:’understanding the health and social well-being trajectories of Australian aboriginal adolescents aged 10–24 years: Study protocol. BMJ open. 2019;9(3) doi: 10.1136/bmjopen-2018-028734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haswell-Elkins M., Sebasio T., Hunter E., Mar M. Challenges of measuring the mental health of indigenous Australians: Honouring ethical expectations and driving greater accuracy. Australasian Psychiatry. 2007;15(Supp 1):S29–S33. doi: 10.1080/10398560701701155. [DOI] [PubMed] [Google Scholar]
- Henson M., Sabo S., Trujillo A., Teufel-Shone N. Identifying protective factors to promote health in American Indian and Alaska native adolescents: A literature review. Journal of Primary Prevention. 2017;38(1–2):5–26. doi: 10.1007/s10935-016-0455-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holmes W., Stewart P., Garrow A., Anderson I., Thorpe L. Researching Aboriginal Health: Experience from a study of urban young people's health and well-being. Social Science & Medicine. 2002;54(8):1267–1279. doi: 10.1016/S0277-9536(01)00095-8. [DOI] [PubMed] [Google Scholar]
- Jones C.P. Invited commentary:“race,” racism, and the practice of epidemiology. American Journal of Epidemiology. 2001;154(4):299–304. doi: 10.1093/aje/154.4.299. [DOI] [PubMed] [Google Scholar]
- Laliberté A., Haswell-Elkins M., Reilly L. The healing journey: Empowering aboriginal communities to close the health gap. Australasian Psychiatry. 2009;17(1_suppl):S64–S67. doi: 10.1080/10398560902948704. [DOI] [PubMed] [Google Scholar]
- Le Grande M., Ski C.F., Thompson D.R., Scuffham P., Kularatna S., Jackson A.C. Social and emotional wellbeing assessment instruments for use with indigenous Australians: A critical review. Social Science & Medicine. 2017;187:164–173. doi: 10.1016/j.socscimed.2017.06.046. [DOI] [PubMed] [Google Scholar]
- Lindström B., Eriksson M. Salutogenesis. Journal of Epidemiology & Community Health. 2005;59(6):440–442. doi: 10.1136/jech.2005.034777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lovett R., Thurber K.A., Wright A., Maddox R., Banks E. Deadly progress: Changes in aboriginal and Torres Strait islander smoking prevalence, 2004-2015. Public Health Research and Practice. 2017;27(5) doi: 10.17061/phrp2751742. [DOI] [PubMed] [Google Scholar]
- Marmor A., Harley D. What promotes social and emotional wellbeing in aboriginal and Torres Strait islander children? Lessons in measurement from the longitudinal study of indigenous children. Australian Institute of Family Studies: Family Matters. 2018;100:1–18. https://search.informit.com.au/documentSummary;dn=765360684971624;res=IELHSS [Google Scholar]
- Mittelmark M.B., Bauer G.F. The handbook of salutogenesis. Springer; Cham: 2017. The meanings of salutogenesis; pp. 7–13. [Google Scholar]
- Mittelmark M.B., Bull T. The salutogenic model of health in health promotion research. Global Health Promotion. 2013;20(2):30–38. doi: 10.1177/1757975913486684. [DOI] [PubMed] [Google Scholar]
- National Aboriginal Health Strategy Working Party . 1989. National aboriginal health strategy. Canberra, Australia. [Google Scholar]
- National Health and Medical Research Council . National Health and Medical Research Council; 2002. The nhmrc road map: A strategic framework for improving aboriginal and Torres Strait islander health through research. Canberra, Australia: Aboriginal and Torres Strait island research agenda working group. [DOI] [PubMed] [Google Scholar]
- Nicholson R.A., Kreuter M.W., Lapka C., Wellborn R., Clark E.M., Sanders-Thompson V.…Casey C. Unintended effects of emphasizing disparities in cancer communication to african-Americans. Cancer Epidemiology and Prevention Biomarkers. 2008;17(11):2946–2953. doi: 10.1158/1055-9965.EPI-08-0101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Penman R. Australian Government Department of Families Housing Community Services and Indigenous Affairs; Canberra, Australia: 2006. Occasional paper No. 15 -- the 'growing up' of aboriginal and Torres Strait islander children: A literature review. [Google Scholar]
- Pyett P., Waples-Crowe P., van der Sterren A. Challenging our own practices in indigenous health promotion and research. Health Promotion Journal of Australia. 2008;19(3):179–183. doi: 10.1071/HE08179. [DOI] [PubMed] [Google Scholar]
- Rossingh B., Yunupingu Y. Evaluating as an outsider or an insider: A two-way approach guided by the knowers of culture. Evaluation Journal of Australasia. 2016;16(3):5. doi: 10.1177/1035719X1601600302. [DOI] [Google Scholar]
- Salmon M., Skelton F., Thurber K.A., Bennetts Kneebone L., Gosling J., Lovett R. Intergenerational and early life influences on the well-being of Australian aboriginal and Torres Strait islander children: Overview and selected findings from Footprints in time, the longitudinal study of indigenous children. Journal of Developmental Origins of Health and Disease. 2018:1–7. doi: 10.1017/S204017441800017X. [DOI] [PubMed] [Google Scholar]
- Search investigators The study of environment on aboriginal resilience and child health (SEARCH): Study protocol. BMC Public Health. 2010;10(1):287. doi: 10.1186/1471-2458-10-287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith L.T. Zed Books Ltd; 2005. Decolonizing methodologies: Research and indigenous peoples. [Google Scholar]
- Smylie J., Anderson M. Understanding the health of indigenous peoples in Canada: Key methodological and conceptual challenges. Canadian Medical Association Journal. 2006;175(6) doi: 10.1503/cmaj.060940. 602-602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smylie J., Lofters A., Firestone M., O'Campo P. Chapter 4. Population-based data and community empowerment. In: O'Campo P., Dunn J.R., editors. Rethinking social epidemiology: Towards a science of change. Springer Science & Business Media; New York: 2011. [Google Scholar]
- Stoneham M., Goodman J., Daube M. The portrayal of indigenous health in selected Australian media. The International Indigenous Policy Journal. 2014;5(1):1–13. http://hdl.handle.net/20.500.11937/33658 [Google Scholar]
- Sweet M. 2009. Is the media part of the aboriginal health problem, and part of the solution.https://insidestory.org.au/is-the-media-part-of-the-aboriginal-health-problem-and-part-of-the-solution/ Accessed 12 June 2019). Inside story. Retrieved from. [Google Scholar]
- Thurber K.A., Banks E., Banwell C. Cohort profile: Footprints in time, the Australian longitudinal study of indigenous children. International Journal of Epidemiology. 2014 doi: 10.1093/ije/dyu122. dyu122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thurber K.A., Walker J., Dunbar T., Guthrie J., Calear A., Batterham P.…Lovett R. Commissioned by the Australian Government Department of Social Services; Canberra, Australia: 2019. Technical Report: Measuring child mental health, psychological distress, and social and emotional wellbeing in the Longitudinal Study of Indigenous Children. [Google Scholar]
- Walter M., Andersen C. Left Coast Press Inc; Walnut Creek, United States: 2013. Indigenous statistics: A quantitative research methodology. [Google Scholar]
- Wand A.P.F., Eades S.J. Navigating the process of developing a research project in aboriginal health. Medical Journal of Australia. 2008;188(10):584. doi: 10.5694/j.1326-5377.2008.tb01796.x. [DOI] [PubMed] [Google Scholar]
- Williamson A., McElduff P., Dadds M., D'Este C., Redman S., Raphael B.…Eades S. The construct validity of the strengths and Difficulties Questionnaire for aboriginal children living in urban new south wales, Australia. Australian Psychologist. 2014;49(3):163–170. doi: 10.1111/ap.12045. [DOI] [Google Scholar]
- Williamson A., Redman S., Dadds M., Daniels J., D'Este C., Raphael B. Acceptability of an emotional and behavioural screening tool for children in Aboriginal Community Controlled Health Services in urban NSW. Australian and New Zealand Journal of Psychiatry. 2010;44(10):894–900. doi: 10.3109/00048674.2010.489505. [DOI] [PubMed] [Google Scholar]
- Zubrick S., Lawrence D., De Maio J., Biddle N. Australian Bureau of Statistics; Canberra, Australia: 2006. Testing the reliability of a measure of aboriginal children's mental health: An analysis based on the western Australian aboriginal child health survey-cat. No. 1351.0.55.011. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.