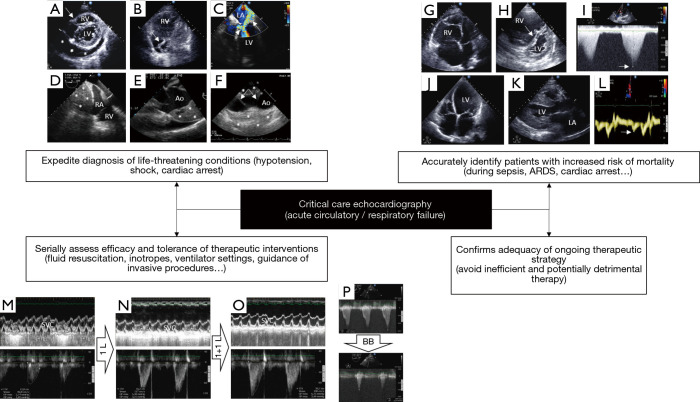
Figure 1.
Illustrative examples of the diagnostic capabilities of critical care echocardiography in patients with cardiopulmonary compromise, when performed by the transthoracic or transesophageal approach according to clinical settings. (A) Parasternal short-axis view depicting a large pericardial effusion (asterisks) with tamponade physiology (inverted right ventricular free wall, arrow); (B) apical four-chamber view depicting enlarged right cardiac cavities and a thrombus-in-transit highly mobile within the right atrium in real time (arrow); (C) transesophageal echocardiography four-chamber view disclosing a massive eccentric mitral regurgitation due to a systolic anterior motion of the mitral valve (arrow); note that a dynamic left ventricular outflow tract obstruction is present, as reflected by a highly turbulent flow with color Doppler mapping (arrowhead); (D) transesophageal echocardiography view depicting a large mediastinal hematoma (asterisks) impeding right atrial filling and resulting in extracardiac tamponade physiology after a complicated open-heart surgery; (E) transesophageal echocardiography view showing a large intramural hematoma of the initial ascending aorta (asterisks) associated with hemopericardium in a patient ventilated for acute circulatory failure; (F) longitudinal transesophageal echocardiography view depicting a complex medial tear (arrows) associated with a subadventitial disruption of the aortic isthmus in a patient ventilated for severe blunt chest trauma. Note the large posterior hemomediastinum (asterisks) which reflects the risk of imminent lethal blood extravasation; (G) apical four-chamber view disclosing a marked enlargement of the right ventricle which size exceeds that of the left ventricle in a patient under protective ventilation for an acute respiratory distress syndrome; (H) in the same patient, the parasternal short axis view confirms the marked dilatation of the right ventricular cavity and depicts a bulging of the interventricular septum towards the left ventricle at end-systole (arrow). Taken together, these findings are consistent with a severe acute cor pulmonale; (I) maximal Doppler tricuspid regurgitation velocity (arrow) allows estimating quantitatively the systolic pressure gradient between the right atrium and right ventricle. In this patient hospitalized for a decompensated chronic respiratory insufficiency, pulmonary artery systolic pressure is estimated at approximately 110 mmHg; (J) apical four-chamber view depicting a dilated cardiomyopathy in a patient sustaining cardiogenic shock; (K) parasternal long-axis view showing a concentric hypertrophic cardiomyopathy in a patient who presented with cardiogenic pulmonary edema. Note the marked left atrial dilatation reflecting chronically elevated filling pressures; (L) in the same patient, tissue Doppler imaging at the lateral aspect of the mitral ring depicts markedly low E’ velocity (arrow), consistent with severe left ventricular diastolic dysfunction (impaired relaxation); (M) transesophageal echocardiography monitoring the effects of serial fluid challenges in a hypotensive ventilated patient with early septic shock. At baseline, marked respiratory variation of the superior vena cava with inspiratory collapse indicates preload dependence (upper panel) at the origin of reduced left ventricular stroke volume, as reflected by a decreased velocity-time integral of left ventricular outflow tract (lower panel; 12.8 cm); (N) after a 1-L fluid challenge, the velocity-time integral of left ventricular outflow tract significantly increased (lower panel; 16.2 cm) while variation of the size of the superior vena cava within the respiratory cycle remains relevant (upper panel); (O) after a second 1-L fluid challenge, the velocity-time integral of left ventricular outflow tract significantly increased (lower panel; 20.7 cm), while respiratory variation of superior vena cava decreased (upper panel); (P) left ventricular outflow tract obstruction in an elderly patient with septal hypertrophy who was assessed for weaning-induced pulmonary oedema (upper panel; maximal pressure gradient: 131 mmHg). Beta-blocker therapy markedly decreased the dynamic outflow tract obstruction, allowing successful ventilator weaning (lower panel; maximal pressure gradient: 16 mmHg). RV, right ventricle; LV, left ventricle; LA, left atrium; RA, right atrium; Ao, aorta; SVC, superior vena cava; BB, beta-blocker.