 Diabetes mellitus is of major public health concerns; its incidence is continuously increasing.
Diabetes mellitus is of major public health concerns; its incidence is continuously increasing.
Abstract
Background: Diabetes mellitus is of major public health concerns; its incidence is continuously increasing. Diabetes mellitus is associated with a high risk of cardiovascular complications such as hypertension. Red wine has been reported to reduce cardiovascular risk factors. We quantified the effects of red wine on cardiovascular factors. Methods: We retrieved English-language articles published from January 1990 to April 2019. Cardiovascular risk factors were compared using means with 95% confidence intervals (95% CIs). Results: We identified five eligible randomized controlled trials. Diabetic patients who drank red wine exhibited significantly reduced systolic blood pressure (BP) (mean difference [MD] –1.33, 95% CI –1.81, –0.85) and diastolic BP (MD –1.31, 95% CI –1.80, –0.83) than those who did not. Compared to the observations for diabetics who did not drink red wine, the high-density lipoprotein (HDL) level was significantly higher in red wine drinkers (MD –0.24, 95% CI –0.39, –0.09). However, red wine had no effect on the body mass index (BMI) (MD –0.27, 95% CI –1.80, 1.25), the total cholesterol level (MD 0.13, 95% CI –0.17, 0.44), or the low-density lipoprotein (LDL) level (MD 0.08, 95% CI –0.21, 0.37). Conclusions: Red wine consumption significantly lowered BP and increased the HDL level in diabetics. Red wine had no significant effect on BMI or cholesterol and LDL levels. Given the heterogeneity of the studied populations and the lack of standardization and completeness across the published studies, caution is required while interpreting these findings.
1. Introduction
Diabetes is a non-communicable disease that has become a major cause of mortality worldwide.1 In 2012, of the 38 million deaths from non-communicable diseases that were reported globally, 1.5 million deaths were from diabetes and 17.5 million deaths were from cardiovascular diseases.1 Diabetes is among the most prevalent chronic diseases; it affected 333 million persons in 2005 but the number increased dramatically to 435 million in 2015.2 Concern about the greater risk of cardiovascular diseases in diabetics is rising, with obesity, elevated blood pressure (BP), and high cholesterol levels as major risk factors. Treatments to reduce these risks are urgently required.
Wine is one of the most popular drinks worldwide; approximately 70% of wine is red wine.3 Wine production commenced in Persia in 6000 B.C.4 Wine is a rich dietary source of resveratrol, a bioactive polyphenol of grape roots; red wine has been reported to benefit health, in particular, by reducing the risks of diabetes and cardiovascular diseases.5–7
Earlier randomized controlled trials (RCTs) indicated that red wine significantly increased the high-density lipoprotein cholesterol (HDL-C) level and decreased the total cholesterol : HDL-C ratio.8 It is essential to modify the serum cholesterol landscape to protect against cardiovascular diseases.9 In diabetic rats, resveratrol prevents cardiovascular effects by exerting an anti-oxidative action.10 However, any such effects in human diabetics have not been well evaluated. The results of RCTs exploring whether red wine reduces cardiovascular risk factors (BP, total cholesterol, and HDL and LDL levels) in diabetics have been inconsistent possibly because of different confounding factors. For example, the wine consumption level may affect the risk as may the country, region, or diabetes type. Therefore, we systematically reviewed relevant RCTs using the recognized meta-analysis methodology; we explored whether red wine influenced the body mass index (BMI), BP, and total cholesterol, HDL, and LDL levels. Previous studies have revealed that red wine conserves different organic compounds from grapes, such as polysaccharides and flavonoids, which have been known to possess anti-inflammatory and antioxidant properties.11
The purpose of this study was to conduct the association between moderate red wine intake and cardiovascular risk among diabetic population by performing a meta-analysis of randomized clinical trials (RCTs).
2. Methods
We adhered to the PRISMA statement when systematically reviewing and meta-analyzing whether diabetics who did or did not drink red wine differed in terms of cardiovascular risk factors.
2.1. Study selection and eligibility criteria
First of all, the criteria for considering RCT for this review were as follows: (1) type of participants: patients with a clinical diagnosis of diabetes and cardiovascular diseases. (2) Type of intervention: moderate red wine. (3) Comparison between interventions: body mass index, total cholesterol, blood pressure, HDL and LDL levels. We retrieved studies published from January 1990 to April 2019. We explored the effects of red wine on risk factors for cardiovascular diseases including BMI, BP, total cholesterol, HDL and LDL levels of diabetic who did or did not drink red wine. We initially established the inclusion and exclusion criteria that all the selected studies had to meet. The inclusion criteria were: (1) evaluation of the effects of red wine in patients with any type of diabetes, provided that the control groups did not drink any form of alcohol; (2) adult patients only; (3) any amount of red wine taken with or without food; (4) red wine as the only interventional factor; (5) providing the results of the means and standard deviations (SDs) of BMI, BP, cholesterol, HDL and LDL levels between control and intervention group; and, (6) English-language works only. All other studies were excluded. Letters, correspondence, case reports, and conference abstracts lacking detailed results were also excluded, as were the studies that enrolled pregnant patients.
2.2. Search strategy
Two researchers independently searched PubMed, SpringerLink, Embase, the Cochrane Library, Medline, Orbis, and the Web of Science using the following keywords: (“red”[All Fields] AND (“wine”[MeSH Terms] OR “wine”[All Fields]) AND (“cardiovascular system”[MeSH Terms] OR (“cardiovascular”[All Fields] AND “system”[All Fields]); “red”[All Fields] AND (“wine”[MeSH Terms] OR “wine”[All Fields]) AND (“diabetes mellitus”[MeSH Terms] OR (“diabetes”[All Fields] AND “mellitus”[All Fields]) OR “diabetes mellitus”[All Fields] OR “diabetes”[All Fields] OR “diabetes insipidus”[MeSH Terms] OR (“diabetes”[All Fields] AND “insipidus”[All Fields]) OR “diabetes insipidus” [All Fields]). The reference lists of all the retrieved studies were reviewed.
2.3. Data extraction and quality assessment
Both researchers independently extracted data: first author name, publication date, country of publication, subject details, total number of participants (controls and intervention group), red wine consumption duration, wine intake, means and SDs, and conclusions. Table 1 lists the eligible studies chosen by reviewer consensus. Quality assessment reflected the reviewers’ judgments of random sequence generation, allocation concealment, blinding of participants and personnel, blinding to outcome assessment, incomplete outcome data, and selective reporting as analyzed by Revman ver. 5.0 (; https://community.cochrane.org/help/tools-and-software/revman-5); this free software is used to prepare and update Cochrane reviews.
Table 1. Characteristics of included studies.
| Author, year, country | Subjects | Mean age (control/intervention) | Total number of participants (control/intervention) | Alcohol consumption duration | Control | Types, dosage | Authors’ conclusion |
| J. W. Y. Beulens, et al., 2010, The Netherlands15 | Patients with diabetes mellitus (type 1 and 2) | 59.3/59.2 | 1632 (1100/532) | 6 months | Normal | Red wine, 11–20 glasses per week | Moderate alcohol consumption is not only associated with a reduced risk of vascular but also with reduced risks of CHD |
| R. Marfella, et al., 2006, Italy16 | Patients with type 2 diabetes | 35.1/36.5 | 115 (58/57) | 1 year | Normal | Red wine, with red wine intake of one 118 mL per glass of wine each day | Moderate red wine intake with meals may have a beneficial effect in the prevention of cardiovascular complications in patients with diabetes |
| Rachel Golan, et al., 2017, Israel17 | Patients with type 2 diabetes | 58.9/58.9 | 126 (69/57) | 2 years | Normal | Red wine, average daily consumption 150 mL per glass | Moderate red wine intake was associated with no progression in carotid plaque |
| Mori, et al., 2016, Australia18 | Patients with type 2 diabetes | 59.3/59.3 | 24 (self-controlled trial) | 4 weeks | Normal | Red wine, women drinking 230 mL day–1 (∼24 g alcohol per day) and men drinking 300 mL day–1 (∼31 g alcohol per day) | In patients with type 2 diabetes, 24–31 g alcohol per day raises blood pressure but does not favourably or adversely modify cardiovascular risk factors |
| Yftach Gepner, et al., 2015, Israel8 | Patients with type 2 diabetes | 59.1/59.3 | 156 (83/73) | 2 years | Normal | Red wine, 150 mL at dinnertime | This long-term RCT suggests that initiating moderate red wine among well-controlled diabetes is safe and modestly decreases cardiometabolic risk |
2.4. Statistical analysis
The mean and SD were used as the principal comparators. Revman ver. 5.0 was used to perform the meta-analysis. Statistical heterogeneity was calculated using the I2 test and the extent of inconsistency was assessed using the I2 statistic. In general, an I2 value ≥50% was considered as evidence of heterogeneity and a random-effects model was selected for meta-analysis. An I2 value <50% was considered to indicate low heterogeneity and a fixed-effects model was used. The publication bias of texts reporting positive outcomes was analyzed by drawing funnel plots. A two-tailed p-value <0.05 was considered to reflect statistical significance. Sensitivity analysis featured deletion of individual studies.12–14
3. Results
3.1. Literature search and characteristics of the included studies
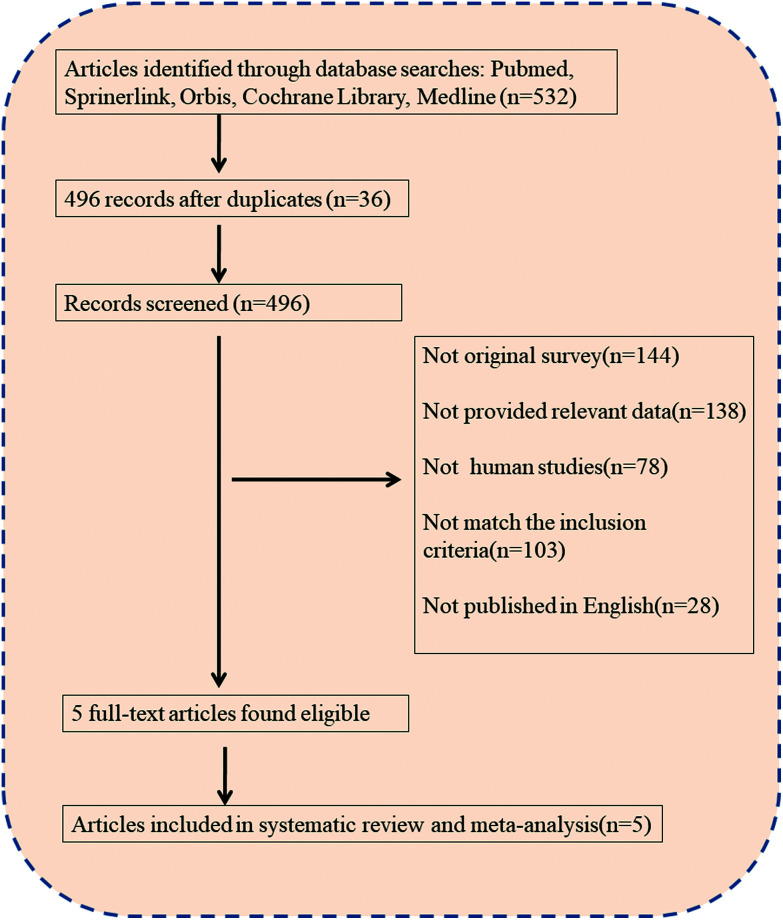
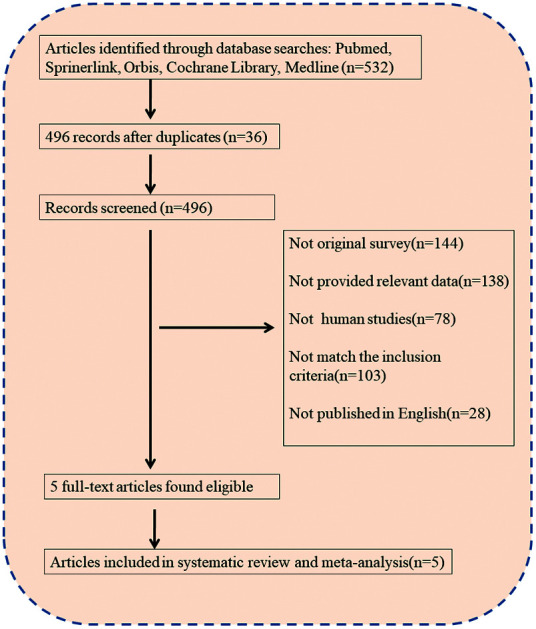
532 texts were initially retrieved by both reviewers; 36 duplicates were removed. Of the remaining 496, 144 did not report relevant work, 138 lacked important data, 78 were not human studies, 103 did not meet our inclusion criteria, and 28 were not published in English. Eventually, five full-text articles fulfilled both the inclusion and exclusion criteria, and were included in meta-analyses.8,15–18 Fig. 1 shows the search process and study exclusions as suggested by the PRISMA search flow.19 All the included studies were RCTs. Table 1 lists the first authors, study years, countries or regions, total numbers of participants (controls and intervention group), alcohol consumption durations, wine doses, and the conclusions. The five studies included a total of 2068 diabetics, some of whom drank red wine. In the work of J. W. Y. et al., 11–20 glasses per week were consumed; Marfella et al. provided red wine at 118 mL day–1. Four of the five studies explored the effect of red wine on the BMI;8,15,17,18 one did not. All five studies measured the effects of wine on the level of total cholesterol (mmol L–1), systolic BP (mmHg), diastolic BP (mmHg), the HDL level (mmol L–1), and the LDL level (mmol L–1).8,15,17,18,20 We did not perform subgroup meta-analysis by wine dose because some authors reported doses in milliliters and others in glasses (Fig. 2).
Fig. 1. PRISMA flow diagram of articles included in the meta-analysis.
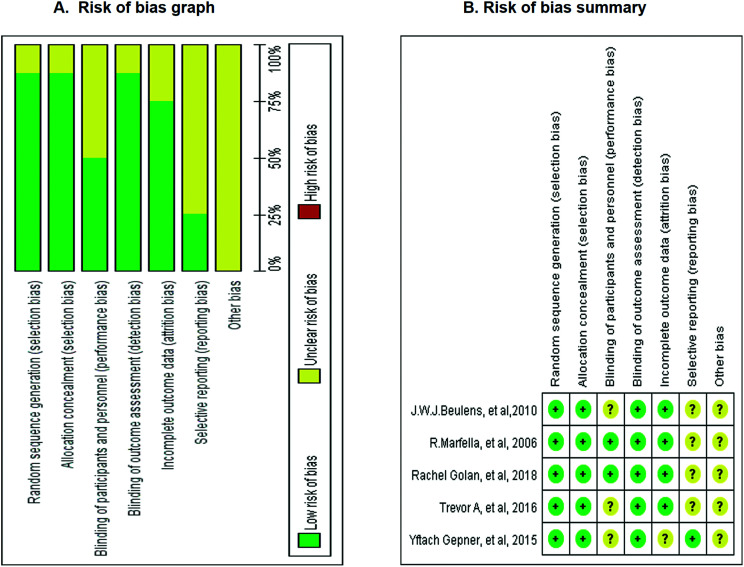
Fig. 2. Analysis the quality of enrolled studies for meta-analysis (A) risk of bias graph, with each risk of bias item presented as a percentage across all the included studies. (B) Risk of bias summary, with each risk of bias item for each included study.
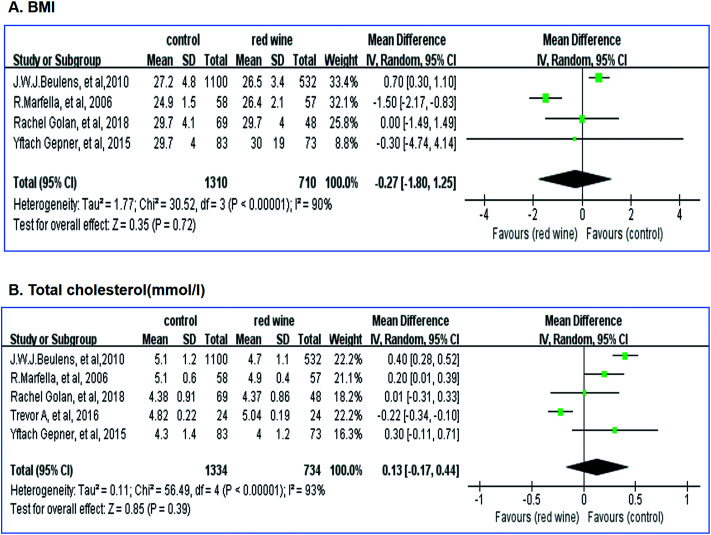
3.2. Effects of red wine on BMI and total cholesterol level
The effects of red wine on the BMI and total cholesterol level were investigated using data from the five studies. Given the significant heterogeneity, a random-effects model was employed. Red wine had no effect on the BMI (MD –0.27, 95% CI –1.80, 1.25; I2 = 90%, Fig. 3A) or the total cholesterol level (MD 0.13, 95% CI –0.17, 0.44; I2 = 93%, Fig. 3B) of diabetics.
Fig. 3. MD scoring with moderate red wine intervention compared to control intervention. (A) MD of BMI with moderate red wine intervention compared to non-red wine intervention group. (B) MD of total cholesterol with moderate red wine intervention compared to non-red wine intervention group.
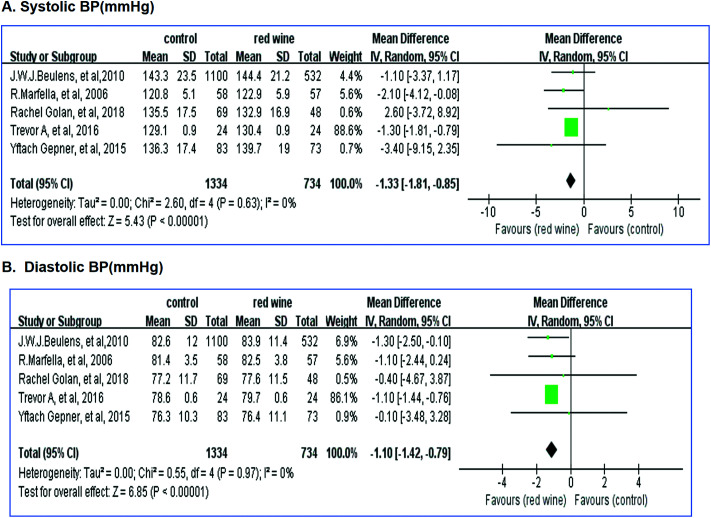
3.3. Effects of red wine on BP
The effects of red wine on BP were investigated using data from the five studies. No significant heterogeneity was apparent. Red wine significantly affected the systolic BP (MD –1.33, 95% CI –1.81, –0.85; I2 = 0%, Fig. 4A) and the diastolic BP (MD –1.31, 95% CI –1.80, –0.83; I2 = 0%, Fig. 4B).
Fig. 4. MD scoring with moderate red wine intervention compared to control intervention. (A) MD of systolic BP with moderate red wine intervention compared to non-red wine intervention group. (B) MD of diastolic BP with moderate red wine intervention compared to non-red wine intervention group.
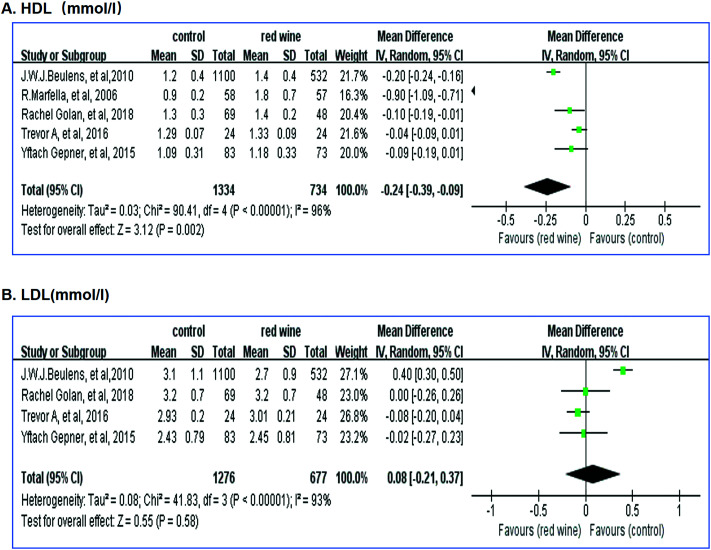
3.4. Effects of red wine on HDL and LDL levels
The effects of red wine on the HDL and LDL levels were investigated using data from the five studies. Given the significant heterogeneity, a random-effects model was employed. Red wine significantly affected the HDL level (MD –0.24, 95% CI –0.39, –0.09; I2 = 96%, Fig. 5A) but not the LDL level (MD 0.08, 95% CI –0.21, 0.37; I2 = 96%, Fig. 5B).
Fig. 5. MD scoring with moderate red wine intervention compared to control intervention. (A) MD of HDL with moderate red wine intervention compared to non-red wine intervention group. (B) MD of diastolic LDL with moderate red wine intervention compared to non-red wine intervention group.
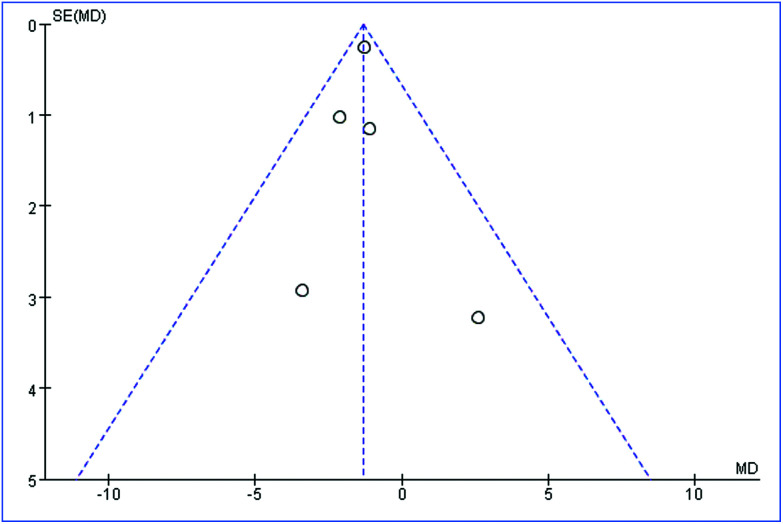
3.5. Publication bias
RevMan software was used to draw funnel plots (Fig. 6); each dot represents data from a single RCT. The funnel plots were rather asymmetrical, indicating potential publication bias because studies with positive outcomes are more likely to be published than are those with negative outcomes.
Fig. 6. Funnel plot: SE by mean difference; each dot represents 1 RCT.
3.6. Sensitivity testing
We excluded all studies individually from the analysis; the results did not change significantly.
4. Discussion
4.1. Primary results from this meta-analysis
We found that diabetics who drink red wine experienced significantly reduced systolic BP (MD –1.33, 95% CI –1.81, –0.85) and diastolic BP (MD –1.31, 95% CI –1.80, –0.83) compared to diabetics who did not drink wine. Compared to the latter patients, the HDL level was significantly higher in those who drink red wine (MD –0.24, 95% CI –0.39, –0.09). However, red wine had no effect on the BMI (MD –0.27, 95% CI –1.80, 1.25), total cholesterol level (MD 0.13, 95% CI –0.17, 0.44), or the LDL level (MD 0.08, 95% CI –0.21, 0.37). Therefore, both overall and in terms of most individual items analyzed, our results are consistent with those of the previous studies showing that red wine reduces some cardiovascular risk factors in diabetics. However, red wine has no effect on other risk factors, including the BMI and the total cholesterol and LDL levels. The reason why red wine affects some risk factors but not others remains unclear and thus, more mechanisms should be investigated.
4.2. Strengths of this meta-analysis
The strengths of our study include the fact that we analyzed RCTs with large numbers of diabetics, we set stringent inclusion criteria, and we evaluated only a few important cardiovascular risk factors. However, our work had several limitations. First, our methods compensated for only some of the limitations in the published works; our results require cautious interpretation. Second, because the red wine intake varied, we could not define any dose–response relationship between wine consumption and reductions in cardiovascular risks. However, our study is the best analysis to date of earlier works on the effects of red wine on cardiovascular risk factors in diabetics. We offer a systematic and detailed assessment of the effects of red wine in diabetics in terms of cardiovascular disease prevention.
4.3. Red wine should be recommended only cautiously to diabetics
Diabetes is characterized by a high incidence of cardiovascular complications such as hypertension. The BMI, BP, the cholesterol, HDL and LDL levels are all cardiovascular risk factors.21–25 Over the past decade, many studies (RCTs or in vitro works) have explored whether alcohol reduces cardiovascular disease in diabetics; the red wine effect has attracted both scientific and public interest. However, recommending red wine to diabetics remains controversial, as red wine contains many bioactive components, including ethanol and resveratrol. Commonly, red wine is 14–18% ethanol by volume and contains about 250–300 mg L–1 gallic acid equivalents (GAE) of total phenols, particularly resveratrol.26 A recent cross-sectional survey indicated that alcohol consumption exhibited various associations; for example, the risk/wine consumption graph was U-shaped for stroke.27 Kang et al. showed, in a diabetic rat model, that low concentrations of ethanol played a cardioprotective role; red wine activated the PI3K pathway and inhibited mitoPTP pore opening.28 Epidemiologically, moderate red wine consumption prevents cardiovascular diseases because of the antioxidant effects of resveratrol.29 However, Mostofsky et al. found that moderate alcohol consumption was associated with an immediately higher cardiovascular risk.30 We suggest that this paradox may reflect the dose consumed. In Mosco, sudden cardiac-related deaths increase dramatically at weekends as alcohol consumption rises.31 In 1996, the World Health Organization stated that, in the West, “alcohol is cardio-protective at all levels of consumption”.31 A population-based case-control study indicated that every 5 g increment of alcohol daily intake was inversely associated with the risk of type 2 diabetes (DMT2).32 Our analysis also suggests that red wine consumption may reduce some cardiovascular risk factors, including BP, and improve the HDL level. However, as diabetics are at higher risk of cardiovascular disease than others and as the drinking pattern/volume may affect cardiac-related outcomes, red wine should be recommended only cautiously to diabetics. Prospective cohort studies are required.
The BMI and the cholesterol and LDL levels of diabetics are associated with cardiovascular disease risks. Diabetics usually develop dysfunctional lipid metabolism; the BMI is linked to changes in serum lipid levels.33 Wakabayashi found that a high BMI attenuated the association between alcohol intake and a lower LDL level.34 Previous studies indicated that light to moderate alcohol consumption may decrease the LDL level35 but the debate continues. We found that red wine did not influence the BMI or the cholesterol or LDL levels. One possible reason is genetics. Corella et al. found that the effect of alcohol intake on the LDL level was modulated in part by variability at the APOE locus.36 Another possible reason is gender. Boivin et al. indicated that in females, an LDL over 1.60 g L–1 was associated with poor BP control after excessive alcohol consumption in comparison to normal consumption but in males, the responsible factor was an HDL over 0.40 g L–1 rather than the LDL level.37 Wakabayashi divided ethanol intake into four levels: very light (<10 g per day), light (≥10 but <20 g per day), moderate (≥20 but <30 g per day), and heavy (≥30 g per day).38 Alcohol elevated BP more in males than in females. Maahs et al. found that females with diabetes mellitus type 1 (DMT1) had lower HDL levels and higher LDL levels than males with DMT1.39 The third possible reason may reflect differences between DMT1 and DMT2. Femlak et al. reported that LDL increased more markedly during DMT2 than during DMT1 progression.40 Also, age, lifestyle, dietary customs, and even environmental pollution41 may change the BMI and the cholesterol and LDL levels. However, no genetic, gender, lifestyle, or dietary data were available; we could not perform subgroup analysis. In addition, we could not test the influence of mean age because in four studies the mean age was about 50 years but it was only about 35 years in the fifth.
We used means with SDs as the principal indicators of the effects of red wine on cardiovascular risks. However, the mean is a measure of the absolute effect size. Of the five eligible studies, the mean accumulated over each period of observation and was thus the most important measure of improved outcomes. However, the relative risk is usually employed to compare the risks of two different groups. In the future, we will compute and publish relative risks.
As the global incidence of diabetes increases, more patients must contend with the consequent risk of cardiovascular disease. Current preventative strategies to reduce the risk of cardiovascular diseases and other complications include limited sugar intake, exercise, BMI control, and regular examinations. However, a much clearer understanding of the benefits and risks of red wine intake by diabetics is essential if preventative strategies are to be effective; the information must be current and readily applicable. The reporting of cardiovascular risk outcomes related to red wine consumption requires improvement. Studies must be scientifically sound, reproducible, generally applicable, and give clinically useful definitions of the conditions undergoing intervention. For example, the red wine doses varied in the works were viewed. This greatly compromised among-study comparisons and the assessment of cardiovascular risks. We recommend that fixed wine doses be employed. Two studies did not distinguish between diabetes types and no study subdivided patients by gender. Hence, future studies should be better organized along these lines.
5. Conclusions
Our meta-analysis supports the suggestion that red wine reduces BP and the HDL level but has no effect on the BMI, or the cholesterol or LDL levels. Future studies should use scientifically sound, reproducible, generally applicable clinical interventions, and carefully evaluate outcomes of interest (such as stroke).
Author contributions
RXH conceived and designed the study; SAN and DCL performed eligibility screening and data extraction; SAN analyzed the data and performed the statistical analysis. DCL drafted the initial manuscript. RXH critically reviewed and revised the manuscript.
Conflicts of interest
The authors declare no conflict of interest.
Sources of Funding
This study is supported by grants from National Natural Science Foundation of China (Grant No. U1803124) and the Natural Science Foundation of Hunan Province (Grant No. 2019JJ40396).
References
- Balakumar P., Maung U. K., Jagadeesh G. Pharmacol. Res. 2016;113(Pt A):600–609. doi: 10.1016/j.phrs.2016.09.040. [DOI] [PubMed] [Google Scholar]
- Ingelfinger J. R., Jarcho J. A. N. Engl. J. Med. 2017;376(15):1473–1474. doi: 10.1056/NEJMe1616575. [DOI] [PubMed] [Google Scholar]
- Stephan L. S., Almeida E. D., Markoski M. M., Garavaglia J., Marcadenti A. Nutrients. 2017;9(11):E1190. doi: 10.3390/nu9111190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diaz-Cruz C., Chua A. S., Malik M. T., Kaplan T., Glanz B. I., Egorova S., Guttmann C. R. G., Bakshi R., Weiner H. L., Healy B. C. Mult. Scler. Relat. Disord. 2017;17:47–53. doi: 10.1016/j.msard.2017.06.011. [DOI] [PubMed] [Google Scholar]
- Martin M. A., Goya L., Ramos S. Food Chem. Toxicol. 2017;109(Pt 1):302–314. doi: 10.1016/j.fct.2017.09.015. [DOI] [PubMed] [Google Scholar]
- Lippi G., Franchini M., Favaloro E. J., Targher G. Semin. Thromb. Hemostasis. 2010;36(1):59–70. doi: 10.1055/s-0030-1248725. [DOI] [PubMed] [Google Scholar]
- Hausenblas H. A., Schoulda J. A., Smoliga J. M. Mol. Nutr. Food Res. 2015;59(1):147–159. doi: 10.1002/mnfr.201400173. [DOI] [PubMed] [Google Scholar]
- Gepner Y., Golan R., Harman-Boehm I., Henkin Y., Schwarzfuchs D., Shelef I., Durst R., Kovsan J., Bolotin A., Leitersdorf E. Ann. Intern. Med. 2015;163(8):569–579. doi: 10.7326/M14-1650. [DOI] [PubMed] [Google Scholar]
- Sharif S., Groenwold R. H., van der Graaf Y., Berkelmans G. F., Cramer M. J., Visseren F. L., Westerink J., S. S. Group Diabetes, Obes. Metab. 2019;21(8):1935–1943. doi: 10.1111/dom.13759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sedlak L., Wojnar W., Zych M., Wygledowska-Promienska D., Mrukwa-Kominek E., Kaczmarczyk-Sedlak I. Nutrients. 2018;10(10):E1423. doi: 10.3390/nu10101423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Markoski M. M., Garavaglia J., Oliveira A., Olivaes J., Marcadenti A. Nutr. Metab. Insights. 2016;9:51–57. doi: 10.4137/NMI.S32909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang R., Zhou Y., Hu S., Ren G., Cui F., Zhou P. K. Front. Neurol. 2019;10:233. doi: 10.3389/fneur.2019.00233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qin J., Ning H., Zhou Y., Hu Y., Yang L., Huang R. Biomed. Pharmacother. 2018;99:363–368. doi: 10.1016/j.biopha.2018.01.037. [DOI] [PubMed] [Google Scholar]
- Huang R., Wang K., Hu J. Nutrients. 2016;8(8):E483. [Google Scholar]
- Beulens J. W., Algra A., Soedamah-Muthu S. S., Visseren F. L., Grobbee D. E., van der Graaf Y., S. S. Group Atherosclerosis. 2010;212(1):281–286. doi: 10.1016/j.atherosclerosis.2010.04.034. [DOI] [PubMed] [Google Scholar]
- Marfella R., Cacciapuoti F., Siniscalchi M., Sasso F. C., Marchese F., Cinone F., Musacchio E., Marfella M. A., Ruggiero L., Chiorazzo G. Diabetic Med. 2006;23(9):974–981. doi: 10.1111/j.1464-5491.2006.01886.x. [DOI] [PubMed] [Google Scholar]
- Golan R., Shai I., Gepner Y., Harman-Boehm I., Schwarzfuchs D., Spence J. D., Parraga G., Buchanan D., Witkow S., Friger M. Eur. J. Clin. Nutr. 2018;72(6):871–878. doi: 10.1038/s41430-018-0091-4. [DOI] [PubMed] [Google Scholar]
- Mori T. A., Burke V., Zilkens R. R., Hodgson J. M., Beilin L. J., Puddey I. B., J. Hypertens., 2016, 343 , 421 –428 , ; discussion 428 . [DOI] [PubMed] [Google Scholar]
- Shamseer L., Moher D., Clarke M., Ghersi D., Liberati A., Petticrew M., Shekelle P., Stewart L. A., P.-P. Group Br. Med. J. 2015;350:g7647. doi: 10.1136/bmj.g7647. [DOI] [PubMed] [Google Scholar]
- Bray F., Ferlay J., Soerjomataram I., Siegel R. L., Torre L. A., Jemal A. CA-Cancer J. Clin. 2018;68(6):394–424. doi: 10.3322/caac.21492. [DOI] [PubMed] [Google Scholar]
- Huang R., Zhou P. Environ. Pollut. 2019;247:64–71. doi: 10.1016/j.envpol.2019.01.014. [DOI] [PubMed] [Google Scholar]
- Huang R., Yu T., Li Y., Hu J. Toxicol. Res. 2018;7(3):415–422. doi: 10.1039/c8tx00031j. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu X. D., Xie D. F., Wang Y. L., Guan H., Huang R. X., Zhou P. K. Int. J. Radiat. Biol. 2019;95(2):144–155. doi: 10.1080/09553002.2019.1539880. [DOI] [PubMed] [Google Scholar]
- Mo L. J., Song M., Huang Q. H., Guan H., Liu X. D., Xie D. F., Huang B., Huang R. X., Zhou P. K. Br. J. Cancer. 2018;119(4):492–502. doi: 10.1038/s41416-018-0192-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou P. K., Huang R. X. Toxicol. Res. 2018;7(6):1008–1011. doi: 10.1039/c8tx00207j. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chiva-Blanch G., Arranz S., Lamuela-Raventos R. M., Estruch R. Alcohol Alcohol. 2013;48(3):270–277. doi: 10.1093/alcalc/agt007. [DOI] [PubMed] [Google Scholar]
- Mukamal K., Lazo M. Br. Med. J. 2017;356.:j1340. doi: 10.1136/bmj.j1340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kang P. F., Wu W. J., Tang Y., Xuan L., Guan S. D., Tang B., Zhang H., Gao Q., Wang H. J. Oxid. Med. Cell. Longevity. 2016;2016:6190504. doi: 10.1155/2016/6190504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xia N., Daiber A., Forstermann U., Li H. Br. J. Pharmacol. 2017;174(12):1633–1646. doi: 10.1111/bph.13492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mostofsky E., Chahal H. S., Mukamal K. J., Rimm E. B., Mittleman M. A. Circulation. 2016;133(10):979–987. doi: 10.1161/CIRCULATIONAHA.115.019743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Britton A., McKee M. J. Epidemiol. Community Health. 2000;54(5):328–332. doi: 10.1136/jech.54.5.328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rasouli B., Andersson T., Carlsson P. O., Dorkhan M., Grill V., Groop L., Martinell M., Tuomi T., Carlsson S. Eur. J. Endocrinol. 2014;171(5):535–543. doi: 10.1530/EJE-14-0403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao Y., Asimi S., Wu K., Zheng J., Li D. Clin. Nutr. 2015;34(4):612–619. doi: 10.1016/j.clnu.2014.06.003. [DOI] [PubMed] [Google Scholar]
- Wakabayashi I. Eur. J. Clin. Invest. 2012;42(2):179–185. doi: 10.1111/j.1365-2362.2011.02568.x. [DOI] [PubMed] [Google Scholar]
- Tabara Y., Arai H., Hirao Y., Takahashi Y., Setoh K., Kawaguchi T., Kosugi S., Ito Y., Nakayama T., Matsuda F. Atherosclerosis. 2017;257:22–28. doi: 10.1016/j.atherosclerosis.2016.12.008. [DOI] [PubMed] [Google Scholar]
- Corella D., Tucker K., Lahoz C., Coltell O., Cupples L. A., Wilson P. W., Schaefer E. J., Ordovas J. M. Am. J. Clin. Nutr. 2001;73(4):736–745. doi: 10.1093/ajcn/73.4.736. [DOI] [PubMed] [Google Scholar]
- Boivin J. M., Koch C., Vigie L., Meppiel L. Ann. Cardiol. Angeiol. 2015;64(3):150–157. doi: 10.1016/j.ancard.2015.04.006. [DOI] [PubMed] [Google Scholar]
- Wakabayashi I. Am. J. Hypertens. 2008;21(12):1310–1317. doi: 10.1038/ajh.2008.299. [DOI] [PubMed] [Google Scholar]
- Maahs D. M., Hokanson J. E., Wang H., Kinney G. L., Snell-Bergeon J. K., East A., Bergman B. C., Schauer I. E., Rewers M., Eckel R. H. Diabetes. 2010;59(7):1771–1779. doi: 10.2337/db09-1626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Femlak M., Gluba-Brzozka A., Cialkowska-Rysz A., Rysz J. Lipids Health Dis. 2017;16(1):207. doi: 10.1186/s12944-017-0594-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yao H., Lv J. Acta Cardiol. Sin. 2017;33(6):637–645. doi: 10.6515/ACS20170518A. [DOI] [PMC free article] [PubMed] [Google Scholar]