Abstract
Background
School closures and other public health responses have decreased the extent that children interact with mandated reporters and other professionals trained to detect child maltreatment.
Objective
To assess associations between the pandemic public health response and the number of allegations of child abuse or neglect.
Methods
This study analyzed monthly data from New York City of the number of child maltreatment allegations, stratified by reporter type (e.g., mandated reporter, education personnel, healthcare personnel), as well as the number of Child Protective Services (CPS) investigations warranting child welfare preventative services. SARIMA models were trained using data from January 2015 to February 2020 to predict expected values for March, April, and May 2020. Observed values were compared against predicted values at an alpha of .05.
Results
Substantially fewer allegations of child maltreatment were reported than expected in March (-28.8 %, deviation: 1848, 95 % CI: [1272, 2423]), April (-51.5 %, deviation: 2976, 95 % CI: [2382, 3570]), and May 2020 (-46.0 %, deviation: 2959, 95 % CI: [2347, 3571]). Significant decreases in child maltreatment reporting were also noted for all reporter subtypes examined for March, April, and May 2020. Fewer CPS investigations warranted preventative services than expected in March 2020 (-43.5 %, deviation: 303, 95 % CI: [132, 475]).
Conclusions
Precipitous drops in child maltreatment reporting and child welfare interventions coincided with social distancing policies designed to mitigate COVID-19 transmission. In light of these findings, educators and healthcare providers must be especially vigilant when engaging online with children and their families for signs of child abuse and/or neglect.
Keywords: Child abuse, Child neglect, Mandated reporter, Coronavirus, COVID-19
1. Introduction
In March 2020, unprecedented physical distancing measures such as school and business closures were introduced nationally to slow the spread of the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). Although these distancing policies helped reduce the morbidity and mortality of the pandemic (Thunström, Newbold, Finnoff, Ashworth, & Shogren, 2020), they have had substantial societal consequences, including the loss of over 20 million jobs in the U.S. (Coibion, Gorodnichenko, & Weber, 2020), the transition of millions of employees to working from home, the closure of stores and restaurants, and, importantly for children and parents, the shutdown of schools and child care programs. School closure has presented additional parenting burdens, and for many caregivers, the challenge of providing continuous care for children while working from home has likely precipitated heightened stress and anxiety (Coyne et al., 2020). For other caregivers, loss of employment or reduced household income has likely similarly impacted mental health (Kawohl & Nordt, 2020). Furthermore, the shutdown of restaurants and bars, in conjunction with overall increases in alcohol consumption, has increased the quantity and frequency of alcohol consumption in the home (Micallef, 2020). These challenges associated with the COVID-19 pandemic response, including unemployment, financial instability, parenting stress, social isolation, poorer mental health, and substance abuse, have previously been identified as risk factors for family violence (Milner, 1994; Moncher, 1995; Rodriguez & Green, 1997). Furthermore, previous research has demonstrated that child abuse tends to increase following national emergencies (Seddighi, Salmani, Javadi, & Seddighi, 2019). This phenomenon as it relates to COVID-19 has been substantiated by reports of elevated numbers of children being admitted to hospitals since March 2020 with injuries related to severe child abuse (Schmidt & Natanson, 2020). These factors collectively have led many researchers to suggest that there has been a heightened threat of child abuse for children across the nation who have been isolated at home with potential perpetrators due to the COVID-19 pandemic (Campbell, 2020; Galea, Merchant, & Lurie, 2020; Holmes et al., 2020).
However, concerns have been raised that many cases of child abuse or neglect have not been identified or reported since professionals trained to identify child maltreatment have had markedly less contact with children due to policies promoting distancing (Rosenthal & Thompson, 2020). The majority of U.S. child maltreatment cases are identified by mandated reporters, with educators representing the largest source of reports (20.5 %), and pediatricians and other healthcare providers also identifying a substantial amount of cases (10.7 %) (New York City Administration for Children’s Services, 2020). However, school shutdowns and transitions to virtual classrooms, as well as the substitution of in-person medical care with telehealth visits, have dramatically decreased direct contact between mandated reporters and children (Wosik et al., 2020).
We hypothesized that, although children may have likely been at an elevated risk of abuse and neglect due to psychosocial and financial stressors caused by the COVID-19 pandemic, there may have been a substantial reduction in the number of reports of suspected child maltreatments. While other researchers have suggested a decrease in child abuse reports (Rosenthal & Thompson, 2020), few studies have used statistical modeling to demonstrate the association between the COVID-19 pandemic response and decreased reporting (Baron, Goldstein, & Wallace, 2020; Cabrera-Hernández & Padilla-Romo, 2020). Furthermore, no studies to date have examined child maltreatment reporting stratified by reporter type, precluding discussion of potential links between specific responses to the pandemic and decreases in reporting by particular subgroups of individuals (e.g., teachers or medical professionals).
In New York City (NYC), the initial epicenter of the COVID-19 outbreak in the United States, officials mandated the closure of public schools by March 16, 2020, and the closure of childcare centers and school-based childcare programs by April 6, 2020 (NYC DOE, 2020). The present study aimed to evaluate to what extent there was a decrease in the number of allegations of child maltreatment by various subgroups of reporters and a decrease in the number of child protective services (CPS) investigations warranting child welfare preventative services in NYC coinciding with the response to SARS-CoV-2 in March, April, and May 2020.
2. Methods
This study analyzed the number of child abuse or neglect allegations received monthly by NYC’s Administration for Children’s Services (2020) from January 2015 to May 2020, stratified by allegation source, to determine whether child maltreatment reporting deviated from typical levels during March, April, and May 2020, the first 3 months of widespread social distancing and school closures in response to the SARS-CoV-2 pandemic in New York. The monthly number of NYC CPS investigations which warranted child welfare preventative services was also examined.
Using data from January 2015 to February 2020, Seasonal Autoregressive Integrated Moving Average (SARIMA) modeling was conducted using R, version 4.0.0 (R Foundation), to compare observed and forecasted numbers of maltreatment allegations and CPS investigations warranting child welfare preventative services for March, April, and May 2020; separate analyses were conducted for reporting subgroups (i.e., all reporters, nonmandated reporters, mandated reporters, and subtypes of mandated reporters such as educators and healthcare professionals). The cyclical pattern of child maltreatment reporting, with reporting decreasing during summer vacations and other periods when children have limited contact with mandated reporters, necessitated SARIMA modeling, which allowed us to account for longitudinal and seasonal trends, as well as autoregressive and moving average components in the data through the selection of SARIMA hyperparameters which best accounted for the trend and seasonal elements of the time series examined.
SARIMA model fitting was performed using the Box-Jenkins methodology (Box, Jenkins, Reinsel, & Ljung, 2015). For each time series examined, first, the stationarity of the time series was evaluated using the augmented Dickey-Fuller test to determine whether the time series had a unit root (Hansen, 1995). For each time series with a unit root, seasonal and/or nonseasonal differencing was applied to the data to obtain stationary time series and to determine the trend difference order and seasonal difference order hyperparameters of the SARIMA model. Subsequently, correlograms and partial correlograms were used to determine the upper bounds of SARIMA hyperparameters (i.e., trend autoregressive order, trend moving average order, seasonal autoregressive order, and seasonal moving average order). For each time series examined, the Akaike information criterion was used to select the most parsimonious SARIMA model from the subset of SARIMA models specified by all possible combinations of hyperparameters within the bounds established by the correlogram and partial correlogram (Akaikei, 1973, 1974). Goodness-of-fit was evaluated for selected models using the Ljung-Box Q-test to confirm that residuals followed white noise processes (Box et al., 2015). Additionally, model residuals and their correlograms and partial correlograms were examined to verify that residuals were homoscedastic and uncorrelated. Once an optimal model was selected for each time series, models were fitted to data spanning from January 2015 to February 2020 and forecasting was conducted to determine expected values for March, April, and May 2020. Two-sided confidence intervals for deviations between the observed and expected numbers of reports and CPS investigations warranting preventative services were calculated at an alpha of .05. This study was exempt from review by the institutional review board of Northwell Health.
3. Data availability
The data that support the findings of this study are available upon request from the New York City Administration for Children’s Services.
4. Results
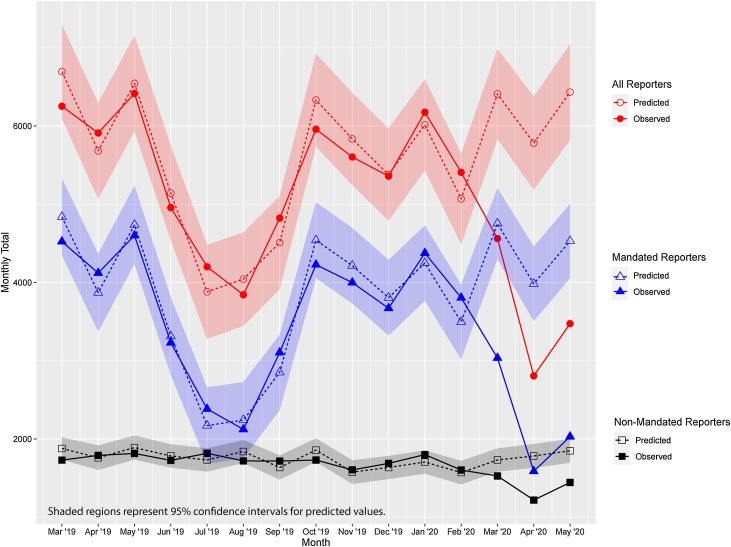
Fewer allegations of child maltreatment were reported in NYC than typically expected in March (-28.8 %, deviation: 1848, 95 % CI: [1272, 2423]), April (-51.5 %, deviation: 2976, 95 % CI: [2382, 3570]), and May 2020 (-46.0 %, deviation: 2959, 95 % CI: [2347, 3571]) (Fig. 1 and Table 1 ). Significant decreases in child maltreatment reporting were noted for all subgroups of interest for March, April, and May 2020 (Table 1). Fewer CPS investigations warranted preventative services than expected in March 2020 (-43.5 %, deviation: 303, 95 % CI: [132, 475]); decreases in the number of investigations warranting preventative services were noted for April 2020 (-29.1 %, deviation: 182, 95 % CI: [-12, 377]) and May 2020 (-23.8 %, deviation: 146, 95 % CI: [-62, 354]), but these decreases were not statistically significant at an alpha of 0.05 (Table 1).
Fig. 1.
Child Maltreatment Allegations in New York City, March 2019 to May 2020. The figure shows observed and predicted values for the number of allegations of child maltreatment reported to the Administration for Children’s Services in New York City from March 2019 to May 2020. Predicted values for March 2019 to February 2020 were derived from SARIMA models trained using data from January 2015 up to, but not including, the month being predicted. Predicted values for March 2020 to May 2020 were derived from SARIMA models trained using data from January 2015 to February 2020. (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article).
Table 1.
Comparison of Observed and Expected Child Abuse/Neglect Reports by Reporter and Child Welfare Prevention Cases for March, April, and May 2020 in New York City.
| Month | Number of Reports |
Expected - Observed (95 % CI) | P value | ||
|---|---|---|---|---|---|
| Observed | Expected | ||||
| All Reporters | March | 4562 | 6410 | 1848 (1272, 2423) | <.001 |
| April | 2806 | 5782 | 2976 (2382, 3570) | <.001 | |
| May | 3474 | 6433 | 2959 (2347, 3571) | <.001 | |
| Nonmandated Reportersa |
March | 1527 | 1731 | 204 (56, 353) | .007 |
| April | 1219 | 1783 | 564 (412, 715) | <.001 | |
| May | 1444 | 1849 | 405 (252, 557) | <.001 | |
| Mandated Reportersb | March | 3035 | 4754 | 1719 (1268, 2171) | <.001 |
| April | 1587 | 3984 | 2397 (1922, 2871) | <.001 | |
| May | 2030 | 4530 | 2500 (2025, 2975) | <.001 | |
| Educational Personnel | March | 1038 | 2003 | 965 (665, 1265) | <.001 |
| April | 357 | 1418 | 1061 (756, 1366) | <.001 | |
| May | 352 | 1815 | 1463 (1153, 1773) | <.001 | |
| Social Service Personnel | March | 822 | 1153 | 331 (189, 473) | <.001 |
| April | 461 | 1073 | 612 (464, 760) | <.001 | |
| May | 631 | 1143 | 512 (358, 667) | <.001 | |
| Law Enforcement Personnel | March | 636 | 756 | 120 (52, 188) | <.001 |
| April | 470 | 807 | 337 (265, 409) | <.001 | |
| May | 642 | 841 | 199 (123, 275) | <.001 | |
| Medical and Mental Health Personnel | March | 466 | 654 | 188 (110, 266) | <.001 |
| April | 254 | 608 | 354 (275, 433) | <.001 | |
| May | 363 | 680 | 317 (237, 397) | <.001 | |
| Child Care Personnel | March | 46 | 77 | 31 (9, 54) | .007 |
| April | 26 | 79 | 53 (31, 76) | <.001 | |
| May | 17 | 77 | 60 (37, 84) | <.001 | |
| Child Welfare Prevention Cases | March | 393 | 696 | 303 (132, 475) | <.001 |
| April | 444 | 626 | 182 (-12, 377) | .07 | |
| May | 467 | 613 | 146 (-62, 354) | .17 | |
Nonmandated reporter group included caregivers, friends/neighbors/other relatives, anonymous reporters, and other unspecified non-mandated reporters.
Mandated reporter subgroup included educational, social service, law enforcement, and medical and mental health personnel. This subgroup additionally included foster parents and other unspecified mandated reporters. Analyses were not performed on the number of reports from these subgroups due to low numbers of reports.
5. Discussion
Based on our analyses, which accounted for both seasonal and longitudinal trends, we found that there were 29 % fewer total reports of child maltreatment in March 2020 than forecasted, and that in April and May 2020, the number of reports was approximately half of what was expected. Notably, the deviations in April and May 2020 were approximately double the magnitude of those in March 2020; this is consistent with the fact that social distancing guidelines and school and business closures were implemented in the middle of March 2020, so the first half of the month likely had typical levels of child maltreatment reporting. These findings, taken together, are concerning and suggest a broader health crisis. In 2018, NYC recorded 67,686 (2.8 %) of the 2,402,827 allegations of child maltreatment reported nationwide (United States Children’s Bureau, 2020). If the 7783 report deficit in NYC for the months of March to May 2020 is extrapolated, we estimate that approximately 276,293 allegations of child maltreatment which would have otherwise been reported nationally in March to May 2020 were not reported. Even though NYC had a higher infection rate than much of the country, we think this estimate is reasonable since the impact of the pandemic on child maltreatment reporting is likely associated with school closures and public policy, rather than the prevalence of the viral infection itself.
According to national data, health care personnel and education personnel are responsible for over a third of suspected child maltreatment reports (New York City Administration for Children’s Services, 2020). In May 2020, the American Academy of Pediatrics (American Academy of Pediatrics News, 2020) reported the results of a survey of over 200 primary care pediatricians assessing the impact of COVID-19 on their practices. The majority of respondents reported more than a 50 % reduction in preventive and sick care visits as a result of the COVID-19 pandemic response. Although many medical practices and schools have transitioned to telehealth visits and online learning, respectively, these virtual formats do not lend themselves readily to the identification of child maltreatment because children and caregivers may not feel comfortable sharing sensitive information, and there is limited opportunity for direct observation of children. Additionally, privacy limitations may preclude children from sharing confidential or embarrassing information, especially if there is a risk that their abuser may overhear them (Humphreys, Myint, & Zeanah, 2020). The reduced contact between children and both health care providers and educators during the initial months of the COVID-19 pandemic is consistent with our findings, which demonstrated substantial deviations in the number of child maltreatment allegations by health care and education personnel in March, April, and May 2020. Given that many schools face uncertainty regarding in-person instruction during the 2020–2021 school year and that many physicians may continue to conduct patient visits virtually to reduce the likelihood of spreading COVID-19 among patients and office staff, we anticipate that child maltreatment will continue to be grossly underreported and hundreds of thousands of suspected child maltreatment cases may be missed nationally due to restricted contact between children and professionals who are trained to recognize and obligated to report suspected child abuse and neglect.
Although it is possible that our findings can be partially explained by a decrease in child abuse due to shelter-in-place policies that have limited the exposure of children to non-family members, the overwhelming majority of child maltreatment perpetrators are parents of their victims (New York City Administration for Children’s Services, 2020), so this explanation is unlikely to be the basis for our findings. To the contrary, it is probable that our predicted deviation in the number of suspected child maltreatment reports is an underestimate of the actual number since the psychological and socioeconomic consequences of the COVID-19 pandemic have likely resulted in an increased incidence of child abuse and neglect (Humphreys et al., 2020). Research has shown that the risk factors for child maltreatment, as well as child maltreatment itself, often increase following disasters (Seddighi et al., 2019). A recent systematic review suggested that this association is due to the heightened psychological, social, and economic pressures faced by family members during disasters and conflicts (Seddighi et al., 2019). Furthermore, social isolation and lack of access to support networks have also been identified previously as risk factors for instances of child abuse (Moncher, 1995). Given that unprecedented levels of economic hardship and social isolation were necessary, albeit unintended, consequences of sustained social distancing policies, the response to the COVID-19 pandemic has likely elevated the risk of child abuse and neglect on a national scale.
Moreover, alternative methods of tracking child abuse provide evidence of a surge in the actual prevalence of abuse during the COVID-19 pandemic. The Childhelp National Child Abuse Hotline, which often receives reports from victims of child abuse rather than from mandated reporters, experienced a 31 % increase in the number of reports received in March 2020 (Schmidt & Natanson, 2020). Furthermore, hospitals such as Cook Children’s Medical Center in Texas and Children’s National Hospital in Washington D.C. have reported a spike in the number of children admitted with life-threatening injuries from familial violence (Schmidt & Natanson, 2020). This pattern was similarly noted in a study on the prevalence of severe child abuse following Hurricane Floyd, which used medical records of inflicted traumatic brain injury rather than social service records to quantify child abuse, demonstrating that child abuse increased in the wake of the hurricane (Keenan, Marshall, Nocera, & Runyan, 2004).
Although studies have examined the extent to which child maltreatment increases during past emergencies, the duration and scope of the broad and sustained school closures caused by COVID-19 pandemic responses have been unprecedented, making it difficult to estimate the extent to which child maltreatment has increased. In terms of school closures, the most similar experience in U.S. history was the closure of schools following Hurricane Katrina (Kamenetz, 2020), which damaged or destroyed approximately 700 schools and initially dislocated 372,000 students (Singleton, 2008). However, in the case of Hurricane Katrina, many students were relocated to other schools in surrounding communities or nearby states, whereas this was not possible for students affected by COVID-19-related public health measures.
Our study has several notable strengths. Importantly, our SARIMA models account for longitudinal and seasonal trends, as well as autoregressive and moving average components, of measures of interest using data spanning the past five years, thus improving our ability to detect real deviations from typical values. Furthermore, while other regional studies have similarly found decreases in child maltreatment reporting during the COVID-19 pandemic (Baron et al., 2020; Cabrera-Hernández & Padilla-Romo, 2020), this is the first study to date to analyze child maltreatment reporting stratified by reporter type and profession. This approach allowed us to identify decreases in child maltreatment reporting across all subgroups of interest, indicating that previously noted decreases in child maltreatment reporting are likely attributable to many factors. The fact that reporting by nonmandated reporters and mandated reporters both decreased suggests that extended family, friends, and neighbors (i.e., nonmandated reporters) have not been an adequate safety net for identifying cases of child maltreatment which had typically been identified by health care professionals, educators, and other mandated reporters in the past.
However, our study must also be interpreted in the context of its limitations. Most notably, only data from March, April, and May 2020 were available for examining deviations associated with the implementation of social distancing public policies. Additionally, due to the structure of the publicly available monthly data used in our analyses, we were unable to examine whether the prevalence of specific types of maltreatment allegations (e.g., physical abuse, lack of medical care, and educational neglect) made by subgroups of reporters differed from typical levels. Also, since we used estimates from NYC to approximate the national impact of COVID-19 on child maltreatment reports, regional variability in the timing and extent of social distancing (Institute for Health Metrics & Evaluation, 2020) and other pandemic responses may have compromised the accuracy of our extrapolation. Another important consideration is that our study likely underestimates the extent of underreporting of child maltreatment since the incidence of child maltreatment has likely increased beyond typical levels during the pandemic. Therefore, our study could only comment on the extent to which child maltreatment reporting was lower in March to May 2020 than we would have expected to see if pre-COVID-19 trends in child maltreatment reporting had continued through the spring. Through other analytic methods, such as SARIMAX or polynomial regression modeling, it may be possible to account for some of the increase in child maltreatment associated with factors such as widespread unemployment. However, due to the unprecedented effect that the pandemic has had on these factors, analyses using models which include exogenous measures may be limited in their ability to make meaningful predictions since forecasting would be predicated on extrapolation (rather than interpolation) of associations noted in the data used for model fitting because, in many cases, the observed levels of exogenous measures during the pandemic will be outside the range of values observed in the training data.
Even though the present study demonstrated drastic disparities between expected and observed numbers of child maltreatment reports for March, April, and May 2020, it is too early to adequately predict the long-term impact of COVID-19 on child maltreatment reporting or the need for child welfare preventative services. Some regions started loosening social distancing restrictions as of June 2020 (Tolbert, Kates, & Levitt, 2020), which may have increased contact between children and trained professionals, potentially improving reporting of child abuse and neglect. In these areas, reporting of child maltreatment may rebound. Of note, our findings suggest that the number of CPS investigations warranting child welfare preventative services may have started to return to typical levels as of May 2020. As additional data are made available for both NYC and other regions, continued monitoring of child maltreatment reporting and child welfare preventative services will be essential for properly quantifying and understanding the scope of the public health concerns identified in this study.
In the meantime, there needs to be greater awareness of the potential for child maltreatment to go unreported. Educators, the single most common source of child maltreatment reports, must continue to be vigilant for signs of child abuse or neglect, even when using virtual platforms to engage with children. The Maine Department of Education (2020) issued guidance for educators on recognizing signs that may suggest child abuse or neglect when engaging with children virtually. In addition to looking for marks of abuse during virtual contact, their guidance includes monitoring video chats for background noises such as yelling, which may be indicative of household tension, regularly engaging with children and their caregivers, and ensuring that children and their family members have the ability to have private conversations with the educator.
For health care providers, Humphreys et al. (2020) provides a list of recommendations to identify child maltreatment during virtual patient visits. In addition to looking for signs of parental stress, irritability, and depression, Humphreys suggests that clinicians specifically ask about stress levels in the home and coping strategies, as well as inquiring about substance use. Moreover, clinicians should be attentive for children who appear overly fearful and parents who are unduly harsh or over-controlling. Clinicians should also be mindful of known risk factors for child maltreatment, such as financial hardship, which may be exacerbated by the social distancing policies and economic uncertainties created by the COVID-19 pandemic. In addition to these suggestions, Humphreys provides clinicians with specific recommendations for parents to help mitigate parenting stress. Although many families have been reluctant to bring their children to doctors’ offices due to fears of COVID-19 transmission, the American Academy of Pediatrics (2020a) recommends that “all well-child care should occur in person whenever possible.” Office-based visits not only provide clinicians with the unique opportunity to do a thorough physical examination, but they also provide better opportunities to meaningfully engage with families and have private conversations about sensitive topics with children and caregivers as needed. For these reasons, pediatricians should advise parents to schedule in-person well-child visits when possible and appropriate.
Additionally, for families struggling with the mental health consequences of the COVID-19 pandemic response, pediatricians and other child care professionals should encourage virtual engagement with friends and family to combat loneliness, maintenance of daily routines for work, rest, exercise, and meals, and the utilization of mental health services as needed (Rosenthal & Thompson, 2020). Given the increased strain that the pandemic has placed on households, mental health professionals and pediatricians should promote strategies for maintaining strong child-parent relationships, including encouraging parents to answer questions about the pandemic honestly, recognize their child’s feelings, and use rewards and privileges to reinforce good behavior (American Academy of Pediatrics, 2020b). Furthermore, child care professionals should refer struggling parents to resources available online through a joint initiative by various organizations, including the World Health Organization, UNICEF, and the Global Partnership to End Violence Against Children (Cluver et al., 2020).
6. Conclusion
The COVID-19 pandemic is unprecedented in terms of scope and impact. It has been estimated that policies promoting social distancing, including the closure of schools and daycares, have saved over 1 million lives in the U.S (Thunström et al., 2020). Even though these policies have been essential from a public health perspective, several researchers have expressed concerns that an unintended consequence of social distancing policies may be an increase in the incidence of undetected and unreported child maltreatment (Campbell, 2020; Humphreys et al., 2020). Our findings demonstrate a marked decrease in child maltreatment reporting and provision of CPS interventions in NYC during the COVID-19 pandemic; if reflective of national trends, our study suggests that, nationally, over a quarter million cases of child abuse or neglect may have gone unreported as a result of the pandemic.
Given that many families may endure great economic hardships in the months ahead, and given that material hardship and infrequent employment have been shown to be associated with increased child maltreatment (Slack, Holl, McDaniel, Yoo, & Bolger, 2004), mandated and nonmandated reporters should exercise heightened vigilance for signs of child abuse and neglect as social contact with children resumes in the coming months. Additionally, prolonged school closures and physical distancing measures decrease the quality and duration of contact that children are having with mandated reporters, thereby increasing the importance of vigilance for signs of child maltreatment by family members, neighbors, and other nonmandated reporters. Until schools reopen and society returns to typical levels of social engagement, health care providers, educators, and other trained professionals must adapt to the unique challenges posed by virtual contact with children and their families to adequately detect signs of child maltreatment.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Declaration of Competing Interest
The authors report no declarations of interest.
Acknowledgement
The authors would like to thank Sarah A. Keim, PhD, MA, MS at Nationwide Children’s Hospital for her insightful comments and constructive suggestions regarding this manuscript.
References
- Akaike H. A new look at the statistical model identification. IEEE Transactions on Automatic Control. 1974;19(6):716–723. [Google Scholar]
- Akaikei H. Information theory and an extension of maximum likelihood principle. Proc. 2nd Int. Symp. on Information Theory. 1973:267–281. [Google Scholar]
- American Academy of Pediatrics. (2020a, May 8). Guidance on Providing Pediatric Well-Care During COVID-19. https://services.aap.org/en/pages/2019-novel-coronavirus-covid-19-infections/clinical-guidance/guidance-on-providing-pediatric-well-care-during-covid-19/.
- American Academy of Pediatrics. (2020b, June 24). Parenting in a Pandemic: Tips to Keep the Calm at Home. Retrieved August 31, 2020 from https://www.healthychildren.org/English/health-issues/conditions/COVID-19/Pages/Parenting-in-a-Pandemic.aspx.
- American Academy of Pediatrics News. (2020, May 21). Survey: Pandemic disrupting practices, finances of early, midcareer pediatricians. https://www.aappublications.org/news/2020/05/21/research052120.
- Baron E.J., Goldstein E.G., Wallace C.T. 2020. Suffering in silence: How COVID-19 school closures inhibit the reporting of child maltreatment. Available at SSRN 3601399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Box G.E., Jenkins G.M., Reinsel G.C., Ljung G.M. Vol. 5. John Wiley & Sons; 2015. pp. 177–354. (Time series analysis: Forecasting and control). [Google Scholar]
- Cabrera-Hernández F., Padilla-Romo M. 2020. Hidden violence: How COVID-19 school closures reduced the reporting of child maltreatment. Working paper No. 2020-02. Available at https://ideas.repec.org/p/ten/wpaper/2020-02.html. [Google Scholar]
- Campbell A.M. An increasing risk of family violence during the Covid-19 pandemic: Strengthening community collaborations to save lives. Forensic Science International: Reports. 2020 doi: 10.1016/j.fsir.2020.100089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cluver L., Lachman J.M., Sherr L., Wessels I., Krug E., Rakotomalala S.…Butchart A. Parenting in a time of COVID-19. Lancet. 2020;395:e64. doi: 10.1016/S0140-6736(20)30736-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coibion O., Gorodnichenko Y., Weber M. National Bureau of Economic Research; 2020. Labor markets during the covid-19 crisis: A preliminary view (No. w27017) [Google Scholar]
- Coyne L.W., Gould E.R., Grimaldi M., Wilson K.G., Baffuto G., Biglan A. First things first: Parent psychological flexibility and self-compassion during COVID-19. Behavior Analysis in Practice. 2020;1 doi: 10.1007/s40617-020-00435-w. [published online ahead of print May 6, 2020] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galea S., Merchant R.M., Lurie N. The mental health consequences of COVID-19 and physical distancing: The need for prevention and early intervention. JAMA Internal Medicine. 2020;180(6):817–818. doi: 10.1001/jamainternmed.2020.1562. [DOI] [PubMed] [Google Scholar]
- Hansen B.E. Rethinking the univariate approach to unit root testing: Using covariates to increase power. Econometric Theory. 1995:1148–1171. [Google Scholar]
- Holmes E.A., O’Connor R.C., Perry V.H., Tracey I., Wessely S., Arseneault L.…Ford T. Multidisciplinary research priorities for the COVID-19 pandemic: A call for action for mental health science. The Lancet Psychiatry. 2020;7(6):547–560. doi: 10.1016/S2215-0366(20)30168-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Humphreys K.L., Myint M.T., Zeanah C.H. Increased risk for family violence during the COVID-19 pandemic. Pediatrics. 2020;145(4) doi: 10.1542/peds.2020-0982. [DOI] [PubMed] [Google Scholar]
- Institute for Health Metrics and Evaluation. Covid-19 Projections: Social distancing. Updated June 10, 2020. Retrieved June 11, 2020 from https://covid19.healthdata.org/united-states-of-america.
- Kamenetz, A. (2020, April 2). 9 out of 10 children are out of school worldwide. What now. National Public Radio. https://www.npr.org/2020/04/02/824964864/nine-out-of-10-of-the-world-s-children-are-out-of-school-what-now.
- Kawohl W., Nordt C. COVID-19, unemployment, and suicide. The Lancet Psychiatry. 2020;7(5):389–390. doi: 10.1016/S2215-0366(20)30141-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keenan H.T., Marshall S.W., Nocera M.A., Runyan D.K. Increased incidence of inflicted traumatic brain injury in children after a natural disaster. American Journal of Preventive Medicine. 2004;26(3):189–193. doi: 10.1016/j.amepre.2003.10.023. [DOI] [PubMed] [Google Scholar]
- Maine Department of Education. (2020, April 15). Spotting Signs of Child Abuse and Neglect During the COVID-19 Emergency: An updated guide for educational professionals and others who care for Maine children. https://mainedoenews.net/2020/04/15/priority-notice-spotting-signs-of-child-abuse-and-neglect-during-the-covid-19-emergency-an-updated-guide-for-educational-professionals-and-others-who-care-for-maine-children/.
- Micallef, J. (2020, April 4). How the COVID-19 Pandemic is Upending the Alcoholic Beverage Industry. Forbes. https://www.forbes.com/sites/joemicallef/2020/04/04/how-the-covid-19-pandemic-is-upending-the-alcoholic-beverage-industry/#1109a0204b0b.
- Milner J.S. Assessing physical child abuse risk: The child abuse potential inventory. Clinical Psychology Review. 1994;14(6):547–583. [Google Scholar]
- Moncher F.J. Social isolation and child-abuse risk. Families in society. 1995;76(7):421–433. [Google Scholar]
- New York City Administration for Children’s Services. (2020, June). Monthly Indicator Flash Report. Retrieved June 25, 2020 from https://www1.nyc.gov/site/acs/about/flashindicators.page.
- New York City Department of Education. (2020, April 3). Learn at Home for All Students. Retrieved June 11, 2020 from https://www.schools.nyc.gov/alerts/nyc-public-schools-will-close-starting-monday-march-16-2020.
- Rodriguez C.M., Green A.J. Parenting stress and anger expression as predictors of child abuse potential. Child Abuse & Neglect. 1997;21(4):367–377. doi: 10.1016/s0145-2134(96)00177-9. [DOI] [PubMed] [Google Scholar]
- Rosenthal C.M., Thompson L.A. Child Abuse Awareness Month during the coronavirus disease 2019 pandemic. JAMA Pediatrics. 2020 doi: 10.1001/jamapediatrics.2020.1459. [DOI] [PubMed] [Google Scholar]
- Schmidt, S., & Natanson, H. (2020, April 30). With kids stuck at home, ER doctors see more severe cases of child abuse. Washington Post. https://www.washingtonpost.com/education/2020/04/30/child-abuse-reports-coronavirus/.
- Seddighi H., Salmani I., Javadi M.H., Seddighi S. Child abuse in natural disasters and conflicts: A systematic review. Trauma, Violence & Abuse. 2019 doi: 10.1177/1524838019835973. [DOI] [PubMed] [Google Scholar]
- Singleton D.M., editor. The aftermath of Hurricane Katrina: Educating traumatized children pre-k through college. University Press of America; 2008. [Google Scholar]
- Slack K.S., Holl J.L., McDaniel M., Yoo J., Bolger K. Understanding the risks of child neglect: An exploration of poverty and parenting characteristics. Child Maltreatment. 2004;9(4):395–408. doi: 10.1177/1077559504269193. [DOI] [PubMed] [Google Scholar]
- Thunström L., Newbold S.C., Finnoff D., Ashworth M., Shogren J.F. The benefits and costs of using social distancing to flatten the curve for COVID-19. [published online ahead of print April 28, 2020] Journal of Benefit-cost Analysis. 2020:1–27. [Google Scholar]
- Tolbert, J., Kates, J., & Levitt, L. (2020, May 4). Lifting Social Distancing Measures in America: State Actions and Metrics. Kaiser Family Foundation. Retrieved June 11, 2020 from https://www.kff.org/coronavirus-policy-watch/lifting-social-distancing-measures-in-america-state-actions-metrics/.
- United States Children’s Bureau . United States Children’s Bureau; 2020. Child Maltreatment 2018.https://www.acf.hhs.gov/sites/default/files/cb/cm2018.pdf [Google Scholar]
- Wosik J., Fudim M., Cameron B., Gellad Z.F., Cho A., Phinney D., Katz J.N. Telehealth transformation: COVID-19 and the rise of virtual care. Journal of the American Medical Informatics Association. 2020;27(6):957–962. doi: 10.1093/jamia/ocaa067. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available upon request from the New York City Administration for Children’s Services.