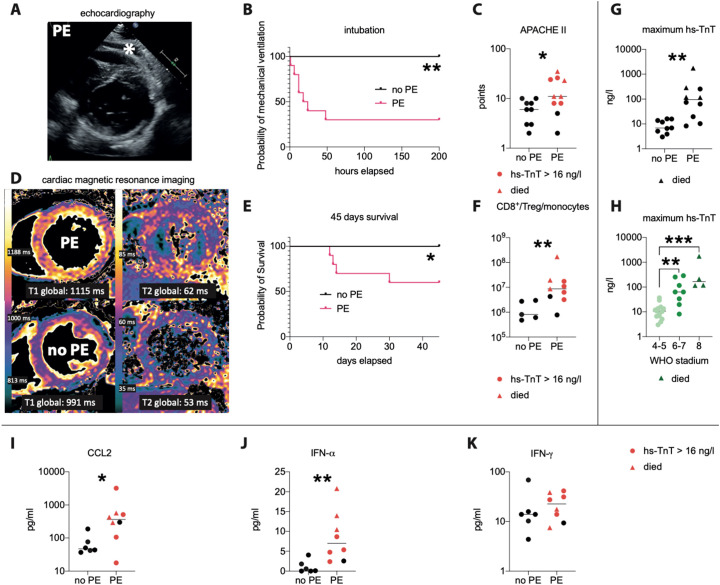
Fig. 1.
PE, hs-TnT and the CD8/Treg/monocyte quotient predict heart injury and clinical course of COVID-19 patients.
(A): representative transthoracic echocardiography (TTE) image, asterisk indicates pericardial effusion. (B): necessity for intubation, (C) APACHE II-score. (D): Representative cardiac magnetic resonance images from a patient with (upper row) and without PE (lower row), showing a diffuse inflammatory pattern with increased markers of edema (T1 and T2 relaxation times) only in PE patients. (E) Survival of COVID-19 patients with or without pericardial effusion (PE) at admission, showing that a PE predicts poorer prognosis. (F): ratio between CD8+ T cells to Tregs and CD14+ HLA-DR+ monocytes, as a parameter for disease severity, which was higher in patients with PE, especially in those who subsequently developed a hs-TnT rise (red symbols) and those who died (red triangles). (G): hs-TnT correlates with PE and with disease severity indicated by (H) the new WHO COVID-19 classification. (I–K): Serum concentrations of the antiviral cytokines CCL2 (I), IFN-α (J) and IFN-γ (K) in patients exhibiting a pericardial effusion (PE) or not (no PE). Subsequent hs-TnT rise (red symbols), deceased (red triangle). Data is presented as scatter plot with median (line). p < 0.05 was considered statistically significant (*). **, p < 0.01; ***, p < 0.001. (For interpretation of the references to color in this figure legend, the reader is referred to the web version of this article.)