Abstract
Stakeholders have implemented a multitude of system-level policies to address the U.S. opioid overdose epidemic. Because the crisis was fueled by opioid prescribing and prescribing of medications for opioid addiction treatment is a key prevention strategy, it is critical to understand prescriber perceptions of policies in these domains. This article reviews prescriber awareness and opinions of the following system-level policies: opioid prescribing guidelines, prescription drug monitoring programs (PDMPs), medications for addiction treatment, and naloxone distribution programs. Most providers are aware of these policies, especially PDMPs, albeit a smaller proportion actively participate in their implementation. Low engagement in certain system-level policies is concerning and deserves attention, given that prescribers play an integral role in achieving optimal impact and mitigating the crisis.
Keywords: opioid prescribing, system-level, policy, provider, perceptions, awareness
Introduction
Prescribers experienced significant pressure starting in the 1990s to adequately manage patient pain and prescribe opioids, closely followed by increases in prescription opioid supply (through 2010) and opioid-related overdose deaths [1]. Although synthetic opioids—mostly illicitly-sourced fentanyl and heroin—now dominate opioid-related overdose deaths, prescription opioids still account for a significant number of deaths per year (almost 15,000 in 2017) [2]. Moreover, prescription opioids remain a source of initial opioid exposure for many who go on to misuse opioids [3].
Today’s ever-evolving drug epidemic has spurred a multitude of policies responsive to its causes and cures. A growing body of evidence that evaluates opioid prescriber-related policies for intended effects finds some to decrease the number and dosage of opioid prescriptions, increase addiction treatment, and even prevent overdose [4–9]. Unintended consequences of opioid harm prevention policies on prescriber behavior (e.g., ceasing to prescribe), patient behavior (e.g., doctor and/or pharmacy shopping, diversion, substituting to illicit substances), and health harms (e.g., overdose by illicit opioids), among other life outcomes, are under active investigation.
Given certain origins of this epidemic in opioid prescribing and the importance of medications for opioid addiction treatment as a prevention strategy, prescriber perceptions of system-level opioid prescribing and addiction treatment policies are important to understand but were little-studied until recently. Many of these policies rely on prescriber behavior change to achieve impact, thus rendering prescriber perceptions critical mediators to understanding policy effects. This article seeks to provide a comprehensive review of current studies probing providers’ knowledge, attitudes, and opinions of system-level opioid prescribing and addiction treatment policies to offer insights into potential mechanisms of policy effects and avenues for future study.
Scope of System-Level Opioid Prescribing and Addiction Treatment Policies
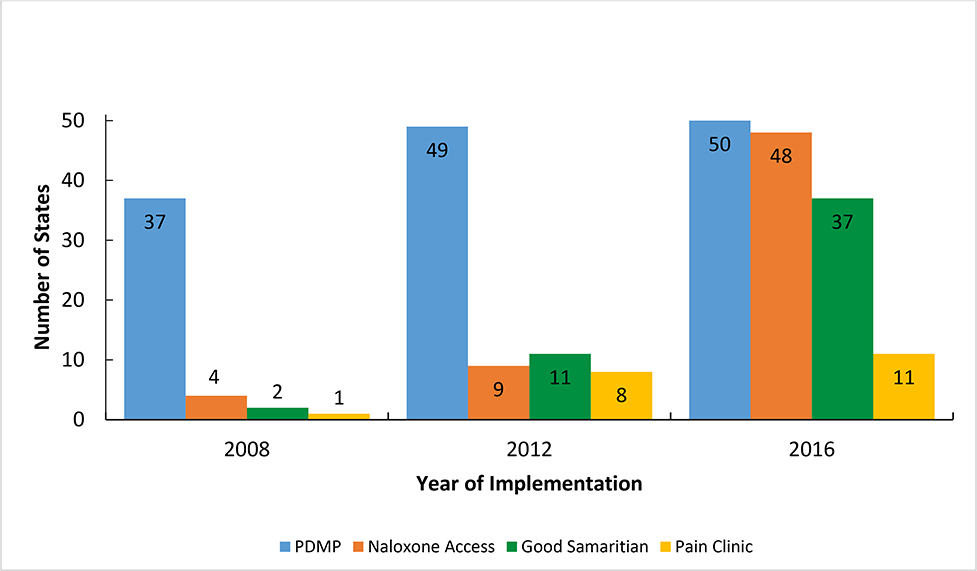
Opioid prescribing and addiction treatment policies implemented in the United States on a system-wide level—that is, large and systemic in nature—are the focus of this review. Prominent national policies have included prescription opioid reformulations (e.g., Oxycontin), rescheduling of prescription opioids (i.e., hydrocodone), and the Centers for Disease Control Guidelines for Prescribing Opioids for Chronic Pain [10]. State-level policies have been numerous and span the prevention continuum from upstream prescribing (e.g., prescribing guidelines and limits, prescription drug monitoring programs (PDMPs), pain clinic regulation) to minimizing harms for persons with opioid addiction (e.g., naloxone access policies, Good Samaritan laws, medications for opioid addiction treatment) [11]. Figure 1 shows the change in state-level adoption of four prominent such state laws from 2008–2016, to demonstrate the rapid adoption of policies at this level. Providers and payers, as well, have actively implemented their own interventions—such as pain contracts, prescribing policies, screening tools, and audit programs.
Figure 1. State Implementation of Select System-Level Opioid Prescribing and Addiction Treatment Policies, 2008–2016.
Notes: PDMP, prescription drug monitoring program. All policies indicate state law implementation in relevant domain. Number of states includes the District of Columbia. Data source: Prescription Drug Abuse Policy System, 2018, pdaps.org.
Guided by available evidence, as further elaborated below in Methods, we evaluated provider (meaning individual practitioner, typically prescriber) perceptions of the following system-level opioid prescribing and addiction treatment policies in this review:
Opioid prescribing guidelines
For the purposes of this review, opioid prescribing guidelines fall into one of three categories: 1) dosage guidelines, 2) risk mitigation strategies, and 3) intervention-related guidelines. Dosage guidelines of focus include CDC Guidelines for Prescribing Opioids for Chronic Pain [9] (hereinafter, the “CDC Guidelines”), state-specific [12,13] or system-specific (e.g., Veteran’s Affairs [14]) guidelines that detail dosage, length of prescription, and other recommendations related to the prescribing of opioid analgesics for the management of chronic, non-cancer pain. Risk mitigation strategies concern the Food and Drug Administration’s (FDA) Risk Evaluation and Mitigation Strategy (REMS) guidelines [15] and the American Pain Society’s Guidelines [16], which both focus on reducing risks related to opioid prescriptions and opioid use disorder (OUD). Lastly, intervention-related guidelines cover the Substance Abuse and Mental Health Services Administration (SAMHSA) guidelines for screening, brief intervention, and referral to treatment (SBIRT) that focus on appropriate intervention for patients with OUD [17].
Prescription drug monitoring programs
PDMPs are state-level electronic databases that track opioid prescriptions and related information within a specific state. Data are increasingly shared between states and available to a variety of prescribers, pharmacists and other professionals, such as law enforcement officers. States typically recommend and, in some cases, mandate that providers register with and/or check their state’s PDMP when prescribing opioids for pain management [18,19].
Medications for opioid addiction treatment
Medications to treat opioid addiction include three evidence-based FDA-approved medications shown to reduce opioid overdose and related harms [20]. Often these medications are accompanied by behavioral therapies or counseling to treat the whole-patient. Relatively recently, opioid addiction treatment provision shifted from the predominantly the domain of specialists (often directly supervising and administering methadone treatment) to expand into non-specialty, office-based settings that facilitate take-home medication (namely, buprenorphine and naltrexone) [20]. In line with this secular shift, policies around buprenorphine and naltrexone medications to treat opioid addiction constitute the focus of this review.
Naloxone access and distribution programs
Naloxone-hydrochloride (i.e., naloxone) is an opioid antagonist that can be administered intravenously, injected into a muscle, or sprayed into the nose; it counters the effects of an opioid overdose. Naloxone access and distribution programs occur at many levels (e.g., clinical, emergency response, law enforcement, lay person) and provide naloxone and related education to patients and others to utilize the medication in the case of opioid overdose [21]. We focus on naloxone access and distribution programs at the clinical level in this review.
Methods
We generated the following concept blocks to identify studies focused on provider perceptions of system-level opioid prescribing and addiction treatment policies: physicians, opioids, guidelines/policies, dosage, PDMP, attitudes/beliefs/knowledge, tamper-resistant formulas, hydrocodone rescheduling, medications to treat opioid addiction/OUD, and naloxone. Using Medline, we searched the aforementioned concept blocks in multiple permutations and combinations. Prior knowledge and bibliography searches were also performed. These searches resulted in an initial compilation of articles.
Within the initial set of articles, we focused on those that covered physician or prescriber attitudes, beliefs, knowledge, and/or opinions of opioid prescribing or addiction treatment policies at system-wide levels. We did not restrict the search by prescriber or physician type, research methodology, or geographic location within the United States.
We excluded the following literature from our review: purely evaluative articles of opioid-related policies (lacking any measurement of provider perceptions); articles without a larger, systematic focus; and articles published prior to 2010. We designated the year 2010 as a cutoff date for article inclusion because our target literature was scant before this period and because many target policies went into effect and started to enter prescribers’ consciousness around this time. A total of 51 articles were selected for this review, 18 of which we annotated as of special interest (9) or outstanding interest (9). We organize our discussion of the literature by policy type: opioid prescribing guidelines, PDMPs, medications for opioid addiction treatment, and naloxone access and distribution programs. We analyzed each article for provider attitudes, knowledge, beliefs, opinions, awareness and/or behavior changes related to the respective policy.
Results
Our results, organized by system-level policy type, are summarized in Table 1 and explained in greater detail below.
Table 1.
Summary of Provider Perceptions of System-Level Opioid Prescribing and Addiction Treatment Policies.
| Findings | Evidence | |
|---|---|---|
| Opioid Prescribing Guidelines | ||
| General Guidelines | • Often local (practice-based) guidelines superseded government guidelines | • Kilaru et al., 2014 |
| Dosage | • Physicians were more aware than other prescribers of state guidelines • Most physicians (67%) were aware of CDC Guidelines • Awareness of guidelines was associated with confidence in prescribing • Providers with higher number of CME hours had higher knowledge and utilization of CDC guidelines |
• Franklin, 2013 • Ebbert, 2017 • McCalmont et al., 2018 |
| Risk Mitigation | • Majority of surveyed prescribers were unaware of REMS guidelines • 50% of physicians surveyed were unwilling to perform mandatory education requirements for REMS • Primary care physicians only partially compliant with American Pain Association Guidelines |
• Salinas, Robinson & Abdolrasulnia, 2012 • Slevin & Ashburn, 2011 • Khalid et al., 2015 |
| Intervention-focused | • Only 27.7% of surveyed primary care physicians knew of SBIRT • Prescribers had mixed feelings on elements of SBIRT: some found urine screening useful and identifying high risk patients, others felt urine screening did not facilitate trust with patients |
• Harris & Yu, 2016 • Barry et al., 2010; Krebs et al., 2014 |
| Prescription Drug Monitoring Programs | ||
| PDMPs | • Awareness of PDMPs across medical specialties is high, between 70–90% • Prescribers did not register for PDMP largely because of registration difficulties • States with PDMP use mandates experienced higher prescribers registration • Prescribers who use PDMP report increased awareness of prescribing behaviors and prescribe fewer and smaller doses of opioids |
• Blum, Nelson & Hoffman, 2016; Kohlbeck et al., 2018; Hwang et al., 2016; Irvine et al., 2014; Perrone, DeRoos & Nelson, 2012; Rutkow et al., 2015 • Blum, Nelson & Hoffman, 2016; Feldman et al., 2011; Fleming et al., 2014; Kohlbeck et al., 2018; Perrone, DeRoos & Nelson, 2012 • Williams et al., 2018 • Lin et al., 2017; Martello et al., 2018; McAllister et al., 2015; Pomerleau, Schrager & Morgan, 2016 |
| Medications for Opioid Addiction Treatment | ||
| Buprenorphine | • Majority of providers support buprenorphine as an effective medication to treat OUD, but only 25% felt confident they could actually prescribe buprenorphine • Federal regulations (buprenorphine cap and waiver) as well as prior authorization requirements proved quite cumbersome for providers in prescribing buprenorphine |
• DeFlavio et al., 2015 • Andraka-Christou & Capone, 2018; DeFlavio et al., 2015; Hutchinson et al., 2014; Kermack et al., 2017 |
| Naltrexone | • Little is known about prescriber opinions of naltrexone as it is a fairly new drug • Barriers regarding insurer reimbursement policies (prior authorization, fail-first therapies) are a concern |
• Andraka-Christou & Capone, 2018 |
| Naloxone Access and Distribution Programs | ||
| Naloxone | • Providers had overwhelming support for naloxone distribution programs at the clinical level • Gaps in knowledge about how to effectively prescribe naloxone and identify patients in need explain the few providers who participate in naloxone distribution |
• Behar et al., 2018; Okoro et al., 2018; Peckham et al., 2018; Wilson et al., 2016 • Behar et al., 2018; Wilson et al., 2016 |
Opioid Prescribing Guidelines
Dosage
Awareness of state opioid prescribing guidelines, specifically those implemented in Washington state in 2007, was higher among physicians than among advanced practice nurse practitioners; however, this awareness increased over time for all prescribers surveyed [12]. A high proportion of physicians have awareness of the CDC guidelines (67%) [22]. Those aware of the CDC Guidelines were also more confident in treating patients with chronic, non-cancer pain [23]. Furthermore, increasing continuing medical education (CME) hours is associated with increasing awareness and use of CDC guidelines [24].
Risk mitigation
The majority of physicians surveyed were not aware of REMS recommendations [25]. Only 50% of surveyed physicians were willing to complete education requirements associated with REMS [24]. Primary care physicians were only partially compliant with American Pain Society Guidelines, based on review of their prescribing in electronic medical records [16]. While residents and attending physicians had similar rates of entering into opioid agreements with patients (42.4% and 45.1%, respectively), less than half of physicians were compliant with the terms [16]. Residents also managed more patients at high risk of substance misuse than attendings and their patients had more frequent early refills [16].
Intervention-related recommendations
Most physicians surveyed (family practitioners, internists, and primary care physicians) highly support clinical interventions to reduce prescription opioid misuse—namely the use of patient contracts (98%) and urine drug testing (90%) [26]. However, surveyed providers in New York State were generally unaware that SBIRT encompasses these interventions, with only 27.7% reporting awareness of SBIRT recommendations [27]. Some providers implemented SBIRT related techniques, even if they reported unawareness of SBIRT recommendations. For example, 57% screened patients for substance use, 46% provided brief intervention, and 47% referred patients to treatment [27]. Some office-based physicians considered patient agreements and urine testing to be helpful in identifying at-risk patients [28], while others perceived urine screening practices as too “policing”. One provider claimed: “I think [drug screening is] destructive to a basic patient-doctor relationship. You’re there to help them and they can tell you their deepest, darkest secrets, but yet you’re policing them,” [29].
General guidelines
Often, policies implemented at the provider level—by healthcare systems, hospitals, clinics—have superceded national and state guidelines [30]. In some cases, guidelines are implemented as communication tools instead of as dosage and/or intervention recommendations [30]. Some emergency departments have deliberately not complied with opioid prescribing guidelines in order to expedite patient discharge and increase patient satisfaction [31].
PDMPs
Overall awareness of PDMPs, across medical specialties is fairly high, ranging from 72% to 90% of surveyed providers [25,32–36]. Despite these high awareness levels, many physicians did not register with PDMPs due to an inability to access the PDMP or difficulties with registration and login [32–38]. Higher program registration was associated with state mandated PDMP checks [39]. Emergency medicine and primary care physicians registered with and utilized PDMPs most frequently, along with providers specializing in pain and addiction treatment [34]. Across surgical residency programs, the vast majority of surgical residents (94.5%) were allowed to prescribe opioids even though their program directors lacked knowledge about the existence of a PDMP 26.4% of the time, along with lacking information about other state controlled substance education and licensure requirements [40].
Prescribers exhibit mixed opinions regarding PDMP effectiveness and usefulness. Providers who utilized PDMPs found the information to be very helpful [41–43]. However, just over 40% of users of New York’s mandated PDMP, I-STOP, found the program unhelpful or very unhelpful [34]. Beyond general opinion about the utility of PDMP information, many providers report that utilization of these programs made them more aware of their prescribing practices, helped with prescribing decisions, and decreased length and dosage of opioids prescribed [43–48]. PDMPs were used most often when providers were prescribing opioids to a patient for the first time, when drug abuse was suspected, to guide decision-making, or when mandated by the state [41,49–51]. Persistent barriers associated with PDMP utilization included the time associated with obtaining the data, poor integration with electronic health records, and the need for interoperability with other PDMPs and real-time data [36,37,52].
Medications for Opioid Addiction Treatment
Buprenorphine
Despite overall positive perceptions of buprenorphine as an effective medication to treat opioid addiction and OUD across studies, the proportion of family physicians who felt they could effectively prescribe buprenorphine was only around 25% [53]. Providers who prescribed lower dosages than recommended of buprenorphine often also held the strong beliefs about the spiritual or moral basis of addiction [54]. Providers deemed certain policies, including the need for prior authorization and waivers to prescribe buprenorphine, to be major barriers to provision of this type of medication to treat OUD [55–57]. Providers also commonly perceived that the federal patient cap associated with buprenorphine waivers was too low and that remuneration for obtaining buprenorphine authorization waivers and providing buprenorphine services was inadequate [53,58]. Buprenorphine prescribers working in states supportive of Medicaid expansion had more positive perceptions of the Affordable Care Act’s impact on substance use disorder treatment, compared to prescribers working in states that did not expand Medicaid [59].
Naltrexone
Because naltrexone is a relatively new medication to treat OUD, many providers’ perceptions of policies surrounding its provision were not yet well known. However, similar to buprenorphine, providers were concerned with the insurer prior authorization requirements and fail-first therapy requirements, including those imposed by federal payers, associated with naltrexone [55].
Naloxone Access and Distribution Programs
Overall, providers across different specialties overwhelmingly supported naloxone access and distribution programs [60–64]. Some of this support derived from the personal responsibility providers feel to address opioid overdoses, especially if they are prescribing opioids for chronic pain [65]. Despite this support, few providers actually prescribed naloxone regularly [64]. The discrepancy between support and practice was largely attributable to gaps in knowledge regarding naloxone prescribing, inability to identify patients at risk for overdose, and fear of consequences related to its prescribing [61,64]. Where naloxone prescribing did occur, it was found to be positively associated with comfort and knowledge around such prescribing and awareness of naloxone-related state legislation [62,63]. Certain providers, including psychiatrists and substance use disorder treatment specialists, exhibited greater comfort in prescribing naloxone [63]. Naloxone education programs have increased provider knowledge and confidence in naloxone prescribing [65].
Discussion
Over time, general prescriber knowledge and awareness of the opioid crisis and related policies has increased due to national publicity—such as the Surgeon Generals’ distribution of CDC Guideline pocket cards and naloxone access campaigns. Also, the Trump Administration’s declaration of the opioid crisis as a public health emergency and the passage of the SUPPORT for Patients and Communities Act (“SUPPORT Act”) further highlighted this crisis as a national priority. Increasing secular awareness of the drug epidemic holds the promise of increasing prescriber compliance with policy. This review revealed that a majority of providers studied were aware of many policies covered—namely PDMPs, state and federal opioid prescribing guidelines, and buprenorphine policies. Still, there were some policies with which providers had less familiarity (e.g., intervention-focused guidelines, REMS, and naltrexone and surrounding policies, and naloxone distribution programs). Persistent lack of awareness is somewhat concerning, as prescribers are integral actors through which these policies and guidelines are implemented in medical settings.
Provider perceptions of system-level opioid prescribing and addiction treatment policies discussed in this review suggest many opportunities for improvements to achieve policy impact. Across all policies covered, providers voiced a real need for education to increase their competency and, in some cases, knowledge, around these policies. Prescribers also proposed several policy-specific improvements, particularly in relation to PDMPs and medications for opioid addiction treatment. For example, providers expressed the desire for interoperability between PDMPs and with existing electronic health records, and that PDMPs include timely data [41,52]. Cumbersome federal and insurer policies, such as the need for a waiver and the inadequate and burdensome reimbursement for opioid addiction treatment, were serious barriers to effective treatment provision. Providers called for intensive review and revision of these elements of treatment policy at the federal level [53,57]. The Comprehensive Addiction and Recovery Act (CARA) and the SUPPORT for Patients and Communities Act that expand buprenorphine waivers to physician assistants and nurse practitioners, as well as increase the number of patients physicians are able to treat with buprenorphine waivers, are steps in the right direction. These national policies deserve future study to assess whether they actually change prescriber attitudes and behavior.
While the 22% decrease in opioid prescriptions between 2013 and 2017 [67] supports the idea that awareness and compliance with opioid prescribing guidelines and PDMP utilization has indeed increased, this by no means suggests that the opioid crisis is surmounted. With fentanyl and other illicit opioids fueling more and more deaths and opioid-related harms, new policies are needed that involve additional stakeholders, such as law enforcement and communities. As the population with OUD continues to grow, prescribers must play an increasing role in treating opioid addiction with medications and in contributing to robust naloxone provision.
At the same time, while opioid prescribing laws remain an important tool in policymaking and can help avoid initial exposure or over-exposure to opioids (particularly if opioids are not appropriately indicated for the type of pain a patient is experiencing), their potential harms deserve attention. Unintended consequences of PDMPs and guidelines must be carefully evaluated. Moreover, studies of provider perceptions of opioid policies not covered in this review due to a dearth of analyses—including federal rescheduling of opioids, more provider-level opioid policies, state pain clinic laws, and newer laws that limit prescription opioid supply (in terms of days or dosages)—deserve additional attention. Provider perceptions and behavior changes in response to these system-level interventions will be very telling as to whether aspects of these policies have swung the pendulum too far in the direction of restricting access to prescription opioids for certain patients.
Acknowledgements
Both authors contributed to the intellectual content of the paper, in the form of conception, design, and drafting. Both authors had full access to the literature reviewed in the study and take responsibility for the accuracy of the content. Ms. French generated the first draft of the manuscript. Both authors participated in the critical revision of the manuscript for important intellectual content. We thank Matthew Myers, M.P.H., of the Centers for Disease Control and Prevention Injury Prevention Center and the Emergency Medicine Department at the University of Michigan Medical School for assistance in generating Figure 1, based on policy coding conducted by Dr. Haffajee.
Funding: Dr. Haffajee’s work on this article was supported by a Walter J. McNerney Research Award, the National Center for Advancing Translational Sciences of the National Institutes of Health (grant #KL2TR002241), and the Centers for Disease Control and Prevention for the University of Michigan Injury Prevention Center (grant #3R49CE002099–05S1).
Footnotes
Conflict of interest statement: None of the authors has relevant financial interests or relationships with entities in the bio-medical arena that could be perceived to influence, or that give the appearance of potentially influencing, this submitted work.
Contributor Information
Rebecca L. Haffajee, Department of Health Management and Policy, University of Michigan School of Public Health, Ann Arbor, MI
Cecelia A. French, Department of Health Behavior and Health Education, University of Michigan School of Public Health, Ann Arbor, MI
References and Recommended Reading
Papers of particular interest, published within the period of review, have been highlighted as:
* of special interest
** of outstanding interest
- 1.National Institute on Drug Abuse, (2018a): Opioid Overdose Crisis. Retrieved November 18, 2018 from: https://www.drugabuse.gov/drugs-abuse/opioids/opioid-overdose-crisis
- 2.Hedegaard H, Miniño AM, Warner M: Drug overdose deaths in the United States, 1999–2017. NCHS Data Brief 2018, 329:1–8. Retrieved December 3, 2018 from: https://www.cdc.gov/nchs/products/databriefs/db329.htm [PubMed] [Google Scholar]
- 3.National Institute on Drug Abuse, (2018b): Prescription Opioids and Heroin. Retrieved November 26, 2018 from: https://www.drugabuse.gov/publications/research-reports/relationship-between-prescription-drug-heroin-abuse/prescription-opioid-use-risk-factor-heroin-use
- 4.Finley EP, Garcia A, Rosen K, McGeary D, Pugh MJ, Potter JS: Evaluating the impact of prescription drug monitoring program implementation: A scoping review. BMC Health Serv Res 2017, 17(1):1–8. 10.1186/s12913-017-2354-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lewis DA, Park JN, Vail L, Sine M, Welsh C, Sherman SG: Evaluation of the overdose education and naloxone distribution program of the Baltimore Student Harm Reduction Coalition. Am J Pub Health 2016, 106(7):1243–1246. 10.2105/AJPH.2016.303141 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pauly JB, Vartan CM, Brooks AT: Implementation and evaluation of an opioid overdose education and naloxone distribution (OEND) program at a Veterans Affairs Medical Center. Subst Abuse 2018, 7077:1–17. 10.1080/08897077.2018.1449174 [DOI] [PubMed] [Google Scholar]
- 7.Piper TM, Stancliff S, Rudenstine S, Sherman S, Nandi V, Clear A, Galea S: Evaluation of a naloxone distribution and administration program in New York City. Subst Use & Misuse 2008, 43(7):858–870. 10.1080/10826080701801261 [DOI] [PubMed] [Google Scholar]
- 8.Thomas CP, Fullerton CA, Kim M, Montejano L, Lyman DR, Dougherty RH, Daniels AS, Ghose SS, Delphin-Rittmon ME: Medication-assisted treatment with buprenorphine: assessing the evidence. Psych Serv 2014, 65(2):158–170. 10.1176/appi.ps.201300256 [DOI] [PubMed] [Google Scholar]
- 9.Haffajee RL, Mello MM, Zhang F, Zaslavsky AM, Larochelle MR, Wharam JF. Four states with robust prescription drug monitoring programs reduced opioid dosages. Health Aff 2018, 37(6):964–974. 10.1377/hlthaff.2017.1321 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Centers for Disease Control and Prevention. (2018) Guideline for Prescribing Opioids for Chronic Pain. Retrieved November 12, 2018 from: https://www.cdc.gov/drugoverdose/pdf/Guidelines_Factsheet-a.pdf
- 11.Haegerich TM, Paulozzi LJ, Manns BJ, Jones CM: What we know, and don’t know, about the impact of state policy and systems-level interventions on prescription drug overdose. Drug Alcohol Depend 2014, 145:34–47. 10.1016/j.drugalcdep.2014.10.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Franklin GM, Fulton-Kehoe D, Turner JA, Sullivan MD, Wickizer TM: Changes in opioid prescribing for chronic pain in Washington State. J Am Board Fam Med 2013, 26(4):394–400. 10.3122/jabfm.2013.04.120274 [DOI] [PubMed] [Google Scholar]
- 13.Morse J, Stockbridge H, Egan K, Mai J, Wickizer T, Franklin G: Primary care survey of the value and effectiveness of the Washington State opioid dosing guideline. J Opioid Manag 2011, 7(6):427–433. 10.5055/jom.2011.0083 [DOI] [PubMed] [Google Scholar]
- 14.Morasco BJ, Duckart JP, Dobscha SK: Adherence to clinical guidelines for opioid therapy for chronic pain in patients with substance use disorder. J Gen Intern Med 2011, 26(9):965–971. 10.1007/s11606-011-1734-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Food and Drug Administration. (2018). Risk Evaluation and Mitigation Strategies (REMS). Retrieved November 18, 2018 from: https://www.fda.gov/Drugs/DrugSafety/REMS/default.htm
- 16.Khalid L, Liebschutz JM, Xuan Z., Dossabhoy S, Kim Y, Crooks D, Shanahan C, Lange A, Heymann O, Lasser KE: Adherence to prescription opioid monitoring guidelines among residents and attending physicians in the primary care setting. Pain Med 2015, 16(3):480–487. 10.1111/pme.12602 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Substance Abuse and Mental Health Services Administration. (2018). Screening, Brief Intervention, and Referral to Treatment. Retrieved November 18, 2018 from: https://www.samhsa.gov/sbirt
- 18.Haffajee RL, Jena AB, Weiner SG: Mandatory use of prescription drug monitoring programs. JAMA 2015, 313(9):891–892. 10.1001/jama.2014.18514 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Davis CS, Johnston JE, Pierce MW: Overdose epidemic, prescription monitoring programs, and public health: A review of state laws. American Journal of Public Health 2015, 105(11), e9–e11. 10.2105/AJPH.2015.302856 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Schuckit MA: Treatment of opioid-use disorders. New Eng J Med 2016, 375(4):357–368. 10.1056/NEJMra1604339 [DOI] [PubMed] [Google Scholar]
- 21.Kerensky T, Walley AY: Opioid overdose prevention and naloxone rescue kits: what we know and what we don’t know. Addiction Sci & Clin Pract 2017, 12(1):4 10.1186/s13722-016-0068-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ebbert JO, Philpot LM, Clements CM, Lovely JK, Nicholson WT, Jenkins SM, Lamer TJ, Gazelka HM: Attitudes, beliefs, practices, and concerns among clinicians prescribing opioids in a large academic institution. Pain Med 2018, 19(9):1790–1798. 10.1093/pm/pnx140 Authors find that 67% of surveyed providers were aware of CDC prescribing guidelines, 55% were registered for the state PDMP, and 2% always or frequently co-prescribed naloxone with opioids.** Of particular importance, the authors find that providers who were aware of a patient that overdosed were 31% more likely to be enrolled in the PDMP and express concern with patient addiction.
- 23.McCalmont JC, Jones KD, Bennett RM, Friend R: Does familiarity with CDC guidelines, continuing education, and provider characteristics influence adherence to chronic pain management practices and opioid prescribing? J Opioid Manag 2018, 14(2):103–116. 10.5055/jom.2018.0437** Using a web-based survey, this article demonstrates that more hours of continuing medical education (CME) training hours is positively associated with correct use of CDC opioid prescribing guidelines, comfort with opioid prescribing, and confidence in pain management. This relationship held true when controlling for provider profession (physician vs. nurse practitioner) and geographic setting (rural vs. urban); however, physicians reported being more confident in opioid dose conversions as compared to nurse practitioners.
- 24.Salinas GD, Robinson CO, Abdolrasulnia M: Primary care physician attitudes and perceptions of the impact of FDA-proposed REMS policy on prescription of extended-release and long-acting opioids. J Pain Res 2012, 5:363–369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Slevin KA, Ashburn MA: Primary care physician opinion survey on FDA opioid Risk Evaluation and Mitigation Strategies. J Opioid Manag 2011, 7(2):109–115. 10.5055/jom.2011.0053 [DOI] [PubMed] [Google Scholar]
- 26.Hwang CS, Turner LW, Kruszewski SP, Kolodny A, Alexander GC: Primary care physicians’ knowledge and attitudes regarding prescription opioid abuse and diversion. Clin J Pain 2016, 32(4):279–284. 10.1097/AJP.0000000000000268 [DOI] [PubMed] [Google Scholar]
- 27.Harris BR, Yu J: Attitudes, perceptions and practice of alcohol and drug screening, brief intervention and referral to treatment: a case study of New York State primary care physicians and non-physician providers. Pub Health 2016, 139:70–78. 10.1016/j.puhe.2016.05.007 [DOI] [PubMed] [Google Scholar]
- 28.Barry DT, Irwin KS, Jones ES, Becker WC, Tetrault JM, Sullivan LE, Hansen H, O’Connor PG, Schottenfeld RS, Fiellin DA: Opioids, chronic pain, and addiction in primary care. J Pain 2010, 11(12):1442–1450. 10.1016/j.jpain.2010.04.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Krebs EE, Bergman AA, Coffing JM, Campbell SR, Frankel RM, Matthias MS: Barriers to guideline-concordant opioid management in primary care—A qualitative study. J Pain 2014, 15(11):1148–1155. 10.1016/j.jpain.2014.08.006 [DOI] [PubMed] [Google Scholar]
- 30.Kilaru AS, Gadsden SM, Perrone J, Paciotti B, Barg FK, Meisel ZF: How do physicians adopt and apply opioid prescription guidelines in the emergency department? A qualitative study. Ann Emerg Med 2014, 64(5):482–489. 10.1021/nl061786n.Core-Shell [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Pomerleau AC, Nelson LS, Hoppe JA, Salzman M, Weiss PS, Perrone J. The impact of prescription drug monitoring programs and prescribing guidelines on emergency department opioid prescribing: a multi-center survey. Pain Med 2017, 18(5):889–897. 10.1093/pm/pnw032** Using a web-based survey, the authors illuminate that of emergency department (ED) physicians, 59% were aware of PDMPs and 40% reference opioid prescribing guidelines when prescribing to patients. Of particular concern were ED physicians that were unaware of prescribing guidelines (35%), prescribed opioid analgesics to expedite patient discharge (16%), and prescribed opioids to increase patient satisfaction (12%).
- 32.Kohlbeck S, Akert B, Pace C, Zosel A: A multistep approach to address clinician knowledge, attitudes, and behavior around opioid prescribing. WMJ : Offic Pub State Med Society Wisconsin 2018, 117(1):38–41. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/29677414* After implementation of HOPE legislation and related educational modules in Wisconsin, physicians demonstrated statistically significant improvements in accessing the state PDMP, comfort-level in using the PDMP, understanding of an upcoming PDMP use mandate, and beliefs that checking the PDMP is important to effective patient care and public health. This study provides evidence that educational modules can improve use of PDMP and prescribing practices of Wisconsin physicians – an intervention that could be scaled up to impact opioid prescribing on a larger scale.
- 33.Blum CJ, Nelson LS, Hoffman RS: A survey of physicians’ perspectives on the New York State mandatory prescription monitoring program (ISTOP). J Subst Abuse Treatment 2016, 70:35–43. 10.1016/j.jsat.2016.07.013 [DOI] [PubMed] [Google Scholar]
- 34.Irvine JM, Hallvik SE, Hildebran C, Marino M, Beran T, Deyo RA: Who uses a prescription drug monitoring program and how? insights from a statewide survey of Oregon clinicians. J Pain 2014, 15(7):747–755. 10.1016/j.jpain.2014.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Perrone J, DeRoos FJ, Nelson LS: Prescribing practices, knowledge, and use of prescription drug monitoring programs (PDMP) by a national sample of medical toxicologists, 2012. J Med Toxicol 2012, 8(4):341–352. 10.1007/s13181-012-0250-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Rutkow L, Turner L, Lucas E, Hwang C, Alexander G: Most primary care physicians are aware of prescription drug monitoring programs, but many find the data difficult to access. Health Aff 2015, 34(3):484–492. 10.1377/hlthaff.2014.1085**The majority of surveyed primary care physicians in a nationally representative sample report awareness (72%) and use (53%), on at least one occasion, of PDMPs. Given the non-routine and somewhat sporadic use of PDMPs, the authors suggest the following to increase the number of providers regularly using PDMPs: educational measures, state mandates, and enhanced ease of access.
- 37.Feldman L, Williams KS, Coates J, Knox M: Awareness and utilization of a prescription monitoring program among physicians. J Pain & Palliat Care Pharmacother 2011, 25(4):313–317. 10.3109/15360288.2011.606292 [DOI] [PubMed] [Google Scholar]
- 38.Fleming ML, Hatfield MD, Wattana MK, Todd KHL: Exploratory study of emergency physicians’ use of a prescription monitoring program using a framework of technology acceptance. J Pain & Palliat Care Pharmacother 2014, 28(1):19–27. 10.3109/15360288.2013.879242 [DOI] [PubMed] [Google Scholar]
- 39.Williams KS, Magalotti S, Schrouder K, Knox M, Feldman L, Ujwal D, Lynch D: Prescription drug monitoring programs: relationships among program awareness, use, and state mandates. J Pain & Palliat Care Pharmacother 2018:1–5. 10.1080/15360288.2018.1488793** Through self-report surveys, the authors find that states that have mandated PDMP checks, such as Ohio, have higher reported physician use of these programs compared to states that do not have PDMP mandates, such as North Carolina. Despite the similar awareness of PDMPs across states, this article provides evidence that state mandates could increase use of PDMPs.
- 40.Yorkgitis BK, Raygor D, Bryant E, Brat G, Smink DS, Crandall M: Surgery program directors’ knowledge of opioid prescribing regulations: a survey study. J Surg Res 2018, 227:194–197. 10.1016/j.jss.2018.02.036* The vast majority (94.5%) of surgical residency program directors allow residents to prescribe opioid analgesics, despite some surgical program director lack of knowledge about controlled substances regulations. For example, 20% of program directors were unsure if their state required opioid prescribing education for licensure (when it did), 26.4% were uncertain if a state PDMP existed (when it did), and 9.1% did not know if their state required additional registration to prescribe controlled substances (when it did). This gap between knowledge and practice among surgical training directors is of concern and suggests the need for increased education of these providers regarding opioid regulations.
- 41.Freeman PR, Curran GM, Drummond KL, Martin BC, Teeter BS, Bradley K, Schoenberg N, Edlund M: Utilization of prescription drug monitoring programs for prescribing and dispensing decisions: results from a multi-site qualitative study. Res Social & Admin Pharm 2018: 10.1016/J.SAPHARM.2018.09.007*Qualitative interviews illuminate how primary care providers use PDMPs when making opioid prescribing decisions. State mandates seem to improve the use of these programs. However, more seamless integration of patient history with PDMP data would further aid in use and decision-making surrounding opioid prescribing.
- 42.Gershman JA, Gershman JA, Fass AD, Popovici I: Evaluation of Florida physicians’ knowledge and attitudes toward accessing the state prescription drug monitoring program as a prescribing tool. Pain Med 2014, 15(12):2013–2019. 10.1111/pme.12476 [DOI] [PubMed] [Google Scholar]
- 43.Lin DH, Lucas E, Murimi IB, Jackson K, Baier M, Frattaroli S, Gielen AC, Moyo P, Simoni-Wastila L, Alexander GC: Physician attitudes and experiences with Maryland’s prescription drug monitoring program (PDMP). Addiction 2017, 112(2):311–319. 10.1111/add.13620**The majority of physicians that use PDMPs in Maryland report that its utilization helps them to improve opioid prescribing through decreasing the amount of opioids prescriber and increasing comfort level. This study also highlights barriers to PDMP use: lack of knowledge about the program, trouble with registering, and data access issues.
- 44.Martello J, Cassidy B, Mitchell A: Evaluating emergency department opioid prescribing behaviors after education about mandated use of the Pennsylvania prescription drug monitoring program. J Addiction Nurs 2018, 29(3):196–202. 10.1097/JAN.0000000000000236*This study illuminates the need for education surrounding mandated PDMPs. Educational measures regarding the nature of the opioid epidemic and use of PDMPs helped to increase knowledge and use of monitoring programs, improve prescribing practices, and address barriers.
- 45.McAllister MW, Aaronson P, Spillane J, Schreiber M, Baroso G, Kraemer D, Smotherman C, Gray-Eurom K: Impact of prescription drug-monitoring program on controlled substance prescribing in the ED. Am J Emerg Med 2015, 33(6):781–785. 10.1016/j.ajem.2015.03.036 [DOI] [PubMed] [Google Scholar]
- 46.Pomerleau AC, Schrager JD, Morgan BW: Pilot Study of the Importance of Factors Affecting Emergency Department Opioid Analgesic Prescribing Decisions. J Med Toxicol 2016, 12(3):282–288. 10.1007/s13181-016-0553-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Baehren DF, Marco CA, Droz DE, Sinha S, Callan EM, Akpunonu P: A statewide prescription monitoring program affects emergency department prescribing behaviors. Ann Emerg Med 2010, 56(1):19–23. 10.1016/j.annemergmed.2009.12.011 [DOI] [PubMed] [Google Scholar]
- 48.Weiner SG, Griggs CA, Mitchell PM, Langlois BK, Friedman FD, Moore RL, Lin S, Nelson KP, Feldman JA: Clinician impression versus prescription drug monitoring program criteria in the assessment of drug-seeking behavior in the emergency department. Ann Emerg Med 2013, 62(4):281–289. 10.1016/j.annemergmed.2013.05.025 [DOI] [PubMed] [Google Scholar]
- 49.Wilson HD, Dansie EJ, Kim MS, Moskovitz BL, Chow W, Turk DC. Clinicians’ attitudes and beliefs about opioids survey (CAOS): Instrument development and results of a national physician survey. J Pain 2013, 14(6):613–627. 10.1016/j.jpain.2013.01.769 [DOI] [PubMed] [Google Scholar]
- 50.Smith RJ, Kilaru AS, Perrone J, Paciotti B, Barg FK, Gadsden SM, Meisel ZF: How, why, and for whom do emergency medicine providers use prescription drug monitoring programs? Pain Med 2015, 16(6):1122–1131. 10.1111/pme.12700 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Feldman L, Williams KS, Knox M, Coates J: Influencing controlled substance prescribing: Attending and resident physician use of a state prescription monitoring program. Pain Med 2012, 13(7):908–914. 10.1111/j.1526-4637.2012.01412.x [DOI] [PubMed] [Google Scholar]
- 52.Carnes NA, Wright ER, Norwood CW: A qualitative analysis of prescribers’ and dispensers’ views on improving prescription drug monitoring programs. Res Social & Administrat Pharm 2017, 13(6):1167–1174. 10.1016/j.sapharm.2016.12.002* Prescriber’s opinions on prescription drug monitoring programs (PDMP) and prescribing practices were obtained through responses to open ended questions. Disagreement about administrative and ethical uses of PDMPs and provider suggestions for improving functionality of these programs was unearthed through these responses.
- 53.DeFlavio JR, Rolin SA, Nordstrom BR, Kazal LA: Analysis of barriers to adoption of buprenorphine maintenance therapy by family physicians. Rural Remote Health 2015, 15(1):1–11. [PubMed] [Google Scholar]
- 54.MacDonald K, Lamb K, Thomas ML, Khentigan W: Buprenorphine maintenance treatment of opiate dependence: Correlations between prescriber beliefs and practices. Subst Use & Misuse 2016, 51(1):85–90. 10.3109/10826084.2015.1089905 [DOI] [PubMed] [Google Scholar]
- 55.Andraka-Christou B, Capone MJ: A qualitative study comparing physician-reported barriers to treating addiction using buprenorphine and extended-release naltrexone in U.S. office-based practices. Int’l J Drug Pol’y 2018, 54:9–17. 10.1016/j.drugpo.2017.11.021**Authors highlight the barriers associated with buprenorphine and naltrexone prescribing. Buprenorphine barriers related to regulatory restrictions and liability, which are echoed in other articles. However, the barriers related to naltrexone, a fairly new drug are newly documented in this article. Barriers associated with naltrexone include some of the same regulatory concerns as buprenorphine, but also concern the lack of knowledge and awareness of this medication.
- 56.Hutchinson E, Catlin M, Andrilla CHA, Baldwin LM, Rosenblatt RA: Barriers to primary care physicians prescribing buprenorphine. Ann Fam Med 2014, 12(2):128–133. 10.1370/afm.1595 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Kermack A, Flannery M, Tofighi B, McNeely J, Lee JD: Buprenorphine prescribing practice trends and attitudes among New York providers. J Subst Abuse Treat 2017, 74:1–6. 10.1016/j.jsat.2016.10.005*The authors utilize online surveys to understand buprenorphine prescribing patterns and barriers for New York City buprenorphine prescribers serving largely Medicaid patients. Prior authorization commonly required for buprenorphine prescribing presents a particular concern, highlighting the mismatch between opioid painkiller and buprenorphine prescribing and the need for greater alignment between policy and practice.
- 58.Molfenter T, Sherbeck C, Zehner M, Quanbeck A, McCarty D, Kim JS, Starr S: Implementing buprenorphine in addiction treatment: payer and provider perspectives in Ohio. Subst Abuse: Treat, Prev, & Pol’y 2015, 10(1):1–10. 10.1186/s13011-015-0009-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Knudsen HK, Studts JL: Perceived impacts of the Affordable Care Act: perspectives of buprenorphine prescribers. J Psychoact Drugs 2017, 49(2):111–121. 10.1080/02791072.2017.1295335**Through a mailed survey, the studies demonstrates buprenorphine prescriber ambivalence regarding the impacts the Affordable Care Act would have on buprenorphine access and prescription. However, in states that adopted Medicaid-expansion and state-based health insurance exchanges (both elements of the Affordable Care Act), providers generally had more positive outlooks about what this Act could do for buprenorphine accessibility.
- 60.Behar E, Bagnulo R, Coffin PO: Acceptability and feasibility of naloxone prescribing in primary care settings: a systematic review. Prev Med 2018, 114:79–87. 10.1016/j.ypmed.2018.06.005**This systematic review analyzes the literature around naloxone related practices, such as willingness to prescribe naloxone, feasibility of naloxone prescribing, and prescriber related training. Several studies on naloxone implementation programs in primary care settings—that is, programs that train providers to prescribe naloxone, educate about indications for naloxone prescribing, train on patient education regarding naloxone, and cover logistics for filling naloxone prescriptions—found that although these programs are novel and diverse, they can assist in making naloxone access a standard part of clinical care and increase uptake of naloxone. Authors conclude that naloxone prescribing in primary care settings is not only feasible and acceptable, but also that physicians’ willingness to prescribe naloxone has increased in recent years.
- 61.Behar E, Rowe C, Santos GM, Coffa D, Turner C, Santos NC, Coffin PO: Acceptability of naloxone co-prescription among primary care providers treating patients on long-term opioid therapy for pain. J Gen Intern Med 2016, 32(3):291–295. 10.1007/s11606-016-3911-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Okoro ON, Bastianelli KM, Wen YF, Bilden EF, Konowalchuk BK, Schneiderhan ME: Awareness of state legislation on naloxone accessibility associated with willingness to prescribe naloxone. Subst Abuse 2018, 39(1):14–20. 10.1080/08897077.2017.1356787** Assessment of providers in two mid-western healthcare systems reveal incomplete knowledge of state legislation regarding naloxone, namely Good Samaritan laws and laws conferring naloxone prescribing authority. Authors find that providers who were more aware of state legislation, as well as more confident in their dosing and prescription writing abilities, had higher levels of personal responsibility regarding the need to address opioid misuse and overdose and greater willingness to prescribe naloxone.
- 63.Peckham AM, Niculete ME, Steinberg H, Boggs DL: A survey of prescribers’ attitudes, knowledge, comfort, and fear of consequences related to an opioid overdose education and naloxone distribution program. J Pub Health Manag & Pract 2018, 24(4):310–317. 10.1097/PHH.0000000000000668**Survey results reveal that the majority of Veteran’s Affairs prescribers in primary care/medicine, mental health, and substance use disorder specialties in a Connecticut healthcare system support the dispensing of naloxone. However, only substance use disorder prescribers and psychiatrists report comfort with and knowledge about naloxone prescribing. These comfort levels can be improved through naloxone training education.
- 64.Wilson JD, Spicyn N, Matson P, Alvanzo A, Feldman L: Internal medicine resident knowledge, attitudes, and barriers to naloxone prescription in hospital and clinic settings. Subst Abuse 2016, 37(3):480–487. 10.1080/08897077.2016.1142921 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Winograd RP, Davis CS, Niculete M, Oliva E, Martielli RP: Medical providers’ knowledge and concerns about opioid overdose education and take-home naloxone rescue kits within Veterans Affairs health care medical treatment settings. Subst Abuse 2017, 38(2):135–140. 10.1080/08897077.2017.1303424*This study demonstrates overwhelming Veterans’ Affairs provider support for the policy of co-prescribing of opioid analgesics with naloxone take-home kits and patient education. Despite this support, authors find a lack of knowledge and confidence in prescribing and education around naloxone, which speaks to the need for further education around this topic.
- 66.IQVIA Institute for Human Data Science. (2018). Medicine Use and Spending in the U.S. A Review of 2017 and Outlook to 2022. Retrieved November 27, 2018 from: https://www.iqvia.com/-/media/iqvia/pdfs/institute-reports/medicine-use-and-spending-in-the-us-a-review-of-2017-and-outlook-to-2022.pdf?_=1543433908423