Abstract
BACKGROUND:
Health communication is a field that uses social and behavioral models to improve health outcomes and raise awareness on major health risks that threaten human well-being. Low-income countries (LICs) suffer from the effects of communicable and noncommunicable diseases that are exacerbated by weak health-care systems, lack of awareness campaigns, and ineffective communication tactics. This work aims to explore health communication research in LICs to find strategies that help improve health outcomes in the future.
MATERIALS AND METHODS:
The PubMed database was explored systematically for publications related to health communication from LICs between January 1, 1960, and January 1, 2020. Publications were categorized according to country of origin and were analyzed with respect to population size, gross domestic product (GDP), and primary school enrollment of each state as obtained from the World Bank Open Data.
RESULTS:
Collectively, LICs published 796 contributions, comprising 1.08% of the total biomedical research published by LICs and 0.27% of the world's health communication research. Malawi had the highest number of publications per GDP, with 32.811 publications per billion US$. Uganda had the most contributions per population, with 9.579 publications per million persons. Ethiopia had the highest amount of contributions per primary school enrollment with a ratio of 2.461 publications per %gross. The role of health communication in promoting HIV awareness and prevention was the most common theme explored. Other infectious diseases, such as malaria, tuberculosis, and Ebola, were also highlighted. Improving communication in health education was also explored.
CONCLUSION:
Health communication is a rising field in LICs, with research focusing on disease prevention. Efforts to amplify research are key to effectively utilize the health communication models and improve health outcomes in LICs.
Keywords: Health communication, health education, low-income countries, prevention, public health
Introduction
Health communication constitutes the utilization of social and behavioral models to better health outcomes.[1] It comprises tactics that spread health awareness and data with the goal of encouraging people to follow healthy habits and be better informed about the major health risks that threaten their communities.[2]
According to the World Bank, low-income countries (LICs) are defined as the nations that attain <$1,025 of gross national income/capita in 2018.[3] They consist of 31 countries that are spread unevenly around the globe, through which sub-Saharan Africa is home to the highest number of LICs, whereas South America records the lowest.[3]
LICs face many health challenges due to a variety of economic, social, environmental, and technological factors. This results in weakening the quality of health care provided. The World Bank estimates that the population number of LICs has more than quadrupled in the past 60 years,[3] adding more burden to the currently weak health-care infrastructure.
Today, more than half of the LICs are endemic with chronic illnesses as well as infectious diseases, such as HIV, tuberculosis, and malaria.[4] In addition, maternal, perinatal, and nutritional conditions are important contributors to mortality and deaths.[4] It has been shown that 50% of pregnant women in LICs lack access to medical care services for labor, where most women give birth in rural areas or at home.[5] Nations receive and depend on health aids from international organizations such as the United Nations and nongovernmental organizations. These major health risks, among others, fueled the field of health communication forward, attracting more interest and investment.[6,7] In the past decade, the surge in the influence of social media paved the way for health awareness campaigns to have a wider audience and a far-reaching impact.
Despite various interventions, the health status in LICs does not seem to be significantly improving. One important reason is the lack of investment in research and development to achieve efficient communication between the different constituents of the public health sector. This study aims to assess and explore the research output of LICs in the field of health communication. Bibliometric and thematic analyses were conducted for health communication contributions that originated in the past 60 years from LICs.
Materials and Methods
On April 19, 2020, the PubMed database was investigated for health communication research coming out of LICs. Publications were searched for using the word “communication” as a consistent term in the search field, followed by the [mesh] system to facilitate and narrow down our research, followed by the separator Boolean operator (AND), followed by the name of the targeted country, succeeded by [ad]. For example, to search for health communication articles originating from Benin, the following search format was used: Communication [mesh] AND Benin [ad]. Research results were then scrutinized to make sure that the contributions are coming out of the country concerned [Figure 1].
Figure 1.
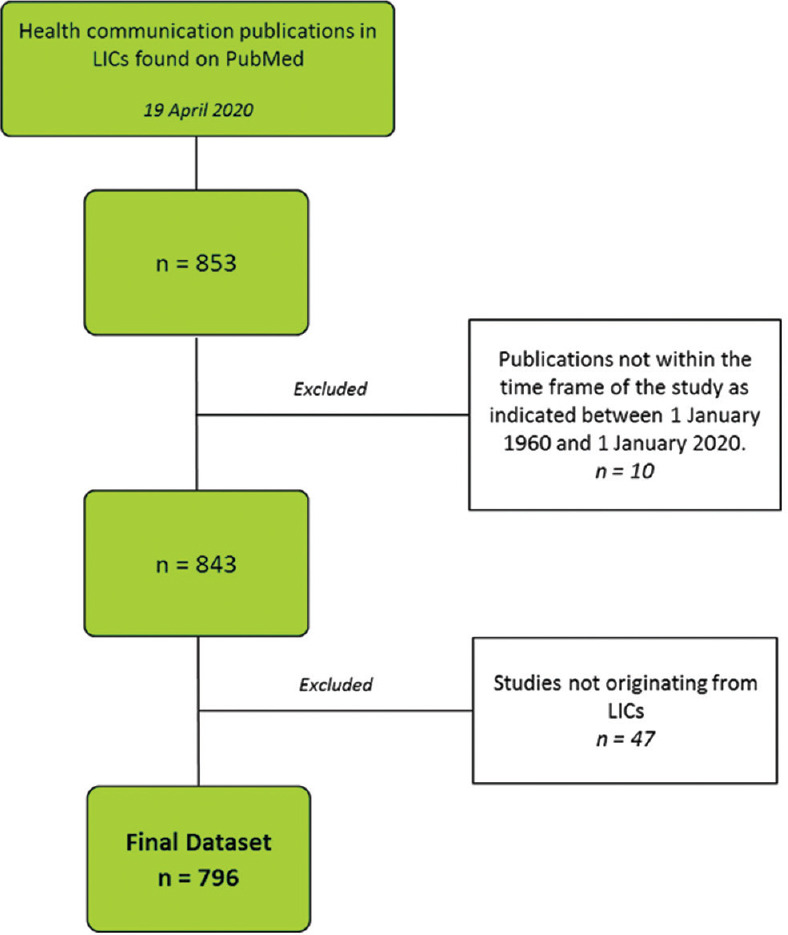
Selection process of health communication publications in the study. LICs = low-income countries
The date range of the study included the 60 years between January 1, 1960, and January 1, 2020. The targeted nations of the research were the 31 countries comprising the LICs.
The number of articles was normalized per gross domestic product (GDP) for each country in order to exclude any bias as a result of the variation of GDP between the countries. This was done by dividing the number of articles of each county by the average GDP/billion US dollars from 1960 till 2020. The number of publications was also explored with respect to population for the purpose of excluding any propensity due to differences in population numbers. The number of articles of each country was divided over the average population per million persons from 1960 till 2020. In addition, health communication publications were explored per average primary school enrollment of each state between 1960 and 2020.
The World Bank Open Data database was used as a source for all the information and metrics used for LICs (https://data.worldbank.org/). The epidemiological nature of the study did not require ethical approval as there was no human or animal involvement.
Results
The number of communication articles related to health and medicine that came out from LICs between 1960 and 2020 is 796, comprising 1.08% of the total biomedical research published by LICs and 0.27% of the world's health communication research within the same time period [Table 1].
Table 1.
Ratio of health communication publications to the total biomedical publications in low-income countries (1960-2020)
| Country | Number of health communication contributions | Total number of biomedical contributions | Percent |
|---|---|---|---|
| Afghanistan | 3 | 551 | 0.544 |
| Benin | 12 | 4009 | 0.299 |
| Burkina Faso | 37 | 3202 | 1.156 |
| Burundi | 1 | 262 | 0.382 |
| Central African Republic | 1 | 275 | 0.364 |
| Chad | 0 | 860 | 0.000 |
| The Democratic Republic of Congo | 3 | 698 | 0.430 |
| Eritrea | 2 | 549 | 0.364 |
| Ethiopia | 120 | 12501 | 0.960 |
| Gambia | 7 | 1888 | 0.371 |
| Guinea | 5 | 2433 | 0.206 |
| Guinea-Bissau | 2 | 470 | 0.426 |
| Haiti | 5 | 714 | 0.700 |
| North Korea | 0 | 14 | 0.000 |
| Liberia | 8 | 387 | 2.067 |
| Madagascar | 5 | 1775 | 0.282 |
| Malawi | 75 | 4589 | 1.634 |
| Mali | 9 | 1848 | 0.487 |
| Mozambique | 37 | 1873 | 1.975 |
| Nepal | 91 | 8749 | 1.040 |
| Niger | 3 | 1103 | 0.272 |
| Rwanda | 33 | 1755 | 1.880 |
| Sierra Leone | 15 | 814 | 1.843 |
| Somalia | 0 | 139 | 0.000 |
| South Sudan | 6 | 176 | 3.409 |
| Syrian Arab Republic | 13 | 1629 | 0.798 |
| Tajikistan | 2 | 177 | 1.130 |
| Tanzania | 103 | 8277 | 1.244 |
| Togo | 7 | 1209 | 0.579 |
| Uganda | 185 | 9541 | 1.939 |
| Yemen | 6 | 1425 | 0.421 |
The research output of LICs is on a rising trend in general [Figure 2]. The publication rate increased slightly from 1980 till 2000 (25 articles). In the past decade, a major increase in output rate took place as articles related to health communication were extensively published. The number of publications per country ranged from 0 (Somalia, North Korea, and Chad) to 185 (Uganda).
Figure 2.
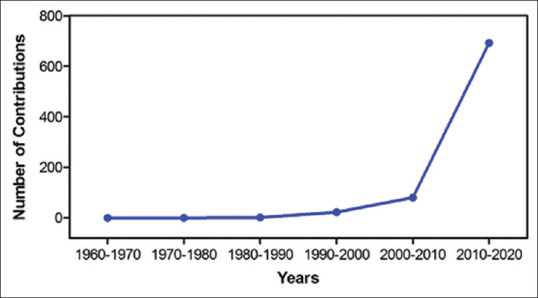
The trend of health communication research output in low-income countries across the decades
The performance of publication issuance of each country was analyzed with respect to several indicators. In terms of publications per GDP, Malawi ranked the first with a ratio of 32.811 publications per billion US$, ahead of Uganda that scored 25.481 publications/billion US$. With respect to publications per population, Uganda ranked first with a ratio of 9.579 publications/million persons. The second highest was Malawi with a ratio of 8.194 publications/million persons. In terms of publications per primary school enrollment, Ethiopia was the first with a ratio of 2.461 publications per %gross, followed by Uganda with a ratio of 2.156 publications per % gross [Table 2].
Table 2.
Ratio of health communication contributions to gross domestic product (billion US$), population (million persons), and primary school enrollment in each low-income country
| Country | Number of health communication contributions | Average GDP (per Billion US$) | Publications per Billion US$ | Average population (per million persons) | Publications per million persons | Average primary school enrolment (%gross) | Publications per % gross |
|---|---|---|---|---|---|---|---|
| Afghanistan | 3 | 7.023 | 0.427 | 18.029 | 0.166 | 56.040 | 0.054 |
| Benin | 12 | 2.863 | 4.191 | 5.605 | 2.141 | 80.021 | 0.150 |
| Burkina Faso | 37 | 3.639 | 10.168 | 9.842 | 3.759 | 44.261 | 0.836 |
| Burundi | 1 | 1.053 | 0.950 | 5.694 | 0.176 | 69.289 | 0.014 |
| Central African Republic | 1 | 0.991 | 1.009 | 2.932 | 0.341 | 73.341 | 0.014 |
| Chad | 0 | 3.343 | 0.000 | 7.047 | 0.000 | 59.238 | 0.000 |
| The Democratic Republic of Congo | 3 | 12.731 | 0.236 | 39.158 | 0.077 | 90.945 | 0.033 |
| Eritrea | 2 | 1.031 | 1.939 | 1.964 | 1.018 | 77.030 | 0.026 |
| Ethiopia | 120 | 22.089 | 5.433 | 53.701 | 2.235 | 48.748 | 2.462 |
| Gambia | 7 | 0.551 | 12.696 | 1.044 | 6.705 | 64.600 | 0.108 |
| Guinea | 5 | 4.926 | 1.015 | 6.785 | 0.737 | 51.728 | 0.097 |
| Guinea-Bissau | 2 | 0.425 | 4.709 | 1.051 | 1.903 | 66.084 | 0.030 |
| Haiti | 5 | 3.032 | 1.649 | 7.093 | 0.705 | 75.901 | 0.066 |
| North Korea | 0 | 443.275 | 0.000 | 19.525 | 0.000 | 102.248 | 0.000 |
| Liberia | 8 | 1.979 | 4.042 | 41.074 | 0.195 | 71.976 | 0.111 |
| Madagascar | 5 | 4.148 | 1.205 | 12.860 | 0.389 | 115.397 | 0.043 |
| Malawi | 75 | 2.286 | 32.811 | 9.153 | 8.194 | 101.795 | 0.737 |
| Mali | 9 | 4.587 | 1.962 | 9.685 | 0.929 | 48.056 | 0.187 |
| Mozambique | 37 | 6.834 | 5.414 | 15.196 | 2.435 | 86.773 | 0.426 |
| Nepal | 91 | 6.142 | 14.817 | 19.016 | 4.786 | 113.006 | 0.805 |
| Niger | 3 | 2.683 | 1.118 | 9.507 | 0.316 | 35.483 | 0.085 |
| Rwanda | 33 | 2.408 | 13.707 | 6.634 | 4.974 | 99.879 | 0.330 |
| Sierra Leone | 15 | 1.337 | 11.217 | 4.313 | 3.478 | 64.980 | 0.231 |
| Somalia | 0 | 1.115 | 0.000 | 7.454 | 0.000 | 20.210 | 0.000 |
| South Sudan | 6 | 12.632 | 0.475 | 5.830 | 1.029 | 81.520 | 0.074 |
| Syrian Arab Republic | 13 | 11.615 | 1.119 | 12.364 | 1.051 | 104.487 | 0.124 |
| Tajikistan | 2 | 3.741 | 0.535 | 5.121 | 0.391 | 96.334 | 0.021 |
| Tanzania | 103 | 21.784 | 4.728 | 27.254 | 3.779 | 79.316 | 1.299 |
| Togo | 7 | 1.592 | 4.398 | 3.988 | 1.755 | 105.449 | 0.066 |
| Uganda | 185 | 7.260 | 25.481 | 19.314 | 9.579 | 85.775 | 2.157 |
| Yemen | 6 | 18.407 | 0.326 | 13.480 | 0.445 | 87.776 | 0.068 |
GDP=Gross domestic product
Discussion
Health communication is an emerging field in LICs; the total contribution of its countries constitutes 0.27% of the world's communication research in medicine and public health. Research carried out in LICs explored different topics and appeared to reflect each country's challenges and concerns. The main themes that predominated communication research were HIV disease disclosure and prevention and health education and research. Other infectious diseases, such as tuberculosis, malaria, and Ebola, and noncommunicable diseases, such as cancer and anemia, were also highlighted.
HIV-related Research
HIV is an extensively spread disease in LICs. Its prevalence in 2018 reached 2.2% among the total population aging between 15 and 49 years.[8] In the African continent, HIV was clearly the major concern of LICs, as it seized a significant portion of their health communication research. Uganda, with the highest number of health communication publications, focused on HIV disclosure and preventive methods through social engagement. In 2018, close to 1.4 million people were living with HIV in Uganda and 23,000 deaths were reported due to HIV.[9] Communication research explored the frequency, factors, and outcomes of HIV disclosure among pregnant women[10] and children.[11] Research also explored the positive effect of social engagement of elderly Ugandans with HIV on overall survival.[12] Ethiopia's communication research discussed the impact of socio-cultural drivers on modern family planning methods among individuals with HIV.[13] In 2018, 690,000 Ethiopians were living with HIV and 11,000 died from it.[14] Research in the endemic country focused on the importance of sexual and reproductive health to promote safe sexual practices and HIV prevention.[15] The Democratic Republic of Congo also highlighted HIV, as it lost 17,000 people from the disease in 2018.[16] Its research stressed on HIV disclosure and its effect on the loss of follow-up of patients on antiretroviral therapy.[17] In Malawi, communication research focused on evaluating the precision of HIV self-reported status in transgender women and homosexual men.[18] It also explored the perceptions and experiences of health-care workers, community leaders, and teachers in dealing with children infected with HIV.[19] Tanzania's health communication research in the rural areas studied the influence of HIV care and examined the reaction of HIV prevention methods done in those areas.[20,21] Other studies focused on the risks associated with sexual relationship between homosexual men and its implications for HIV, the importance of parental communication in supporting HIV patients, and the significance of social networks in increasing the willingness for HIV self-testing.[22,23,24,25]
HIV disclosure status, specifically, was highlighted in most of the research publications related to communication.[10,11,17,19,26] Health communication methods, including group sessions and peer-to-peer support, were emphasized in a multinational workshop to explore the experience of HIV disclosure among children and adolescents from LICs in Central and West Africa.[27] It was estimated that 34% of disclosing adolescents were 10–12 years old and the median age of disclosure was 13 years.[27,28] Fear of the loss of communication with parents and closed ones was shared to be a common theme affecting the young ones’ practice of HIV disclosure.[27] In Burkina Faso, a quasi-experimental approach using a mobile telephone system was set up at five health centers to provide an automated reminder service for health-care consultation appointments targeting women, children, and people living with HIV/AIDS. The new communication method increased prenatal coverage by 7.34%, decreased loss to follow-up by 84%, and increased assisted deliveries by 31%.[29]
Understanding the barriers to and facilitators of proper and functional communication in HIV settings is crucial for designing effective prevention methods. A multinational study from LICs in Africa surveyed children, adolescents, and young adults through HIV-themed scriptwriting competitions to check their awareness on mother-to-child transmission of HIV and its prevention.[30] While prevention awareness and narratives were reported to be more prevalent, intergenerational belief in which mother-to-child transmission of HIV was depicted as inevitable persisted in some groups, emphasizing the need for better communication methods to reflect the full promise of developments and prevention mechanisms available today.[30] In Guinea, a study examined gender norms and perceptions in children on topics of sex, sexual relationships, and HIV.[31] Males were reported to use more explicit language in discussions related to sex and talk more publicly about it, which emphasize the need for proper health communication tools to increase sex and HIV education programs among females.[31] In a cross-sectional survey from Guinea-Bissau, poor adherence to HIV treatment was studied to reveal the barriers for effective antiretroviral therapy. Illiteracy on proper health practices related to HIV was prevalent in 41% of the studied patients with HIV.[32] Forgetfulness, side effects, lack of food, and other illnesses were common justifications, emphasizing the need for better awareness and a holistic approach to improving life conditions of patients with HIV.[32] In Togo, a single-center study explored HIV disclosure among partners and determined that only 60% of patients with HIV had disclosed their HIV serostatus to their sexual partners, emphasizing the need for better health communication between sexual partners.[26] In the Democratic Republic of Congo, a retrospective study explored the impact of nondisclosure of HIV status on the loss to follow-up of patients receiving antiretroviral therapy.[17] The study revealed that patients who did not disclose HIV status had a higher hazard of not following up on medical condition.[17]
Education-related Research
Education in LICs also faces many challenges as 20.8 million children were estimated to be out of school in 2018.[33] In addition, upper-secondary out-of-school rate reaches 59%.[34] The topic of health education was addressed in LICs by emphasizing the instrumentality of research in health communication. Uganda's communication research, for example, focused on enhancing the adherence of inpatients to prescribed medications using health quality improvement educational techniques.[35] Baseline data collection revealed a pre-intervention median inpatient medication adherence rate of 46.5% on the study ward. Deficiencies were also identified in attendant (lay caretaker) education, and prescriber and pharmacy metrics.[35] Plan-Do-Study-Act cycle interventions were implemented, whereby attendant involvement and education, physician prescription practices, and improving pharmacy communication with clinicians and attendants were focused on and emphasized.[35] These techniques improved health-care delivery, especially in environments with scarce resources.[35] Another Ugandan study emphasized the importance of teaching children how to evaluate and understand treatment effects to improve their health knowledge and their engagement in a healthy society.[36] A network of pre-trained primary school teachers was established to teach children how to assess claims of treatment effects. Afterwards, 92% of the participating children reported understanding the explained concepts well, rating their own understanding above 75 on a self-assessment scale of 1-to-100.[36]
In Ethiopia, community-based education was analyzed to evaluate its role in raising awareness, addressing health problems, and enhancing health-care practices among students.[37] Results of cross-sectional surveys in schools showed the need for faculty motivation, deployment of students across expanded health centers, and the adoption of innovation.[37] Research from Gambia examined the importance of antenatal care education for pregnant women.[38] Providing necessary information and communication about childbirth assisted women in improving certain choices and resulted in maintaining a healthier pregnancy.[38] In Rwanda, research focused on palliative care increased palliative literacy and provided better communication between stakeholders.[39] In Nepal, a cross-sectional study on health students showed that students had moderate support and skills to manage their own health, highlighting the need for universities to implement interventions that aim at improving access to health information and facilitating engagement with health-care providers.[40] The Medical Education Partnership Initiative was also highlighted after it had influenced many areas of African medical training in fields such as information technology and scientific output.[37,41]
Medical Research in Health Communication
Medical research was also one of the common themes of health communication research in LICs. Contributions emphasized the importance of bridging health policy and research to enhance health outcomes[42] and facilitate knowledge exchange in the health system.[43] In addition, studies highlighted the role of research in enhancing maternal and child health practices in LICs in Africa and Latin America.[44] Furthermore, improving health research, strengthening its receptive environment and capacity, and facilitating its access were major concerns in a portion of the health communication contributions.[45,46]
Health Communication and Endemic Diseases
Other endemic diseases such as malaria, tuberculosis, and Ebola were also discussed in terms of health communication. A study from Guinea assessed the reception of text messages that are designed to remind health workers of the malaria treatment protocol, facilitating the efficient administration of malaria treatment.[47] Whereas in Tanzania, research focused on raising awareness on the importance of malarial vaccine among parents.[48]
Benin's health communication research on tuberculosis explored the introduction of a digital information system that facilitates early diagnosis and prevention of the disease.[49] Text messages aimed at reminding patients with tuberculosis of their medical appointments and checkups were studied in Mozambique to decrease the number of missed appointments, strengthen the communication between health workers and patients, and assist in increasing the patients’ motivation toward therapy.[50]
After the Ebola outbreak hit West Africa in 2013, researchers from Guinea and Sierra Leone focused on communication strategies to overcome the disease. Health communication research from Guinea revealed that the main challenges in raising the country's readiness against Ebola spread were due to the country's health system that suffers from poor coordination mechanisms, inadequate training of human resources, and lack of equipment and supplies to field teams and health facilities.[51] In Sierra Leone, researchers addressed the operational challenges during the Ebola outbreak, highlighting the need for proper communication resources to resolve challenges in Ebola case investigations.[52]
Miscellaneous Health Communication Themes in LICs
Prevention was an important goal of health communication research in cancer and anemia. The need to educate Ugandan women on the prevention methods of cervical cancer was highlighted.[53] In Ethiopia, anemia awareness among pregnant women was explored in terms of socioeconomic factors, such as job status and literacy, to reduce its prevalence.[54] Furthermore, the factors, magnitude, and severity of child anemia were studied to provide preventive guidelines that can reduce the intensity of anemia among children.[55]
Health communication coming out of LICs outside Africa highlighted other important challenges. Afghanistan's communication research focused on the consequences of politicizing humanitarian aids in the country.[56] In South Sudan, a study on posttraumatic stress disorder (PTSD) collected and analyzed people's opinions on PTSD to address misconceptions and misinformation on the disease.[57]
Research from other countries addressed distinct topics. In Syria, for example, dentistry constituted 30% of the total research in health communication. Studies discussed the causes and effects of a gummy smile and its possible treatments,[58] compared between different orthodontic retainers,[59] and assessed speech performance upon the introduction of lingual and labial appliances.[60]
Strengths and Limitations
This study is unique as it addresses health communication, as a novel and rising field, in LICs. It analyzes research in the field – epidemiologically and thematically – to explore quantitative and qualitative output and to highlight key themes of public health importance in LICs. In addition, the study covers a time period of > 60 years to encompass a wide search of health communication research. Nevertheless, the study is limited as it solely explores articles found through the PubMed database.
Conclusion
Health communication is a rising field in LICs, with research in the field mostly focusing on disease prevention and disclosure. Some countries, such as Chad, Somalia, and North Korea, had nil contributions in health communication. The lack of academic freedom, poverty, political instability, and conflict are important contributors of low research output.[1,61,62,63,64] With the rapid rise in use and popularity of social media platforms, health communication, as a field, will become a major tool to address public and global health needs.[65] As such, more efforts ought to be exerted to promote a research culture that make use of the current rise of communication media to promote healthy lifestyles and habits in LICs.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Mheidly N, Fares J. Health communication research in the Arab world: A bibliometric analysis. Integrated Healthc J. 2020;2:e000011. doi: 10.1136/ihj-2019-000011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention. Health Communication Basics. 2020. [Last accessed on 2020 Apr 15]. Available from: https://wwwcdcgov/healthcommunication/healthbasics/WhatIsHChtml .
- 3.World Bank. World Bank Country and Lending Groups. 2020. [Last accessed on 2020 Apr 15]. Available from: https://datahelpdeskworldbankorg/knowledgebase/articles/906519-world-bank-country- and-lending-groups .
- 4.Institute for Health Metrics and Evaluation. Findings from the Global Burden of Disease Study 2017. IHME; 2018. [Google Scholar]
- 5.Bösenberg AT. 51-Pediatric anesthesia in developing countries. In: Coté CJ, Lerman J, Anderson BJ, editors. A Practice of Anesthesia for Infants and Children. 6th ed. Philadelphia: Content Repository Only!; 2019. pp. 1161–74.e1163. [Google Scholar]
- 6.Pantoja T, Opiyo N, Lewin S, Paulsen E, Ciapponi A, Wiysonge CS, et al. Implementation strategies for health systems in low-income countries: An overview of systematic reviews. Cochrane Database Syst Rev. 2017;9:CD011086. doi: 10.1002/14651858.CD011086.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hurt K, Walker RJ, Campbell JA, Egede LE. mHealth Interventions in low and middle-income countries: A systematic review. Glob J Health Sci. 2016;8:54429. doi: 10.5539/gjhs.v8n9p183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.World Bank. Prevalence of HIV, Total (% of Population ages 15-49) – Low Income. 2019. [Last accessed on 2020 Apr 15]. Available from: https://dataworldbankorg/indicator/SHDYNAIDSZSlocations=XM .
- 9.UNAIDS. Uganda. 2018. [Last accessed on 2019 Dec 26]. Available from: https://wwwunaidsorg/en/regionscountries/countries/uganda .
- 10.Ngonzi J, Mugyenyi G, Kivunike M, Mugisha J, Salongo W, Masembe S, et al. Frequency of HIV status disclosure, associated factors and outcomes among HIV positive pregnant women at Mbarara Regional Referral Hospital, southwestern Uganda. Pan Afr Med J. 2019;32:200. doi: 10.11604/pamj.2019.32.200.12541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Klingberg S, King R, Seeley J, Lubwama R, Namuganga M, Nabiryo B, et al. Courage and confidence to stop lying: Caregiver perspectives on a video to support paediatric HIV disclosure in Kampala, Uganda. Afr J AIDS Res. 2018;17:273–9. doi: 10.2989/16085906.2018.1521850. [DOI] [PubMed] [Google Scholar]
- 12.Mugisha JO, Schatz EJ, Hansen C, Leary E, Negin J, Kowal P, et al. Social engagement and survival in people aged 50 years and over living with HIV and without HIV in Uganda: A prospective cohort study. Afr J AIDS Res. 2018;17:333–40. doi: 10.2989/16085906.2018.1542322. [DOI] [PubMed] [Google Scholar]
- 13.Derek A, Seme A, Anye CS, Nkfusai CN, Cumber SN. Modern family planning use among people living with HIV/AIDS: A facility based study in Ethiopia. Pan Afr Med J. 2019;33:224. doi: 10.11604/pamj.2019.33.224.19025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.UNAIDS. Ethiopia. 2018. [Last accessed on 2019 Dec 26]. Available from: https://wwwunaidsorg/en/regionscountries/countries/ethiopia .
- 15.Mekonen MT, Dagnew HA, Yimam TA, Yimam HN, Reta MA. Adolescent-parent communication on sexual and reproductive health issues and associated factors among high school students in Woldia town, Northeastern Ethiopia. Pan Afr Med J. 2018;31:35. doi: 10.11604/pamj.2018.31.35.13801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.UNAIDS. Democratic Republic of the Congo. 2018. [Last accessed on 2019 Dec 26]. Available from: https://wwwunaidsorg/en/regionscountries/countries/democraticrepublicofthecongo .
- 17.Akilimali PZ, Musumari PM, Kashala-Abotnes E, Kayembe PK, Lepira FB, Mutombo PB, et al. Disclosure of HIV status and its impact on the loss in the follow-up of HIV-infected patients on potent anti-retroviral therapy programs in a (post-) conflict setting: A retrospective cohort study from Goma, Democratic Republic of Congo. PLoS One. 2017;12:e0171407. doi: 10.1371/journal.pone.0171407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fogel JM, Sandfort T, Zhang Y, Guo X, Clarke W, Breaud A, et al. Accuracy of self-reported HIV status among African men and transgender women who have sex with men who were screened for participation in a research study: HPTN 075. AIDS Behav. 2019;23:289–94. doi: 10.1007/s10461-018-2231-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kalembo FW, Kendall GE, Ali M, Chimwaza AF, Tallon MM. Primary caregivers, healthcare workers, teachers and community leaders’ perceptions and experiences of their involvement, practice and challenges of disclosure of HIV status to children living with HIV in Malawi: A qualitative study. BMC Public Health. 2018;18:884. doi: 10.1186/s12889-018-5820-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sanga ES, Mukumbang FC, Mushi AK, Lerebo W, Zarowsky C. Understanding factors influencing linkage to HIV care in a rural setting, Mbeya, Tanzania: Qualitative findings of a mixed methods study. BMC Public Health. 2019;19:383. doi: 10.1186/s12889-019-6691-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cawley C, Wringe A, Wamoyi J, Lees S, Urassa M. 'It is just the way it was in the past before I went to test': A qualitative study to explore responses to HIV prevention counselling in rural Tanzania. BMC Public Health. 2016;16:489. doi: 10.1186/s12889-016-3109-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Conserve DF, Bay C, Kilonzo MN, Makyao NE, Kajula L, Maman S. Sexual and social network correlates of willingness to self-test for HIV among ever-tested and never-tested men: Implications for the Tanzania STEP project. AIDS Care. 2019;31:169–76. doi: 10.1080/09540121.2018.1537466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ross MW, Larsson M, Jacobson J, Nyoni J, Agardh A. Social networks of men who have sex with men and their implications for HIV/STI interventions: Results from a cross-sectional study using respondent-driven sampling in a large and a small city in Tanzania. BMJ Open. 2016;6:e012072. doi: 10.1136/bmjopen-2016-012072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ross MW, Nyoni J, Ahaneku HO, Mbwambo J, McClelland RS, McCurdy SA. High HIV seroprevalence, rectal STIs and risky sexual behaviour in men who have sex with men in Dar es Salaam and Tanga, Tanzania. BMJ Open. 2014;4:e006175. doi: 10.1136/bmjopen-2014-006175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kajula LJ, Sheon N, De Vries H, Kaaya SF, Aarø LE. Dynamics of parent-adolescent communication on sexual health and HIV/AIDS in Tanzania. AIDS Behav. 2014;18(Suppl 1):S69–74. doi: 10.1007/s10461-013-0634-6. [DOI] [PubMed] [Google Scholar]
- 26.Yaya I, Saka B, Landoh DE, Patchali PM, Patassi AA, Aboubakari AS, et al. HIV status disclosure to sexual partners, among people living with HIV and AIDS on antiretroviral therapy at Sokodé regional hospital, Togo. PLoS One. 2015;10:e0118157. doi: 10.1371/journal.pone.0118157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Dahourou DL, Masson D, Aka-Dago-Akribi H, Gauthier-Lafaye C, Cacou C, Raynaud JP, et al. HIV disclosure to the child/adolescent in central and West Francophone Africa. Bull Soc Pathol Exot. 2019;112:14–21. doi: 10.3166/bspe-2019-0063. [DOI] [PubMed] [Google Scholar]
- 28.Dahourou D, Raynaud JP, Leroy V. The challenges of timely and safe HIV disclosure among perinatally HIV-infected adolescents in sub-Saharan Africa. Curr Opin HIV AIDS. 2018;13:220–9. doi: 10.1097/COH.0000000000000462. [DOI] [PubMed] [Google Scholar]
- 29.Yé M, Kagoné M, Sié A, Bagagnan C, Sanou H, Millogo O, et al. Promoting access equity and improving health care for women, children and people living with HIV/AIDS in Burkina Faso through mHealth. J Public Health (Oxf) 2018;40:ii42–51. doi: 10.1093/pubmed/fdy196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Winskell K, Kus L, Sabben G, Mbakwem BC, Tiéndrébéogo G, Singleton R. Social representations of mother-to-child transmission of HIV and its prevention in narratives by young Africans from five countries, 1997-2014: Implications for communication. Soc Sci Med. 2018;211:234–42. doi: 10.1016/j.socscimed.2018.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kelly A, Worth H, Akuani F, Kepa B, Kupul M, Walizopa L, et al. Gendered talk about sex, sexual relationships and HIV among young people in Papua New Guinea. Cult Health Sex. 2010;12:221–32. doi: 10.1080/13691050903181107. [DOI] [PubMed] [Google Scholar]
- 32.Dyrehave C, Rasmussen DN, Hønge BL, Jespersen S, Correia FG, Medina C, et al. Nonadherence is associated with lack of HIV-related knowledge: A cross-sectional study among HIV-infected individuals in Guinea-Bissau. J Int Assoc Providers AIDS Care. 2015;15:350–8. doi: 10.1177/2325957415599211. [DOI] [PubMed] [Google Scholar]
- 33.World Bank. Low Income. 2019. [Last accessed on 2020 Apr 15]. Available from: https://dataworldbankorg/income-level/low-income .
- 34.UNESCO. Education Data Release: One in Every Five Children, Adolescents and Youth is Out of School. 2018. [Last accessed on 2020 Apr 15]. Available from: http://uisunescoorg/en/news/education-data-release-one-every-five-children-adolescents- and-youth-out-school .
- 35.Alupo P, Ssekitoleko R, Rabin T, Kalyesubula R, Kimuli I, Bodnar BE. Improving inpatient medication adherence using attendant education in a tertiary care hospital in Uganda. Int J Qual Health Care. 2017;29:587–92. doi: 10.1093/intqhc/mzx075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Nsangi A, Semakula D, Oxman AD, Sewankambo NK. Teaching children in low-income countries to assess claims about treatment effects: Prioritization of key concepts. J Evid Based Med. 2015;8:173–80. doi: 10.1111/jebm.12176. [DOI] [PubMed] [Google Scholar]
- 37.Mariam DH, Sagay AS, Arubaku W, Bailey RJ, Baingana RK, Burani A, et al. Community-based education programs in Africa: Faculty experience within the Medical Education Partnership Initiative (MEPI) network. Acad Med. 2014;89(8 Suppl):S50–54. doi: 10.1097/ACM.0000000000000330. [DOI] [PubMed] [Google Scholar]
- 38.Anya SE, Hydara A, Jaiteh LE. Antenatal care in The Gambia: Missed opportunity for information, education and communication. BMC Pregnancy Childbirth. 2008;8:9. doi: 10.1186/1471-2393-8-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Rosa WE, Male MA, Uwimana P, Ntizimira CR, Sego R, Nankundwa E, et al. The advancement of palliative care in rwanda: transnational partnerships and educational innovation. J Hosp Palliat Nurs. 2018;20:304–12. doi: 10.1097/NJH.0000000000000459. [DOI] [PubMed] [Google Scholar]
- 40.Budhathoki SS, Pokharel PK, Jha N, Moselen E, Dixon R, Bhattachan M, et al. Health literacy of future healthcare professionals: A cross-sectional study among health sciences students in Nepal. Int Health. 2019;11:15–23. doi: 10.1093/inthealth/ihy090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Bagala JP, Macheka ND, Abebaw H, Wen LS. Implementation of the Medical Education Partnership Initiative: Medical students’ perspective. Acad Med. 2014;89(8 Suppl):S32–4. doi: 10.1097/ACM.0000000000000343. [DOI] [PubMed] [Google Scholar]
- 42.Theobald S, Brandes N, Gyapong M, El-Saharty S, Proctor E, Diaz T, et al. Implementation research: New imperatives and opportunities in global health. Lancet. 2018;392:2214–28. doi: 10.1016/S0140-6736(18)32205-0. [DOI] [PubMed] [Google Scholar]
- 43.Cole DC, Nyirenda LJ, Fazal N, Bates I. Implementing a national health research for development platform in a low-income country – A review of Malawi's Health Research Capacity Strengthening Initiative. Health Res Policy Syst. 2016;14:24. doi: 10.1186/s12961-016-0094-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Vargas E, Becerril-Montekio V, Gonzalez-Block MÁ, Akweongo P, Hazel CN, Cuembelo Mde F, et al. Mapping the use of research to support strategies tackling maternal and child health inequities: Evidence from six countries in Africa and Latin America. Health Res Policy Syst. 2016;14:1. doi: 10.1186/s12961-015-0072-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Aidam J, Sombié I. The West African Health Organization's experience in improving the health research environment in the ECOWAS region. Health Res Policy Syst. 2016;14:30. doi: 10.1186/s12961-016-0102-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Dagenais C, Somé TD, Boileau-Falardeau M, McSween-Cadieux E, Ridde V. Collaborative development and implementation of a knowledge brokering program to promote research use in Burkina Faso, West Africa. Glob Health Action. 2015;8:26004. doi: 10.3402/gha.v8.26004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kurumop SF, Bullen C, Whittaker R, Betuela I, Hetzel MW, Pulford J. Improving health worker adherence to malaria treatment guidelines in Papua New Guinea: Feasibility and acceptability of a text message reminder service. PLoS One. 2013;8:e76578. doi: 10.1371/journal.pone.0076578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Romore I, Ali AM, Semali I, Mshinda H, Tanner M, Abdulla S. Assessment of parental perception of malaria vaccine in Tanzania. Malar J. 2015;14:355. doi: 10.1186/s12936-015-0889-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Andre E, Isaacs C, Affolabi D, Alagna R, Brockmann D, de Jong BC, et al. Connectivity of diagnostic technologies: Improving surveillance and accelerating tuberculosis elimination. Int J Tuberc Lung Dis. 2016;20:999–1003. doi: 10.5588/ijtld.16.0015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Nhavoto JA, Grönlund Š, Klein GO. Mobile health treatment support intervention for HIV and tuberculosis in Mozambique: Perspectives of patients and healthcare workers. PLoS One. 2017;12:e0176051. doi: 10.1371/journal.pone.0176051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Thiam S, Delamou A, Camara S, Carter J, Lama EK, Ndiaye B, et al. Challenges in controlling the Ebola outbreak in two prefectures in Guinea: Why did communities continue to resist? Pan Afr Med J. 2015;22(Suppl 1):22. doi: 10.11694/pamj.supp.2015.22.1.6626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Boland ST, Polich E, Connolly A, Hoar A, Sesay T, Tran AA. Overcoming operational challenges to ebola case investigation in Sierra Leone. Glob Health Sci Pract. 2017;5:456–67. doi: 10.9745/GHSP-D-17-00126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Mukama T, Ndejjo R, Musabyimana A, Halage AA, Musoke D. Women's knowledge and attitudes towards cervical cancer prevention: A cross sectional study in Eastern Uganda. BMC Womens Health. 2017;17:9. doi: 10.1186/s12905-017-0365-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Mekonnen FA, Ambaw YA, Neri GT. Socio-economic determinants of anemia in pregnancy in North Shoa Zone, Ethiopia. PLoS One. 2018;13:e0202734. doi: 10.1371/journal.pone.0202734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Birhanu M, Gedefaw L, Asres Y. Anemia among school-age children: Magnitude, severity and associated factors in Pawe Town, Benishangul-Gumuz Region, Northwest Ethiopia. Ethiop J Health Sci. 2018;28:259–66. doi: 10.4314/ejhs.v28i3.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Atmar MH. Politicisation of humanitarian aid and its consequences for Afghans. Disasters. 2001;25:321–30. doi: 10.1111/1467-7717.00181. [DOI] [PubMed] [Google Scholar]
- 57.Ng LC, López B, Pritchard M, Deng D. Posttraumatic stress disorder, trauma, and reconciliation in South Sudan. Soc Psychiatry Psychiatr Epidemiol. 2017;52:705–14. doi: 10.1007/s00127-017-1376-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Alammar AM, Heshmeh OA. Lip repositioning with a myotomy of the elevator muscles for the management of a gummy smile. Dent Med Probl. 2018;55:241–6. doi: 10.17219/dmp/92317. [DOI] [PubMed] [Google Scholar]
- 59.Saleh M, Hajeer MY, Muessig D. Acceptability comparison between Hawley retainers and vacuum-formed retainers in orthodontic adult patients: A single-centre, randomized controlled trial. Eur J Orthod. 2017;39:453–61. doi: 10.1093/ejo/cjx024. [DOI] [PubMed] [Google Scholar]
- 60.Khattab TZ, Farah H, Al-Sabbagh R, Hajeer MY, Haj-Hamed Y. Speech performance and oral impairments with lingual and labial orthodontic appliances in the first stage of fixed treatment. Angle Orthod. 2013;83:519–26. doi: 10.2319/073112-619.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Fares J, Salhab HA, Fares MY, Khachfe HH, Fares Y. Academic medicine and the development of future leaders in healthcare. In: Laher I, editor. Handbook of Healthcare in the Arab World. Cham: Springer; 2020. [Google Scholar]
- 62.Fares MY, Fares J, Baydoun H, Fares Y. Sport and exercise medicine research activity in the Arab world: A 15-year bibliometric analysis. BMJ Open Sport Exerc Med. 2017;3:e000292. doi: 10.1136/bmjsem-2017-000292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Fares Y, Fares J. Neurosurgery in Lebanon: History, development, and future challenges. World Neurosurg. 2017;99:524–32. doi: 10.1016/j.wneu.2016.12.014. [DOI] [PubMed] [Google Scholar]
- 64.Fares Y, Fares J, Kurdi MM, Bou Haidar MA. Physician leadership and hospital ranking: Expanding the role of neurosurgeons. Surg Neurol Int. 2018;9:199. doi: 10.4103/sni.sni_94_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Mheidly N, Fares J. Leveraging media and health communication strategies to overcome the COVID-19 infodemic. J Public Health Policy. 2020 doi: 10.1057/s41271-020-00247-w. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]


