Figure 3. Precision Medicine for Obesity Care.
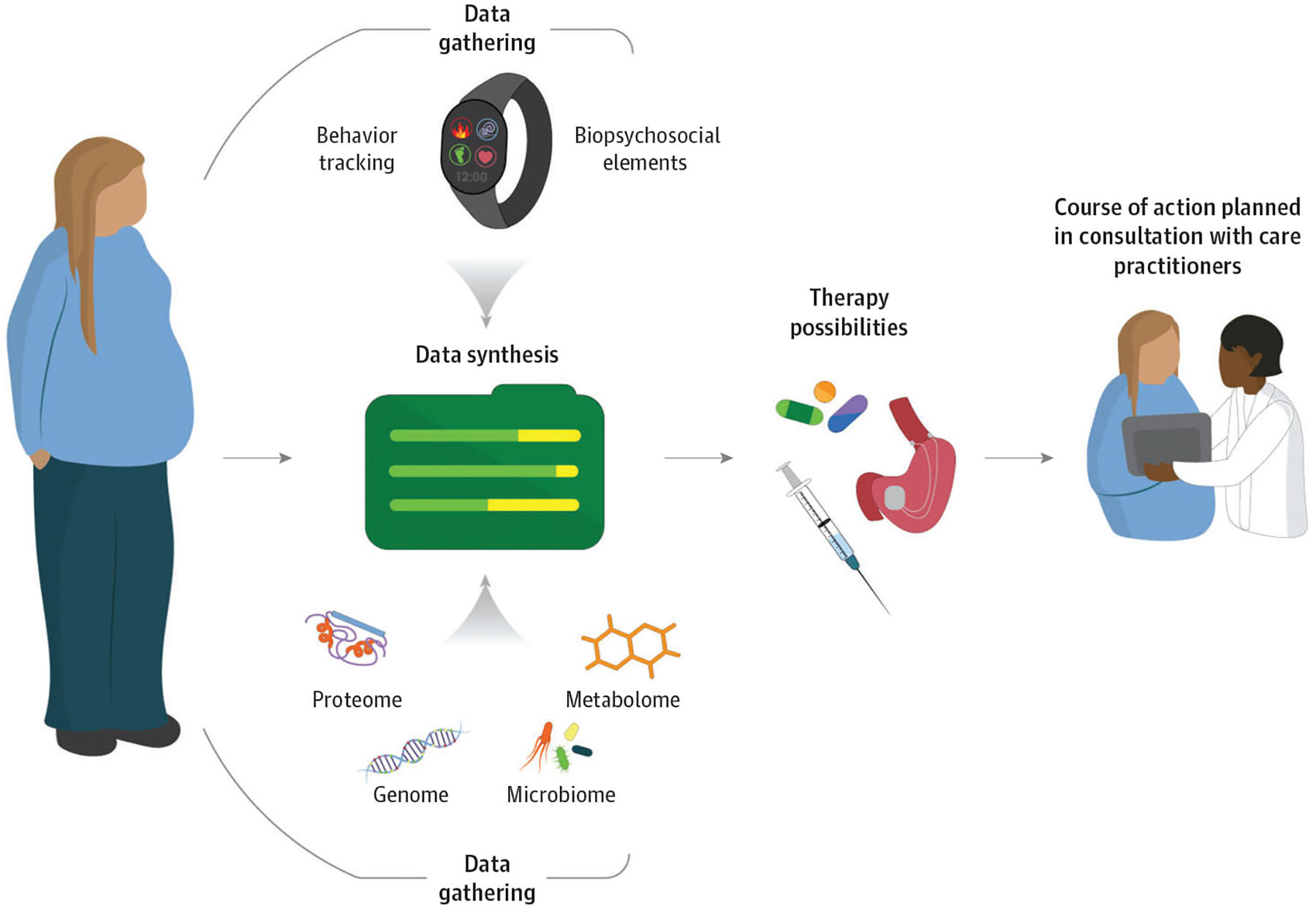
This figure outlines gaps and opportunities for future research aimed at developing more effective and targeted treatments for adolescents with obesity, based on a 2017 National Institutes of Health-sponsored workshop devoted to this topic.81 Numerous areas were identified as potentially strategic opportunities, including achieving consensus on appropriate body mass index metrics, development of valid measures of phenotypes and predictors, characterization of mechanisms associated with development of severe obesity, discovery of novel treatments informed by biologically and psychosocially plausible mechanisms, identification of biopsychosocial phenotypes predicting treatment response, standardization of outcome measures, and improving clinical care.81 An important goal will be to characterize physiologic information (eg, genetics, metabolomics, and microbiome) with biopsychosocial elements (eg, behavior, psychological factors, and social factors such as socioeconomic status), to synthesize the data into meaningful predictors to identify and maximize treatments with the most potential for a particular individual. As the knowledge base grows in these areas, tailored treatment strategies may be developed, rigorously evaluated, and ultimately translated to the clinical setting to enhance care delivery for adolescents living with obesity.
