Abstract
Introduction.
There is growing evidence that computer-delivered or –assisted forms of cognitive-behavior therapy (CCBT) are helpful, but cost-effectiveness versus standard therapies is not well established.
Objective.
To evaluate the cost-effectiveness of a therapist-supported method for CCBT in comparison to standard CBT.
Method.
154 drug-free MDD outpatients were randomly assigned to either 16 weeks of standard CBT (up to twenty 50-minute sessions) or CCBT using the Good Days Ahead program (including up to 5.5 hours of therapist contact). Outcomes were assessed at baseline, weeks 8 and 16, and at 3 and 6 months post-treatment. Economic analyses took into account the costs of services received and work/social role impairment.
Results.
In the context of almost identical efficacy, a form of CCBT that used only about one- third the amount of therapist contact as conventional CBT was highly cost-effective compared to conventional therapy and reduced cost of treatment by $928 per patient.
Conclusions.
A method of CCBT that blended internet-delivered modules and abbreviated therapeutic contact reduced the cost of treatment substantially without adversely affecting outcomes. Results suggest that use of this approach can more than double the access to CBT. Because clinician support in CCBT can be provided by telephone, videoconference, and/or email, this highly efficient form of treatment could be a major advance in remote treatment delivery.
Keywords: Computer-Assisted Cognitive-Behavior Therapy, Depression, Cost-effectiveness
Cognitive-behavior therapy (CBT) is the best studied form of psychotherapy and is considered to be a first-line option for depressed outpatients in contemporary practice guidelines.(1,2) The efficacy of CBT in randomized controlled trials (RCTs) is comparable to that of antidepressant medications(3–5) and, when effective, the benefits may be more long-lasting than pharmacotherapy.(6,7) Nevertheless, the public health impact CBT is limited by factors such as cost, the perceived inconvenience of traveling to weekly face-to-face sessions and a shortage of trained therapists, particularly in public mental health settings or rural regions.(8–10) Computer-assisted models of CBT – also known as CCBT - have been introduced over the past 25 years to reduce such barriers.(11,12) Several models of CCBT are accessible via the internet, thus facilitating remote treatment delivery.(13–15) The efficacy of CCBT is documented by meta-analyses of RCTs.(16–18) However, in studies that test CCBT as a “stand alone” intervention (i.e., no clinical support is provided), the observed effects are typically smaller than observed when CCBT includes at least several hours of therapist support.(18,19) One approach to CCBT specifically developed for use as an adjunct to individual therapy, Good Days Ahead (GDA),(15) blends a 9-module multimedia program with abbreviated sessions with a clinician. Research conducted to date suggests that GDA has efficacy comparable to conventional CBT despite a substantial reduction in therapist contact.(20,21) The current report examines the cost-effectiveness of GDA in the second, larger-scale RCT.(21)
METHODS
A detailed description of this two-center study is published elsewhere.(21) To summarize, the study was open to adult outpatients presenting for treatment of Major Depressive Disorder (MDD) (Structured Clinical Interview for DSM-IV)(22). All participants provided written informed consent for research participation. The Institutional Review Boards of our respective university medical centers approved the consent documents and the study was conducted according to the principles of ethical research practice outlined by the Declaration of Helsinki. After completion of baseline evaluations, eligible, unmedicated patients scoring ≥14 on the Hamilton Rating Scale for Depression (HAMD)(23) were randomized to receive either CCBT or CBT for 16 weeks of acute phase therapy. Experienced therapists (n=9) conducted both interventions; mode-specific consultation was provided by two of the investigators (GKB & JHW) and centered on review of audio recordings to ensure protocol adherence.
The face-to-face component of CCBT consisted of a 50-minute-long introductory session and eleven 25-minute sessions. The first 9 sessions focused of one of the 9 internet-delivered GDA modules. The GDA software was accessible on personal computers (PCs), laptops or tablets; it was not fully operational on smartphones. Workstations with PCs were available for patients who did not have own their own device. Patients were encouraged to work through each module at their own pace; generally, it took between 30 to 60 minutes to finish each module. After completion of the 9 modules, the final three 25-minute “booster” sessions focused on mastery of skills and practice of relapse prevention strategies. CCBT thus consisted of a maximum of 5.5 hours of therapist contact.
Conventional CBT utilized the methods of A.T. Beck and colleagues,(24) as updated by J. Beck(25) and Wright and colleagues.(26) To ensure a strong test of the efficacy of GDA, we employed a relatively intensive CBT protocol consisting of twenty 50-minute sessions (twice weekly for 4 weeks, weekly for 12 weeks; maximum therapist time: 16 hours 40 minutes).(27,28) Outcome assessments were conducted after 8 and 16 weeks of acute phase therapy and repeated 3 and 6 months post-treatment.
Cost-effectiveness analyses were guided by the earlier studies of McCrone et al.(29,30) The Client Service Receipt Inventory (CSRI),(31) which was administered at baseline, week 16 and 3 and 6 months post-treatment, was used to record information on primary care and hospital-based services, as well as other community-based services and medications. The specific costs of CCBT were relatively small (total: $100 per patient, including the manufacturer’s suggested license fee and hardware maintenance). Otherwise, the difference in cost of CBT and CCBT was largely determined by the study’s design, as the CCBT group incurred only about one third of the cost attributable to therapist time of the CBT group. The costs of other services were based on local Medicaid, Medicare, and private insurer prices in addition to overhead for clinical space. Lost income was estimated using the human capital approach by combining lost workdays with average daily hourly earnings.(31) For the purposes of the cost- effectiveness evaluation, the Quality of Well Being Scale – Self Administered (QWB-SA) (32) was used to generate quality-adjusted life years (QALYs), which permitted comparison of the results of the interventions evaluated here with other clinical interventions. Service costs and total costs (including lost workdays) were compared between the treatment groups using regression models, controlling for baseline differences. Bootstrap methods were used to produce confidence intervals around the cost differences due to the likely skewness in the distribution of regression residuals. The cost-effectiveness of CCBT and CBT was compared by combining service cost data and information on symptoms and QALYs.(33) If either intervention had both lower costs and better outcomes than the other, it would be the preferred option. Uncertainty in cost-effectiveness estimates was explored by calculating cost and outcome differences on 1000 bootstrapped re-samples and plotting these on a cost-effectiveness plane. This analysis showed the probability that, when compared to CBT, CCBT could result in: (i) lower costs and worse outcomes, (ii) higher costs and worse outcomes, (iii) lower costs and better outcomes, or (iv) higher costs and better outcomes. Cost-effectiveness acceptability curves were used to indicate the probability that CCBT or CBT was the most cost-effective option for different values placed on a unit improvement in outcome, i.e., one extra QALY.
RESULTS
As reported elsewhere in detail,(21) there were 154 patients in the intent-to-treat (ITT) sample (n=77 per group). Participants’ mean age was 45, two thirds were female, three quarters were white, and about 50% had attended at least some years of college; there were no significant between-group differences at baseline. Acute phase completion rates were 79.2% for CBT (16.0[5.0] sessions; 13.3 hours therapist contact) and 81.8% for CCBT (8.1 [2.1] GDA modules; 11.0[3.0] therapy sessions; 5.0 hours therapist contact). CCBT met a priori criteria for noninferiority to CBT. In the ITT sample, for example, the CBT group had a mean HAMD score of 9.2 (sd=6.3; 95% CI 7.6–10.8) at week 16 or endpoint, whereas the CCBT group had a mean HAMD score of 8.9 (sd=5.6; 95% CI 7.5–10.3). Remission rates also were almost identical (CBT: 41.6; CCBT: 42.9%). Improvements were sustained at the three and six month post-treatment follow-ups; fewer than 10% of remitters relapsed.
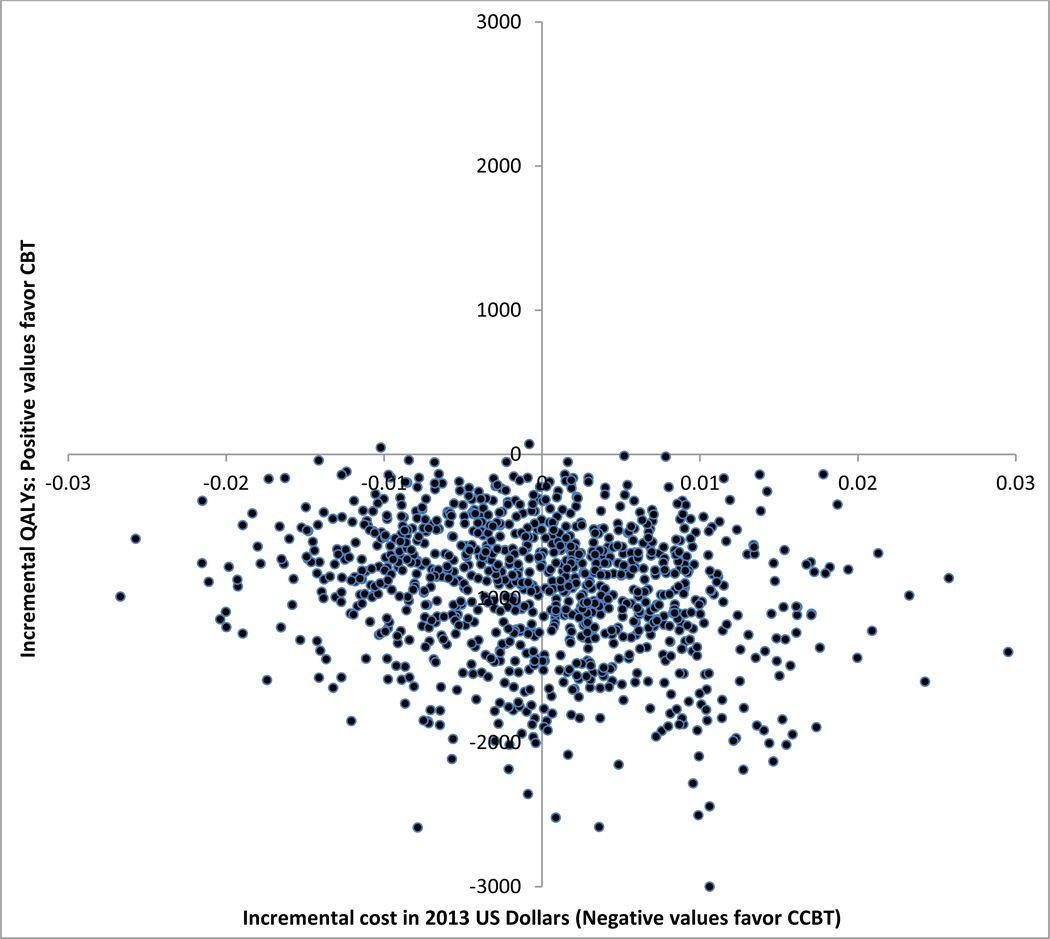
Service use and cost data in the 6 months prior to intake are summarized in Tables 1 and 2. Although total service use costs were slightly higher for the CCBT group, the difference was not significant because of substantial variability. About half of each group saw their primary care providers; most of other services were seldom. At follow-up, these findings were largely unchanged, and therapy assignment did not affect subsequent service utilization (see Table 1). The total cost of care was significantly higher for CBT ($2,166) than CCBT ($1,247) (mean difference adjusted for baseline: $945; 95% CI: $200 to $1,925; see Table 2). Mean QALYs over the follow-up were almost identical (CBT: 0.3412; CCBT: 0.3415). Adjusting for baseline quality of life and site resulted in 0.0007 more QALYs for CCBT (95% CI, −0.0141 to 0.0164). The cost-effectiveness plane demonstrated a 99.7% likelihood that CCBT resulted in lower cost than CBT (see Figure 1). Within the two quadrants representing simulations in which CCBT was significantly less costly, outcomes were almost evenly distributed: there was a 53.7% likelihood CCBT resulted in greater QALYs than CBT and a 45.8% likelihood of fewer QALYs than CBT (see Figure 1). At a threshold of $50,000 per QALY, there was a 96% likelihood that CCBT was the more cost- effective option (Figure available upon request to MET).
Table 1.
Use of services at baseline and 6-month follow-up.
| Number (%) using service | Mean (sd) contacts by those using service | |||||||
|---|---|---|---|---|---|---|---|---|
| Baseline | 6-month follow-up | Baseline | 6-month follow-up | |||||
| Service | CBT | cCBT | CBT | cCBT | CBT | cCBT | CBT | cCBT |
| Cognitive behavior Therapy | 0 (0) | 0 (0) | 58 (100) | 57 (100) | - | - | 17.2 (2.8) | 11.7 (1.1) |
| Primary Care Physician | 39 (51) | 42 (55) | 28 (48) | 27 (47) | 1.6 (0.8) | 2.5 (3.8) | 1.5 (0.6) | 1.2 (0.4) |
| Psychiatrist | 9 (12) | 6 (8) | 4 (7) | 4 (7) | 2.1 (0.9) | 2.3 (1.9) | 1.7 (0.6) | 2.0 (0.8) |
| Other doctor | 33 (43) | 41 (53) | 23 (40) | 27 (47) | 3.8 (4.7) | 4.9 (8.7) | 1.7 (0.9) | 2.2 (2.3) |
| Emergency room | 11 (14) | 13 (17) | 6 (10) | 9 (16) | 1.0 (0.0) | 1.1 (0.3) | 1.2 (0.4) | 1.1 (0.3) |
| Practice nurse | 9 (12) | 11 (14) | 4 (7) | 2 (4) | 1.3 (0.7) | 1.2 (0.4) | 1.3 (0.5) | 2.0 (1.4) |
| District nurse | 2 (3) | 0 (0) | 0 (0) | 0 (0) | 1.5 (0.7) | - | - | - |
| Other nurse | 2 (3) | 1 (1) | 1 (2) | 0 (0) | 1.5 (0.7) | 1.0 (−) | 20.0 (−) | - |
| Health visitor | 0 (0) | 0 (0) | 1 (2) | 1 (2) | - | - | 20.0 (−) | 6.0 (−) |
| Psychologist | 7 (9) | 5 (7) | 4 (7) | 2 (4) | 10.8 (18.3) | 7.8 (10.0) | 4.7 (1.2) | 2.0 (−) |
| Counselor | 6 (8) | 9 (12) | 4 (7) | 2 (4) | 6.3 (4.0) | 3.8 (2.9) | 2.7 (1.5) | 1.5 (0.7) |
| Other therapist | 5 (7) | 7 (9) | 4 (7) | 2 (4) | 5.4 (2.9) | 3.3 (2.1) | 6.8 (8.9) | 7.5 (6.4) |
| Alternative medicine | 12 (16) | 7 (9) | 6 (10) | 3 (4) | 6.1 (7.1) | 7.4 (7.7) | 5.3 (7.3) | 2.3 (2.3) |
| Occupational therapist | 3 (4) | 0 (0) | 1 (2) | 0 (0) | 6.3 (3.5) | - | 1.0 (−) | - |
| Social worker | 4 (5) | 5 (7) | 2 (3) | 1 (2) | 2.8 (1.7) | 6.2 (7.9) | 2.5 (2.1) | 1.0 (−) |
| Homecare worker | 0 (0) | 0 (0) | 1 (2) | 1 (2) | - | - | 20.0 (−) | 4.0 (−) |
| House work | 0 (0) | 0 (0) | 0 (0) | 0 (0) | - | - | - | - |
| Volunteer | 3 (4) | 6 (8) | 1 (2) | 2 (4) | 1.3 (0.6) | 3.5 (4.2) | 2.0 (−) | 24.5 (33.2) |
| Inpatient (days) | 2 (3) | 2 (3) | 4 (7) | 4 (7) | 2.3 (0.4) | 0.8 (0.4) | 6.8 (9.5) | 3.5 (2.5) |
Table 2.
Mean (sd) Service Costs at Baseline and Follow-up (2013 US dollars).
| Baseline | 6-Month Follow-Up | |||
|---|---|---|---|---|
| Service | CBT | CCBT | CBT | CCBT |
| Cognitive Behavior Therapy | 0 (0) | 0 (0) | 1232 (203) | 555 (39) |
| Primary Care Physician | 105 (125) | 175 (394) | 94 (114) | 73 (85) |
| Psychiatrist | 41 (123) | 30 (130) | 20 (76) | 23 (90) |
| Other doctor | 267 (590) | 430 (1111) | 114 (167) | 170 (316) |
| Emergency room | 102 (252) | 130 (301) | 86 (270) | 125 (306) |
| Nurse | 23 (57) | 18 (44) | 76 (512) | 17 (87) |
| Psychologist | 62 (360) | 40 (223) | 25 (95) | 9 (50) |
| Counsellor | 42 (171) | 38 (132) | 14 (60) | 3 (23) |
| Other therapist | 20 (118) | 28 (103) | 44 (260) | 21 (155) |
| Alternative medicine | 63 (231) | 45 (202) | 36 (180) | 8 (45) |
| Occupational therapist | 24 (132) | 0 (0) | 2 (13) | 0 (0) |
| Social worker | 4 (18) | 5 (20) | 3 (15) | 3 (15) |
| Homecare worker | 0 (0) | 0 (0) | 28 (215) | 6 (43) |
| Volunteer | 1 (3) | 2 (14) | <1 (1) | 26 (196) |
| Inpatient | 49 (307) | 16 (107) | 394 (2356) | 208 (908) |
| Total cost | $778 (958) | $957 (1332) | $2164 (3465) | $1247 (1423)* |
Adjusting for baseline costs, the mean difference at follow-up was $945 favoring CCBT (bootstrapped 95% CI, $202 to $2123)
Figure 1.
The Cost-Effectiveness Plane is constructed from a bootstrapping analysis based on 1000 simulations of the associations of cost data and QALYs for depressed people randomly assigned to 16 weeks of treatment with either CBT or CCBT. The virtual absence of data points in the upper two quadrants reflects the certainty that CCBT is less costly than CBT. The nearly even distribution of data points in the lower two quadrants reflects the near equivalent efficacy of CBT and CCBT.
DISCUSSION
Several methods of CCBT have been introduced to improve access to this effective form of psychotherapy of depression. Collectively, these therapies promise to reduce cost, enhance the convenience of treatment, allow for fully remote delivery, and maximize the impact of a limited number of trained therapists.(34) In parallel with these clinical developments, there has been substantial growth in research on CCBT for depression. One recent meta-analysis identified 40 RCTs from a wide range of countries.(35) Because all forms of CCBT use of less therapeutic support than conventional psychotherapy, it is has been assumed that CCBT is a cost-effective strategy.(10,19,34,35) However, only a small number of earlier studies included the components necessary to assess cost-effectiveness in comparison to standard, first-line interventions (i.e., randomization to a credible, active comparison group and a detailed assessment of service utilization, costs and lost economic potential).(36–41) Keeping in mind these limitations, results of a meta-analysis of the earlier RCTs suggested that CCBT may more cost-effective than standard CBT.(42)
The findings of the current report provide the strongest evidence of cost-effectiveness of CCBT to date. Not only did we find that the clinical benefits of a 16-week course of treatment with the GDA model of CCBT were noninferior to those of a relatively intensive course of individual CBT,(21) such therapeutic equivalence was achieved with a cost savings of $945 per patient. One practical implication of the reduced use of therapist time is that nearly three times as many depressed people could be treated without any loss of clinical benefit if this approach was routinely used instead of conventional CBT as a first-line therapy.
The current study has several limitations.(21) Our therapists were highly experienced with conventional CBT and most learned to use GDA in order to participate in this study. As such, it is not known if less experienced or more eclectically oriented therapists could achieve comparable results. Conversely, it is possible that nondoctoral therapists or counselors could be trained to deliver CCBT, which could result in an even greater increase in cost-effectiveness.
A second limitation is that the “dose” of therapist time – up to 5.5 hours across 16 weeks – is larger than used in most other investigations of CCBT. Because results of several meta-analyses suggest that as little as 1–3 hours of therapist support may be sufficient to facilitate CCBT in some settings,(18,19,35) the cost-effectiveness of GDA could be further increased by a judicious reduction in therapist time. The importance of therapist support for treatment in clinical populations should not be minimized, however, as one large primary care study(43) that offered only a small amount (less than 10 minutes on average) of technical support found no clinical advantage compared to usual care.
At a time in which remote or “at home” access to therapy is urgently needed,(34) a third limitation of our study is that therapeutic support was provided face-to-face. The web-based platform of the current edition of GDA is well suited to range of remote applications and, since completing this study, our groups have gained extensive experience using telephone and videoconferencing. In our experience, both of these forms of support are judged to be useful by therapists and highly acceptable by depressed patients.(44) Other investigators have reported successful use of email or chat room support for delivery of CCBT.(35) Although videoconferencing has not yet been researched extensively, we predict this method will be at least as effective as providing therapeutic support by telephone —a method with established efficacy for CBT.(45–47)
Although the emphasis of this component of our research was on the cost-effectiveness of CCBT for depression, the impact of the COVID-19 pandemic underscores the potential public health significance of broader dissemination of modes of therapy for both depressive and anxiety disorders that do not require the patient and therapist to be in the same room.(34) Both voluntary quarantines and mandated social distancing policies preclude all forms of conventional psychotherapy at the very time that our anxious and depressed patients’ worries and isolation may warrant even greater therapeutic support. In this regard, the availability of a range of programs that reliably deliver proven therapies at low cost has potentially great public health significance. Given the rapid progress in information technology and the growing sophistication of web-based therapeutic applications, there is good reason for optimism that even more efficient, accessible, and affordable therapies will be increasingly available to address common psychiatric conditions.
Acknowledgements
This research was supported by grants R01-MH082762 (JHW) and R01-MH082794 (MET) from the National Institute of Mental Health. The authors wish to express their appreciation to the therapists for this study (Louisville: Don Kris Small, Ph.D., Virginia Evans, L.C.S.W., Mary Hosey, L.C.S.W., and Thomas Heddon, L.C.S.W.; Philadelphia: Elizabeth Hembree, Ph.D., Kevin Kuehlwein, Psy.D., J. Russell Ramsay, Ph.D., and Rita Ryan, Ph.D.). At the Philadelphia site, one of the authors (MET) treated two patients during a staff shortage. We thank Kitty de Voogd, Jordan Coella, Christine Johnson and Carol Wahl for their assistance. Andrew S. Wright, M.D., and Aaron T. Beck, M.D. coauthored the prototype for the GDA program along with one of the researchers (JHW). Eve Phillips, M.B.A., provided support for the GDA software.
Footnotes
Disclosure Statement
Dr. Thase reports the following other relationships during the past three years. He has been an advisory/consultant to: Acadia, Akili Inc., Alkermes, Allergan (Activis, Naurex), BioHaven, Boerhinger-Ingleheim, Calla Pharmaceuticals, Clexio Pharmaceuticals, GenoMind, Johnson & Johnson (Janssen, Ortho-McNeil), Lundbeck, Otsuka, Pfizer, Sunovion, and Takeda. He received grant support from the Agency for Healthcare Research and Quality, Alkermes, Allergan (Forest Pharmaceuticals), Assurex, Axsome, BioHaven, Intracellular Therapeutics, Johnson & Johnson (Janssen), Otsuka Pharmaceuticals, and Takeda. Dr. Thase received royalties from the American Psychiatric Press, Guilford Publications, Herald House and W.W. Norton & Company, Inc. Dr. Thase’s spouse, Dr. Diane Sloan, works for Peloton Advantage, which does business with a number of pharmaceutical companies. None of other authors at the Penn and University of Pittsburgh sites report disclosures or conflict of interest. Neither the Penn authors nor the University of Pennsylvania have any financial relationship with Empower Interactive or Mindstreet.
Dr. Jesse Wright is an author of Good Days Ahead (GDA) and has an equity interest in Empower Interactive and Mindstreet, developers and distributors of GDA. He receives no royalties or other payments from sales of this program. His conflict of interest is managed by an agreement with the University of Louisville. All other authors have no disclosures or conflict of interest regarding GDA and no other disclosures pertaining to this research.
REFERENCES
- 1.American Psychiatric Association. Practice guideline for the treatment of patients with major depressive disorder, Third edition, Arlington, VA: [http://www.guideline.gov/content.aspx?id=24158] (Accessed 11/27/16). [Google Scholar]
- 2.Parikh SV, Quilty LC, Ravitz P, et al. Canadian Network for Mood and Anxiety Treatments (CANMAT) 2016 Clinical Guidelines for the Management of Adults with Major Depressive Disorder: Section 2. Psychological Treatments. Can J Psychiatry. 2016;61(9):524–539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cuijpers P, Berking M, Andersson G, Quigley L, Kleiboer A, Dobson KS. A meta-analysis of cognitive- behavioural therapy for adult depression, alone and in comparison with other treatments. Can J Psychiatry. 2013;58(7):376–385. [DOI] [PubMed] [Google Scholar]
- 4.Cuijpers P, van Straten A, van Oppen P, Andersson G. Are psychological and pharmacologic interventions equally effective in the treatment of adult depressive disorders? A meta-analysis of comparative studies. J Clin Psychiatry. 2008;69(11):1675–1685. [DOI] [PubMed] [Google Scholar]
- 5.Weitz ES, Hollon SD, Twisk J, et al. Baseline Depression Severity as Moderator of Depression Outcomes Between Cognitive Behavioral Therapy vs Pharmacotherapy: An Individual Patient Data Meta- analysis. JAMA Psychiatry. 2015;72(11):1102–1109. [DOI] [PubMed] [Google Scholar]
- 6.Vittengl JR, Clark LA, Dunn TW, Jarrett RB. Reducing relapse and recurrence in unipolar depression: a comparative meta-analysis of cognitive-behavioral therapy’s effects. J Consult Clin Psychol. 2007; 75(3): 475–488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Biesheuvel-Leliefeld KE, Kok GD, Bockting CL, et al. Effectiveness of psychological interventions in preventing recurrence of depressive disorder: meta-analysis and meta- regression. J Affect Disord. 2015;174:400–410. [DOI] [PubMed] [Google Scholar]
- 8.Marcus SC, Olfson. National trends in the treatment for depression from 1998 to 2007. Arch Gen Psychiatry. 2010;67(12):1265–1273. [DOI] [PubMed] [Google Scholar]
- 9.Blane D, Williams C, Morrison J, Wilson A, Mercer S. Cognitive behavioural therapy: why primary care should have it all. Br J Gen Pract. 2013; 63(607):103–104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Eells TD, Barrett MS, Wright JH, Thase ME. Computer-assisted cognitive-behavior therapy for depression. Psychotherapy. 2014;51(2):191–197. [DOI] [PubMed] [Google Scholar]
- 11.Griest JH. Computer interviews for depression management. J Clin Psychiatry. 1998;59 (suppl 16): 20–42. [PubMed] [Google Scholar]
- 12.Wright JH, Wright A. Computer assisted psychotherapy. J Psychother Pract Res. 1997;6(4):315–329. [PMC free article] [PubMed] [Google Scholar]
- 13.Beating the Blues US – Helping you to manage your emotional well-being. http://beatingthebluesus.com/ (Accessed 11/27/16).
- 14.MoodGYM training program. https://moodgym.anu.edu.au/welcome (Accessed 11/27/16).
- 15.Empower Interactive. Good Days Ahead. http://www.empower-interactive.com/solutions/good-days-ahead/ (Accessed 11/27/16).
- 16.Richards D, Richardson T. Computer-based psychological treatments for depression: a systematic review and meta-analysis. Clin Psychol Rev. 2012;32(4):329–342. [DOI] [PubMed] [Google Scholar]
- 17.Arnberg FK, Linton SJ, Hultcrantz M, Heintz E, Jonsson U. Internet-delivered psychological treatments for mood and anxiety disorders: a systematic review of their efficacy, safety, and cost- effectiveness. PLoS One. 2014;9(5):e98118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.So M, Yamaguchi S, Hashimoto S, et al. Is computerized CBT really helpful for adult depression? A meta-analytic re-evaluation of CCBT for adult depression in terms of clinical implementation and methodological validity. BMC Psychiatry. 2013;13:113. doi: 10.1186/1471-244X-13-113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Andersson G, Topooco N, Havik O, Nordgreen T. Internet-supported versus face-to-face cognitive behavior therapy for depression. Expert Rev Neurother. 2016;16(1):55–60. [DOI] [PubMed] [Google Scholar]
- 20.Wright JH, Wright AS, Albano AM, et al. Computer-assisted cognitive therapy for depression: maintaining efficacy while reducing therapist time. Am J Psychiatry. 2005;162(6):1158–1164. [DOI] [PubMed] [Google Scholar]
- 21.Thase ME, Wright JH, Eells TD, Barrett MS, Wisniewski SR, Balasubramani GK, et al. Improving the Efficiency of Psychotherapy for Depression: Computer-Assisted Versus Standard CBT. Am J Psychiatry. 2018;175(3):242–250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.First MB, Spitzer RL, Gibbon M, Williams JW. Structured Clinical Interview for DSM-5 Axis I Disorders, Research Version, Patient/Non-patient Edition (SCID-I/P w/PSY SCREEN). New York: Biometrics Research, New York State Psychiatric Institute, 2015. [Google Scholar]
- 23.Hamilton M A rating scale for depression. J Neurol Neurosurg Psychiatry. 1960; 23: 56–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Beck AT, Rush AJ, Shaw BF, et al. Cognitive Therapy of Depression. New York, Guilford, 1979. [Google Scholar]
- 25.Beck J Cognitive Therapy: Basics and Beyond. Vol 2 New York, Guilford, 2011. [Google Scholar]
- 26.Wright JH, Brown GK, Thase ME, Basco MR. Learning Cognitive-Behavior Therapy: An Illustrated Guide – Second Edition. Arlington, VA: American Psychiatric Publishing, Inc, 2017. [Google Scholar]
- 27.Thase ME, Simons AD, Cahalane J, McGeary J, Harden T. Severity of depression and response to cognitive behavior therapy. Am J Psychiatry. 1991;148(6):784–789. [DOI] [PubMed] [Google Scholar]
- 28.Thase ME, Reynolds CF III, Frank E, et al. Response to cognitive behavior therapy in chronic depression. J Psychother Pract Res. 1994;3:204–214. [Google Scholar]
- 29.McCrone P, Knapp M, Proudfoot J, Ryden C, Cavanaugh K, Shapiro D, et al. Cost-effectiveness of computerized cognitive-behavioral therapy for anxiety and depression in primary care: randomized controlled trial. Brit J Psychiatry. 2004;185:55–62. [DOI] [PubMed] [Google Scholar]
- 30.McCrone P, Sharpe M, Chalder T, et al. Adaptive pacing, cognitive behaviour therapy, graded exercise, and specialist medical care for chronic fatigue syndrome: A cost- effectiveness analysis. PLoS ONE. 2012;7(8):e40808, doi: 10.1371/journal.pone.0040808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Beecham J, Knapp M. Costing Psychiatric Interventions. In Thornicroft G, Brewin CR, and Wing J (Eds.) Measuring Mental Health Needs 2001;(pp 163–183) London: Gaskell/Royal College of Psychiatrists. [Google Scholar]
- 32.Pyne JM, Sieber WJ, David K, Kaplan RM, Rapaport MH, Keith Williams D. Use of the quality of well- being self-administered version (QWB-SA) in assessing health-related quality of life in depressed patients. J Affect Disord. 2003;76(1–3):237–247. [DOI] [PubMed] [Google Scholar]
- 33.Thompson SG, Barber JA. How should cost data in pragmatic randomised trials be analysed? Brit Med Jour. 2000;320(7243):1197–1200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Wright JH, Caudill R. Remote Treatment Delivery in Response to the COVID-19 Pandemic. Psychotherapy and Psychosomatics. ePublished March 26, 2020; 10.1159/000507376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Wright JH, Owen JJ, Eells TD, Richards D, Richardson T, Brown GK, et al. Computer-assisted Cognitive-Behavior Therapy for Depression: A systematic review and meta-analysis. J Clin Psychiatry. 2019; doi: 10.4088/JCP.18r12188,80(2):18r12188. [DOI] [PubMed] [Google Scholar]
- 36.Gerhards SAH, de Graaf LE, Jacobs LE, Severens JL, Huibers MJH, Arntz A, et al. Economic evaluation of online computerized cognitive-behavioural therapy without support for depression in primary care: randomised trial. Brit Jour Psychiatry. 2010; 196(4):310–318. [DOI] [PubMed] [Google Scholar]
- 37.Hollingshurst S, Peters TJ, Kaur S, Wiles N, Lewis G, Kessler D. Cost-effectiveness of therapist- delivered online cognitive-behavioural therapy for depression: randomised controlled trial. Brit Jour Psychiatry. 2010;197(4):297–304. [DOI] [PubMed] [Google Scholar]
- 38.Titov N, Dear BF, Ali S, Zou JB, Lorian CN, Johnston L, et al. Clinical and cost-effectiveness of therapist-guided internet-delivered cognitive behavior therapy for older adults with symptoms of depression: A randomized controlled trial. Behav Ther. 2015;46(2): 193–205. [DOI] [PubMed] [Google Scholar]
- 39.Warmerdam L, Smit F, van Straten A, Riper H, Cuijpers P. Cost-Utility and Cost-Effectiveness of Internet-Based Treatment for Adults with Depressive Symptoms: Randomized Trial. Jour Med Internet Res. 2010;12(5):e53. doi: 10.2196/jmir.1436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Solomon D, Proudfoot J, Clarke J, and Christensen H. e-CBT (myCompass), Antidepressant Medication, and Face-to-Face Psychological Treatment for Depression in Australia: A Cost-Effectiveness Comparison. Jour Med Internet Res. 2015;17(11):e255, doi: 10.2196/jmir.4207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Holst A, Bjorkelund C, Metsini A, Madsen J-H, Hange D, Petersson E-L L, et al. Cost-effectiveness analysis of internet-mediated cognitive behavioural therapy for depression in the primary care setting: results based on a controlled trial. Brit Med Jour. 2018;8(6):e019716, doi: 10.1136/bmjopen-2017-019716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kolovos S, van Dongen JM, Riper H, Buntrock C, Cuijpers P, Ebert DD, et al. Cost-effectiveness of guided Internet-based interventions for depression in comparison with control conditions: An individual- participant data meta-analysis. Depress Anxiety. 2018. March;35(3):209–219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Duarte A, Walker S, Littlewood E, Brabyn S, Hewitt C, Gilbody S, et al. Cost-effectiveness of computerized cognitive-behavioural therapy for the treatment of depression in primary care: findings from the randomised evaluation of the effectiveness and acceptability of computerised therapy. Psychol Med. 2017;47(10):1825–1835. [DOI] [PubMed] [Google Scholar]
- 44.Antle BF, Owen JJ, Eells TD, Wells MJ, Harris LM, Cappiccie A, et al. Dissemination of computer-assisted cognitive-behavior therapy for depression in primary care. Contemp Clin Trials. 2019; 78:46–52. [DOI] [PubMed] [Google Scholar]
- 45.Mohr DC, Hart SL, Julian L, Catledge C, Honos-Webb L, Vella L, et al. Telephone-administered psychotherapy for depression. Arch Gen Psychiatry. 2005. September;62(9):1007–14 [DOI] [PubMed] [Google Scholar]
- 46.Mohr DC, Ho J, Duffecy J, Reifler D, Sokol L, Burns MN, et al. Effect of telephone-administered vs face-to-face cognitive behavioral therapy on adherence to therapy and depression outcomes among primary care patients: a randomized trial. JAMA. 2012. June 6;307(21):2278–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Mohr DC, Lattie EG, Tomasino KN, Kwasny MJ, Kaiser SM, Gray EL, et al. A randomized noninferiority trial evaluating remotely-delivered stepped care for depression using internet cognitive behavioral therapy (CBT) and telephone CBT. Behav Res Ther. 2019;123:103485. doi: 10.1016/j.brat.2019.103485 [DOI] [PMC free article] [PubMed] [Google Scholar]