Abstract
Objective
To assess the proportion of individuals who report dizziness and/or vertigo during the prodromal phase or headache phase of migraine.
Methods
The databases of MEDLINE and EMBASE were searched for studies on dizziness and/or vertigo during the prodromal phase or headache phase of migraine. Pooled relative frequencies were estimated using a random-effects meta-analysis.
Results
We identified 9 articles eligible for inclusion. Of these, one study reported results for the prodromal phase, seven studies for the headache phase and one study for both the prodromal- and headache phase. In the prodromal phase, 9.0% of individuals with migraine reported dizziness, while 3.3% reported vertigo. During the headache phase, relative frequency of dizziness ranged from 6.7% to 59.6%, while vertigo ranged from 6.4% to 44.7%. The meta-analysis showed a relative frequency of 35.7% for dizziness (95% CI = 13.7–61.5%, I2=99%) and 33.9% for vertigo (95% CI = 26.7–41.5%, I2=87%). Study quality was rated 5/9 or below for 7 studies and 6/9 or above for 2 studies.
Conclusion
We found that there is a scarcity of literature on dizziness and vertigo as prodromal- and headache-associated symptoms in individuals with migraine. Methodological variations confound comparisons of epidemiological patterns, although it appears that dizziness and vertigo are more frequent during the headache phase of migraine, compared with prodromal phase. Future studies should ensure use of standardized definitions and rigorous methodology to enable accurate measurements of dizziness and vertigo in migraine.
Keywords: Epidemiology, Vestibular Symptoms, Associated Symptoms, Vestibular Migraine, Classification
Introduction
The association between vestibular symptoms and migraine has been well-established(1). This recently led the International Headache Society and the International Society for Neuro-Otology (Bárány Society) to propose research criteria for vestibular migraine(2). In one clinic-based study, 10% of individuals with migraine fulfilled the research criteria for vestibular migraine(3). Interestingly, another clinic-based study found that 72% of individuals with migraine reported dizziness as an associated symptom to their migraine attack (4). Thus, the current research criteria may be too restrictive and thereby unable to ascertain the full scope of dizziness and vertigo symptoms in migraine. An understanding of the symptoms appearing in the prodromal phase and headache phase of migraine can provide clues about the pathophysiologic chain of events involved in the migraine attack. For migraine patients with vestibular symptoms, the vestibular symptom is of particular interest. Therefore, we decided to perform a systematic review and meta-analysis to assess the prevalence of individuals with migraine experiencing dizziness and/or vertigo in the prodromal phase and headache phase of migraine.
Methods
Data Sources
No protocol was registered for this study. We searched MEDLINE and Embase databases for articles on the relative frequency of vertigo and/or dizziness in individuals with migraine. The first database search was performed on January 24th, 2019 with the following search string and no restrictions in terms of date of publication: migraine AND (vertigo OR dizziness OR lightheadedness OR disequilibrium OR presyncope). A second search was performed on April 17th, 2019 with the following search string and no restrictions in terms of date of publication: migraine AND (premonitory OR pre monitory OR pre-monitory) AND (symptom OR symptoms).
Study selection
The database searches were limited to articles on human subjects that were published in English. In addition, we reviewed the reference lists of relevant primary articles and reviews to identify studies that were missed in the search process. All eligible studies were screened in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) reporting guidelines. The full eligibility criteria are presented in Supplemental Figure 1. In brief, we included original, observational studies with a case-control or cohort design, including study participants meeting the International Classification of Headache Disorders(ICHD) two-digit diagnostic criteria for migraine without aura, migraine with aura or chronic migraine. To be eligible, studies were required to report the number or proportion of study participants reporting dizziness and/or vertigo during the prodromal phase and/or headache phase of migraine. Prodromal symptoms were defined as features that preceded a migraine headache by up to 48 hours(5) while associated symptoms were defined as features that occurred concurrently with the headache phase of a migraine attack. It was a requirement that results for “dizziness” or “vertigo” were reported separately. Studies solely reporting the pooled numbers of patients experiencing “dizziness/vertigo” were thus excluded. Studies were only considered eligible when they included a sample of individuals with migraine whose study participation was solely based on a two-digit diagnosis of migraine in accordance with any version of the ICHD(5–8). Consequently, we excluded studies in which a diagnosis of specific migraine subtypes was an inclusion criterion. Migraine subtypes were here defined as a migraine diagnosis at the three-digit level or more specific, e.g. 1.2.3 Hemiplegic migraine or A1.6.6 Vestibular migraine. If studies with overlapping populations were encountered, the study published first would be included and the other discarded.
Study Inclusion and Data Extraction
One investigator (B.C.) screened all articles by title and abstract. This step was then duplicated by the same investigator (B.C.) who subsequently performed a full-text screening to determine which articles should be included. Following this, another investigator (A.I.) reassessed all included articles and a random sample of excluded articles. Final inclusion was decided by consensus between the two investigators (B.C. and A.I.). If consensus was not reached, two independent investigators (H.A. and S.A.) were available to provide advice and resolve any disagreement. For each study, two investigators (B.C. and A.I.) independently extracted data on the following variables: study design, age, gender, total number of subjects with migraine (including if reported any subtypes), definition and terminology used for dizziness or vertigo number of subjects with migraine who reported dizziness or vertigo and the natural course of the symptom of dizziness or vertigo. Study quality was assessed with a modified version of the Newcastle-Ottawa Scale (NOS) for assessing study quality in non-randomized studies(9). The tool assesses three domains: selection (four items), comparability (two items) and exposure (three items). A total of nine points are awarded, with higher sum scores reflecting superior study quality.
Statistical Analysis
The outcomes of interest were the relative frequencies of “dizziness” or “vertigo” in random samples of individuals with migraine. Meta-analysis was performed whenever three or more studies were available, in which case all subjects were pooled across migraine without aura, migraine with aura and chronic migraine. Pooled relative frequency estimates were calculated by pooling study-specific estimates using a random-effects meta-analyses that accounts for heterogeneity among studies and weighting based on sample size. The I2 statistic was used to assess between-study heterogeneity, with values ≥ 75% indicating considerable heterogeneity. Freeman-Tukey transformation (arcsine square root transformation) was used to calculate the weighted pooled relative frequency estimates. Sources of study heterogeneity can be explored through subgroup analysis and meta-regression. Both methods require a substantial number of studies(10), with a recommendation of at least ten studies for each modelled characteristic(10). As we did not include enough studies to meet the recommendations, subgroup analysis and meta-regression was not performed. Statistical analysis was performed with R version 3.6.0 with the “meta” and “metafor” packages.
Results
The first database search yielded 6,659 hits. Furthermore, one additional article was identified through other sources. After removal of duplicates, 5,667 articles were screened by title and abstract, of which 194 articles were retrieved. Of these, 184 did not meet the inclusion or exclusion criteria outlined in supplemental figure 1 and were thus excluded. Eight articles met the eligibility criteria and were included in the qualitative synthesis (Supplemental Figure 2)(11–18). The second search yielded 266 search hits. Following removal of duplicates, 190 titles and abstracts were screened. Twenty-three articles were retrieved and assessed in full. Of these, 21 did not meet the eligibility criteria and were subsequently excluded Two relevant articles were identified (Supplemental Figure 2)(18,19). However, one of these was also included in the first search(18). Thus, we collectively included nine articles in the present review. One article reported data on the prodromal phase of migraine(19), seven articles reported data for the headache-phase of migraine(11–17), and one article reported data for both the prodromal phase and headache phase of migraine(18). Study quality was rated to 0/9 for one study (17), 1/9 for two studies (8,19), 2/9 for two studies (12,13), 3/9 for two studies (16,18), 6/9 for one study (14) and 7/9 for one study (11).
Vertigo and Dizziness as Prodromal Symptoms of Migraine
Two clinic-based, observational studies investigated vertigo or dizziness symptoms as a prodromal feature of migraine (Table 1). One study assessed “dizziness”(19) while the other study assessed “vertigo”(18). In both studies, assessment of prodromal symptoms was a primary endpoint(18,19).
Table 1.
Individual-Level Study Characteristics for Studies on Premonitory Symptoms
| First Author, Publication Year | Study Type | Term for Vestibular Symptom | Clinical Description | Female/Male (%) | Headache Classification | Number of Subjects (n) | Subjects with Vestibular Symtom, n (%) | MA, MO, n (%) | MA/MO with Vestibular Symptom, n (%) | NOS Score |
|---|---|---|---|---|---|---|---|---|---|---|
| Lampl, 2019 | Clinic-based | Vertigo | Spontaneous attacks of vertigo not explained by either central or otological abnormalities, that did not lead to permanent deficits | 73%/27% | ICHD-3-β | 487 | 16 (3.3%) | *** | *** | 3 |
| Santoro, 1990 | Clinic-based | Dizziness | Not defined | 76%/24% | ICHD-1 | 100 | 9 (9%) | 0 (0%), 100 (100%) | 0 (0%), 9 (9%) | 1 |
Discrepancy between Table 1 and text in results section, and Figure 1: Table 1 shows that 16/487 patients experience vertigo as premonitory symptom. Figure 1 presents the results stratified by migraine subtype and shows that 7/375 patients with MO and 2/112 patients with MA experience vertigo as a premonitory symptoms.
Abbreviations: ICHD: International Classification of Headache Disorders; MA: Migraine with aura; MO: Migraine without aura; NOS: Newcastle-Ottawa Scale.
In an observational cohort study(19), prodromal symptoms were assessed prospectively in 100 patients with migraine without aura using a headache diary. Dizziness was found to be a prodromal symptom in 9% of the migraine patients. The other study investigated prodroal symptoms in 487 patients who had either migraine without aura (MO) or migraine with aura (MA) (18). Prodromal symptoms were assessed by instructing patients to fill out a self-administered questionnaire immediately after their next migraine attack. Episodic vertigo was reported to be a prodromal symptom in 3.3% of the overall sample. In terms of methodology, none of the studies provided a clinical description of vertigo/dizziness. None of the three studies reported on duration or frequency of vertigo/dizziness as a prodromal symptom of migraine. In addition, none of the studies included a control population.
Vertigo and Dizziness Symptoms as Headache Phase-Associated Symptoms in Migraine
Eight studies reported on vertigo or dizziness as associated symptoms to the headache phase of migraine (Table 2) (11–18). Of these, four studies were clinic-based(11,14,16,18), two studies were community-based(15,17), one study was population-based(12), and one study was a combined population-based survey with additional data from a clinic-based sample(13) (Table 2). Five studies reported outcome data for dizziness (11,13–16) and five studies reported outcome data for vertigo(11,12,14,17,18).
Table 2.
Individual-Level Study Characteristics for studies on associated symptoms
| First Author, Publication Year | Study Type | Clinical Description | Female/Male (%) | Headache Classification | Number of Subjects (n) | Subjects with Vestibular Symtom, n (%) | MA, MO, n (%) | MA/MO with Vestibular Symptom (%) | NOS score |
|---|---|---|---|---|---|---|---|---|---|
| Studies using the term “dizziness” | |||||||||
| Akdal, 2013 | Clinic-based | Sense of unsteadiness or imbalance | 88%/12% | ICHD-2 | 1880 | 7.0% | 320 (17%), 1560 (83%) | 14%/6% | 7 |
| Bisdorff, 2010 | Combined Clinic- and Population-based | Not defined | 83%/17% | ICHD-1 | 1271 | 59.6% | Not reported | Not reported | 2 |
| Carvalho, 2018 | Clinic-based | Disturbed spatial orientation | 100%/0% | ICHD-3-β | 180 | 6.7% | 60(33%), 60(33%)* | 6%/3% | 6 |
| Hsu, 2010 | Community-based | Not defined | 100%/0% | ICHD-2 | 238 | 47.9% | Not reported | Not reported | 1 |
| Kelman, 2006 | Clinic-based | Not defined | 86%/14% | ICHD-2 | 1009 | 36.3% | 363 (36%), 646 (64%) | Not reported | 3 |
60/180 patients were classified as chronic migraine. In the chronic migraine group, 11% experienced dizziness and 54% experienced vertigo as associated symptoms.
Discrepancy between Table 1 and text in results section, and Figure 1: Table 1 shows that 79/487 + 51/487 patients experience vertigo as an associated symptom. Figure 1 presents the results stratified by migraine subtype and shows that 65/375 + 48/375 patients with MO and 14/112 + 12/112 patients with MA experience vertigo as an associated symptom.
Abbreviations: ICHD: International Classification of Headache Disorders; MA: Migraine with aura; MO: Migraine without aura; NOS: Newcastle-Ottawa Scale.
Dizziness
The relative frequency of headache phase-associated dizziness in three clinic-based studies was 6.7% (n=180)(14), 7.0% (n=1.880)(11) and 36.3% (n=1.009)(16). All three studies reported on the proportion of MO and MA patients with dizziness (11,14,16). Two of three studies reported the relative frequency of dizziness stratified by migraine subtype. Both studies showed that dizziness was more prevalent among patients with MA compared to MO(11,14). One study reported that 14% of patients with MA compared to 6% of patients reported dizziness(11). The corresponding results were 6% for MA and 3% for MO in the other study(14). The latter study also included a subgroup of patients with chronic migraine, of which 11% reported dizziness as an associated symptom(14). One of three clinic-based studies compared migraine patients with controls suffering from non-migraine headache disorders(11). The study showed that 7.0% of patients with migraine experienced headache-associated dizziness compared to 1.3% of patients with tension-type headache (TTH)(11). Two studies defined dizziness(11,14), of which one study did so according to the International Classification of Vestibular Symptoms (ICVD)(14). None of studies reported the duration or natural course of dizziness as an associated symptom to migraine. None of the studies reported on the clinical characteristics of the headache during migraine with dizziness.
Two non-clinic based studies investigated the relative frequency of dizziness in patients with migraine(13,15). One community-based study among Taiwanese women found that 47.9% experienced headache-associated dizziness in a sample of 238 patients with migraine(15).The study did not define dizziness, compare the rates between MA and MO, or compare the relative frequency of dizziness in migraine to that of controls. One study pooled the responses from a population-based sample with responses from a clinic-based sample(13). The relative frequency of dizziness was 59.6% (n=1.271) (13). Dizziness was more frequent in females with migraine compared to males (61.7% vs. 49.4%), and more frequent in migraine vs. non-migraine headache (59.6% vs. 34.6%) (13).
Vertigo
The relative frequency of headache-associated vertigo in three clinic-based studies was 6.4% (n=1.880)(11), 44.7% (n=180)(14) and 26.7% (n=487)(18). All three studies reported on the proportion of patients with MA and MO(11,14,18). Two of the studies found that vertigo was more frequent as an associated symptom among patients with MA, with the following results: 12% vs. 6%(11) and 54% vs. 26%(14). The latter study also included a subgroup of patients with chronic migraine, of which 54% reported vertigo as an associated symptom(14). One of three clinic-based studies compared migraine patients with controls suffering from non-migraine headache disorders(11). The study showed that 6.4% of patients with migraine experienced headache-associated vertigo compared to 1.6% of patients with tension-type headache (TTH)(11). Two studies defined vertigo(11,14), of which one was made according to the ICVD(14). None of the studies reported the duration or natural course of vertigo. None of the studies reported on the clinical characteristics of the headache during migraine with vertigo.
Two non-clinic based studies investigated the relative frequency of headache-associated vertigo in patients with migraine(12,17). One community-based study among Indian medical students found that 30.0% experienced vertigo in association with their migraines (n=144)(17). The study did not define vertigo, compare the rates between MA and MO, or compare the relative frequency of vertigo in migraine to that of controls. One population-based study in Turkey found that 35.5% of migraine patients experience headache phase-associated vertigo (n=871)(12). Aura was more prevalent among patients with headache-associated vertigo compared to patients without vertigo. The study did not provide a clinical description of what was meant by “vertigo”, nor did the study compare the prevalence of headache-associated vertigo in migraine patients to non-migraine controls(12).
Meta-analysis
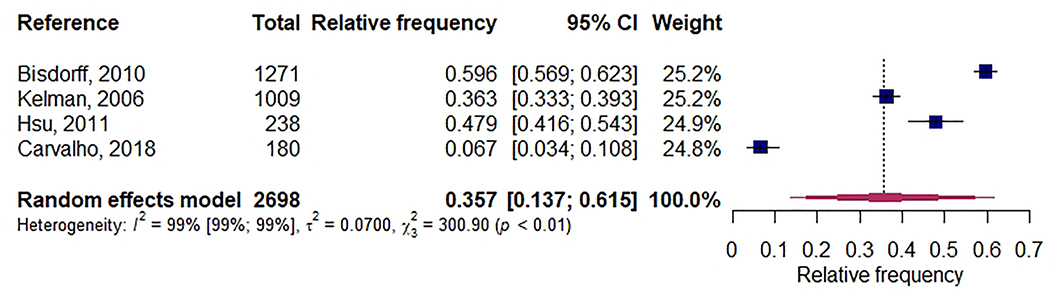
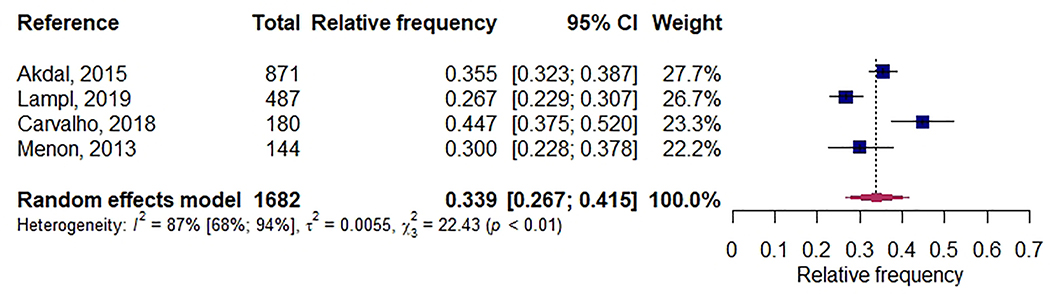
We included seven studies in the quantitative synthesis(12–18). One study required that the headache-associated dizziness/vertigo should have duration of minimum 60 minutes(11). We decided to exclude this study from the quantitative analysis because the definitions used in this research inappropriately skew the results. The remainder of the studies did not have time constraints on the duration of dizziness or vertigo. By pooling the results of 2.698 subjects from four studies, the relative frequency of headache phase-associated dizziness in patients with migraine was 35.7% (95% CI=13.7% to 61.5%, I2=99%, 95% CI= 99% to 99%)(13–16) (Figure 1). By pooling the results of 1.682 subjects from four studies, the relative frequency of headache-associated vertigo in patients with migraine was 33.9% (95% CI=26.7% to 41., I2=87%, 95% CI = 68% to 94%)(12,14,17,18) (Figure 2).
Figure 1.
Forest plot: “Dizziness” in Adult Patients with Migraine
Figure 2.
Forest plot: “Vertigo” in Adult Patients with Migraine
Discussion
To our knowledge, this is the first systematic review and meta-analysis to assess the proportion of individuals with migraine who report dizziness or vertigo during the prodromal phase and headache phase of the migraine attack. Two studies reported on vestibular symptoms during the prodromal phase, with relative frequencies at 3.3% and 9.0%, respectively. Eight studies reported on dizziness or vertigo during the headache phase, with relative frequencies ranging from 6.4% to 59.6%. By pooling the study specific estimates, we found that the pooled relative frequency was 35.7% for dizziness and 33.9% for vertigo. Both estimates were biased by considerable study heterogeneity.
Vestibular symptoms as prodromal symptoms of migraine attacks have previously been reported (20). In our review, we identified just two studies reporting the proportion migraine patients reporting vestibular symptoms in the prodromal phase of migraine(18,19). The variability in the rates reported in these studies could be due to methodological variations. First, prodromal symptoms were assessed retrospectively, which may introduce recall bias(21). Second, only one of the studies reported the frequency of migraine headaches with prodromal symptoms(19). In this study, 9% reported that at least 50% of migraines were preceded by dizziness(19). In comparison, another study including 97 individuals with migraine reported that 22.9% of migraine attacks were preceded by dizziness in this cohort(20). This study did not report number of participants reporting dizziness, and, therefore, it is not possible to compare whether dizziness is a specific prodrome for a limited subgroup of patients. Lastly, one of the studies provided a description of how “dizziness” or “vertigo” was described to the patients.
We found that the 95% confidence intervals for the pooled relative frequencies were wide, which is also reflected by the considerable study heterogeneity. Interestingly, no significant difference was observed between the pooled rates of dizziness and vertigo, although these findings are limited by a considerable study heterogeneity. The reason for such a considerable heterogeneity is not certain, but could be explained by some of the following concerns:
First, there is a lack of adherence to standardized terminology. The Bárány Society introduced their classification of vestibular symptoms in 2009(22). Despite this, just one of eight studies published after 2009 defined dizziness or vertigo according to the classification(14). Of the remaining studies, one applied definitions of dizziness and vertigo that did not conform with the current classification(11), while the remaining studies did not provide any description(12,13,15–18). The lack of clear-cut definitions raises methodological concerns and limits the reliability of study comparisons. As such, future studies should emphasize defining the vestibular symptom of interest and specify its relation to the natural course of migraine attacks. Although this has partly been investigated for patients who fulfill the ICHD appendix criteria for vestibular migraine(1), it remains unknown for the broader group of migraine patients who experience vestibular symptoms but do not have vestibular migraine. This challenge can be overcome by implementing the classification system proposed the Bárány Society routinely when assessing patients with vestibular symptoms.
Second, results could be influenced by demographic characteristics and migraine phenotype. Both of the studies with available data showed that dizziness and vertigo were more prevalent among patients with migraine with aura compared to patients with migraine without aura(11,14). Other studies have shown that there is a significant age- and sex effect on the prevalence of vestibular symptoms, with symptoms being more prevalent among women and individuals older than 50 years(23). These factors could have been elucidated through meta-regression or subgroup analysis, which was not feasible due to a low number of included studies(10).
Third, the duration and frequency of the dizziness or vertigo might influence study heterogeneity. None of the included studies reported the frequency of migraine headaches with dizziness or vertigo as associated symptom. Furthermore, none of the studies described the duration of the dizziness or vertigo or how the patients perceived the dizziness or vertigo. In addition, it was not reported whether patients experienced any dizziness- or vertigo-related trigger-, aggravating- or alleviating factors. As such, it is unknown whether the reported symptoms of dizziness or vertigo amounted to comparable clinical symptoms. Further knowledge on the clinical presentation of headache-associated dizziness or vertigo in the general population of migraine patients is warranted.
Finally, the use of preventive headache medications could account for some of the between-study heterogeneity. Vestibular symptoms are common side effects to migraine preventives such as antihypertensives and anticonvulsants(24). This was largely unaccounted for in the included studies. The concerns raised above are reflected in the study quality of the included studies. Seven of the nine included studies scored ≤ 3 out of a possible score of 9, which attests to an insufficient study quality. The low study quality was mainly due to a lack of outcome definitions, improper methods of ascertainment (primarily self-report) and few studies utilizing control groups.
The present review and meta-analysis raises some concerns for the clinical utility of vestibular migraine as an independent diagnostic entity. At present, vestibular migraine is found in the appendix criteria of the ICHD-3(5). The proposed criteria strongly emphasize vertigo, while dizziness is only accepted as a symptom in vestibular migraine when it is induced by head-motion and present with nausea(5). In this context, it is worth noting that in our meta-analysis, no significant difference was observed in the relative frequency of dizziness compared to vertigo. Thus, it remains unclear whether the vestibular migraine criteria are too narrow and of clinical utility. To answer these questions, there is a need for studies that adhere to standardized definition of vestibular symptoms.
It is worth to mention some methodological limitations to this review. This review was designed to be comprehensive with a search string that included all common terms used for vestibular symptoms. However, it is possible that not all eligible studies were identified. Consequently, we made a concerted effort to manually search the reference lists of all included articles. Moreover, the meta-analysis was limited by small samples and a considerable between-study heterogeneity. This introduced risk of bias in the analysis of the studies and limited our ability to quantitatively explore the data due to a low number of studies.
Conclusions
There is a scarcity in the literature on the prevalence of migraine patients experiencing dizziness and vertigo in the prodromal phase of migraine. Approximately one third experience headache-associated dizziness or vertigo, with similar rates for both symptoms. The findings from the meta-analysis indicates the current research criteria for vestibular migraine may be inadequate, as migraine patients where dizziness is the primary manifestation the vestibular symptom might be overlooked. However, methodological variations confound comparisons of epidemiological patterns. Future studies should use rigorous methodology and adhere to standardized definitions to enable accurate measurements of vestibular symptoms during both the prodromal phase and headache phase of migraine.
Supplementary Material
Inclusion and exclusion criteria
Flow Diagram: Study selection
Article highlights.
Approximately one-third of patients with migraine experience dizziness or vertigo during the headache-phase of their migraine attacks
Meta-analysis showed that the 95% confidence interval for the pooled relative frequency was 13.7% to 61.5% for dizziness and 26.7% to 41.5% for vertigo, and as such, these results need to be interpreted with caution due to significant study heterogeneity.
There is a need for further studies investigating the frequency and clinical characteristics of migraine headaches accompanied by headache-phase associated dizziness or vertigo. These findings could shed light on the pathophysiologic connection between migraine and vestibular dysfunction. Future studies should utilize standardized definitions of vestibular symptoms, such as the symptom classification provided by the Bárány Society, to facilitate accurate data measurements and enable comparative analyses.
Funding/Support
No funding was received for this study.
Footnotes
Conflict of Interest Disclosures
Afrim Iljazi, Håkan Ashina, Basit Chaudhry, Haidar Muhsen Al-Khazali, James G. Naples, Vlasta Vukovic Cvetkovic and Rami Burstein have no conflicts of interest to declare. Richard B. Lipton is the Edwin S. Lowe Professor of Neurology at the Albert Einstein College of Medicine in New York. He receives research support from the NIH: 2PO1 AG003949 (Multiple Principal Investigator), 5U10 NS077308 (Principal Investigator), RO1 NS082432 (Investigator), 1RF1 AG057531 (Site Principal Investigator), RF1 AG054548 (Investigator), 1RO1 AG048642 (Investigator), R56 AG057548 (Investigator), K23 NS09610 (Mentor), K23AG049466 (Mentor), 1K01AG054700 (Mentor). He also receives support from the Migraine Research Foundation and the National Headache Foundation. He serves on the editorial board of Neurology, senior advisor to Headache, and associate editor to Cephalalgia. He has reviewed for the NIA and NINDS, holds stock options in eNeura Therapeutics and Biohaven Holdings; serves as consultant, advisory board member, or has received honoraria from: the American Academy of Neurology, Alder, Allergan, American Headache Society, Amgen, Autonomic Technologies, Avanir, Biohaven, Biovision, Boston Scientific, Dr Reddy’s, Electrocore, Eli Lilly, eNeura Therapeutics, GlaxoSmithKline, Merck, Pernix, Pfizer, Supernus, Teva, Trigemina, Vector, and Vedanta. He receives royalties from Wolff’s Headache, 7th and 8th Edition, Oxford Press University, 2009, Wiley and Informa. Henrik W. Schytz has received consultant fees from Teva, Novartis and BalancAir and received grants from Novartis. Sait Ashina has received consulting fees from Novartis, Amgen, Allergan, Elli Lilly, Supernus, Satsuma, Percept Promius and Theranica.
References
- 1.Von Brevern M and Lempert T. Vestibular migraine In: Vinken PJ and Bruyn GW Handbook of Clinical Neurology. Volume 137 (3rd series). Elsevier B.V., 2016, pp. 301–16. [DOI] [PubMed] [Google Scholar]
- 2.Lempert T, Olesen J, Furman J, et al. Vestibular migraine: Diagnostic criteria. J Vestib Res. 2012;22(4):167–72. [DOI] [PubMed] [Google Scholar]
- 3.Cho SJ, Kim BK, Kim BS, et al. Vestibular migraine in multicenter neurology clinics according to the appendix criteria in the third beta edition of the International Classification of Headache Disorders. Cephalalgia. 2016;36(5):454–62. [DOI] [PubMed] [Google Scholar]
- 4.Kelman L and Tanis D. The relationship between migraine pain and other associated symptoms. Cephalalgia. 2006;26(5):548–53. [DOI] [PubMed] [Google Scholar]
- 5.Headache Classification Committee of the International Headache Society. The International Classification of Headache Disorders, 3rd Edition. Cephalalgia. 2018;38(1):1–211. [DOI] [PubMed] [Google Scholar]
- 6.Headache Classification Committee of the International Headache Society. The International Classification of Headache Disorders, 3rd Edition (beta version). Cephalalgia. 2013;33(9):629–808. [DOI] [PubMed] [Google Scholar]
- 7.Headache Classification Committee of the International Headache Society. International Classification of Headache Disorders, 1st Edition. Int Headache Soc. 1988;1–96. [PubMed] [Google Scholar]
- 8.Headache Classification Committee of the International Headache Society. The International Classification of Headache Disorders, 2nd Edition. Cephalalgia. 2004;24 Suppl 1:1–160. [DOI] [PubMed] [Google Scholar]
- 9.Wells G, Shea B, O’Connell D, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. Online Referencing, http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp (accessed 28 January 2020). [Google Scholar]
- 10.Higgins JPT and Green S. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0. Online Referencing, https://handbook-5-1.cochrane.org/chapter_9/9_6_5_1_ensure_that_there_are_adequate_studies_to_justify.htm (2011, accessed 30 January 2020) [Google Scholar]
- 11.Akdal G, Özge A, Ergör G. The prevalence of vestibular symptoms in migraine or tension-type headache. J Vestib Res. 2013;23(2):101–6. [DOI] [PubMed] [Google Scholar]
- 12.Akdal G, Baykan B, Ertaş M, et al. Population-based study of vestibular symptoms in migraineurs. Acta Otolaryngol. 2015;135(5):435–9. [DOI] [PubMed] [Google Scholar]
- 13.Bisdorff A, Andrée C, Vaillant M, et al. Headache-associated dizziness in a headache population: Prevalence and impact. Cephalalgia. 2010;30(7):815–20. [DOI] [PubMed] [Google Scholar]
- 14.Carvalho GF, Vianna-Bell FH, Florencio LL, et al. Presence of vestibular symptoms and related disability in migraine with and without aura and chronic migraine. Cephalalgia. 2018;0(0):1–9. [DOI] [PubMed] [Google Scholar]
- 15.Hsu LC, Wang SJ, Fuh JL. Prevalence and impact of migrainous vertigo in mid-life women: A community-based study. Cephalalgia. 2011;31(1):77–83. [DOI] [PubMed] [Google Scholar]
- 16.Kelman L Migraine changes with age: IMPACT on migraine classification. Headache. 2006;46(7):1161–71. [DOI] [PubMed] [Google Scholar]
- 17.Menon B and Kinnera N. Prevalence and characteristics of migraine in medical students and its impact on their daily activities. Ann Indian Acad Neurol. 2013;16(2):221–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lampl C, Rapoport A, Levin M, et al. Migraine and episodic vertigo: A cohort survey study of their relationship. J Headache Pain. 2019;20(1):2–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Santoro G, Bernasconi F, Sessa F,et al. Premonitory Symptoms in Migraine Without Aura: A Clinical Investigation. Funct Neurol. 1990;5(4):339–44. [PubMed] [Google Scholar]
- 20.Giffin NJ, Ruggiero L, Lipton RB, et al. Premonitory symptoms in migraine: An electronic diary study. Neurology. 2003;60:935–40. [DOI] [PubMed] [Google Scholar]
- 21.Lipton RB, Pavlovic JM, Haut SR, et al. Methodological Issues in Studying Trigger Factors and Premonitory Features of Migraine. Headache. 2014;54(10):1661–9. [DOI] [PubMed] [Google Scholar]
- 22.Bisdorff A, Von Brevern M, Lempert T, et al. Classification of vestibular symptoms: Towards an international classification of vestibular disorders. J Vestib Res. 2009;19(1–2):1–13. [DOI] [PubMed] [Google Scholar]
- 23.Teggi R, Manfrin M, Balzanelli C, et al. Point prevalence of vertigo and dizziness in a sample of 2672 subjects and correlation with headaches. Acta Otorhinolaryngol Ital. 2016;36(3):215–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Vecsei L, Majlath Z, Szok D, et al. Drug Safety Drug safety and tolerability in prophylactic migraine treatment. Expert Opin Drug Saf. 2015;14(5):667–81. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Inclusion and exclusion criteria
Flow Diagram: Study selection