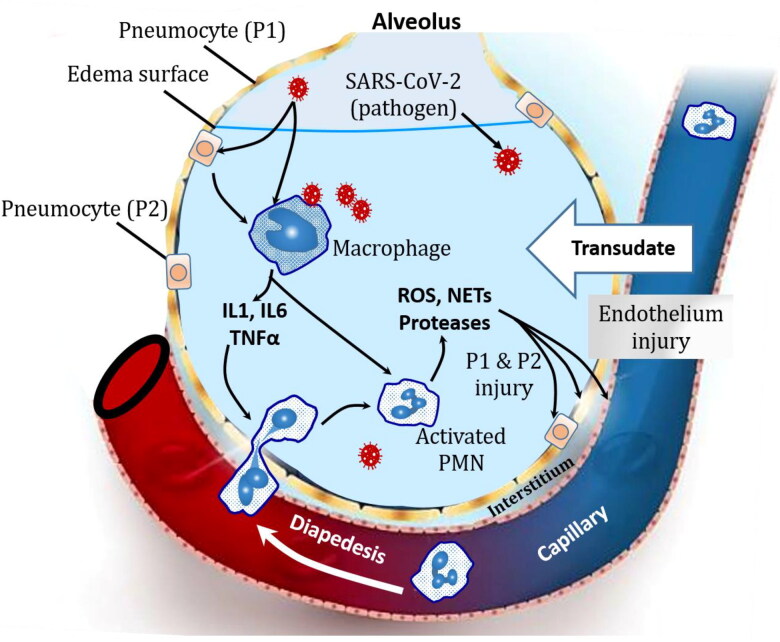
Figure 2.
Pathophysiology of ARDS in SARS-CoV-2 inducing COVID-19 patients with severe symptoms. Once SARS-CoV-2 gets into the body, it uses its S-spike type, as a key to enter the cells by binding to angiotensin-converting enzyme (ACE2). The virus use the mainly pneumocytes 2 components for its own proliferation. The infected cells secret a high amount of specific inflammatory mediators that enhance macrophages to release cytokines Tumor Necrosis Factor alpha (TNFα) and interleukins (IL-1 and IL-6). These cytokines lead to the disruption of the alveolar-capillary membrane integrity and increased the vascular permeability. The disrupted integrity of the alveolar-capillary allow the plasma leakage into the alveoli and the lungs interstitial spaces. The formation of protein rich edema, known as exudate, in the interstitium and alveolar spaces leads to alveolar flooding making it very difficult to breathe and lead to hypoxemia. Driven by IL-1, IL-6 and TNFα, PMNs invade the alveoli and release reactive oxygen species (ROS), neutrophil extracellular traps (NETs) and proteases that damage the vascular and the alveoli components that exacerbates the hypoxemia, the alveoli collapsing and lead to a worse situation: alveolar consolidation.