Abstract
Background
Although mental health issues constitute an increasing global burden affecting a large number of people, the mental health care industry is still facing several care delivery barriers such as stigma, education, and cost. Connected mental health (CMH), which refers to the use of information and communication technologies in mental health care, can assist in overcoming these barriers.
Objective
The aim of this systematic mapping study is to provide an overview and a structured understanding of CMH literature available in the Scopus database.
Methods
A total of 289 selected publications were analyzed based on 8 classification criteria: publication year, publication source, research type, contribution type, empirical type, mental health issues, targeted cohort groups, and countries where the empirically evaluated studies were conducted.
Results
The results showed that there was an increasing interest in CMH publications; journals were the main publication channels of the selected papers; exploratory research was the dominant research type; advantages and challenges of the use of technology for mental health care were the most investigated subjects; most of the selected studies had not been evaluated empirically; depression and anxiety were the most addressed mental disorders; young people were the most targeted cohort groups in the selected publications; and Australia, followed by the United States, was the country where most empirically evaluated studies were conducted.
Conclusions
CMH is a promising research field to present novel approaches to assist in the management, treatment, and diagnosis of mental health issues that can help overcome existing mental health care delivery barriers. Future research should be shifted toward providing evidence-based studies to examine the effectiveness of CMH solutions and identify related issues.
Keywords: mental health, connected health, eHealth, mobile health, telehealth, mHealth, mobile phone, health informatics, review, interdisciplinary research, information technology, information systems
Introduction
Background
Mental health issues can decrease the quality of life [1,2], increase the risk of communicable and noncommunicable diseases, and contribute to both unintentional and intentional injury [3]. They may also cause, among other issues, lower educational achievements, substance abuse, and violence [4]. Mental illness is considered as “one of the main causes of unhappiness in the world. It produces nearly as much of the misery that exists as poverty does, and more than is caused by physical illness” [5]. On average, they reduce national income by 5% through unemployment, absenteeism, lowered productivity, and extra physical health care costs [6].
Although mental health issues constitute a global concern and threat, the mental health care industry is still struggling to overcome various barriers and reach people in need [7]. In low- and middle-income countries, more than 75% of people identified with serious anxiety, problematic mood changes, impulse control, or substance abuse disorders did not receive any care [8]. Among the barriers and challenges that threaten the mental health care industry are cost issues [9], shortage of mental health care providers, health plan barriers, lack of coverage or inadequate coverage [10], stigma, and poor mental health literacy [11]. Cultural orientations can, in some cases, be considered as a barrier for seeking mental help and access [12]. Mental health care delivery can also face barriers in complicated situations such as the recent coronavirus disease (COVID-19) global outbreak [13,14]. Such pandemics create global feelings of fear, worry, sadness, and anger and cause a global increase in stress and anxiety, especially for people with existing mental health problems [15,16], putting more load on health care institutions. They also create new obstacles to mental health care delivery as many people are in quarantine and several countries are in complete lockdown, making access to mental health care even more challenging [17].
Connected mental health (CMH), which refers to the use of information and communication technologies (ICT) to support and improve mental health conditions and mental health care, can help alleviate some of the aforementioned barriers [18]. This presents unlimited possibilities and opportunities to help overcome the challenges, barriers, and limitations of the mental health care industry [18].
CMH solutions are connected health solutions for mental health care. The term connected health is used to “encompass terms such as wireless, digital, electronic, mobile, and tele-health” [19]. Connected health has become an established research field in the past 5 years [20]. In this paper, we use the term CMH to refer to topics related to electronic mental (e-mental) health, mobile mental (m-mental) health, telemental health, and digital mental health, among others. CMH solutions have the potential to allow anonymous access to overcome care preventing stigma, access to care with minimal to no cost, reach remote areas, enhance patients’ engagement, and access information [21,22]. They also have the potential to deliver cost-effective mental health services [23]; overcome geographical barriers [24]; and provide a better understanding of mental illnesses’ development, recovery, symptom assessment, and monitoring through the use of technology [25]. CMH can use technology-based interventions such as video conferencing; telemental health [26]; mobile-based interventions [27,28]; internet-based solutions [29,30], which are necessary in situations such as global health pandemics; and novel digital data collection interventions [31,32]. In addition, CMH can improve several important areas of mental health care, including primarily information provision, screening, assessment, monitoring, intervention, and social support [22].
Objectives
This paper presents the results of a systematic mapping study conducted to analyze the current research landscape of CMH literature in the Scopus database. To conduct the analysis, 8 mapping questions (MQs) were addressed, which allowed us to classify 289 selected publications indexed in Scopus according to their publication year, publication source, research type, contribution, empirical type, mental health issues, and targeted cohort.
Methods
Overview
This study follows the mapping process proposed by Petersen et al [33]. This process covers the selection of relevant publications, the construction of a classification scheme, and a systematic mapping of publications. The principal objective of a systematic mapping study is to structure a research area and provide an overview of the available literature, primarily by investigating the covered topics and classifying the available contributions [34].
MQs
Textbox 1 presents the 8 MQs and their rationale. The MQs were defined to provide an overview and a structured understanding of the existing CMH literature in the Scopus database.
Mapping questions.
MQ1 (mapping question)
How has the frequency of publications addressing CMH (connected mental health) changed over time?
MQ2
Which publication channels are the main target for CMH research?
MQ3
What are the research types of studies addressing CMH?
MQ4
What are the contributions of published CMH studies?
MQ5
Are CMH studies empirically validated or evaluated?
MQ6
What are the mental health disorders addressed in CMH literature?
MQ7
Who are the target audience in CMH studies?
MQ8
In which countries were the selected empirically evaluated studies conducted?
Search Strategy
The search was conducted in the Scopus database, which is considered to be the largest indexation database that includes articles from various disciplines such as engineering, medicine, business, and computer science [35].
The aim of the selection process was to identify the articles that are most relevant to the objective of this mapping study. To further focus the search and include relevant studies, the search was focused on the titles of the publications.
The following search strings were applied to the titles of the publications indexed in Scopus:
“e-” AND “mental” AND “health”
(“Mobile” OR “M-”) AND “mental” AND “health”
“Digital” AND “mental” AND “health”
“Connected” AND “mental” AND “health”
“Tele” AND “mental” AND “health”
The search strings were formulated to include a broad selection of literature and were not combined in one search string for the purpose of identifying the number of results for each term separately. The search for publications was conducted on January 23, 2020.
Papers Selection
The first author (ND) retrieved candidate papers from the results of the search and entered information in an Excel (Microsoft Corporation) file that was shared with the second author (SO) for revision. The two authors examined the title, abstract, and keywords and then commented on whether the paper was to be included in or excluded from the selection according to the inclusion and exclusion criteria (EC).
The inclusion criterion was limited to publications that addressed an aspect of CMH, and the studies that satisfied any one of the following EC were eliminated:
EC1: studies published after 2019 to construct a clear trend of publication
EC2: studies not published in English, as there is a clear dominance of the English language in the international communications, science, and literature [36,37]
EC3: papers published as notes, editorials, or letters
EC4: publications not addressing mental health issues
EC5: publications not addressing the use of technology for mental health.
Figure 1 shows the selection results. A total of 289 papers (out of 571 candidate studies) were included in the final selection. EC 1, 2, and 3 were applied in the Excel file. Checking for EC 4 and 5 and the screening of studies were conducted by inspecting the abstracts and, in some cases, the full texts of the candidate studies.
Figure 1.
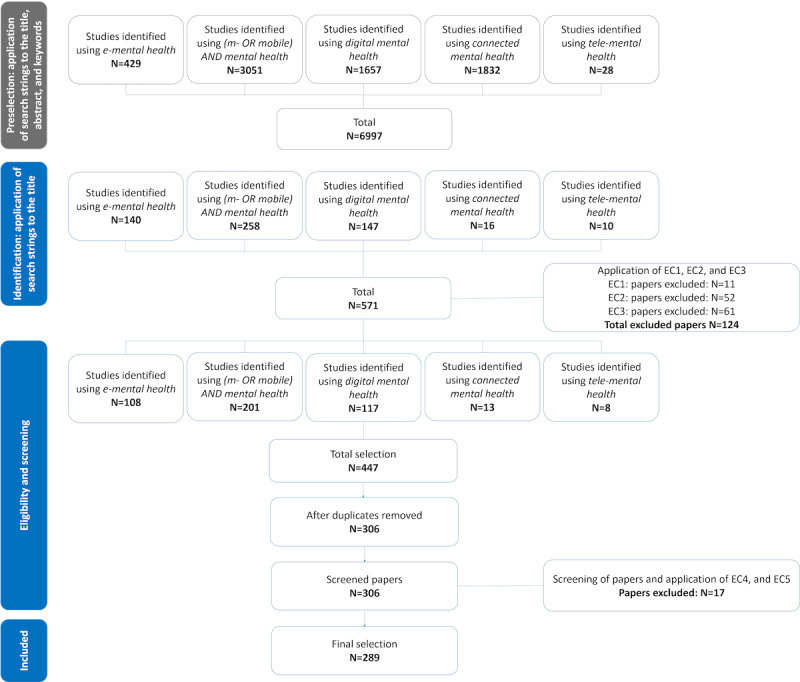
Selection process. EC: exclusion criteria; e-mental: electronic mental; tele-mental health: telehealth for mental health.
Data Extraction Strategy
The extraction of data from the selected studies was focused primarily on providing answers to the MQs according to the criteria presented in Textbox 2.
Classification criteria.
MQ1 (mapping question)
Identifying the publication year and term used can assist in suggesting the publication trend. The main term of each study was not based on the results of the selection process but was based on an analysis of the content of the publications
MQ2
Identifying the publication channel and the publication source of each study
MQ3
Research types can be classified as follows: (1) solution proposal: a solution to an existing problem, either novel solution or a significant extension of an existing solution; (2) review: analysis of the existing literature; (3) exploratory study: conducting research and investigating on a specific aspect; (4) opinion paper: these papers express the personal opinion of the author on a specific technique not relying on related work or research methodologies; (5) validation research: this type of paper investigates novel solutions that have not been implemented yet; (6) evaluation research: conducting a study on an implemented solution by identifying how the solution has been implemented in practice, the benefits and drawbacks of the implementation, and relevant problems in the field; (7) feasibility study: an analysis of relevant factors of success of an intervention to determine the likelihood of its implementation successfully; and (8) books and book chapters
MQ4
The contributions of the selected studies can be classified as follows: (1) tool-based techniques: techniques based on software or devices used to accomplish a connected mental health (CMH)–related task; (2) model: a system that allows structured utilization of CMH solutions; (3) method: development or design of an approach by creating a series of steps that can assist in utilizing CMH solutions; (4) guidelines: a set of rules or recommendations to be followed during the course of an action related to CMH; (5) framework: a real or conceptual structure intended to support and guide the creation of CMH-related contributions; (6) protocol: a set of rules guiding use of technology for mental health care; (7) perspectives and attitudes toward CMH: results on perspectives, attitudes, acceptance, and preferences toward CMH in general or in a specific group of people; (8) advantages and challenges of CMH: views regarding the advantages, benefits, risks, challenges, and limitations of CMH; and (9) other: results of general research on the efficacy, effectiveness, and usability of CMH interventions
MQ5
The empirical types can be classified as follows: (1) experiment: testing a hypothesis by creating a situation with controlled conditions; (2) case study: testing a solution in real life, with the purpose of gathering new information and detecting potential issues by analyzing real cases; (3) questionnaire: a set of specific, easy to answer questions targeting an audience to collect large amounts of data; (4) interview: a conversational method based on asking specific questions to gather in-depth, precise, and meaningful data; (5) mixed methods: using more than one empirical evaluation method; (6) focus group: investigating results and feedback in a relatively small group of participants; (7) other: all empirical evaluation methods that do not belong to any of the categories above; and (8) none: all solutions that were not validated empirically were classified as theories
MQ6
Identifying the mental problem addressed in each study
MQ7
Identifying the targeted cohort group
MQ8
Identifying the country or region where the study has been conducted. Nonempirically evaluated studies are usually general, whereas empirically evaluated studies focus on specific groups and countries or regions. Therefore, for this question, we focus on the latest
Synthesis Method
The synthesis method used in this study consisted of the following steps:
Reading and analyzing the 289 selected studies to extract information presented in the Data Extraction Strategy subsection.
Classifying the studies by enumerating the number of publications per MQ. It should be noted that selected publications addressing more than one mental health issue (MQ6), more than one cohort group (MQ7), and more than one country (MQ8) were counted in each category.
Presenting the classification results in figures and charts, such as bubble plots, as visualization of the results facilitated their analysis.
Presenting a narrative summary to describe the principal findings.
Compliance With Ethical Standards
This paper does not contain any study with human participants or animals.
Results
This section summarizes the results of the MQs. The results of the mapping study can be found in Multimedia Appendix 1.
MQ1: How Has the Frequency of Publications Addressing CMH Changed Over Time?
Figure 2 shows the publication trend per term used in the selected papers: mobile or m-mental, e-mental, digital, and telemental health. This shows a significant increase in interest in the field of CMH research in the past decade. The publication trend began with fewer than 5 publications per year until 2011. We estimate that the trend of publication will continue to increase in 2020, particularly owing to the increasing interest in mental health during the recent COVID-19 pandemic.
Figure 2.
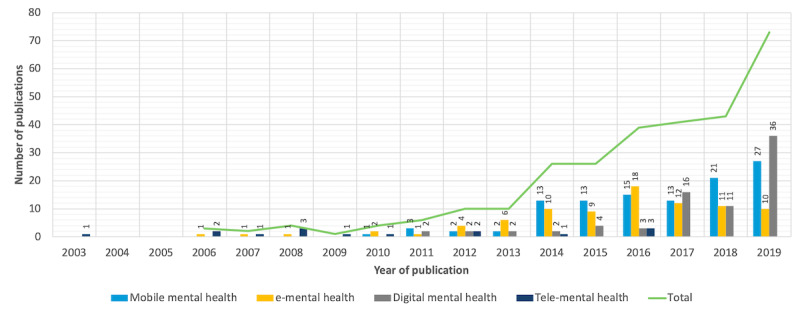
Connected mental health publication trend. e-mental: electronic mental; tele-mental health: telehealth for mental health.
MQ2: Which Publication Channels Are the Main Target for CMH Research?
A total of 3 publication channels have been identified from the selected studies: journals, conferences, and books. Overall, 82.3% (238/289) of the selected papers were published in journals, 11.4% (33/289) were published in conference proceedings, and 6.2% (18/289) were published in books. A total of 39 of the selected studies were retrieved from the Journal of Medical Internet Research. Table 1 presents publication sources that published two or more selected studies.
Table 1.
Publication sources that published more than one selected publication.
| Publication sources | Publications, n | References |
| Journal of Medical Internet Research | 39 | [38-76] |
| e-Mental Health | 8 | [77-84] |
| Journal of Mental Health | 7 | [18,25,85-89] |
| BMC Psychiatry | 7 | [90-96] |
| Psychiatric Services | 7 | [22,97-102] |
| Frontiers in Psychiatry | 7 | [103-109] |
| Studies in Health Technology and Informatics | 6 | [110-115] |
| Current Treatment Options in Psychiatry | 6 | [116-121] |
| Journal of Technology in Human Services | 5 | [122-126] |
| Professional Psychology: Research and Practice | 4 | [127-130] |
| Australian and New Zealand Journal of Psychiatry | 4 | [131-134] |
| Internet Interventions | 3 | [135-137] |
| Current Psychiatry Reports | 3 | [138-140] |
| Asian Journal of Psychiatry | 3 | [141-143] |
| Australian Family Physician | 3 | [144-146] |
| Evidence-Based Mental Health | 3 | [147-149] |
| Lecture Notes in Computer Science (including subseries Lecture Notes in Artificial Intelligence and Lecture Notes in Bioinformatics) | 3 | [150-152] |
| PLoS ONE | 3 | [153-155] |
| International Journal of Mental Health Nursing | 3 | [156-158] |
| Telemedicine and e-Health | 3 | [159-161] |
| Psychiatric Times | 3 | [162-164] |
| Frontiers in Public Health | 3 | [165-167] |
| Health Informatics Journal | 3 | [168-170] |
| Indian Journal of Psychological Medicine | 3 | [171-173] |
| JAMA Psychiatry | 2 | [174,175] |
| Journal of Psychosocial Nursing and Mental Health Services | 2 | [176,177] |
| Journal of Physics: Conference Series | 2 | [178,179] |
| BMC Medical Informatics and Decision Making | 2 | [180,181] |
| Psychiatry (New York) | 2 | [182,183] |
| Conference on Human Factors in Computing Systems—Proceedings | 2 | [184,185] |
| Journal of Affective Disorders | 2 | [186,187] |
| Cyberpsychology, Behavior, and Social Networking | 2 | [188,189] |
| Journal of Psychiatric Research | 2 | [190,191] |
| European Journal of Psychotraumatology | 2 | [192,193] |
| IEEE International Symposium on Computer-Based Medical Systems—Proceedings | 2 | [194,195] |
| Advances in Mental Health | 2 | [196,197] |
| The Digitization of Healthcare: New Challenges and Opportunities | 2 | [198,199] |
| Australian Psychologist | 2 | [200,201] |
It is worth noting that there might be relevant studies conducted in e-mental health and mobile health companies intended for internal use only and not published in scientific venues. The findings of such studies might offer new interesting insights and might help evolve the CMH field.
MQ3: What Are the Research Types of Studies Addressing CMH?
Figure 3 presents the research types identified in the selected papers. The largest number of the selected publications were exploratory research (104/289, 35.9%), followed by reviews (61/289, 21.1%) and solution proposals (49/289, 16.9%); however, 10.0% (29/289) and only 1.3% (4/289) were evaluation studies and validation research, respectively.
Figure 3.
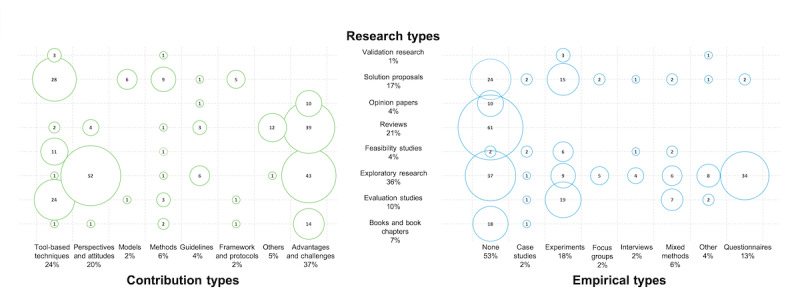
Bubble graph associating the research types with the empirical types and the contribution types.
MQ4: What Are the Contributions of the Selected CMH Studies?
Figure 3 shows the different contributions of the selected papers: 36.6% (106/289) of the selected studies addressed the advantages, challenges, and limitations of CMH; 24.2% (70/289) proposed tool-based solutions; and 19.7% (57/289) investigated perspectives and attitudes toward CMH. Only 3.8% (11/289) of the studies presented guidelines, and only 2.4% (7/289) provided frameworks and protocols.
MQ5: What Are the Empirical Types of the Selected CMH Studies?
Figure 3 shows the identified empirical types of the selected papers. Overall, 52.5% (152/289) of the studies were not evaluated empirically, and 17.9% (52/289) and 12.4% (36/289) were evaluated empirically through experiments and questionnaires, respectively. Only a few publications used empirical evaluation methods such as case studies (7/289, 2.4%), focus groups (7/289, 2.4%), and interviews (6/289, 2.0%). In addition, 10.0% (29/289) of the studies implemented either a mixed method approach (17/289, 5.8%) or used a different, not largely used empirical evaluation approach (12/289, 4.1%).
MQ6: What Are the Mental Health Issues Addressed in the CMH Literature?
Figure 4 shows the mental health issues identified in the selected studies. Most of the selected studies (219 publications) addressed mental well-being in general. A total of 38 publications addressed depression, whereas 22 publications focused on anxiety. Furthermore, 37 papers addressed serious mental illnesses such as bipolar disorder, psychosis, schizophrenia, personality disorders, dementia, panic disorders, and major depressive disorders. Among the identified mental health issues addressed in the selected papers were addiction, suicide, cognitive disorders, sleeping disorders, emotional problems, mindfulness, and productivity influenced by mental state.
Figure 4.
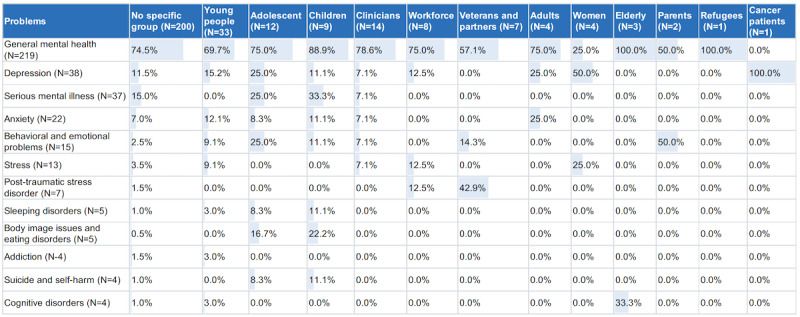
Mental health issue types versus targeted cohort. The color and the percentage represent the frequency of appearance of a problem in the selected studies dealing with a specific cohort.
MQ7: Who Are the Targeted Cohorts in the Selected CMH Studies?
Figure 4 shows all groups identified in the studies. Most studies (200 selected publications) did not address a particular group of people. The remaining publications focused either on age-based groups, such as children, adolescents, and the elderly, or on specific groups, such as veterans, refugees, and cancer patients.
MQ8: In Which Countries Were the Selected Empirically Evaluated Studies Conducted?
Figure 5 shows the geographical distribution of the selected empirically evaluated studies. Most studies were conducted in Australia, followed by the United States and Canada. Some studies included more than one country and were counted for each one.
Figure 5.
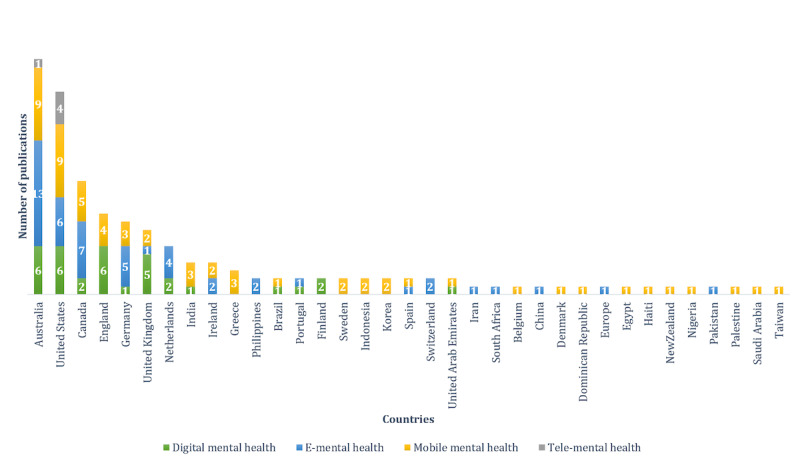
Geographical distribution of empirically evaluated studies. E-mental: electronic mental; tele-mental health: telehealth for mental health.
Discussion
Principal Findings
Trends in Publication and Usage of Terms
There has been an increasing interest in CMH publications in the past decade. This can be explained by the fact that CMH research has been influenced continuously by novel technological interventions and the growth in ICT usage, especially with the appearance of Web 2.0 between 2003 and 2004 [202]. Web 2.0 introduced an architecture of participation [203], focusing on social interactions and collective intelligence [204]. These changes were accompanied by a significant increase in the number of internet users worldwide [205] as well as ownership and usage of smartphones [206] and computers [207-209]. This has also impacted the use of ICT, which has been incorporated in many fields, including transport [210], tourism [211], education [212], virtual work teams [213], and health care [214].
An increase in the number of publications in the field of CMH could have also been influenced by the changes in the general literature. There has been a shift from paper copies to electronic copies, which significantly increased the accessibility to published studies, particularly open access publications [215]. Consequently, the research evaluations performed by peers became reliant on different bibliometrics [216]. The productivity of researchers has mainly been measured by bibliometrics (eg, journal’s impact factor [217,218] and researcher’s h-index [219]), which is impacting hiring processes, academic promotion, and funding decisions [219,220]. This puts more pressure on researchers to produce more publications in the literature, particularly publications indexed in Scopus.
The earliest term used in the selected CMH studies was telemental health, which falls in the same group of terms as telemedicine and telepsychiatry. These terms have been used to describe remote health care and informatization of some elements of the health care process since the 1990s [221,222]. The term telemental health has rarely been used in recent years as e-mental health began emerging since 2006.
The term eHealth was introduced in the late 1990s. It was defined at the 7th International Congress on Telemedicine and Telecare in London at the end of November 1999 by John Mitchell as “a new term needed to describe the combined use of electronic communication and information technology in the health sector” and as “the health industry’s equivalent of e-commerce” [223]. Although previously used terms were linked to medical professionals, eHealth was found to be driven by nonprofessionals, namely, patients (or consumers) [224]. Many journals after the introduction of eHealth changed their names to include it; for example, the Telemedicine Journal added an “and eHealth” to its title. Nevertheless, publications were not including the term eHealth, and researchers preferred to use more specific terms such as medical informatics, telemedicine, and electronic patient records, which are considered more meaningful than the generic term eHealth [223]. This might explain its late and delayed emergence in the literature.
The trend of publications also showed an increasing use of the term m-mental health, primarily since 2010. The expansion in the use and ownership of smartphones [225] brings new opportunities for the mental health care industry to face some of the most pressing global challenges and make mental health care more accessible, faster, less expensive, and better [226]. Studies have proven the interest and willingness of people with mental health issues to try mobile solutions [73,227]. Hence, it is expected that m-mental health will continue to attract the attention of CMH researchers and practitioners.
The term digital mental health has been used since 2011. This term is associated with the use of recent and advanced technologies, such as sensors [228] and machine learning techniques, and it has been used as a modern synonym for e-mental health, especially since 2017. It must be noted that researchers use different terms to refer to the same concept, and, in many studies, authors use more than one term, which might occasionally create confusion, especially in cases in which known definitions of each term overlap. Consequently, there is a need for a broad term such as connected mental health to encompass the different terms used. Although connected health has become an established field [20], we did not find the use of such a term in mental health care. To the best of our knowledge, this is the first study that uses this term to refer to the use of ICT in mental health.
Publication Channels
Most of the selected papers (238/289, 82.3%) were published in scientific journals. Publishing in a rigorous scientific journal is based on a set of ethics and rules [229] that can result in the production of high-quality content. This result could have been impacted also by the choice of digital library. More journals than conference proceedings in CMH might have satisfied the criteria of Scopus indexation. There are also many scientific journals that are categorized in health informatics. This encourages researchers to conduct studies suited for journals and indicates a particular level of maturity in the field from a quantitative perspective. Articles published in journals tend to be more detailed and extensive. Conferences are also an important venue for publications. Conferences with proceedings provide fast tracking of publication to keep researchers and practitioners up to date with the latest findings. The first identified publication in the selected studies, which appeared in 2003, was a book. Books are used to introduce or provide a detailed overview of a topic.
Research Types and Empirical Types
The multidisciplinary nature of the CMH field and its various subareas resulted in a high ratio of exploratory research and reviews compared with other types of research, such as solution proposals, validation, and evaluation research. The diversity of the identified empirical evaluation types points to the uncertainty regarding adequate methods to evaluate CMH solutions. There is a need for evidence-based studies that will verify the efficiency of CMH interventions, create accurate results for future research, and identify challenges that need to be addressed. Most of the selected studies (152/289, 52.5%) were not evaluated empirically, which can be linked to the fact that a large number of empirical evaluation studies in the health informatics field have not been published [230]. Most of the remaining studies were empirically evaluated through experiments (52/289, 17.9%), primarily owing to their controlled environments. Case studies are more suited for sensitive problems such as mental health issues and would be more beneficial for the growth of the field, as they help identify many issues that can be faced in real-life implementation of ICT interventions. However, only 2.4% (7/289) of the selected studies were evaluated empirically through case studies. Questionnaires represented an important part of the empirical evaluation methods of the selected studies (36/289, 12.4%) used mainly in exploratory research (104/289, 35.9%) to investigate perspectives and attitudes toward the use of technology for mental health and on advantages, challenges, and limitations of CMH. Questionnaires are useful tools for data collection as they can be formulated to collect significant amounts and various types of data and can be delivered through various means to reach large groups of people.
Contributions of the Selected Studies
The largest number of the selected studies focused on investigating the advantages, benefits, risks, challenges, and limitations of CMH (106/289, 36.6%) as well as perspectives and attitudes of patients, clinicians, and various stakeholders toward CMH (57/289, 19.7%). An important part of the identified contributions was about tool-based techniques (70/289, 24.2%), whereas only a few studies represented frameworks, protocols, and models (14/289, 4.8%). This points to a level of ambiguity in the field as frameworks, protocols, and models are typically signs of clear understanding of a concept, its benefits, and its limitations. Tool-based techniques are usually relatively specific to one area of implementation and target a specific need, for instance, a mobile app for tracking mood changes or a website for evaluating levels of depression. Despite an increasing number of CMH publications, the types of research identified are primarily theoretical and hypothetical, indicating that researchers are still proposing their conceptual ideas for CMH. Only 4.4% (13/289) of the studies, categorized as others in Figure 3, addressed topics such as effectiveness, efficiency, usability, and quality of technological solutions for mental health care. The lack of publications on these topics is related to the aforementioned lack of empirical evaluation studies.
Mental Disorders and the Targeted Cohort
Most of the selected studies did not target a specific group of people (200/289, 69.2%). The remaining studies focused primarily on young people, adolescents, and children (33/89, 37%; 12/89, 13%; and 9/89, 10%, respectively). There was an overlap of age ranges among the categories, primarily owing to the existing overlapping of ages in the known definitions of the categories. The World Health Organization defines adolescence as the age range spanning from 10 to 19 years, youth as those aged between 15 and 24 years, and young people as the group covering the 2 categories from 10 to 24 years [231]. The adolescent group is further divided to include a subgroup of early adolescence (11-14 years) [232], which might be referred to by some authors as children. Targeting primarily the young category of patients can be explained by the fact that this category is characterized by the ownership of mobile devices, high usage of the internet and social networks, and familiarity with the use of technology, which makes it easy for them to become customers of CMH solutions.
On the basis of our findings, the young people category is the main target for studies on technological solutions for depression, anxiety, and related issues. These disorders are the third leading cause of death among adolescents and young adults, with a prevalence of approximately 4% in children and 10% to 20% in adolescents [233]. Other mental health issues such as body image issues, eating disorders, and sleep problems are also common among young people. Most mental health issues identified in this category could be linked to young people’s extensive use of social networks and living a digital life, making them disconnected from real life and absorbed in following other people’s lives and comparing them with their own lives. In many cases, this can cause them to feel worthless and disappointed with their lives, bodies, or achievements. Internet use has become an addiction for many young people, causing, among other problems, loss of sleep and high levels of loneliness [234] as well as many cyber-related mental problems [235].
Depression, followed by anxiety, was identified among most of the cohort groups, owing primarily to the increasing global expression of these disorders. The global population with depression increased by 18.4% between 2005 and 2015; similarly, the total number of people with anxiety increased by 14.9% between 2005 and 2015 [236]. Depression can occur as a result of other health problems, such as perinatal and postpartum depression among women [155,237] and common depression among cancer patients [238].
Many serious disorders such as schizophrenia, psychosis, and personality disorders were the subjects of many of the selected studies, pointing to the potential of using CMH not only for common mental disorders but also for more severe and complicated mental problems.
Most of the selected CMH publications addressed general mental well-being. Having more studies focusing on specific mental issues might help identify specific limitations and issues as well as highlight opportunities related to specific disorders. More studies should also focus on people in war zones as they are vulnerable to various mental problems and have more barriers to obtain mental health care, which CMH can help solve [239].
Countries in Which the Empirical Evaluations Were Conducted
Most empirical evaluations were conducted in developed English-speaking countries such as Australia, the United States, Canada, and England. This might be mainly owing to the advancement in research in these countries. In Australia, universities are considered world-leading in at least one area of research [240], and large investments are provided to research institutes [241]. There is an important research interest in health informatics in Australia [242]. Research in the United States is believed to be essential to the country’s economic growth. Therefore, the federal government has devoted a significant amount of funding for research [243]. The United States has many of the most accomplished individuals in the field of health informatics working in research projects and institutions specialized in the field [244]. Several developing countries have good ICT infrastructures and can benefit from different CMH interventions to solve several existing issues; however, limited research is conducted in developing countries. The same goes for war zones as only 2 studies addressed people in war zones: one conducted for Palestinian children [245] and the other addressed Syrian refugees in Germany, Sweden, and Egypt [106]. CMH interventions are solutions to overcome mental care barriers in developing countries and war zones. Research in this field should be shifted to countries that are most in need of CMH solutions.
Comparison With Related Studies
The findings of this study are aligned with the findings of other studies related to CMH:
The identified increase in interest in the CMH literature was also reported in a literature review of e-mental health [133].
The identified lack of empirical evaluation of the proposed solutions was reflected in the findings of a meta-analysis on digital interventions for alcohol and substance use disorders, reporting limitations in the number of randomized control trials (RCTs) in that area [117]. Another review on RCTs on the effectiveness of occupational e-mental health concluded the need for more detailed and specific effectiveness research [246]. A narrative review on digital mental health in developing countries reported a shortage of studies on the effectiveness and cost-effectiveness of the investigated internet-based programs [166]. A review on the effectiveness of mobile apps reported a lack of clinically validated evidence on the efficiency of most available apps [191].
There was a lack of use of the term telemental health. Related findings were described in a review of the directions for videoconferencing and telemental health [247]. The review reported a limited number of RCTs in the field as well as methodologically flawed and limited research studies, which resulted in the research agenda of telemental health not being fully maximized [247].
Leading countries in the empirical studies selected were Australia and the United States, which are similar to findings from other reviews. A review reported that evidence for telemental health and web-based solutions are largely led by Australia [138]. Two reviews reported that most of their selected publications were found to have mostly originated in the United States and Australia [22,133], and a study [133] found that Australian e-mental health research was higher in diversity and quantity.
Limitations
This study has some limitations. This study did not include other digital databases. However, Scopus is widely considered to be the largest indexing digital library that includes publications from different disciplines [35]. This allowed us to identify different contributions in CMH research. It should be noted that Web of Science (WoS) was not considered as a recent study showed that slight differences exist between the scientific literature covered in Scopus and WoS Core Collection, which will result in a large number of duplicates [248].
The search strings were applied only to the titles to limit the sizes of the selection and to include only relevant and focused CMH publications, possibly omitting other candidate studies. However, we considered that if a paper’s principal focus was CMH, then at least one of the terms from the search strings could be expected to appear in the title, alleviating the risk of discarding relevant publications for this mapping study.
Other terms, particularly terms related to different mental health issues, might have been relevant for inclusion in the search strings, possibly impacting the results. However, our aim was to provide a high-level overview of existing CMH literature.
Other classification criteria might have been relevant to extracting further information from the selected studies, possibly affecting our findings. However, the principal aim of this systematic mapping study was to provide an overview of CMH literature, and the process and criteria presented in the Methods section fit this purpose.
The final study selection depended on the first two authors, ND and SO, who conducted the search process. The first author conducted a preliminary search in Scopus and constructed a preliminary selection of publications. The second author revised the selection. If a disagreement arose between the two authors on the exclusion or inclusion of a paper, then a discussion took place until an agreement was reached. It should be noted that the two authors have experience in conducting mapping studies and systematic literature reviews [228,249,250].
Conclusions
This paper conducted a systematic mapping study of 289 publications indexed in Scopus and provided an overview of the available literature on CMH research. CMH has the potential to overcome some of the mental health care delivery barriers by introducing and exploiting ICT in the process of mental health care. A total of 289 publications were selected, analyzed, and classified. The results showed that CMH is a promising research field that has gained increasing attention from researchers over the years. The frequency of the selected publications was influenced by the continuous developments in digital media and the use of ICT as well as the changes in literature evaluation methods, which mainly relied on bibliometrics. The results also showed that most of the selected CMH literature addressed general mental well-being; depression and anxiety were the mental disorders most addressed in studies on specific mental issues, which is in accordance with their global prevalence; young people were the most targeted cohort group as they are more familiar with digital solutions; exploratory research and reviews were the dominant research types found in the selected literature, which indicates that researchers are more focused on exploring possible venues of implementation of ICT in mental health care and constructing an understanding of the field; and most of the selected studies were not empirically evaluated. Moreover, the results showed that selected studies that were empirically evaluated were mostly conducted in developed countries. Screening of the selected studies that were reviews showed that they targeted specific cohort groups, specific mental disorders, specific types of solutions, or specific terms. To the best of our knowledge, this is the first mapping study that addresses the field of CMH as a whole, including all relevant terms and without excluding any specific criteria. On the basis of our findings, we recommend the following to researchers:
Shift attention to provide evidence-based solutions and studies, and empirically evaluate existing solutions in future CMH studies.
Focus on specific mental issues and cohort groups to better identify possible issues and limitations of the field.
Investigate CMH solution implementation in developing countries and war zones, which experience various mental care delivery barriers.
Use connected mental health as an englobing term for the exploitation of the different types of ICT in mental health care.
Practitioners can use this study to find tool-based studies for specific cohorts and/or mental disorders. They can also find studies related to the attitudes and behaviors of CMH users.
We believe that our study will provide researchers and practitioners with relevant information regarding the existing CMH literature as well as recommendations for future publications. For future work, we intend to develop a conceptual framework for sustainable CMH solutions.
Acknowledgments
This work is part of the Startup project (number 31T131) funded by the United Arab Emirates University (2019-2021).
Abbreviations
- CMH
connected mental health
- COVID-19
coronavirus disease
- EC
exclusion criteria
- e-mental
electronic mental
- ICT
information and communication technologies
- m-mental
mobile mental
- MQ
mapping question
- RCTs
randomized control trials
- WoS
Web of Science
Appendix
Classification results.
Footnotes
Authors' Contributions: All authors contributed to the creation of the manuscript. ND contributed to the design, conception, acquisition and interpretation of data, classification of selected papers, drafting of the manuscript, and revision. SO contributed to the design, conception, statistical support, interpretation of data, drafting of the manuscript, and critical revision. MJ, JL, and MG performed the critical revision. All authors have read and approved this manuscript.
Conflicts of Interest: LL is a shareholder of Salumedia Labs, which is a digital health company.
References
- 1.Westerhof GJ, Keyes CL. Mental illness and mental health: the two continua model across the lifespan. J Adult Dev. 2010 Jun;17(2):110–9. doi: 10.1007/s10804-009-9082-y. http://europepmc.org/abstract/MED/20502508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sawyer MG, Whaites L, Rey JM, Hazell PL, Graetz BW, Baghurst P. Health-related quality of life of children and adolescents with mental disorders. J Am Acad Child Adolesc Psychiatry. 2002 May;41(5):530–7. doi: 10.1097/00004583-200205000-00010. [DOI] [PubMed] [Google Scholar]
- 3.Prince M, Patel V, Saxena S, Maj M, Maselko J, Phillips MR, Rahman A. No health without mental health. Lancet. 2007 Sep 8;370(9590):859–77. doi: 10.1016/S0140-6736(07)61238-0. [DOI] [PubMed] [Google Scholar]
- 4.Patel V, Flisher AJ, Hetrick S, McGorry P. Mental health of young people: a global public-health challenge. Lancet. 2007 Apr 14;369(9569):1302–13. doi: 10.1016/S0140-6736(07)60368-7. [DOI] [PubMed] [Google Scholar]
- 5.Layard R. Mental Illness Destroys Happiness and is Costless to Treat. Global Happiness. 2018. [2020-04-30]. http://ghc-2018.s3.amazonaws.com/GHC_Ch3.pdf.
- 6.Sachs SJ, Layard R, Helliwell J. World Happiness Report 2018. AWS. 2018. [2020-04-30]. https://s3.amazonaws.com/happiness-report/2018/WHR_web.pdf.
- 7.Collins PY, Patel V, Joestl SS, March D, Insel TR, Daar AS, Anderson W, Dhansay MA, Phillips A, Shurin S, Walport M, Ewart W, Savill SJ, Bordin IA, Costello EJ, Durkin M, Fairburn C, Glass RI, Hall W, Huang Y, Hyman SE, Jamison K, Kaaya S, Kapur S, Kleinman A, Ogunniyi A, Otero-Ojeda A, Poo MM, Ravindranath V, Sahakian BJ, Saxena S, Singer PA, Stein DJ. Grand challenges in global mental health. Nature. 2011 Jul 6;475(7354):27–30. doi: 10.1038/475027a. http://europepmc.org/abstract/MED/21734685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Patel V, Prince M. Global mental health: a new global health field comes of age. J Am Med Assoc. 2010 May 19;303(19):1976–7. doi: 10.1001/jama.2010.616. http://europepmc.org/abstract/MED/20483977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rowan K, McAlpine DD, Blewett LA. Access and cost barriers to mental health care, by insurance status, 1999-2010. Health Aff (Millwood) 2013 Oct;32(10):1723–30. doi: 10.1377/hlthaff.2013.0133. http://europepmc.org/abstract/MED/24101061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cunningham PJ. Beyond parity: primary care physicians' perspectives on access to mental health care. Health Aff (Millwood) 2009;28(3):w490–501. doi: 10.1377/hlthaff.28.3.w490. [DOI] [PubMed] [Google Scholar]
- 11.Gulliver A, Griffiths KM, Christensen H. Perceived barriers and facilitators to mental health help-seeking in young people: a systematic review. BMC Psychiatry. 2010 Dec 30;10:113. doi: 10.1186/1471-244X-10-113. https://bmcpsychiatry.biomedcentral.com/articles/10.1186/1471-244X-10-113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Snowden LR. Barriers to effective mental health services for African Americans. Ment Health Serv Res. 2001 Dec;3(4):181–7. doi: 10.1023/a:1013172913880. [DOI] [PubMed] [Google Scholar]
- 13.Coronavirus. World Health Organization. [2020-04-30]. https://www.who.int/health-topics/coronavirus#tab=tab_1.
- 14.Coronavirus Disease (COVID-19) Weekly Epidemiological Update and Weekly Operational Update. World Health Organization. 2020. [2020-04-30]. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports.
- 15.Anxiety on Rise Due to Coronavirus, Say Mental Health Charities. The Guardian. [2020-04-30]. https://www.theguardian.com/world/2020/mar/13/anxiety-on-rise-due-to-coronavirus-say-mental-health-charities.
- 16.Mental Health and Psychosocial Considerations During the Covid-19 Outbreak. World Health Organization. [2020-04-30]. https://www.who.int/docs/default-source/coronaviruse/mental-health-considerations.pdf?sfvrsn=6d3578af_2.
- 17.Coronavirus Disease (COVID-19) Advice for the Public. World Health Organization. 2020. [2020-04-30]. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public.
- 18.Schmidt U, Wykes T. E-mental health - a land of unlimited possibilities. J Ment Health. 2012 Aug;21(4):327–31. doi: 10.3109/09638237.2012.705930. [DOI] [PubMed] [Google Scholar]
- 19.Caulfield BM, Donnelly SC. What is Connected Health and why will it change your practice? QJM. 2013 Aug;106(8):703–7. doi: 10.1093/qjmed/hct114. [DOI] [PubMed] [Google Scholar]
- 20.Karampela M, Isomursu M, Porat T, Maramis C, Mountford N, Giunti G, Chouvarda I, Lehocki F. The extent and coverage of current knowledge of connected health: systematic mapping study. J Med Internet Res. 2019 Sep 25;21(9):e14394. doi: 10.2196/14394. https://www.jmir.org/2019/9/e14394/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Nicholas J, Huckvale K, Larsen ME, Basu A, Batterham PJ, Shaw F, Sendi S. Issues for ehealth in psychiatry: results of an expert survey. J Med Internet Res. 2017 Feb 28;19(2):e55. doi: 10.2196/jmir.6957. https://www.jmir.org/2017/2/e55/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lal S, Adair CE. E-mental health: a rapid review of the literature. Psychiatr Serv. 2014 Jan 1;65(1):24–32. doi: 10.1176/appi.ps.201300009. [DOI] [PubMed] [Google Scholar]
- 23.Helen C, Griffiths K, Evans K. e-Mental health in Australia: Implications of the Internet and related technologies for policy. Canberra: Commonwealth Department of Health and Ageing; 2002. [Google Scholar]
- 24.Sood S, Mbarika V, Jugoo S, Dookhy R, Doarn CR, Prakash N, Merrell RC. What is telemedicine? A collection of 104 peer-reviewed perspectives and theoretical underpinnings. Telemed J E Health. 2007 Oct;13(5):573–90. doi: 10.1089/tmj.2006.0073. [DOI] [PubMed] [Google Scholar]
- 25.Bauer S, Moessner M. Technology-enhanced monitoring in psychotherapy and e-mental health. J Ment Health. 2012 Aug;21(4):355–63. doi: 10.3109/09638237.2012.667886. [DOI] [PubMed] [Google Scholar]
- 26.Wade VA, Karnon J, Elshaug AG, Hiller JE. A systematic review of economic analyses of telehealth services using real time video communication. BMC Health Serv Res. 2010 Aug 10;10:233. doi: 10.1186/1472-6963-10-233. https://bmchealthservres.biomedcentral.com/articles/10.1186/1472-6963-10-233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mitrpanont J, Phandhu-Fung J, Klubdee N, Ratanalaor S, Mitrpanont T. iCare-Stress: An Integrated Mental Health Software. 2nd International Conference on Information Technology; INCIT'17; November 2-3, 2017; Nakhonpathom, Thailand. 2017. [DOI] [Google Scholar]
- 28.Owen JE, Kuhn E, Jaworski BK, McGee-Vincent P, Juhasz K, Hoffman JE, Rosen C. VA mobile apps for PTSD and related problems: public health resources for veterans and those who care for them. Mhealth. 2018;4:28. doi: 10.21037/mhealth.2018.05.07. doi: 10.21037/mhealth.2018.05.07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Batterham PJ, Calear AL, Farrer L, McCallum SM, Cheng VW. Randomised controlled trial of an automatically tailored online program for mood, anxiety, substance use and suicidality. Internet Interv. 2018 Jun;12:91–9. doi: 10.1016/j.invent.2017.08.002. https://linkinghub.elsevier.com/retrieve/pii/S2214-7829(17)30064-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Jani HM. Benefiting From Online Mental Status Examination System and Mental Health Diagnostic System. 3rd International Conference on Information Sciences and Interaction Sciences; ICICIS'10; June 23-25, 2010; Chengdu, China. 2010. [DOI] [Google Scholar]
- 31.Sahu SS, Sharma A. Detecting Brainwaves to Evaluate Mental Health Using Labview and Applications. International Conference on Emerging Technological Trends; ICETT'16; October 21-22, 2016; Kollam, India. 2016. [DOI] [Google Scholar]
- 32.Pham TD, Thang T, Oyama-Higa M. Toward the Development of a Cost-effective E-depression Detection System. International Conference on Computerized Healthcare; ICCH'12; December 17-18, 2012; Hong Kong, China. 2012. [DOI] [Google Scholar]
- 33.Peterson K, Feldt R, Mujtaba S, Mattsson M. Systematic Mapping Studies in Software Engineering. 12th International Conference on Evaluation and Assessment in Software Engineering; EASE'08; June 26-27, 2008; Bari, Italy. 2008. [DOI] [Google Scholar]
- 34.Petersen K, Vakkalanka S, Kuzniarz L. Guidelines for conducting systematic mapping studies in software engineering: an update. Inform Software Tech. 2015 Aug;64:1–18. doi: 10.1016/j.infsof.2015.03.007. [DOI] [Google Scholar]
- 35.Montoya FG, Alcayde A, Baños R, Manzano-Agugliaro F. A fast method for identifying worldwide scientific collaborations using the Scopus database. Telematics and Informatics. 2018 Apr;35(1):168–85. doi: 10.1016/j.tele.2017.10.010. [DOI] [Google Scholar]
- 36.Hamel RE. The dominance of English in the international scientific periodical literature and the future of language use in science. Aila Rev. 2008 Mar 7;20:53–71. doi: 10.1075/aila.20.06ham. [DOI] [Google Scholar]
- 37.Ammon U. The Dominance of English as a Language of Science: Effects on Other Languages and Language Communities. New York, USA: Walter de Gruyter; 2011. [Google Scholar]
- 38.Liverpool S, Webber H, Matthews R, Wolpert M, Edbrooke-Childs J. A mobile app to support parents making child mental health decisions: protocol for a feasibility cluster randomized controlled trial. JMIR Res Protoc. 2019 Aug 14;8(8):e14571. doi: 10.2196/14571. https://www.researchprotocols.org/2019/8/e14571/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Schueller SM, Glover AC, Rufa AK, Dowdle CL, Gross GD, Karnik NS, Zalta AK. A mobile phone-based intervention to improve mental health among homeless young adults: pilot feasibility trial. JMIR Mhealth Uhealth. 2019 Jul 2;7(7):e12347. doi: 10.2196/12347. https://mhealth.jmir.org/2019/7/e12347/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Coelhoso CC, Tobo PR, Lacerda SS, Lima AH, Barrichello CR, Amaro E, Kozasa EH. A new mental health mobile app for well-being and stress reduction in working women: randomized controlled trial. J Med Internet Res. 2019 Nov 7;21(11):e14269. doi: 10.2196/14269. https://www.jmir.org/2019/11/e14269/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Garabiles MR, Harper Shehadeh M, Hall BJ. Cultural adaptation of a scalable world health organization e-mental health program for overseas Filipino workers. JMIR Form Res. 2019 Mar 29;3(1):e11600. doi: 10.2196/11600. https://formative.jmir.org/2019/1/e11600/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Greer B, Robotham D, Simblett S, Curtis H, Griffiths H, Wykes T. Digital exclusion among mental health service users: qualitative investigation. J Med Internet Res. 2019 Jan 9;21(1):e11696. doi: 10.2196/11696. https://www.jmir.org/2019/1/e11696/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Lattie EG, Adkins EC, Winquist N, Stiles-Shields C, Wafford QE, Graham AK. Digital mental health interventions for depression, anxiety, and enhancement of psychological well-being among college students: systematic review. J Med Internet Res. 2019 Jul 22;21(7):e12869. doi: 10.2196/12869. https://www.jmir.org/2019/7/e12869/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Smail-Crevier R, Powers G, Noel C, Wang J. Health-related internet usage and design feature preference for e-mental health programs among men and women. J Med Internet Res. 2019 Mar 18;21(3):e11224. doi: 10.2196/11224. https://www.jmir.org/2019/3/e11224/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Birk MV, Mandryk RL. Improving the efficacy of cognitive training for digital mental health interventions through avatar customization: crowdsourced quasi-experimental study. J Med Internet Res. 2019 Jan 8;21(1):e10133. doi: 10.2196/10133. https://www.jmir.org/2019/1/e10133/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Thomas K, Bendtsen M. Mental health promotion among university students using text messaging: protocol for a randomized controlled trial of a mobile phone-based intervention. JMIR Res Protoc. 2019 Aug 15;8(8):e12396. doi: 10.2196/12396. https://www.researchprotocols.org/2019/8/e12396/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Anastasiadou D, Folkvord F, Serrano-Troncoso E, Lupiañez-Villanueva F. Mobile health adoption in mental health: user experience of a mobile health app for patients with an eating disorder. JMIR Mhealth Uhealth. 2019 May 31;7(6):e12920. doi: 10.2196/12920. https://mhealth.jmir.org/2019/6/e12920/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Andrews JA, Brown L, Hawley M, Astell A. Older adults' perspectives on using digital technology to maintain good mental health: interactive group study. J Med Internet Res. 2019 Feb 13;21(2):e11694. doi: 10.2196/11694. https://www.jmir.org/2019/2/e11694/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Mandryk RL, Birk MV. The potential of game-based digital biomarkers for modeling mental health. JMIR Ment Health. 2019 Apr 23;6(4):e13485. doi: 10.2196/13485. https://mental.jmir.org/2019/4/e13485/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Scholten H, Granic I. Use of the principles of design thinking to address limitations of digital mental health interventions for youth: viewpoint. J Med Internet Res. 2019 Jan 14;21(1):e11528. doi: 10.2196/11528. https://www.jmir.org/2019/1/e11528/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Thornton L, Kay-Lambkin F, Tebbutt B, Hanstock TL, Baker AL. A mobile phone-based healthy lifestyle monitoring tool for people with mental health problems (MyHealthPA): development and pilot testing. JMIR Cardio. 2018 Oct 1;2(2):e10228. doi: 10.2196/10228. https://cardio.jmir.org/2018/2/e10228/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Kaur A, Isaranuwatchai W, Jaffer A, Ferguson G, Abi-Jaoude A, Johnson A, Hollenberg E, Wiljer D. A web- and mobile-based map of mental health resources for postsecondary students (Thought Spot): protocol for an economic evaluation. JMIR Res Protoc. 2018 Mar 29;7(3):e83. doi: 10.2196/resprot.9478. https://www.researchprotocols.org/2018/3/e83/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Zelmer J, van Hoof K, Notarianni M, van Mierlo T, Schellenberg M, Tannenbaum C. An assessment framework for e-mental health apps in Canada: results of a modified delphi process. JMIR Mhealth Uhealth. 2018 Jul 9;6(7):e10016. doi: 10.2196/10016. https://mhealth.jmir.org/2018/7/e10016/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.March S, Day J, Ritchie G, Rowe A, Gough J, Hall T, Yuen CY, Donovan CL, Ireland M. Attitudes toward e-mental health services in a community sample of adults: online survey. J Med Internet Res. 2018 Feb 19;20(2):e59. doi: 10.2196/jmir.9109. https://www.jmir.org/2018/2/e59/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Carolan S, de Visser RO. Employees' perspectives on the facilitators and barriers to engaging with digital mental health interventions in the workplace: qualitative study. JMIR Ment Health. 2018 Jan 19;5(1):e8. doi: 10.2196/mental.9146. https://mental.jmir.org/2018/1/e8/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Hatch A, Hoffman JE, Ross R, Docherty JP. Expert consensus survey on digital health tools for patients with serious mental illness: optimizing for user characteristics and user support. JMIR Ment Health. 2018 Jun 12;5(2):e46. doi: 10.2196/mental.9777. https://mental.jmir.org/2018/2/e46/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Palmius N, Saunders KE, Carr O, Geddes JR, Goodwin GM, De Vos M. Group-personalized regression models for predicting mental health scores from objective mobile phone data streams: observational study. J Med Internet Res. 2018 Oct 22;20(10):e10194. doi: 10.2196/10194. https://www.jmir.org/2018/10/e10194/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Sano A, Taylor S, McHill AW, Phillips AJ, Barger LK, Klerman E, Picard R. Identifying objective physiological markers and modifiable behaviors for self-reported stress and mental health status using wearable sensors and mobile phones: observational study. J Med Internet Res. 2018 Jun 8;20(6):e210. doi: 10.2196/jmir.9410. https://www.jmir.org/2018/6/e210/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.di Matteo D, Fine A, Fotinos K, Rose J, Katzman M. Patient willingness to consent to mobile phone data collection for mental health apps: structured questionnaire. JMIR Ment Health. 2018 Aug 29;5(3):e56. doi: 10.2196/mental.9539. https://mental.jmir.org/2018/3/e56/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Boonstra TW, Nicholas J, Wong QJ, Shaw F, Townsend S, Christensen H. Using mobile phone sensor technology for mental health research: integrated analysis to identify hidden challenges and potential solutions. J Med Internet Res. 2018 Jul 30;20(7):e10131. doi: 10.2196/10131. https://www.jmir.org/2018/7/e10131/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Mohr DC, Lyon AR, Lattie EG, Reddy M, Schueller SM. Accelerating digital mental health research from early design and creation to successful implementation and sustainment. J Med Internet Res. 2017 May 10;19(5):e153. doi: 10.2196/jmir.7725. https://www.jmir.org/2017/5/e153/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Bidargaddi N, Musiat P, Winsall M, Vogl G, Blake V, Quinn S, Orlowski S, Antezana G, Schrader G. Efficacy of a web-based guided recommendation service for a curated list of readily available mental health and well-being mobile apps for young people: randomized controlled trial. J Med Internet Res. 2017 May 12;19(5):e141. doi: 10.2196/jmir.6775. https://www.jmir.org/2017/5/e141/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Grist R, Porter J, Stallard P. Mental health mobile apps for preadolescents and adolescents: a systematic review. J Med Internet Res. 2017 May 25;19(5):e176. doi: 10.2196/jmir.7332. https://www.jmir.org/2017/5/e176/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Rathbone AL, Prescott J. The use of mobile apps and SMS messaging as physical and mental health interventions: systematic review. J Med Internet Res. 2017 Aug 24;19(8):e295. doi: 10.2196/jmir.7740. https://www.jmir.org/2017/8/e295/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Mandryk RL, Birk MV. Toward game-based digital mental health interventions: player habits and preferences. J Med Internet Res. 2017 Apr 20;19(4):e128. doi: 10.2196/jmir.6906. https://www.jmir.org/2017/4/e128/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Bennett-Levy J, Singer J, DuBois S, Hyde K. Translating e-mental health into practice: what are the barriers and enablers to e-mental health implementation by aboriginal and Torres Strait Islander health professionals? J Med Internet Res. 2017 Jan 11;19(1):e1. doi: 10.2196/jmir.6269. https://www.jmir.org/2017/1/e1/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Berry N, Lobban F, Emsley R, Bucci S. Acceptability of interventions delivered online and through mobile phones for people who experience severe mental health problems: a systematic review. J Med Internet Res. 2016 May 31;18(5):e121. doi: 10.2196/jmir.5250. https://www.jmir.org/2016/5/e121/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Robotham D, Satkunanathan S, Doughty L, Wykes T. Do we still have a digital divide in mental health? A five-year survey follow-up. J Med Internet Res. 2016 Nov 22;18(11):e309. doi: 10.2196/jmir.6511. https://www.jmir.org/2016/11/e309/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Meurk C, Leung J, Hall W, Head BW, Whiteford H. Establishing and governing e-mental health care in Australia: a systematic review of challenges and a call for policy-focussed research. J Med Internet Res. 2016 Jan 13;18(1):e10. doi: 10.2196/jmir.4827. https://www.jmir.org/2016/1/e10/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Berrouiguet S, Baca-García E, Brandt S, Walter M, Courtet P. Fundamentals for future mobile-health (mhealth): a systematic review of mobile phone and web-based text messaging in mental health. J Med Internet Res. 2016 Jun 10;18(6):e135. doi: 10.2196/jmir.5066. https://www.jmir.org/2016/6/e135/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Kahn JR, Collinge W, Soltysik R. Post-9/11 veterans and their partners improve mental health outcomes with a self-directed mobile and web-based wellness training program: a randomized controlled trial. J Med Internet Res. 2016 Sep 27;18(9):e255. doi: 10.2196/jmir.5800. https://www.jmir.org/2016/9/e255/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Younes N, Chollet A, Menard E, Melchior M. E-mental health care among young adults and help-seeking behaviors: a transversal study in a community sample. J Med Internet Res. 2015 May 15;17(5):e123. doi: 10.2196/jmir.4254. https://www.jmir.org/2015/5/e123/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Torous J, Friedman R, Keshavan M. Smartphone ownership and interest in mobile applications to monitor symptoms of mental health conditions. JMIR Mhealth Uhealth. 2014 Jan 21;2(1):e2. doi: 10.2196/mhealth.2994. https://mhealth.jmir.org/2014/1/e2/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Ellis LA, Collin P, Davenport TA, Hurley PJ, Burns JM, Hickie IB. Young men, mental health, and technology: implications for service design and delivery in the digital age. J Med Internet Res. 2012 Nov 22;14(6):e160. doi: 10.2196/jmir.2291. https://www.jmir.org/2012/6/e160/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Mohr DC, Duffecy J, Jin L, Ludman EJ, Lewis A, Begale M, McCarthy M. Multimodal e-mental health treatment for depression: a feasibility trial. J Med Internet Res. 2010 Dec 19;12(5):e48. doi: 10.2196/jmir.1370. https://www.jmir.org/2010/5/e48/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Bennett K, Bennett AJ, Griffiths KM. Security considerations for e-mental health interventions. J Med Internet Res. 2010 Dec 19;12(5):e61. doi: 10.2196/jmir.1468. https://www.jmir.org/2010/5/e61/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Mucic Davor., editor. E-Mental Health. Cham, UK: Springer; 2015. [Google Scholar]
- 78.Shoemaker EZ, Hilty DM. E-Mental Health. Cham, UK: Springer; 2016. E-mental health improves access to care, facilitates early intervention, and provides evidence-based treatments at a distance; pp. 43–57. [Google Scholar]
- 79.Mucic D, Hilty DM, Yellowlees PM. E-Mental health. Cham, UK: Springer; 2016. E-Mental health toward cross-cultural populations worldwide; pp. 77–91. [Google Scholar]
- 80.Yellowlees PM, Hilty. DM, Mucic D. E-mental health. Cham, UK: Springer; 2016. Global/worldwide e-mental health: international and futuristic perspectives of telepsychiatry and the future; pp. 233–249. [Google Scholar]
- 81.Donald H, Barb J, Robert MM. E-Mental Health. Cham, UK: Springer; 2016. How e-mental health adds to traditional outpatient and newer models of integrated care for patients, providers, and systems; pp. 129–49. [Google Scholar]
- 82.Donald MH, Erica ZS, Jay S. E-Mental Health. Cham, UK: Springer; 2016. How to build, evaluate, and increase your e-mental health program efficiency; pp. 59–76. [Google Scholar]
- 83.Donald MH, Davor M. E-Mental Health. Cham, UK: Springer; 2016. Technology, health, and contemporary practice: How does e-mental health fit it and what does it offer? pp. 3–27. [Google Scholar]
- 84.Hilty DM, Yellowlees P, Myers K, Parish M, Rabinowitz T. E-mental Health. Cham, UK: Springer; 2016. The effectiveness of e-mental healthvidence base, how to choose the model based on ease/cost/strength, and future areas of research; pp. 95–127. [Google Scholar]
- 85.Clough BA, Zarean M, Ruane I, Mateo NJ, Aliyeva TA, Casey LM. Going global: do consumer preferences, attitudes, and barriers to using e-mental health services differ across countries? J Ment Health. 2019 Feb;28(1):17–25. doi: 10.1080/09638237.2017.1370639. [DOI] [PubMed] [Google Scholar]
- 86.Kirst M, Pridham KF, Narrandes R, Matheson F, Young L, Niedra K, Stergiopoulos V. Examining implementation of mobile, police-mental health crisis intervention teams in a large urban center. J Ment Health. 2015 Dec;24(6):369–74. doi: 10.3109/09638237.2015.1036970. [DOI] [PubMed] [Google Scholar]
- 87.Ennis L, Rose D, Denis M, Pandit N, Wykes T. Can't surf, won't surf: the digital divide in mental health. J Ment Health. 2012 Aug;21(4):395–403. doi: 10.3109/09638237.2012.689437. http://europepmc.org/abstract/MED/22712756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Musiat P, Hoffmann L, Schmidt U. Personalised computerised feedback in e-mental health. J Ment Health. 2012 Aug;21(4):346–54. doi: 10.3109/09638237.2011.648347. [DOI] [PubMed] [Google Scholar]
- 89.Harrison V, Proudfoot J, Wee PP, Parker G, Pavlovic DH, Manicavasagar V. Mobile mental health: review of the emerging field and proof of concept study. J Ment Health. 2011 Dec;20(6):509–24. doi: 10.3109/09638237.2011.608746. [DOI] [PubMed] [Google Scholar]
- 90.Berry N, Lobban F, Bucci S. A qualitative exploration of service user views about using digital health interventions for self-management in severe mental health problems. BMC Psychiatry. 2019 Jan 21;19(1):35. doi: 10.1186/s12888-018-1979-1. https://bmcpsychiatry.biomedcentral.com/articles/10.1186/s12888-018-1979-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Dreier M, Ludwig J, Härter M, von dem Knesebeck O, Baumgardt J, Bock T, Dirmaier J, Kennedy AJ, Brumby SA, Liebherz S. Development and evaluation of e-mental health interventions to reduce stigmatization of suicidality - a study protocol. BMC Psychiatry. 2019 May 17;19(1):152. doi: 10.1186/s12888-019-2137-0. https://bmcpsychiatry.biomedcentral.com/articles/10.1186/s12888-019-2137-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Metz MJ, Elfeddali I, Krol DG, Veerbeek MA, de Beurs E, Beekman AT, van der Feltz-Cornelis CM. A digital intake approach in specialized mental health care: study protocol of a cluster randomised controlled trial. BMC Psychiatry. 2017 Mar 7;17(1):86. doi: 10.1186/s12888-017-1247-9. https://bmcpsychiatry.biomedcentral.com/articles/10.1186/s12888-017-1247-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Agyapong VIO, Mrklas K, Juhás M, Omeje J, Ohinmaa A, Dursun SM, Greenshaw AJ. Cross-sectional survey evaluating Text4Mood: mobile health program to reduce psychological treatment gap in mental healthcare in Alberta through daily supportive text messages. BMC Psychiatry. 2016 Nov 8;16(1):378. doi: 10.1186/s12888-016-1104-2. https://bmcpsychiatry.biomedcentral.com/articles/10.1186/s12888-016-1104-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Clarke J, Proudfoot J, Birch M, Whitton AE, Parker G, Manicavasagar V, Harrison V, Christensen H, Hadzi-Pavlovic D. Effects of mental health self-efficacy on outcomes of a mobile phone and web intervention for mild-to-moderate depression, anxiety and stress: secondary analysis of a randomised controlled trial. BMC Psychiatry. 2014 Sep 26;14:272. doi: 10.1186/s12888-014-0272-1. https://bmcpsychiatry.biomedcentral.com/articles/10.1186/s12888-014-0272-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Krieger T, Meyer B, Sude K, Urech A, Maercker A, Berger T. Evaluating an e-mental health program ('deprexis') as adjunctive treatment tool in psychotherapy for depression: design of a pragmatic randomized controlled trial. BMC Psychiatry. 2014 Oct 8;14:285. doi: 10.1186/s12888-014-0285-9. https://bmcpsychiatry.biomedcentral.com/articles/10.1186/s12888-014-0285-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Musiat P, Goldstone P, Tarrier N. Understanding the acceptability of e-mental health--attitudes and expectations towards computerised self-help treatments for mental health problems. BMC Psychiatry. 2014 Apr 11;14:109. doi: 10.1186/1471-244X-14-109. https://bmcpsychiatry.biomedcentral.com/articles/10.1186/1471-244X-14-109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Ben-Zeev D, Buck B, Hallgren K, Drake RE. Effect of mobile health on in-person service use among people with serious mental illness. Psychiatr Serv. 2019 Jun 1;70(6):507–10. doi: 10.1176/appi.ps.201800542. [DOI] [PubMed] [Google Scholar]
- 98.Fortuna KL, Walker R, Fisher DB, Mois G, Allan S, Deegan PE. Enhancing standards and principles in digital mental health with recovery-focused guidelines for mobile, online, and remote monitoring technologies. Psychiatr Serv. 2019 Dec 1;70(12):1080–1. doi: 10.1176/appi.ps.201900166. http://europepmc.org/abstract/MED/31615369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Torous J, Haim A. Dichotomies in the development and implementation of digital mental health tools. Psychiatr Serv. 2018 Dec 1;69(12):1204–6. doi: 10.1176/appi.ps.201800193. http://europepmc.org/abstract/MED/30256182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Ben-Zeev D, Brian RM, Jonathan G, Razzano L, Pashka N, Carpenter-Song E, Drake RE, Scherer EA. Mobile health (mhealth) versus clinic-based group intervention for people with serious mental illness: a randomized controlled trial. Psychiatr Serv. 2018 Sep 1;69(9):978–85. doi: 10.1176/appi.ps.201800063. [DOI] [PubMed] [Google Scholar]
- 101.Ben-Zeev D. Mobile health for mental health in West Africa: the case for Ghana. Psychiatr Serv. 2018 Jul 1;69(7):741–3. doi: 10.1176/appi.ps.201700555. [DOI] [PubMed] [Google Scholar]
- 102.van der Krieke L, Wunderink L, Emerencia AC, de Jonge P, Sytema S. E-mental health self-management for psychotic disorders: state of the art and future perspectives. Psychiatr Serv. 2014 Jan 1;65(1):33–49. doi: 10.1176/appi.ps.201300050. [DOI] [PubMed] [Google Scholar]
- 103.Iorfino F, Cross SP, Davenport T, Carpenter JS, Scott E, Shiran S, Hickie IB. A digital platform designed for youth mental health services to deliver personalized and measurement-based care. Front Psychiatry. 2019;10:595. doi: 10.3389/fpsyt.2019.00595. doi: 10.3389/fpsyt.2019.00595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Bucci S, Berry N, Morris R, Berry K, Haddock G, Lewis S, Edge D. 'They are not hard-to-reach clients. We have just got hard-to-reach services.' staff views of digital health tools in specialist mental health services. Front Psychiatry. 2019;10:344. doi: 10.3389/fpsyt.2019.00344. doi: 10.3389/fpsyt.2019.00344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Seifert A, Reinwand DA, Schlomann A. Designing and using digital mental health interventions for older adults: being aware of digital inequality. Front Psychiatry. 2019;10:568. doi: 10.3389/fpsyt.2019.00568. doi: 10.3389/fpsyt.2019.00568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Burchert S, Alkneme MS, Bird M, Carswell K, Cuijpers P, Hansen P, Heim E, Harper Shehadeh M, Sijbrandij M, van't Hof E, Knaevelsrud C. User-centered app adaptation of a low-intensity e-mental health intervention for Syrian refugees. Front Psychiatry. 2019;9:663. doi: 10.3389/fpsyt.2018.00663. doi: 10.3389/fpsyt.2018.00663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Garrido S, Millington C, Cheers D, Boydell K, Schubert E, Meade T, Nguyen QV. What works and what doesn't work? A systematic review of digital mental health interventions for depression and anxiety in young people. Front Psychiatry. 2019;10:759. doi: 10.3389/fpsyt.2019.00759. doi: 10.3389/fpsyt.2019.00759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Ebert DD, Cuijpers P, Muñoz RF, Baumeister H. Prevention of mental health disorders using internet- and mobile-based interventions: a narrative review and recommendations for future research. Front Psychiatry. 2017;8:116. doi: 10.3389/fpsyt.2017.00116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Rehm IC, Foenander E, Wallace K, Abbott JM, Kyrios M, Thomas N. What role can avatars play in e-mental health interventions? Exploring new models of client-therapist interaction. Front Psychiatry. 2016;7:186. doi: 10.3389/fpsyt.2016.00186. doi: 10.3389/fpsyt.2016.00186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Bucci S, Ainsworth J, Barrowclough C, Lewis S, Haddock G, Berry K, Emsley R, Edge D, Machin M. A theory-informed digital health intervention in people with severe mental health problems. Stud Health Technol Inform. 2019 Aug 21;264:526–30. doi: 10.3233/SHTI190278. [DOI] [PubMed] [Google Scholar]
- 111.Househ M, Alam T, Al-Thani D, Schneider J, Siddig M, Fernandez-Luque L, Qaraqe M, Alfuquha A, Saxena S. Developing a Digital Mental Health Platform for the Arab World: From Research to Action. ICIMTH; July 2019; Athens, Greece. 2019. Jul 04, pp. 392–395. http://ebooks.iospress.nl/publication/51763. [DOI] [PubMed] [Google Scholar]
- 112.Peyton D, Hiscock H, Sciberras E. Do digital health interventions improve mental health literacy or help-seeking among parents of children aged 2-12 years? A scoping review. Stud Health Technol Inform. 2019 Aug 8;266:156–61. doi: 10.3233/SHTI190788. [DOI] [PubMed] [Google Scholar]
- 113.Strudwick G, Booth R, Strauss J. Identifying how patient portals may be effectively used among mental health populations to support digital inclusion: a study protocol. Stud Health Technol Inform. 2018;250:30. [PubMed] [Google Scholar]
- 114.Wang J, Lam RW, Ho K, Attridge M, Lashewicz BM, Patten SB, Marchand A, Aiken A, Schmitz N, Gundu S, Rewari N, Hodgins D, Bulloch A, Merali Z. Preferred features of e-mental health programs for prevention of major depression in male workers: results from a Canadian national survey. J Med Internet Res. 2016 Jun 6;18(6):e132. doi: 10.2196/jmir.5685. https://www.jmir.org/2016/6/e132/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Perlich A, von Thienen J, Meinel C. Supporting talk-based mental health interventions with digital whiteboards. Stud Health Technol Inform. 2014;205:433–7. [PubMed] [Google Scholar]
- 116.Naslund JA, Gonsalves PP, Gruebner O, Pendse SR, Smith SL, Sharma A, Raviola G. Digital innovations for global mental health: opportunities for data science, task sharing, and early intervention. Curr Treat Options Psychiatry. 2019 Dec;6(4):337–51. doi: 10.1007/s40501-019-00186-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Boumparis N, Schulte MH, Riper H. Digital mental health for alcohol and substance use disorders. Curr Treat Options Psych. 2019 Nov 26;6(4):352–66. doi: 10.1007/s40501-019-00190-y. [DOI] [Google Scholar]
- 118.Becker TD, Torous JB. Recent developments in digital mental health interventions for college and university students. Curr Treat Options Psych. 2019 Jun 14;6(3):210–20. doi: 10.1007/s40501-019-00178-8. [DOI] [Google Scholar]
- 119.Wykes T, Lipshitz J, Schueller SM. Towards the design of ethical standards related to digital mental health and all its applications. Curr Treat Options Psych. 2019 Jul 5;6(3):232–42. doi: 10.1007/s40501-019-00180-0. [DOI] [Google Scholar]
- 120.Schueller SM, Hunter JF, Figueroa C, Aguilera A. Use of digital mental health for marginalized and underserved populations. Curr Treat Options Psych. 2019 Jul 5;6(3):243–55. doi: 10.1007/s40501-019-00181-z. [DOI] [Google Scholar]
- 121.Magee JC, Adut S, Brazill K, Warnick S. Mobile app tools for identifying and managing mental health disorders in primary care. Curr Treat Options Psychiatry. 2018 Sep;5(3):345–62. doi: 10.1007/s40501-018-0154-0. http://europepmc.org/abstract/MED/30397577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Johnson KF, Kalkbrenner MT. The utilization of technological innovations to support college student mental health: mobile health communication. J Tech Hum Serv. 2017 Sep 11;35(4):314–39. doi: 10.1080/15228835.2017.1368428. [DOI] [Google Scholar]
- 123.East ML, Havard B, Hastings NB. Mental health mobile apps’ instruction: technology adoption theories applied in a mixed methods study of counseling faculty. J Tech Hum Serv. 2016 Oct 21;34(4):301–25. doi: 10.1080/15228835.2016.1233842. [DOI] [Google Scholar]
- 124.Mar MY, Neilson EK, Torchalla I, Werker GR, Laing A, Krausz M. Exploring e-mental health preferences of generation Y. J Tech Hum Serv. 2014 Nov 26;32(4):312–27. doi: 10.1080/15228835.2014.943457. [DOI] [Google Scholar]
- 125.Feng XL, Campbell A. Understanding e-mental health resources: personality, awareness, utilization, and effectiveness of e-mental health resources amongst youth. J Tech Hum Serv. 2011 Apr;29(2):101–19. doi: 10.1080/15228835.2011.595276. [DOI] [Google Scholar]
- 126.Zack JS. How sturdy is that digital couch? Legal considerations for mental health professionals who deliver clinical services via the internet. J Tech Hum Serv. 2008 Jul 3;26(2-4):333–59. doi: 10.1080/15228830802097083. [DOI] [Google Scholar]
- 127.Marshall JM, Dunstan DA, Bartik W. Smartphone psychology: new approaches towards safe and efficacious mobile mental health apps. Prof Psychol Res Pr. 2020 Jun;51(3):214–22. doi: 10.1037/pro0000278. [DOI] [Google Scholar]
- 128.Miller KE, Kuhn E, Yu J, Owen JE, Jaworski BK, Taylor K, Blonigen DM, Possemato K. Use and perceptions of mobile apps for patients among VA primary care mental and behavioral health providers. Prof Psychol Res Pr. 2019 Jun;50(3):204–9. doi: 10.1037/pro0000229. [DOI] [Google Scholar]
- 129.Lui JH, Marcus DK, Barry CT. Evidence-based apps? A review of mental health mobile applications in a psychotherapy context. Prof Psychol Res Pr. 2017 Jun;48(3):199–210. doi: 10.1037/pro0000122. [DOI] [Google Scholar]
- 130.Jones N, Moffitt M. Ethical guidelines for mobile app development within health and mental health fields. Professional Psychology: Research and Practice. 2016 Apr;47(2):155–162. doi: 10.1037/pro0000069. https://psycnet.apa.org/doiLanding?doi=10.1037%2Fpro0000069. [DOI] [Google Scholar]
- 131.Titov N, Dear BF, Staples LG, Bennett-Levy J, Klein B, Rapee RM, Andersson G, Purtell C, Bezuidenhout G, Nielssen OB. The first 30 months of the MindSpot clinic: evaluation of a national e-mental health service against project objectives. Aust N Z J Psychiatry. 2017 Dec;51(12):1227–39. doi: 10.1177/0004867416671598. [DOI] [PubMed] [Google Scholar]
- 132.Batterham PJ, Sunderland M, Calear AL, Davey CG, Christensen H, Teesson M, Kay-Lambkin F, Andrews G, Mitchell PB, Herrman H, Butow PN, Krouskos D. Developing a roadmap for the translation of e-mental health services for depression. Aust N Z J Psychiatry. 2015 Sep;49(9):776–84. doi: 10.1177/0004867415582054. [DOI] [PubMed] [Google Scholar]
- 133.Christensen H, Petrie K. State of the e-mental health field in Australia: where are we now? Aust N Z J Psychiatry. 2013 Feb;47(2):117–20. doi: 10.1177/0004867412471439. [DOI] [PubMed] [Google Scholar]
- 134.Jorm AF, Morgan AJ, Malhi GS. The future of e-mental health. Aust N Z J Psychiatry. 2013 Feb;47(2):104–6. doi: 10.1177/0004867412474076. [DOI] [PubMed] [Google Scholar]
- 135.Strauss P, Morgan H, Toussaint DW, Lin A, Winter S, Perry Y. Trans and gender diverse young people's attitudes towards game-based digital mental health interventions: a qualitative investigation. Internet Interv. 2019 Dec;18:100280. doi: 10.1016/j.invent.2019.100280. https://linkinghub.elsevier.com/retrieve/pii/S2214-7829(19)30047-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Apolinário-Hagen J, Fritsche L, Bierhals C, Salewski C. Improving attitudes toward e-mental health services in the general population via psychoeducational information material: a randomized controlled trial. Internet Interv. 2018 Jun;12:141–9. doi: 10.1016/j.invent.2017.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Schueller SM, Washburn JJ, Price M. Exploring mental health providers' interest in using web and mobile-based tools in their practices. Internet Interv. 2016 May;4(2):145–51. doi: 10.1016/j.invent.2016.06.004. http://europepmc.org/abstract/MED/28090438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Hensel JM, Ellard K, Koltek M, Wilson G, Sareen J. Digital health solutions for indigenous mental well-being. Curr Psychiatry Rep. 2019 Jul 1;21(8):68. doi: 10.1007/s11920-019-1056-6. http://europepmc.org/abstract/MED/31263971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Armontrout J, Torous J, Fisher M, Drogin E, Gutheil T. Mobile mental health: navigating new rules and regulations for digital tools. Curr Psychiatry Rep. 2016 Oct;18(10):91. doi: 10.1007/s11920-016-0726-x. [DOI] [PubMed] [Google Scholar]
- 140.Torous J, Staples P, Onnela J. Realizing the potential of mobile mental health: new methods for new data in psychiatry. Curr Psychiatry Rep. 2015 Aug;17(8):602. doi: 10.1007/s11920-015-0602-0. http://europepmc.org/abstract/MED/26073363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Zheng X, Woo BK. E-mental health in ethnic minority: a comparison of YouTube and talk-based educational workshops in dementia. Asian J Psychiatr. 2017 Feb;25:246–8. doi: 10.1016/j.ajp.2016.12.002. [DOI] [PubMed] [Google Scholar]
- 142.Brian RM, Ben-Zeev D. Mobile health (mHealth) for mental health in Asia: objectives, strategies, and limitations. Asian J Psychiatr. 2014 Aug;10:96–100. doi: 10.1016/j.ajp.2014.04.006. [DOI] [PubMed] [Google Scholar]
- 143.Aggarwal NK. Applying mobile technologies to mental health service delivery in South Asia. Asian J Psychiatr. 2012 Sep;5(3):225–30. doi: 10.1016/j.ajp.2011.12.009. [DOI] [PubMed] [Google Scholar]
- 144.Orman J, Clarke J, Whittle E, Anonuevo C, Proudfoot J. A diabetes-specific e-mental health tool: development, acceptability and outcomes of a feasibility study. Aust Fam Physician. 2016 Aug;45(8):600–5. http://www.racgp.org.au/afp/2016/august/a-diabetes-specific-e-mental-health-tool-development,-acceptability-and-outcomes-of-a-feasibility-study/ [PubMed] [Google Scholar]
- 145.Orman J, O'Dea B, Shand F, Berk M, Proudfoot J, Christensen H. e-Mental health for mood and anxiety disorders in general practice. Aust Fam Physician. 2014 Dec;43(12):832–7. [PubMed] [Google Scholar]
- 146.Reid SC, Kauer S, Khor A, Hearps S, Sanci L, Kennedy A, Patton G. Using a mobile phone application in youth mental health - an evaluation study. Aust Fam Physician. 2012 Sep;41(9):711–4. [PubMed] [Google Scholar]
- 147.Punukollu M, Marques M. Use of mobile apps and technologies in child and adolescent mental health: a systematic review. Evid Based Ment Health. 2019 Nov;22(4):161–6. doi: 10.1136/ebmental-2019-300093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Sheehan R, Hassiotis A. Digital mental health and intellectual disabilities: state of the evidence and future directions. Evid Based Ment Health. 2017 Nov;20(4):107–11. doi: 10.1136/eb-2017-102759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Davies EB, Craven MP, Martin JL, Simons L. Proportionate methods for evaluating a simple digital mental health tool. Evid Based Ment Health. 2017 Nov;20(4):112–7. doi: 10.1136/eb-2017-102755. http://europepmc.org/abstract/MED/28993317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Damen K, Van DS. Virtual Reality as e-Mental Health to Support Starting with Mindfulness-Based Cognitive Therapy. International Conference on Entertainment Computing; ICEC'18; September 18-20, 2018; Poznan, Poland. 2018. [DOI] [Google Scholar]
- 151.Chiou W, Kao C, Lo L, Huang D, Wang M, Chen B. Feasibility of Utilizing E-Mental Health with Mobile APP Interface for Social Support Enhencement: A Conceptional Solution for Postpartum Depression in Taiwan. International Conference of Design, User Experience, and Usability; DUXU'17; July 9-14, 2017; Vancouver, Canada. 2017. [DOI] [Google Scholar]
- 152.Martinez SG, Badillo-Urquiola K, Leis R, Chavez J, Green T, Clements T. Investigation of Multimodal Mobile Applications for Improving Mental Health. International Conference on Augmented Cognition; AC'16; July 17-22, 2016; Toronto, Canada. 2016. [DOI] [Google Scholar]
- 153.Fils-Aimé JR, Grelotti DJ, Thérosmé T, Kaiser BN, Raviola G, Alcindor Y, Severe J, Affricot E, Boyd K, Legha R, Daimyo S, Engel S, Eustache E. A mobile clinic approach to the delivery of community-based mental health services in rural Haiti. PLoS One. 2018;13(6):e0199313. doi: 10.1371/journal.pone.0199313. https://dx.plos.org/10.1371/journal.pone.0199313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Sprenger M, Mettler T, Osma J. Health professionals' perspective on the promotion of e-mental health apps in the context of maternal depression. PLoS One. 2017;12(7):e0180867. doi: 10.1371/journal.pone.0180867. https://dx.plos.org/10.1371/journal.pone.0180867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Ketelaar SM, Nieuwenhuijsen K, Gärtner FR, Bolier L, Smeets O, Sluiter JK. Effect of an e-mental health approach to workers' health surveillance versus control group on work functioning of hospital employees: a cluster-RCT. PLoS One. 2013;8(9):e72546. doi: 10.1371/journal.pone.0072546. https://dx.plos.org/10.1371/journal.pone.0072546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Neilsen A, Wilson RL. Combining e-mental health intervention development with human computer interaction (HCI) design to enhance technology-facilitated recovery for people with depression and/or anxiety conditions: an integrative literature review. Int J Ment Health Nurs. 2019 Feb;28(1):22–39. doi: 10.1111/inm.12527. [DOI] [PubMed] [Google Scholar]
- 157.de Vecchi N, Kenny A, Dickson-Swift V, Kidd S. How digital storytelling is used in mental health: a scoping review. Int J Ment Health Nurs. 2016 Jun;25(3):183–93. doi: 10.1111/inm.12206. [DOI] [PubMed] [Google Scholar]
- 158.Lee SJ, Thomas P, Doulis C, Bowles D, Henderson K, Keppich-Arnold S, Perez E, Stafrace S. Outcomes achieved by and police and clinician perspectives on a joint police officer and mental health clinician mobile response unit. Int J Ment Health Nurs. 2015 Dec;24(6):538–46. doi: 10.1111/inm.12153. [DOI] [PubMed] [Google Scholar]
- 159.Naslund JA, Aschbrenner KA, Barre LK, Bartels SJ. Feasibility of popular m-health technologies for activity tracking among individuals with serious mental illness. Telemed J E Health. 2015 Mar;21(3):213–6. doi: 10.1089/tmj.2014.0105. http://europepmc.org/abstract/MED/25536190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Chan S, Torous J, Hinton L, Yellowlees P. Towards a framework for evaluating mobile mental health apps. Telemed J E Health. 2015 Dec;21(12):1038–41. doi: 10.1089/tmj.2015.0002. [DOI] [PubMed] [Google Scholar]
- 161.Khasanshina EV, Wolfe WL, Emerson EN, Stachura ME. Counseling center-based tele-mental health for students at a rural university. Telemed J E Health. 2008 Feb;14(1):35–41. doi: 10.1089/tmj.2006.0038. [DOI] [PubMed] [Google Scholar]
- 162.Torous J, Kossowsky J. Digital Mental Health for Youth: New Evidence but Still Much Unknown. Psychiatric Times. 2018. [2020-08-19]. https://www.psychiatrictimes.com/view/digital-mental-health-youth-new-evidence-still-much-unknown.
- 163.Peek H. Harnessing Social Media and Mobile Apps for Mental Health. Psychiatric Times. 2015. [2020-08-19]. https://www.psychiatrictimes.com/view/harnessing-social-media-and-mobile-apps-mental-health.
- 164.Brooks L, Schirmer T. Mobile Apps for Mental Health. Psychiatric Times. 2014. https://www.psychiatrictimes.com/view/mobile-apps-mental-health.
- 165.Aschbrenner KA, Naslund JA, Tomlinson EF, Kinney A, Pratt SI, Brunette MF. Adolescents' use of digital technologies and preferences for mobile health coaching in public mental health settings. Front Public Health. 2019;7:178. doi: 10.3389/fpubh.2019.00178. doi: 10.3389/fpubh.2019.00178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Rojas G, Martínez V, Martínez P, Franco P, Jiménez-Molina A. Improving mental health care in developing countries through digital technologies: a mini narrative review of the Chilean case. Front Public Health. 2019;7:391. doi: 10.3389/fpubh.2019.00391. doi: 10.3389/fpubh.2019.00391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Moock J. Support from the internet for individuals with mental disorders: advantages and disadvantages of e-mental health service delivery. Front Public Health. 2014;2:65. doi: 10.3389/fpubh.2014.00065. doi: 10.3389/fpubh.2014.00065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Aryana B, Brewster L. Design for mobile mental health: exploring the informed participation approach. Health Informatics J. 2019;26(2):1208–24. doi: 10.1177/1460458219873540. [DOI] [PubMed] [Google Scholar]
- 169.Kenny R, Fitzgerald A, Segurado R, Dooley B. Is there an app for that? A cluster randomised controlled trial of a mobile app-based mental health intervention. Health Informatics J. 2019;26(3):1538–59. doi: 10.1177/1460458219884195. [DOI] [PubMed] [Google Scholar]
- 170.Kenny R, Dooley B, Fitzgerald A. Developing mental health mobile apps: exploring adolescents' perspectives. Health Informatics J. 2016 Jun;22(2):265–75. doi: 10.1177/1460458214555041. [DOI] [PubMed] [Google Scholar]
- 171.Sreejith G, Menon V. Mobile phones as a medium of mental health care service delivery: perspectives and barriers among patients with severe mental illness. Indian J Psychol Med. 2019;41(5):428–33. doi: 10.4103/IJPSYM.IJPSYM_333_18. http://europepmc.org/abstract/MED/31548765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Basavarajappa C, Chand P. Digital platforms for mental health-care delivery. Indian J Psychol Med. 2017;39(5):703–6. doi: 10.4103/IJPSYM.IJPSYM_209_17. http://europepmc.org/abstract/MED/29200576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Singh G, Manjunatha N, Rao S, Shashidhara H, Moirangthem S, Madegowda R, Binukumar B, Varghese M. Use of mobile phone technology to improve follow-up at a community mental health clinic: a randomized control trial. Indian J Psychol Med. 2017;39(3):276–80. doi: 10.4103/0253-7176.207325. http://europepmc.org/abstract/MED/28615760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Graham AK, Lattie EG, Mohr DC. Experimental therapeutics for digital mental health. JAMA Psychiatry. 2019 Aug 21;:-. doi: 10.1001/jamapsychiatry.2019.2075. epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Torous J, Roberts LW. Needed innovation in digital health and smartphone applications for mental health: transparency and trust. JAMA Psychiatry. 2017 May 1;74(5):437–8. doi: 10.1001/jamapsychiatry.2017.0262. [DOI] [PubMed] [Google Scholar]
- 176.Wynn SD, Sherrod RA. Providing mental health care to veterans in rural areas: using telehealth in mobile clinics. J Psychosoc Nurs Ment Health Serv. 2012 Jun;50(6):22–8. doi: 10.3928/02793695-20120508-01. [DOI] [PubMed] [Google Scholar]
- 177.Tschirch P, Walker G, Calvacca LT. Nursing in tele-mental health. J Psychosoc Nurs Ment Health Serv. 2006 May;44(5):20–7. doi: 10.3928/02793695-20060501-05. [DOI] [PubMed] [Google Scholar]
- 178.Sukmawati I, Ardi Z, Ifdil I, Zikra Z. Development and validation of acceptability of mental-health mobile app survey (AMMS) for android-based online counseling service assessment. J Phys: Conf Ser. 2019 Dec 16;1339:012124. doi: 10.1088/1742-6596/1339/1/012124. [DOI] [Google Scholar]
- 179.Ardi Z, Sukmawati I, Ifdil I, Afdal A, Rangka IB, Suranata K. Exploring the acceptability of internet-based mental health mobile app services using network psychometrics analysis. J Phys: Conf Ser. 2018 Dec 7;1114:012106. doi: 10.1088/1742-6596/1114/1/012106. [DOI] [Google Scholar]
- 180.Tielman ML, Neerincx MA, Pagliari C, Rizzo A, Brinkman W. Considering patient safety in autonomous e-mental health systems - detecting risk situations and referring patients back to human care. BMC Med Inform Decis Mak. 2019 Mar 18;19(1):47. doi: 10.1186/s12911-019-0796-x. https://bmcmedinformdecismak.biomedcentral.com/articles/10.1186/s12911-019-0796-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Pelletier J, Rowe M, François N, Bordeleau J, Lupien S. No personalization without participation: on the active contribution of psychiatric patients to the development of a mobile application for mental health. BMC Med Inform Decis Mak. 2013 Jul 27;13:78. doi: 10.1186/1472-6947-13-78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Williams A, Fossey E, Farhall J, Foley F, Thomas N. Going online together: the potential for mental health workers to integrate recovery oriented e-mental health resources into their practice. Psychiatry. 2018;81(2):116–29. doi: 10.1080/00332747.2018.1492852. [DOI] [PubMed] [Google Scholar]
- 183.Morganstein J. Mobile applications for mental health providers. Psychiatry. 2016;79(4):358–63. doi: 10.1080/00332747.2016.1237753. [DOI] [PubMed] [Google Scholar]
- 184.Rooksby J, Morrison A, Murray-Rust D. Student Perspectives on Digital Phenotyping: The Acceptability of Using Smartphone Data to Assess Mental Health. Proceedings of the 2019 CHI Conference on Human Factors in Computing Systems; CHI'19; May 4-19, 2019; Glasgow, Scotland, UK. 2019. [DOI] [Google Scholar]
- 185.Sakata J, Zhang M, Pu S, Xing J, Versha K. Beam: a Mobile Application to Improve Happiness and Mental Health. CHI '14 Extended Abstracts on Human Factors in Computing Systems; CHI EA'14; April 26-May 1, 2014; Toronto, Canada. 2014. [DOI] [Google Scholar]
- 186.Adewuya AO, Momodu O, Olibamoyo O, Adegbaju A, Adesoji O, Adegbokun A. The effectiveness and acceptability of mobile telephone adherence support for management of depression in the mental health in primary care (MeHPriC) project, Lagos, Nigeria: a pilot cluster randomised controlled trial. J Affect Disord. 2019 Jun 15;253:118–25. doi: 10.1016/j.jad.2019.04.025. [DOI] [PubMed] [Google Scholar]
- 187.Bakker D, Rickard N. Engagement in mobile phone app for self-monitoring of emotional wellbeing predicts changes in mental health: MoodPrism. J Affect Disord. 2018 Feb;227:432–42. doi: 10.1016/j.jad.2017.11.016. [DOI] [PubMed] [Google Scholar]
- 188.Seko Y, Kidd S, Wiljer D, McKenzie K. Youth mental health interventions via mobile phones: a scoping review. Cyberpsychol Behav Soc Netw. 2014 Sep;17(9):591–602. doi: 10.1089/cyber.2014.0078. [DOI] [PubMed] [Google Scholar]
- 189.Casey LM, Joy A, Clough BA. The impact of information on attitudes toward e-mental health services. Cyberpsychol Behav Soc Netw. 2013 Aug;16(8):593–8. doi: 10.1089/cyber.2012.0515. [DOI] [PubMed] [Google Scholar]
- 190.Hendrikoff L, Kambeitz-Ilankovic L, Pryss R, Senner F, Falkai P, Pogarell O, Hasan A, Peters H. Prospective acceptance of distinct mobile mental health features in psychiatric patients and mental health professionals. J Psychiatr Res. 2019 Feb;109:126–32. doi: 10.1016/j.jpsychires.2018.11.025. [DOI] [PubMed] [Google Scholar]
- 191.Wang K, Varma DS, Prosperi M. A systematic review of the effectiveness of mobile apps for monitoring and management of mental health symptoms or disorders. J Psychiatr Res. 2018 Dec;107:73–8. doi: 10.1016/j.jpsychires.2018.10.006. [DOI] [PubMed] [Google Scholar]
- 192.Schellong J, Lorenz P, Weidner K. Proposing a standardized, step-by-step model for creating post-traumatic stress disorder (PTSD) related mobile mental health apps in a framework based on technical and medical norms. Eur J Psychotraumatol. 2019;10(1):1611090. doi: 10.1080/20008198.2019.1611090. http://europepmc.org/abstract/MED/31143412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Olff M. Mobile mental health: a challenging research agenda. Eur J Psychotraumatol. 2015;6:27882. doi: 10.3402/ejpt.v6.27882. http://europepmc.org/abstract/MED/25994025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Teles A, Rodrigues I, Viana D, Silva F, Coutinho L, Endler M, Rabêlo R. Mobile Mental Health: A Review of Applications for Depression Assistance. 32nd International Symposium on Computer-Based Medical Systems; CBMS'19; June 5-7, 2019; Cordoba, Spain. 2019. [DOI] [Google Scholar]
- 195.Teles AS, Silva F, Rocha A, Lopes J, O'Sullivan D, Van DV, Endler M. Towards Situation-Aware Mobile Applications in Mental Health. 29th International Symposium on Computer-Based Medical Systems; CBMS'16; June 20-24, 2016; Dublin, Ireland. 2016. [DOI] [Google Scholar]
- 196.Gindidis S, Stewart S, Roodenburg J. A systematic scoping review of adolescent mental health treatment using mobile apps. Adv Mental Health. 2019;17(2):161–77. doi: 10.1080/18387357.2018.1523680. [DOI] [Google Scholar]
- 197.Dragovic M, Davison S, Morgan VA, Chiu VW, Richards N, Vatskalis T, Atkinson A, Waters F. ‘Validated, easy to use and free’: top three requests for mobile device applications (‘apps’) from mental health consumers and clinicians. Adv Mental Health. 2018 Dec 11;:1–9. doi: 10.1080/18387357.2018.1557014. [DOI] [Google Scholar]
- 198.Apolinário-Hagen J. The Digitization of Healthcare. London, UK: Palgrave Macmillan; 2017. Current perspectives on e-mental-health self-help treatments: Exploring the 'black box' Of public views, perceptions, and attitudes toward the digitalization of mental health care; pp. 205–23. [Google Scholar]
- 199.Eftychiou L, El Morr C. The Digitization of Healthcare. London, UK: Palgrave Macmillan; 2017. Mobile mental health virtual communities: challenges and opportunities; pp. 257–75. [Google Scholar]
- 200.Bakker D, Rickard N. Engagement with a cognitive behavioural therapy mobile phone app predicts changes in mental health and wellbeing: MoodMission. Aust Psychol. 2019 Mar 13;54(4):245–60. doi: 10.1111/ap.12383. [DOI] [Google Scholar]
- 201.Dingwall KM, Puszka S, Sweet M, Nagel T. 'Like drawing into sand': acceptability, feasibility, and appropriateness of a new e-mental health resource for service providers working with aboriginal and Torres Strait Islander people. Aus Psychol. 2015 Jan 12;50(1):60–9. doi: 10.1111/ap.12100. [DOI] [Google Scholar]
- 202.Cormode G, Krishnamurthy B. Key Differences Between Web 1.0 and Web 2.0. First Monday. 2008. [2020-08-19]. https://firstmonday.org/ojs/index.php/fm/article/view/2125.
- 203.O'Reilly T. Web 2.0: Compact Definition? Radar – O'Reilly. 2005. [2020-04-30]. http://radar.oreilly.com/2005/10/web-20-compact-definition.html.
- 204.Murugesan S. Understanding Web 2.0. IEEE Computer Society. 2007. [2020-08-19]. https://www.computer.org/csdl/magazine/it/2007/04/f4034/13rRUyYSWoO.
- 205.Number of Internet Users Worldwide From 2005 to 2019. Statista. 2020. https://www.statista.com/statistics/273018/number-of-internet-users-worldwide/
- 206.Number of Smartphones Sold to End Users Worldwide From 2007 to 2020. Statista. 2020. https://www.statista.com/statistics/263437/global-smartphone-sales-to-end-users-since-2007/
- 207.Share of Households That Use Desktop or Portable Computers to Access the Internet in Germany From 2003 to 2014. Statista. 2014. [2020-04-30]. https://www.statista.com/statistics/379251/internet-usage-via-desktop-or-mobile-computer-germany/
- 208.Share of Households That Use Desktop or Portable Computers to Access the Internet in Portugal From 2003 to 2014. Statista. 2014. [2020-04-30]. https://www.statista.com/statistics/380431/internet-usage-via-desktop-or-mobile-computer-portugal/
- 209.Share of Households That Use Desktop or Portable Computers to Access the Internet in Lithuania From 2003 to 2014. Statista. 2014. [2020-04-30]. https://www.statista.com/statistics/379295/internet-usage-via-desktop-or-mobile-computer-lithuania/
- 210.Giannopoulos G. The application of information and communication technologies in transport. Eur J Oper Res. 2004 Jan;152(2):302–20. doi: 10.1016/s0377-2217(03)00026-2. [DOI] [Google Scholar]
- 211.Buhalis D, O'Connor P. Information communication technology revolutionizing tourism. Tour Recreat Res. 2015 Jan 12;30(3):7–16. doi: 10.1080/02508281.2005.11081482. [DOI] [Google Scholar]
- 212.Yusuf MO. Information and communication technology and education: analysing the Nigerian national policy for information technology. Int Educ J. 2005;6(3):316–321. https://files.eric.ed.gov/fulltext/EJ854985.pdf. [Google Scholar]
- 213.Shachaf P. Cultural diversity and information and communication technology impacts on global virtual teams: An exploratory study. Information & Management. 2008 Mar;45(2):131–142. doi: 10.1016/j.im.2007.12.003. [DOI] [Google Scholar]
- 214.Shiferaw F, Zolfo M. The role of information communication technology (ICT) towards universal health coverage: the first steps of a telemedicine project in Ethiopia. Glob Health Action. 2012;5:1–8. doi: 10.3402/gha.v5i0.15638. http://europepmc.org/abstract/MED/22479235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215.Kurtz MJ, Bollen J. Usage bibliometrics. Ann Rev Info Sci Tech. 2012 Jan 18;44(1):1–64. doi: 10.1002/aris.2010.1440440108. [DOI] [Google Scholar]
- 216.Hicks D, Wouters P, Waltman L, de Rijcke S, Rafols I. Bibliometrics: the Leiden Manifesto for research metrics. Nature. 2015 Apr 23;520(7548):429–31. doi: 10.1038/520429a. [DOI] [PubMed] [Google Scholar]
- 217.Stephan P, Veugelers R, Wang J. Reviewers are blinkered by bibliometrics. Nature. 2017 Apr 26;544(7651):411–2. doi: 10.1038/544411a. [DOI] [PubMed] [Google Scholar]
- 218.Haustein S, Larivière V. Incentives and Performance. Cham, UK: Springer; 2015. The use of bibliometrics for assessing research: possibilities, limitations and adverse effects; pp. 121–39. [Google Scholar]
- 219.Agarwal A, Durairajanayagam D, Tatagari S, Esteves S, Harlev A, Henkel R, Roychoudhury S, Homa S, Puchalt N, Ramasamy R, Majzoub A, Ly K, Tvrda E, Assidi M, Kesari K, Sharma R, Banihani S, Ko E, Abu-Elmagd M, Gosalvez J, Bashiri A. Bibliometrics: tracking research impact by selecting the appropriate metrics. Asian J Androl. 2016;18(2):296–309. doi: 10.4103/1008-682X.171582. http://www.ajandrology.com/article.asp?issn=1008-682X;year=2016;volume=18;issue=2;spage=296;epage=309;aulast=Agarwal. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220.Werner R. The focus on bibliometrics makes papers less useful. Nature. 2015 Jan 15;517(7534):245. doi: 10.1038/517245a. [DOI] [PubMed] [Google Scholar]
- 221.Nickelson DW. Telehealth and the evolving health care system: strategic opportunities for professional psychology. Prof Psychol Res Pr. 1998;29(6):527–35. doi: 10.1037/0735-7028.29.6.527. [DOI] [Google Scholar]
- 222.Alberta Heritage Foundation for Medical Research. Simpson J. An Assessment of Routine Telepsychiatry Services. Ponoka, Alberta: Alberta Heritage Foundation for Medical Research; 1999. [Google Scholar]
- 223.Della Mea V. What is e-health (2): the death of telemedicine? J Med Internet Res. 2001;3(2):E22. doi: 10.2196/jmir.3.2.e22. https://www.jmir.org/2001/2/e22/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 224.Allen A. Morphing telemedicine-telecare-telehealth-ehealth. Telemed Today. 2000;1(43):-. [Google Scholar]
- 225.Number of Smartphone Users Worldwide From 2016 to 2021. Statista. 2020. [2020-04-30]. https://www.statista.com/statistics/330695/number-of-smartphone-users-worldwide/
- 226.Emerging mHealth: Paths for Growth. PWC. 2014. [2020-04-30]. https://www.pwc.com/gx/en/healthcare/mhealth/assets/pwc-emerging-mhealth-full.pdf.
- 227.Proudfoot J, Parker G, Hadzi Pavlovic D, Manicavasagar V, Adler E, Whitton A. Community attitudes to the appropriation of mobile phones for monitoring and managing depression, anxiety, and stress. J Med Internet Res. 2010 Dec 19;12(5):e64. doi: 10.2196/jmir.1475. https://www.jmir.org/2010/5/e64/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 228.Drissi N, Ouhbi S, García-Berná J, Janati Idrissi MA, Ghogho M. Sensor-based Solutions for Mental Healthcare: A Systematic Literature Review. 13th International Conference on Health Informatics; HEALTHINF'20; February 24-26, 2020; Valletta, Malta. 2020. pp. 593–600. [DOI] [Google Scholar]
- 229.Shewan LG, Coats AJ. Ethics in the authorship and publishing of scientific articles. Int J Cardiol. 2010 Sep;144(1):1–2. doi: 10.1016/j.ijcard.2010.07.030. [DOI] [Google Scholar]
- 230.Ammenwerth E, de Keizer N. A viewpoint on evidence-based health informatics, based on a pilot survey on evaluation studies in health care informatics. J Am Med Inform Assoc. 2007;14(3):368–71. doi: 10.1197/jamia.M2276. http://europepmc.org/abstract/MED/17329724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 231.Sunitha S, Gururaj G. Health behaviours & problems among young people in India: cause for concern & call for action. Indian J Med Res. 2014 Aug;140(2):185–208. http://www.ijmr.org.in/article.asp?issn=0971-5916;year=2014;volume=140;issue=2;spage=185;epage=208;aulast=Sunitha. [PMC free article] [PubMed] [Google Scholar]
- 232.Stang J, Story M. Guidelines for Adolescent Nutrition Services. University of Minnesota. 2008. https://books.google.ae/books/about/Guidelines_for_Adolescent_Nutrition_Serv.html?id=t-zJDAEACAAJ&redir_esc=y.
- 233.Garber J, Frankel SA, Herrington CG. Developmental demands of cognitive behavioral therapy for depression in children and adolescents: cognitive, social, and emotional processes. Annu Rev Clin Psychol. 2016;12:181–216. doi: 10.1146/annurev-clinpsy-032814-112836. http://europepmc.org/abstract/MED/27019397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 234.Nalwa K, Anand AP. Internet addiction in students: a cause of concern. Cyberpsychol Behav. 2003 Dec;6(6):653–6. doi: 10.1089/109493103322725441. [DOI] [PubMed] [Google Scholar]
- 235.Young K, Pistner M, O'Mara J, Buchanan J. Cyber disorders: the mental health concern for the new millennium. Cyberpsychol Behav. 1999;2(5):475–9. doi: 10.1089/cpb.1999.2.475. [DOI] [PubMed] [Google Scholar]
- 236.Depression and Other Common Mental Disorders: Global Health Estimates. World Health Organization. 2017. https://apps.who.int/iris/bitstream/handle/10665/254610/WHO-MSD-MER-2017.2-eng.pdf.
- 237.Fonseca A, Gorayeb R, Canavarro MC. Women's use of online resources and acceptance of e-mental health tools during the perinatal period. Int J Med Inform. 2016 Oct;94:228–36. doi: 10.1016/j.ijmedinf.2016.07.016. [DOI] [PubMed] [Google Scholar]
- 238.Kim J, Lim S, Lee B, Lee J. Detecting Depression of Cancer Patients with Daily Mental Health Logs from Mobile Applications. Association for Information Systems (AIS) eLibrary. 2015. [2020-08-19]. https://aisel.aisnet.org/cgi/viewcontent.cgi?article=1551&context=icis2015.
- 239.Drissi N, Ouhbi S, Janati Idrissi MA, Ghogho M. Mobile Apps for Post Traumatic Stress Disorder. Conf Proc IEEE Eng Med Biol Soc; EMBC'19; July 23-27, 2019; Berlin, Germany. 2019. Jul, pp. 4279–4282. https://ieeexplore.ieee.org/abstract/document/8857197. [DOI] [PubMed] [Google Scholar]
- 240.Excellence in Research for Australia. Australian Research Council. 2019. [2020-04-30]. https://www.arc.gov.au/excellence-research-australia.
- 241.Research Opportunities. Australian Government. 2020. https://www.studyinaustralia.gov.au/English/Australian-Education/Universities-Higher-Education/research-opportunities.
- 242.About the Australasian Institute of Digital Health. Australasian Institute of Digital Health. 2020. [2020-04-30]. https://digitalhealth.org.au/about/
- 243.Hather GJ, Haynes W, Higdon R, Kolker N, Stewart EA, Arzberger P, Chain P, Field D, Franza BR, Lin B, Meyer F, Ozdemir V, Smith CV, van Belle G, Wooley J, Kolker E. The United States of America and scientific research. PLoS One. 2010 Aug 16;5(8):e12203. doi: 10.1371/journal.pone.0012203. https://dx.plos.org/10.1371/journal.pone.0012203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 244.50 Leaders in Health IT. Becker's Hospital Review - Healthcare News. 2015. [2020-04-30]. https://www.beckershospitalreview.com/healthcare-information-technology/50-leaders-in-health-it.html.
- 245.Hashemi B, Ali S, Awaad R, Soudi L, Housel L, Sosebee SJ. Facilitating mental health screening of war-torn populations using mobile applications. Soc Psychiatry Psychiatr Epidemiol. 2017 Jan;52(1):27–33. doi: 10.1007/s00127-016-1303-7. [DOI] [PubMed] [Google Scholar]
- 246.Phillips EA, Gordeev VS, Schreyögg J. Effectiveness of occupational e-mental health interventions: a systematic review and meta-analysis of randomized controlled trials. Scand J Work Environ Health. 2019 Nov 1;45(6):560–76. doi: 10.5271/sjweh.3839. [DOI] [PubMed] [Google Scholar]
- 247.Richardson LK, Frueh BC, Grubaugh A, Egede L, Elhai J. Current directions in videoconferencing tele-mental health research. Clin Psychol (New York) 2009 Sep 1;16(3):323–38. doi: 10.1111/j.1468-2850.2009.01170.x. http://europepmc.org/abstract/MED/20161010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 248.249 AD, Sivertsen G. A criteria-based assessment of the coverage of Scopus and web of science. J Data Inf Sci. 2019;4(1):1–21. doi: 10.2478/jdis-2019-0001. [DOI] [Google Scholar]
- 249.Karampela M, Ouhbi S, Isomursu M. Personal health data: a systematic mapping study. Int J Med Inform. 2018 Oct;118:86–98. doi: 10.1016/j.ijmedinf.2018.08.006. [DOI] [PubMed] [Google Scholar]
- 250.Souza-Pereira L, Pombo N, Ouhbi S, Felizardo V, Garcia N. Clinical decision support systems for chronic diseases: a systematic literature review. Comput Methods Programs Biomed. 2020 May 23;195:105565. doi: 10.1016/j.cmpb.2020.105565. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Classification results.


