Abstract
Objectives
Using a gendered life course perspective, we examine whether the relationship between age of migration and mortality is moderated by gender among a cohort of older Mexican Americans.
Methods
Data from the Hispanic Established Populations for the Epidemiological Study of the Elderly and recently matched mortality data are used to estimate Cox proportional hazard models.
Results
Our findings indicate that the relationship between age of migration and mortality is moderated by gender, suggesting a more nuanced perspective of the immigrant mortality paradox. Among men, midlife migrants exhibit an 18% lower risk of mortality compared to their U.S.-born co-ethnics, possibly due to immigrant selectivity at the time of migration. Conversely, late-life migrant women exhibit a 17% lower risk of mortality relative to U.S.-born women, attributed in part to socio-cultural characteristics that influence lifestyle risk factors across the life course.
Discussion
Selection mechanisms and acculturation processes associated with the immigrant experience are contingent on both age and gender, suggesting the utility of an integrated life course approach to contextualize the mortality profiles of older immigrants. These findings demonstrate the heterogeneity among immigrants and highlight the need to understand gender differences in the migration process when assessing the immigrant mortality paradox.
Keywords: Gender, Migration, Mortality, Life course analysis
Life course theory suggests that early life experiences set individuals on specific trajectories over time with implications across multiple domains including health (Dannefer, 2003; Elder Jr, Johnson, & Crosnoe, 2003). Research linking early life experiences to late-life health and mortality are plentiful (Hayward & Gorman, 2004; Riosmena, Wong, & Palloni, 2013; Willson & Shuey, 2016). A pivotal life course transition for the foreign-born is migration to a new country (Treas & Gubernskaya, 2016). The migration process is both in itself a stressful event and shapes future opportunities available to immigrants which may produce a variety of health outcomes (Ferraro, Kemp, & Williams, 2017; Jasso, 2003; Treas & Mazumbdar, 2002).
Two important factors in the migration process that differentiate the immigrant experience in the United States are: age of migration and gender. Age of migration is an important factor to consider for understanding immigrant health trajectories across the life course, in part because age of migration shapes immigrants’ exposure to a new culture, health behaviors, and economic incorporation (Burr, Gerst, Kwan, & Mutchler, 2008; Jasso, 2003). For instance, opportunities to adapt and incorporate into U.S. mainstream institutions are greater for individuals migrating at younger ages than at older ages (Rumbaut, 2004). Increased duration in the United States among early-life migrants translates to more opportunities to accumulate wealth through educational and occupational incorporation, which may be protective of late life health (Angel, Buckley, & Sakamoto, 2001; Treas, 2015). Conversely, individuals who migrate in midlife and old age have less time to adapt to American culture and fewer opportunities to build wealth through labor market participation. These important age-graded distinctions in age of migration have led to a growing body of research on how immigrant health may vary by age of migration across the life course (Ferraro et al., 2017; Treas & Gubernskaya, 2016).
Similarly, mounting evidence suggests that the process of migration and its implications for health outcomes across the life course vary by gender (Garcia & Reyes, 2018; Monserud & Markides, 2018). For instance, research on migration from Mexico finds men and women migrate for different reasons and have unique migration experiences (Donato, 2010; Massey, Fischer, & Capoferro, 2006). Among migrants from Mexico to the United States during the 20th century, men were more likely to migrate for occupational opportunities, whereas women were more likely to migrate to follow their husbands or for family reunification at older ages (Carr & Tienda, 2013; Donato, 2010; Massey et al., 2006). In addition, recent findings show the association between age of migration and several health domains including morbidity, physical functioning, cognition, disability, and mental health among older Mexican Americans to vary by gender (Garcia & Reyes, 2018; Garcia, Valderrama-Hinds, et al., 2017; Hill, Angel, Balistreri, & Herrera, 2012; Monserud, 2019; Monserud & Markides, 2018).
Furthermore, previous research has found age of migration to be associated with the risk of mortality in samples of Hispanic immigrants that combine men and women. For example, Holmes and colleagues (2015) document a significant mortality advantage among a national sample of foreign-born Hispanics (inclusive of Mexican, Puerto Rican, Cuban, and “other” Hispanics) arriving at ages 25 and older compared to U.S.-born Hispanics (Holmes, Driscoll, & Heron, 2015). Conversely, regional studies specific to older Mexican Americans have documented a lower risk of all-cause mortality among late-life (age 50 and older) migrants relative to their U.S.-born co-ethnics in the Southwest United States (Angel, Angel, Díaz Venegas, & Bonazzo, 2010) and an increased risk of cardiovascular mortality among early-life migrants (under age 20) compared to Mexicans who migrate at older ages in the Sacramento Metropolitan Area (Colón-López, Haan, Aiello, & Ghosh, 2009). Overall, these findings suggest that the immigrant mortality advantage is stronger among adult migrants than those who migrate as children or during adolescence. Although these studies highlight heterogeneous mortality profiles among Hispanic immigrants, they do not explicitly test for gender differences, thus downplaying potential age of migration differences between men and women that may shape mortality outcomes among foreign-born Hispanics. Consequently, this study incorporates a gendered life course perspective to assess whether the association between mortality and age of migration varies by gender among a cohort of Mexican Americans age 65 and older. Given Hispanic women on average live longer than Hispanic men (Arias, Heron, & Xu, 2017) and differential motivations for migration (Donato, 2010; Massey et al., 2006), we expect gender to be an important factor moderating the relationship between age of migration and the risk of mortality among older foreign-born Mexican Americans.
Background
Mortality Paradox
Research shows that Hispanics (particularly immigrants) residing in the United States have comparable or longer life expectancies at birth and age 65 than non-Hispanic whites, despite lower socioeconomic status (SES; Garcia, Garcia, Chiu, Raji, & Markides, 2018; Lariscy, Hummer, & Hayward, 2015; Markides & Rote, 2015). In 2014, life expectancy at age 65 was 19.7 years for Hispanic men and 22.8 years for Hispanic women compared to 18.0 years for non-Hispanic white men and 20.6 years for non-Hispanic white women (Arias et al., 2017). This Hispanic mortality advantage vis-à-vis non-Hispanics whites is strongest at older ages and among the foreign-born (Fenelon, Chinn, & Anderson, 2017).
Three explanations have been posited for the immigrant mortality advantage: (a) immigrants are more robust than individuals who do not migrate from their country of origin and individuals in the receiving country, resulting in positive health selection that leads to a mortality advantage (Bostean, 2013; Riosmena et al., 2013); (b) strong social ties and positive health behaviors (i.e., lower levels of smoking/drinking and healthier diet) related to societal norms in their country of origin compared to societal norms in the United States may “buffer” against the deleterious effects of socioeconomic disadvantage and contribute to lower mortality among immigrants (Antecol & Bedard, 2006; Markides & Eschbach, 2005); and (c) lastly data quality issues may contribute to an immigrant mortality advantage when immigrants are misclassified or unmatched on death records and when return migration (i.e., the salmon-bias effect) is not captured in vital records (Palloni & Arias, 2004).
Heterogeneity in the Immigrant Health Paradox
A preponderance of evidence suggests that heterogeneity in health and mortality outcomes among immigrants are related to complex migratory and acculturative processes. However, longevity advantages from health selection and disadvantages through negative acculturation (the adoption of poor diets and health habits with increased duration) may not apply uniformly to all immigrants, as these are individual-level processes that likely vary by gender. Indeed, life course theory suggests that the timing of events in biological time may set individuals on different paths (Elder Jr et al., 2003; Treas & Gubernskaya, 2016). Thus, differential migratory experiences by biological age and gender may contribute to complex gendered patterns in mortality outcomes as variation in socioeconomic incorporation, and amount of acculturation (positive or negative) between immigrant men and women may reflect individual characteristics of health selection and socio-cultural retention (Angel et al., 2010; Fenelon et al., 2017).
For example, immigrants who arrive in adolescence or as children are able to adapt more easily into the host society and may have similar health and mortality experiences as their U.S.-born co-ethnics (Angel et al., 2010; Garcia & Reyes, 2018; Holmes et al., 2015). Although this can provide economic advantages, which may be protective of health in later life (Angel et al., 2001; Gubernskaya, Bean, & Van Hook, 2013), it may also imply the adoption of worse health behaviors including poorer diet, sedentary lifestyle, and increased smoking/drinking (Antecol & Bedard, 2006; Riosmena et al., 2013). In addition, children have little autonomy regarding the migration process; thus, gender is unlikely to be a determinant of health selection among early life migrants.
Conversely, men who migrate in midlife are often the active decision makers in the migration process and migrate for occupational and economic opportunities rather than family reunification purposes (Gubernskaya et al., 2013). Given these motives, midlife immigrants are more likely to be positively selected on individual health characteristics that are protective of mortality than youth who migrate with parents or older adults who migrate to join families (Carr & Tienda, 2013; Gubernskaya, 2015). In general, both midlife migrant men and women exhibit healthier outcomes at younger ages than U.S.-born men and women (respectively), though this advantage is larger among men (Garcia & Reyes, 2018; Hill et al., 2012). However, the ability of midlife migrant men and women to retain these health advantages varies across health outcomes. Midlife male migrants from Mexico have slower cognitive decline, yet exhibit a faster decline in self-rated health, chronic conditions, and physical functioning compared to their U.S.-born co-ethnics, whereas midlife female migrants exhibit no advantages in their health trajectories in late life (Garcia & Reyes, 2018; Gubernskaya, 2015; Hill et al., 2012).
Late-life migrants from Mexico are more dependent on their family than individuals who migrated at earlier ages and have limited healthcare resources, which may lead to negative health outcomes due to late detection, and poor treatment of diseases in old age (Burr et al., 2008; Treas & Mazumbdar, 2002). Although individual characteristics among older immigrants may play less of a selective role in the migration process, these migrants are more likely to retain (gendered) social and cultural characteristics that influence positive health behaviors longer than immigrants who migrate early in the life course as they experience less exposure to U.S. society (Kimbro, 2009). More favorable health behaviors combined with stronger family ties among late-life migrants may lead to a “cultural buffering” that is protective of mortality.
In sum, previous research has found that midlife migrants tend to have better health outcomes than individuals born in the United States as well as those arriving in early- or late-life (Garcia & Reyes, 2018; Gubernskaya, 2015). Furthermore, immigrant men from Mexico retain a health advantage longer than immigrant women across several health domains including self-rated health (Gubernskaya, 2015; Read & Reynolds, 2012), disability (Garcia & Reyes, 2018; Monserud, 2019), obesity (Antecol & Bedard, 2006), and cognition (Hill et al., 2012). Two explanations are posited for the observed gender differences: First, women are less autonomous in the migration process (Carr & Tienda, 2013; Treas, 2015), and thus may be less select on individual health characteristics than men upon initial migration and may also experience faster declines in health since arrival (Eschbach, Al-Snih, Markides, & Goodwin, 2007; Markides & Rote, 2015). Second, women are more likely to view processes related to migration and acculturation as stressful (Donato, 2010), which may negatively affect health and well-being across the life course. Building on prior research, we examine the relationship between age of migration and mortality to test whether this association varies by gender.
Hypotheses
Age of migration can be useful for understanding mortality in old age by approximating individual-level characteristics related to motivations for migration and lifetime exposure to social and cultural environments in both sending and receiving countries. Recent research in life course theory and immigrant health leads us to develop the following hypotheses based on age of migration, gender, and mortality.
H1: We hypothesize that age of migration is significantly associated with mortality due to positive health selection among midlife migrants and lower acculturation among late-life migrants. Specifically, we posit that individual characteristics related to health selectivity will be stronger for midlife migrants from Mexico and reflected in lower levels of mortality compared to U.S.-born Mexican Americans. We also predict that late-life migrants will have a lower risk for mortality than their U.S.-born co-ethnics as they are more likely to retain social and cultural characteristics associated with positive health behaviors due to less exposure to negative health behaviors associated with U.S. culture.
H2: Given the migration process varies by gender, we expect health selection and cultural buffering to operate differently for men and women. Thus, we hypothesize that the association between age of migration and mortality will be moderated by gender. Specifically, we posit that the observed health selection among midlife migrants will be more pronounced among men given they are more likely to migrate for occupational and economic opportunities. In addition, we hypothesize that late-life migrant women will have a lower risk for mortality compared to U.S.-born women as research suggests that older foreign-born women are more likely than men to retain protective health behaviors due to socio-cultural norms from their country of origin.
Data and Methods
Data
This study analyzes data from the Hispanic Established Populations for the Epidemiological Study of the Elderly (H-EPESE). The H-EPESE is a longitudinal panel of older Mexican Americans who reside in five Southwestern states: Arizona, California, Colorado, New Mexico, and Texas (Markides, Rudkin, Angel, & Espino, 1997). The survey utilized a multistage area probability sampling design that ensured a sample generalizable to approximately 500,000 Mexican Americans aged 65 and older living in the Southwest. Details on sampling procedures have been described in detail elsewhere (Eschbach, Ostir, Patel, Markides, & Goodwin, 2004). Eligible respondents were identified based on self-identification as Mexican, Mexican American, Chicano, or Hispano, reported birthplace (Mexico or the United States), and a review of ethnic background of a respondent’s parents and grandparents. Respondents were interviewed up to 8 times between 1993 and 2013. The first wave was collected in 1993–1994, with seven subsequent waves of data collected in 1995–1996, 1998–1999, 2000–2001, 2004–2005, 2006–2007, 2010–2011, and 2012–2013. In 2004–2005 a supplemental cohort was added to increase sample size. Retention through wave 8 was 88%. Retention is inclusive of active interviews, known deceased, and refusals. The remaining participants are passively followed-up for mortality through vital statistics.
Item nonresponse reduced the sample by approximately 15%, with missing data on obesity (n = 307) and age of migration (n = 91) accounting for the largest share. To address missing data, we employ multiple imputation by chained equations using Stata’s mi commands (Royston, 2005). To utilize auxiliary variables from across the length of the survey and reduce bias in our imputation estimates, we imputed the data in person-record format and include the Nelson–Aalen estimate of the cumulative hazard to survival time (White & Royston, 2009; Young & Johnson, 2015). Findings are based on combined results from 20 imputed data sets. Key findings were similar using imputed and unimputed data.
Variables
Data on date of death are collected during the survey from proxy respondents who are generally surviving family and from administrative matching using the National Death Index (NDI). Respondents are matched to NDI records using social security numbers and other identifying information. As of December 31, 2016, 3,198 deaths had been identified, comprising approximately 76% of the sample. Since most of the sample has died by the latest match, this makes hazard models of mortality well suited. The 754 respondents who were not matched to the NDI records are presumed to still be alive.
Our main covariate of interest is age of migration to the United States. We combine age of migration with nativity, using U.S.-born respondents as the reference category. Following previous research conducted with the H-EPESE, we categorize the foreign-born by life course stage at migration with respondents who migrated between ages 0 and 19 as early-life migrants, ages 20 and 49 as midlife migrants, and age 50 and older as late-life migrants (Angel et al., 2010; Hill et al., 2012).
We also include a set of sociodemographic, behavior risk factors, and chronic health conditions as controls to account for potential confounding mechanisms which may be associated with our two variables of interest: age of migration and mortality. Given the robust relationship between SES and mortality, we include two controls for SES: education and financial strain. Years of education is a continuous measure of formal schooling which serves as a proxy for lifelong SES. Financial strain controls for current financial problems either in meeting monthly bills or not having enough money at the end of the month. Following previous research, we include marital status and living arrangements to control for demographic and social factors found to be associated with Hispanic mortality (Angel et al., 2010; Colón-López et al., 2009; Fenelon et al., 2017). Marital status indicates if respondents were married at first observation. Living arrangements is coded to indicate those who live alone at first observation.
Previous research has found gender differences in the level of acculturation and adoption of negative health behaviors among immigrants (Antecol & Bedard, 2006; Fenelon, 2013). To determine whether gender and mortality were independent of these factors, we include controls for interview language and health behaviors as proxy measures for level of acculturation among the foreign-born. Linguistic acculturation is coded 1 for those who take the survey in English. Acculturation and the adoption of negative health behaviors controls are: obesity, smoking, and drinking. Obesity is measured using self-reported body weight and height to calculate body mass index (BMI). Those with a BMI greater than 30 are considered obese. Ever smoke, is coded as 1 if respondent ever reports having smoked. Ever drink, is coded as 1 if respondent reports ever having been an alcohol drinker. Finally, we include a baseline measure of morbidity by controlling for a number of chronic conditions known to be associated with mortality to account for any potential confounding between age of migration and mortality (Angel et al., 2010; Holmes et al., 2015). The six self-reported chronic conditions are: heart disease, stroke, cancer, high blood pressure, arthritis, and diabetes. For each condition, those reporting yes or suspect/possible diagnosis by a medical professional are coded as having that condition. We also include two additional controls in all models: 10-year birth cohort and proxy respondent.
Analysis
We estimate Cox proportional hazards models to assess age-specific mortality differences by age of migration (Cox, 1972). The time variable used in the model is age, an adjustment for age at first interview is included to control for age at entry into the risk set. Individuals alive on December 31, 2016 are censored and presumed to be alive. We use Wald tests to assess the significance of covariates. Given the precision of mortality data, very few ties are observed. To deal with tied event times, we use the Efron method of handling ties.
We begin with a set of stepwise models estimated on the full sample to test our first hypothesis that age of migration is associated with mortality among older Mexican Americans. To test our second hypothesis that gender moderates the relationship between age of migration and mortality among older Mexican Americans, we include an interaction between age of migration and gender (Model 2). Next, we stratify our models by gender to simplify model interpretation given previously noted differences in the risk of mortality among older Mexican Americans (Fenelon et al., 2017; Lariscy et al., 2015) and gendered differences in the migration process among Mexican migrants (Donato, 2010; Massey et al., 2006). This model assumes that hazard rates are proportional by age. Supplemental analyses (available upon request) indicate that in our final stratified models all covariates meet proportionality assumption. Supplemental analyses tested the addition of controls for social support and health characteristics; however, the inclusion of these controls did not change our main results (available upon request).
Results
Table 1 reports the mean or proportion for covariates stratified by age of migration and gender. U.S.-born men and women are the most educated in the sample, whereas individuals who migrated at older ages are the least educated. Financial strain was higher among late-life migrants compared to U.S.-born Mexican Americans, regardless of gender. Men in the sample are more likely to be married and not live alone compared to women. Women were more likely to be obese, but less likely to report drinking and smoking than men. Smoking rates are similar by age of migration for men and women. Among women, midlife and late-life migrants have the largest proportion of respondents alive in 2016. Conversely, midlife migrant men have the largest share still living as of 2016.
Table 1.
Descriptive Statistics Stratified by Gender and Age of Migration
| Females (N = 2,290) | Males (N = 1,662) | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| U.S.-Born | Early-life | Midlife | Late-life | U.S.-born | Early-life | Midlife | Late-life | |||||||||
| Mean (sd) or % | ||||||||||||||||
| Sociodemographic | ||||||||||||||||
| Years of education | 5.51 | (4.07) | 4.26* | (3.58) | 4.06* | (3.48) | 2.95* | (3.20) | 6.01 | (4.36) | 3.92* | (3.49) | 3.81* | (3.35) | 2.62* | (2.68) |
| Financial strain | 0.28 | 0.32 | 0.31 | 0.37* | 0.25 | 0.28 | 0.31* | 0.35* | ||||||||
| Married | 0.41 | 0.27* | 0.41 | 0.28* | 0.72 | 0.70 | 0.77 | 0.73 | ||||||||
| Live alone | 0.29 | 0.32 | 0.30 | 0.24 | 0.17 | 0.13 | 0.12* | 0.09* | ||||||||
| Acculturation | ||||||||||||||||
| Interview in English | 0.17 | 0.06* | 0.01* | 0.01* | 0.22 | 0.07* | 0.02* | 0.01* | ||||||||
| Obese | 0.44 | 0.36* | 0.46 | 0.39 | 0.32 | 0.31 | 0.33 | 0.33 | ||||||||
| Drinker | 0.29 | 0.23* | 0.26 | 0.22* | 0.77 | 0.75 | 0.79 | 0.78 | ||||||||
| Smoker | 0.28 | 0.29 | 0.28 | 0.23 | 0.65 | 0.62 | 0.65 | 0.62 | ||||||||
| No. of chronic conditions | 1.59 | (1.21) | 1.56 | (1.17) | 1.63 | (1.1) | 1.41 | (1.07) | 1.33 | (1.19) | 1.21 | (1.14) | 1.27 | (1.1) | 1.2 | (1.08) |
| Mortality info | ||||||||||||||||
| Dead 2015 | 0.77 | 0.82 | 0.72* | 0.69* | 0.85 | 0.88 | 0.72* | 0.82 | ||||||||
| N | 1,306 | 235 | 504 | 245 | 944 | 191 | 380 | 147 | ||||||||
Note: Statistically significant differences (p < .05) for male and female migrants compared to U.S.-born denoted with *.
Mortality
We begin by estimating mortality hazards for the full sample to examine the association between age of migration and mortality (Table 2). Migrating in midlife and late-life is associated with a significantly lower risk (17% and 14%, respectively) of mortality among the foreign-born relative to their U.S.-born counterparts (Model 1). In addition, men have a 27% higher risk of mortality than women. In the next model, we include a set of interaction terms to test our second hypothesis that gender moderates the association between age of migration and mortality (Model 2). Our results indicate that the association between age of migration and mortality varies for immigrant men and women. Among men, migrating in midlife is associated with lower mortality relative to U.S.-born men. In contrast, midlife migrant women do not significantly differ in mortality profiles from U.S.-born women.
Table 2.
Cox Proportional Hazards of Mortality Among Older Mexicans by Age of Migration
| Model 1 | Model 2 | Model 3 | Model 4 | Model 5 | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| HR | CI | HR | CI | HR | CI | HR | CI | HR | CI | |
| Age of Migration (Ref = U.S. Born) | ||||||||||
| Early-life (0–19) | 0.92 | [0.82 1.04] |
0.93 | [0.79 1.09] |
0.91 | [0.78 1.07] |
0.93 | [0.79 1.10] |
0.92 | [0.78 1.09] |
| Midlife (20–49) | 0.83*** | [0.76 0.91] |
0.92 | [0.81 1.04] |
0.93 | [0.82 1.05] |
0.96 | [0.85 1.09] |
0.94 | [0.83 1.07] |
| Late-life (50+) | 0.86* | [0.76 0.98] |
0.84* | [0.71 0.99] |
0.82* | [0.69 0.98] |
0.84 | [0.71 1.00] |
0.85 | [0.72 1.02] |
| Males | 1.27*** | [1.18 1.36] |
1.32*** | [1.20 1.45] |
1.38*** | [1.25 1.52] |
1.35*** | [1.21 1.50] |
1.42*** | [1.28 1.58] |
| Age of Migration*Gender | ||||||||||
| Early-life*Male | 0.98 | [0.78 1.25] |
1.00 | [0.79 1.27] |
1.04 | [0.82 1.32] |
1.05 | [0.83 1.33] |
||
| Midlife*Male | 0.80* | [0.66 0.96] |
0.80* | [0.66 0.96] |
0.81* | [0.67 0.97] |
0.83* | [0.69 1.00] |
||
| Late-life*Male | 1.08 | [0.83 1.40] |
1.10 | [0.85 1.43] |
1.11 | [0.85 1.44] |
1.13 | [0.87 1.46] |
||
| Education | 1.00 | [0.99 1.01] |
1.00 | [0.99 1.01] |
1.00 | [0.99 1.01] |
||||
| Financial strain | 1.14** | [1.05 1.24] |
1.15*** | [1.06 1.25] |
1.14** | [1.05 1.24] |
||||
| Married | 0.88** | [0.80 0.96] |
0.90* | [0.82 0.99] |
0.91* | [0.83 1.00] |
||||
| Live alone | 0.97 | [0.87 1.08] |
0.97 | [0.88 1.08] |
0.98 | [0.89 1.09] |
||||
| Ever obese | 0.80*** | [0.74 0.87] |
0.79*** | [0.73 0.85] |
||||||
| Ever drink | 0.88** | [0.80 0.96] |
0.86*** | [0.78 0.94] |
||||||
| Ever smoke | 1.16*** | [1.07 1.26] |
1.13** | [1.04 1.23] |
||||||
| Interview in English | 1.47*** | [1.30 1.65] |
1.40*** | [1.24 1.58] |
||||||
| Number of chronic conditions | 1.16*** | [1.13 1.20] |
||||||||
| N | 3,952 | |||||||||
Notes: All models control for proxy response and birth cohort. HR = Hazard ratios; CI = 95% Confidence intervals. *p < .05; **p < .01; ***p < .001.
Controlling for socioeconomic and demographic characteristics does not change the association between age of migration and mortality (Model 3). Controlling for health behaviors and interview language related to acculturation, midlife migrants continue to exhibit a lower mortality than their U.S.-born counterparts, whereas late-life migrants no longer exhibit a mortality advantage (Model 4). Controlling for number of chronic conditions does not change the association between age of migration and mortality (Model 5). Taken together, our results suggest complex patterns in the hazard of mortality by age of migration and gender. Therefore, we estimate models separately by gender for ease of interpretation and to better contextualize the mortality experiences of immigrant men and women.
Table 3 presents mortality hazard ratios from models stratified by gender. We start by estimating the association between age of migration and mortality among women (Panel A). Late-life migration among women is associated with a 17% decrease in the risk of mortality relative to U.S.-born women (Model 1). Net of controls for social and demographic factors, late-life migrant women continue to exhibit a mortality advantage over their U.S.-born co-ethnics (Models 2 and 3). In Model 4, we include a control for baseline health. Although late-life migrant women continue to exhibit significantly lower mortality than U.S.-born women, their mortality does not significantly differ from early-life or midlife migrant women.
Table 3.
Stratified Cox Models of Mortality by Age of Migration for Men and Women
| Model 1 | Model 2 | Model 3 | Model 4 | |||||
|---|---|---|---|---|---|---|---|---|
| HR | CI | HR | CI | HR | CI | HR | CI | |
| Panel A: Females | ||||||||
| Age of Migration (Ref = U.S. Born) | ||||||||
| Early-life (0–19) | 0.90 | [0.77 1.07] |
0.89 | [0.75 1.05] |
0.89 | [0.76 1.05] |
0.89 | [0.75 1.05] |
| Midlife (20–49) | 0.92 | [0.81 1.04] |
0.92 | [0.81 1.05] |
0.94 | [0.83 1.07] |
0.92 | [0.81 1.04] |
| Late-life (50+) | 0.83* | [0.70 0.98] |
0.81* | [0.68 0.96] |
0.81* | [0.68 0.97] |
0.83* | [0.70 0.99] |
| Education | 1.00 | [0.99 1.02] |
1.00 | [0.99 1.01] |
1.00 | [0.99 1.01] |
||
| Financial strain | 1.15** | [1.04 1.29] |
1.16** | [1.04 1.29] |
1.13* | [1.02 1.27] |
||
| Married | 0.89 | [0.79 1.00] |
0.90 | [0.80 1.01] |
0.92 | [0.82 1.04] |
||
| Live alone | 0.93 | [0.82 1.04] |
0.93 | [0.82 1.05] |
0.93 | [0.82 1.05] |
||
| Ever obese | 0.85** | [0.77 0.94] |
0.83*** | [0.75 0.92] |
||||
| Ever drink | 0.88* | [0.78 0.98] |
0.85** | [0.76 0.96] |
||||
| Ever smoke | 1.12* | [1.01 1.26] |
1.09 | [0.97 1.21] |
||||
| Interview in English | 1.24* | [1.04 1.46] |
1.17 | [0.99 1.39] |
||||
| No. of chronic conditions | 1.18*** | [1.14 1.23] |
||||||
| Observations | 2,290 | |||||||
| Panel B: Males | ||||||||
| Age of Migration (Ref = U.S. Born) | ||||||||
| Early-life (0–19) | 0.95a | [0.80 1.14] |
0.96a | [0.81 1.15] |
1.05a | [0.88 1.26] |
1.05a | [0.87 1.26] |
| Midlife (20–49) | 0.74*** | [0.64 0.85] |
0.75*** | [0.65 0.86] |
0.81** | [0.70 0.94] |
0.82** | [0.71 0.94] |
| Late-life (50+) | 0.92a | [0.75 1.11] |
0.93a | [0.76 1.14] |
0.99a | [0.80 1.21] |
1.01 | [0.82 1.24] |
| Education | 1.01 | [0.99 1.02] |
0.99 | [0.98 1.01] |
0.99 | [0.98 1.01] |
||
| Financial strain | 1.14* | [1.01 1.29] |
1.16* | [1.02 1.31] |
1.16* | [1.02 1.31] |
||
| Married | 0.90 | [0.76 1.06] |
0.94 | [0.80 1.11] |
0.95 | [0.80 1.12] |
||
| Live alone | 1.10 | [0.90 1.35] |
1.10 | [0.90 1.36] |
1.14 | [0.93 1.40] |
||
| Ever obese | 0.74*** | [0.66 0.84] |
0.73*** | [0.65 0.83] |
||||
| Ever drink | 0.89 | [0.77 1.04] |
0.87 | [0.75 1.02] |
||||
| Ever smoke | 1.20** | [1.05 1.37] |
1.18* | [1.03 1.34] |
||||
| Interview in English | 1.78*** | [1.48 2.13] |
1.69*** | [1.41 2.03] |
||||
| No. of chronic conditions | 1.14*** | [1.09 1.19] |
||||||
| Observations | 1,662 | |||||||
Notes: All models control for proxy response and birth cohort. For age of migration coefficients, a Wald test is used to test for significant group differences.
aDenotes coefficients that are significantly different than midlife coefficients.
HR = Hazard ratios; CI = 95% Confidence intervals.
*p < .05; **p < .01; ***p < .001.
Next, we estimate the association between age of migration and mortality for men (Panel B). We find that midlife migration among men is associated with a 26% lower risk of mortality compared to U.S.-born respondents (Model 1). In addition, our results indicate that among the foreign-born, migrating in midlife is associated with significantly lower mortality than those migrating in early-life or late-life. The association between age of migration and mortality remains net of controls for socioeconomic and demographic characteristics (Model 2). Controlling for differences in health behaviors and language of interview decreases the mortality advantage associated with migrating in midlife from a 25% to 19% lower risk of mortality (Model 3). Controlling for baseline health does not change the mortality advantage associated with midlife migration for men relative to their U.S.-born counterparts or early-life migrants; however, significant differences between late-life migrant men are no longer evident (Model 4).
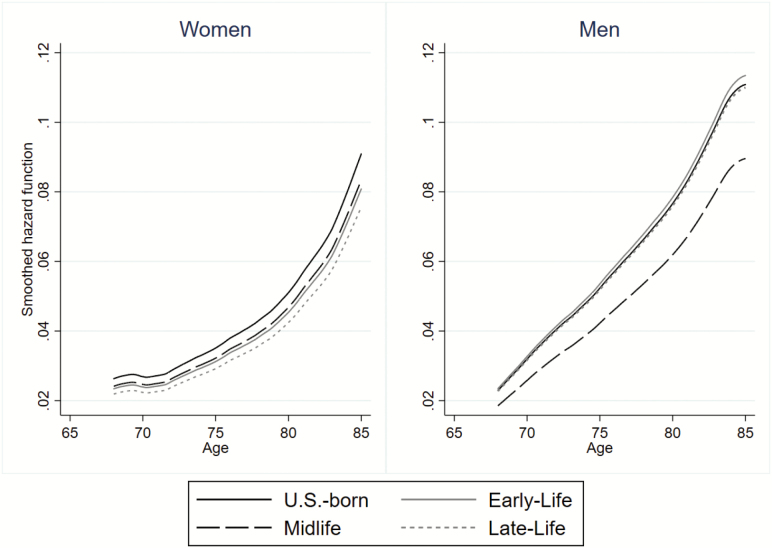
Results from our stratified models indicate that the mortality advantage observed among midlife migrants in the combined sample is largely driven by men, whereas the mortality advantage among late-life migrants in the combined sample is largely driven by women. To illustrate gender differences in mortality by age of migration, we plot smoothed hazard rates for men and women controlling for sociodemographic characteristics and health behaviors (Figure 1). U.S.-born respondents exhibit the highest mortality hazards among women, though for men they are not significantly different from early-life and late-life migrants. However, important gender differences by age of migration are evident in the hazard of mortality. Among women, late-life migrants have the lowest mortality, followed by early-life and midlife migrants. In contrast, midlife migrant men exhibit the lowest mortality. Although foreign-born migrants exhibit lower mortality compared to U.S.-born respondents; age of migration confers different mortality benefits to men and women. Comparing the hazards by gender, men’s hazards of mortality for all groups are higher and steeper compared to the mortality hazards of women, reflecting shorter life expectancies on average for men regardless of nativity or age of migration.
Figure 1.
Mortality hazards by gender and age of migration plotted from Stratified Cox models presented in Table 3, Model 4.
Discussion
In this study, we used a gendered life course perspective to assess whether the association between age of migration and mortality is moderated by gender. Research combining mortality profiles of men and women in a singular group can obscure complex gender patterns related to individual-level characteristics and socio-cultural factors that influence the risk of mortality. We contribute to the growing body of research investigating the immigrant health paradox by examining the association between age of migration and mortality among Mexican Americans and documenting how age of migration interacts with gender in unique ways to affect mortality. Recently matched mortality data through 2016 allows us to examine a longer follow-up period for death than previous studies. This provides us a large enough sample to contextualize the heterogeneous mortality profiles of older Mexican American men and women.
Consistent with previous research, we find support for our first hypothesis stating that age of migration is associated with mortality among older Mexican Americans (Angel et al., 2010; Colón-López et al., 2009). Our results show immigrants who arrived in midlife and to some extent late-life have a significantly lower risk of mortality compared to their U.S.-born co-ethnics reflecting similar patterns observed among a national sample of Hispanics 25 years and older (Holmes et al., 2015). However, this advantage does not extend to early-life migrants and is no longer significant for late-life migrants once we controlled for health behaviors related to acculturation. Building on prior studies (Angel et al., 2010; Colón-López et al., 2009; Holmes et al., 2015), we find that the association between age of migration and mortality is moderated by gender indicating selection mechanisms and acculturation processes operate differently for immigrant men and women. Specifically, we document mortality advantages among midlife migrant men and late-life migrant women relative to U.S.-born men and women, supporting our second hypothesis.
Previous studies have documented inconsistent age of migration findings, with either midlife and/or late-life migrants exhibiting a mortality advantage (Angel et al., 2010; Colón-López et al., 2009; Holmes et al., 2015). Our results may differ from prior research due to differences in data sources and length of follow-up for mortality data (23 years for current analysis vs. 13 years for Angel and colleagues) that allows the inclusion of an additional 900 deaths. In addition, evidence of a disadvantage in CVD mortality among early-life migrants in Sacramento was based on a shorter follow-up (8 years) and included a significantly smaller sample (n = 789) than the current study. More importantly, these studies did not account for gender differences in the association between age of migration and mortality. Studies that do not account for gender differences in the effects of age of migration obscure the heterogeneity between male and female midlife migrants. Our results demonstrate that pooling estimates for men and women downwardly biases the size of the mortality advantage for midlife males. Specifically, we document that the mortality advantage among midlife migrants observed in the pooled estimate increases from 17% to 26% for males in stratified models and is not significant for females.
The mortality advantage among midlife migrants was observed for men relative to their U.S.-born co-ethnics, but not for women, which may reflect patterns of selective migration exclusive to men. These migrant men came during their prime working ages in search of occupational and economic opportunities in physically demanding jobs (Garcia & Reyes, 2018). Consistent with prior studies, we find men who migrated as children have similar mortality profiles as their U.S.-born co-ethnics (Angel et al., 2010; Holmes et al., 2015). These findings corroborate previous research documenting health advantages among midlife migrant men in disability, functional limitations, and cognitive functioning (Garcia & Reyes, 2018; Garcia, Valderrama-Hinds, et al., 2017; Hill et al., 2012; Monserud, 2019).
Among women, late-life migrants exhibited a significantly lower risk of mortality relative to U.S.-born Mexican Americans, which did not extend to men. The magnitude of this mortality advantage remains with the inclusion of socioeconomic controls. Lower mortality among late-life migrant women may be attributed in part to socio-cultural characteristics from their country of origin that influence lifestyle risk factors across the life course. Shorter lifetime exposure to negative health behaviors associated with U.S. culture may contribute to late-life migrant women retaining healthy behaviors that influence survival selection processes. Previous research conducted with the H-EPESE suggests that lower mortality among immigrant women may be attributed to greater social support in communities with large populations of co-ethnics (Eschbach et al., 2004). Despite the large mortality advantage of late-life migrant women, this advantage does not extend to other health domains. Research shows that late-life migrant women spend a larger proportion of their late life years with functional limitations, and cognitive impairment to with U.S.-born Mexican Americans (Garcia, Saenz, et al., 2017; Garcia, Valderrama-Hinds, et al., 2017).
Although previous research has attributed lower mortality among older foreign-born Mexicans to low rates of smoking compared to their U.S.-born co-ethnics (Fenelon, 2013; Lariscy et al., 2015), we found that the association between smoking and higher mortality did not change the magnitude of the association between age of migration and mortality. Our findings are consistent with research that has found smoking does not explain differences in mortality by duration in the United States among Hispanics (Riosmena, Everett, Rogers, & Dennis, 2015). Although we control for other aspects of health behaviors (obesity and alcohol consumption), there may be unmeasured socio-cultural factors that contribute to mortality advantages among late-life women.
This study has some limitations. First, we are unable to account for legal status or citizenship. Migrants with documentation, particularly those who have naturalized, have better access to public resources and opportunities that likely accumulate and lead to better health over the life course (Gubernskaya et al., 2013). Second, we are only tapping into stable or relatively current measures of SES at the end of the life course. Precarious SES and legal status vulnerability during the life course of migrants may have long-term health impacts (Hayward & Gorman, 2004). Third, similar to other studies of immigrant mortality, we are unable to capture any deaths for individuals who return to Mexico. Previous studies have found that relatively low rates of return migration (salmon bias) among foreign-born Mexican Americans do not explain the lower mortality observed among migrants (Riosmena et al., 2015). Fourth, we are unable to capture other elements of the migration process that may be relevant to health including racial discrimination and stress (Cano et al., 2016; Lopez et al., 2017; Vargas, Sanchez, & Juárez, 2017). Finally, our results are based on a population-based sample of Mexican Americans 65 years and older residing in the Southwestern United States and thus may not be generalizable to younger generations of Mexican Americans or to those living outside the Southwest, for instance, those living in new immigrant destinations.
Despite these limitations, this study makes an important contribution to existing research on immigrant mortality. Using a gendered life course perspective, we demonstrate how different migration experiences may be associated with late-life mortality for older migrants. Understanding mortality patterns among Mexican migrants in the Southwest has important implications for families, caregivers, and governmental agencies. Given the advantage in mortality observed among late-life migrant women combined with an extended period of serious impairment late-life migrant women may be an especially important group in need of caregiving at the end of life. Our findings suggest that understanding how gender and age of migration interact to influence mortality can be informative in the development of targeted interventions aimed at vulnerable populations. Although we highlight the heterogeneity in all-cause mortality by gender and age of migration, future work investigating specific causes of death may help identify some of the mechanisms linking gender and age of migration with mortality.
Conflict of interest: None reported.
Funding
This work was supported by the National Institute on Aging (grant numbers T32AG000221 [to A. M. Reyes], T32AG00270 [to M. A. Garcia], and R01 AG010939), and the Nebraska Tobacco Settlement Biomedical Research Development Funds through the University of Nebraska-Lincoln. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Author Contributions
A. M. Reyes planned the study, conducted data analysis, and wrote the paper. M. A. Garcia helped plan the study and write and revise the paper.
References
- Angel R. J., Angel J. L., Díaz Venegas C., & Bonazzo C (2010). Shorter stay, longer life: Age at migration and mortality among the older Mexican-origin population. Journal of Aging and Health, 22, 914–931. doi:10.1177/0898264310376540 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Angel J. L., Buckley C. J., & Sakamoto A (2001). Duration or disadvantage? Exploring nativity, ethnicity, and health in midlife. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 56, S275–S284. 10.1093/geronb/56.5.S275 [DOI] [PubMed] [Google Scholar]
- Antecol H., & Bedard K (2006). Unhealthy assimilation: Why do immigrants converge to American health status levels? Demography, 43, 337–360. doi:10.1353/dem.2006.0011 [DOI] [PubMed] [Google Scholar]
- Arias E., Heron M., & Xu J (2017). United states life tables, 2014. National Vital Statistics Reports: From the Centers for Disease Control and Prevention, National Center for Health Statistics, National Vital Statistics System, 66, 1–64. [PubMed] [Google Scholar]
- Bostean G. (2013). Does selective migration the Hispanic paradox? A comparative analysis of Mexicans in the U.S. and Mexico explain. Journal of Immigrant and Minority Health, 15, 624–635. doi:10.1007/s10903-012-9646-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burr J., Gerst K., Kwan N., & Mutchler J (2008). Economic well-being and welfare program participation among older immigrants in the United States. Generations, 32(4), 53–60. [Google Scholar]
- Cano M. Á., Castro Y., de Dios M. A., Schwartz S. J., Lorenzo-Blanco E. I., Roncancio A. M.,… Zamboanga B. L (2016). Associations of ethnic discrimination with symptoms of anxiety and depression among Hispanic emerging adults: A moderated mediation model. Anxiety, Stress, and Coping, 29, 699–707. doi:10.1080/10615806.2016.1157170 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carr S., & Tienda M (2013). Family sponsorship and late-age immigration in aging America: Revised and expanded estimates of chained migration. Population Research and Policy Review, 32(6), 825–849. doi:org/10.1007/s11113-013-9300-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Colón-López V., Haan M. N., Aiello A. E., & Ghosh D (2009). The effect of age at migration on cardiovascular mortality among elderly Mexican immigrants. Annals of Epidemiology, 19, 8–14. doi:10.1016/j.annepidem.2008.08.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cox D. R. (1972). The statistical analysis of dependencies in point processes. In Lewis, PAW (ed), Stochastic Point Processes: Statistical Analysis, Theory, and Applications, edited by New York: Wiley, 55–66. [Google Scholar]
- Dannefer D. (2003). Cumulative advantage/disadvantage and the life course: Cross-fertilizing age and social science theory. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 58, S327–S337. doi:10.1093/geronb/58.6.S327 [DOI] [PubMed] [Google Scholar]
- Donato K. M. (2010). US migration from latin america: Gendered patterns and shifts. Annals of the American Academy of Political and Social Science, 630, 78–92. doi:10.1177/0002716210368104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elder G. H. Jr, Johnson M. K., & Crosnoe R (2003). The emergence and development of life course theory. In Jeylan T. Mortimer and Michael J. Shanahan (eds) Handbook of the life course (pp. 3–19). New York:Springer. [Google Scholar]
- Eschbach K., Al-Snih S., Markides K. S., & Goodwin J. S (2007). Disability and active life expectancy of older US-and foreign-born Mexican Americans. In Angel, Jacqueline L., and Keith E. Whitfield, (eds) The health of aging Hispanics (pp. 40–49). New York:Springer. [Google Scholar]
- Eschbach K., Ostir G. V., Patel K. V., Markides K. S., & Goodwin J. S (2004). Neighborhood context and mortality among older Mexican Americans: Is there a barrio advantage? American Journal of Public Health, 94, 1807–1812. doi: 10.2105/AJPH.94.10.1807 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fenelon A. (2013). Revisiting the Hispanic mortality advantage in the United States: The role of smoking. Social Science & Medicine (1982), 82, 1–9. doi:10.1016/j.socscimed.2012.12.028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fenelon A., Chinn J. J., & Anderson R. N (2017). A comprehensive analysis of the mortality experience of hispanic subgroups in the United States: Variation by age, country of origin, and nativity. SSM – Population Health, 3, 245–254. doi:10.1016/j.ssmph.2017.01.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferraro K. F., Kemp B. R., & Williams M. M (2017). Diverse aging and health inequality by race and ethnicity. Innovation in Aging, 1, igx002. doi:10.1093/geroni/igx002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garcia M. A., Garcia C., Chiu C.-T., Raji M., & Markides K. S (2018). A Comprehensive analysis of morbidity life expectancies among older hispanic subgroups in the United States: Variation by nativity and country of origin. Innovation in Aging, 2(2), igy014–igy014. doi:10.1093/geroni/igy014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garcia M. A., & Reyes A. M (2018). Physical functioning and Disability Trajectories by age of migration among Mexican elders in the United States. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 73, 1292–1302. doi:10.1093/geronb/gbw167 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garcia M. A., Saenz J. L., Downer B., Chiu C.-T., Rote S., & Wong R (2017). Age of migration differentials in life expectancy with cognitive impairment: 20-year findings from the hispanic-EPESE. The Gerontologist, 58, 894–903. doi:10.1093/geront/gnx062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garcia M. A., Valderrama-Hinds L. M., Chiu C. T., Mutambudzi M. S., Chen N. W., & Raji M (2017). Age of migration life expectancy with functional limitations and morbidity in Mexican Americans. Journal of the American Geriatrics Society, 65, 1591–1596. doi:10.1111/jgs.14875 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gubernskaya Z. (2015). Age at migration and self-rated health trajectories after age 50: Understanding the older immigrant health paradox. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 70, 279–290. doi:10.1093/geronb/gbu049 [DOI] [PubMed] [Google Scholar]
- Gubernskaya Z., Bean F. D., & Van Hook J (2013). (Un)Healthy immigrant citizens: Naturalization and activity limitations in older age. Journal of Health and Social Behavior, 54, 427–443. doi:10.1177/0022146513504760 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayward M. D., & Gorman B. K (2004). The long arm of childhood: The influence of early-life social conditions on men’s mortality. Demography, 41, 87–107. 10.1353/dem.2004.0005 [DOI] [PubMed] [Google Scholar]
- Hill T. D., Angel J. L., Balistreri K. S., & Herrera A. P (2012). Immigrant status and cognitive functioning in late-life: An examination of gender variations in the healthy immigrant effect. Social Science & Medicine (1982), 75, 2076–2084. doi:10.1016/j.socscimed.2012.04.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holmes J. S., Driscoll A. K., & Heron M (2015). Mortality among US-born and immigrant Hispanics in the US: Effects of nativity, duration of residence, and age at immigration. International Journal of Public Health, 60, 609–617. doi:10.1007/s00038-015-0686-7 [DOI] [PubMed] [Google Scholar]
- Jasso G. (2003). Migration, human development, and the life course. In: Mortimer J.T., Shanahan M.J. (eds) Handbook of the Life Course. Handbooks of Sociology and Social Research. Springer, Boston, MA, 331–364. doi:10.1007/978-0-306-48247-2_16 [Google Scholar]
- Kimbro R. T. (2009). Acculturation in context: Gender, age at migration, neighborhood ethnicity, and health behaviors. Social Science Quarterly, 90(5), 1145–1166. 10.1111/j.1540-6237.2009.00651.x [DOI] [Google Scholar]
- Lariscy J. T., Hummer R. A., & Hayward M. D (2015). Hispanic older adult mortality in the United States: New estimates and an assessment of factors shaping the Hispanic paradox. Demography, 52, 1–14. doi:10.1007/s13524-014-0357-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lopez W. D., Kruger D. J., Delva J., Llanes M., Ledón C., Waller A.,… Israel B (2017). Health implications of an immigration raid: Findings from a latino community in the midwestern United States. Journal of Immigrant and Minority Health, 19, 702–708. doi:10.1007/s10903-016-0390-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Markides K. S., & Eschbach K (2005). Aging, migration, and mortality: Current status of research on the Hispanic paradox. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 60 (Spec No 2), 68–75. doi:10.1093/geronb/60.special_issue_2.s68 [DOI] [PubMed] [Google Scholar]
- Markides K. S., & Rote S (2015). Immigrant Health Paradox. In Robert A. Scott and Marlis C. Buchmann (eds.) Emerging Trends in the Social and Behavioral Sciences. New York: John Wiley & Sons, Inc. [Google Scholar]
- Markides K. S., Rudkin L., Angel R. J., & Espino D. V (1997). Health status of Hispanic elderly. Racial and Ethnic Differences in the Health of Older Americans, 285–300. doi:10.17226/5237 [Google Scholar]
- Massey D. S., Fischer M. J., & Capoferro C (2006). International migration and gender in Latin America: A comparative analysis. International Migration (Geneva, Switzerland), 44, 63–91. doi:10.1111/j.1468-2435.2006.00387.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monserud M. A. (2019). Age trajectories of physical health among older adults of Mexican descent: Implications of immigrant status, age at immigration, and gender. Journal of Aging and Health, 31, 3–36. doi:10.1177/0898264317721823 [DOI] [PubMed] [Google Scholar]
- Monserud M. A., & Markides K. S (2018). Age trajectories of depressive symptoms by age at immigration among older men and women of mexican descent: The role of social resources. Sociological Perspectives, 61(4), 513–534. doi:10.1177/0731121417751378. [Google Scholar]
- Palloni A., & Arias E (2004). Paradox lost: Explaining the Hispanic adult mortality advantage. Demography, 41, 385–415. doi:10.1353/dem.2004.0024 [DOI] [PubMed] [Google Scholar]
- Read J. G., & Reynolds M. M (2012). Gender differences in immigrant health: The case of Mexican and Middle Eastern immigrants. Journal of Health and Social Behavior, 53, 99–123. doi:10.1177/0022146511431267 [DOI] [PubMed] [Google Scholar]
- Riosmena F., Everett B. G., Rogers R. G., & Dennis J. A (2015). Negative acculturation and nothing more? cumulative disadvantage and mortality during the immigrant adaptation process among latinos in the United States. The International migration review, 49, 443–478. doi:10.1111/imre.12102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riosmena F., Wong R., & Palloni A (2013). Migration selection, protection, and acculturation in health: A binational perspective on older adults. Demography, 50, 1039–1064. doi:10.1007/s13524-012-0178-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Royston P. (2005). Multiple imputation of missing values: Update. Stata Journal, 5(2), 188. doi: 10.1177/1536867X0500500204 [Google Scholar]
- Rumbaut R. G. (2004). Ages, life stages, and generational cohorts: Decomposing the immigrant first and second generations in the United States. International Migration Review, 38(3), 1160–1205. doi:10.1111/j.1747–7379.2004.tb00232.x [Google Scholar]
- Treas J. (2015). Incorporating immigrants: Integrating theoretical frameworks of adaptation. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 70, 269–278. doi:10.1093/geronb/gbu067 [DOI] [PubMed] [Google Scholar]
- Treas J., & Gubernskaya Z (2016). Immigration, aging, and the life course. In Linda K. George and Kenneth F. Ferraro (eds) Handbook of Aging and the Social Sciences (8th ed., pp. 143–161): San Diego, CA: Academic Press. [Google Scholar]
- Treas J., & Mazumbdar S (2002). Older people in America’s immigrant families: Dilemmas of dependence, integration, and isolation. Journal of Aging Studies, 16(3), 243–258. doi:10.1016/s0890-4065(02)00048-8 [Google Scholar]
- Vargas E. D., Sanchez G. R., & Juárez M (2017). Fear by association: Perceptions of anti-immigrant policy and health outcomes. Journal of Health Politics, Policy and Law, 42, 459–483. doi:10.1215/03616878-3802940 [DOI] [PMC free article] [PubMed] [Google Scholar]
- White I. R., & Royston P (2009). Imputing missing covariate values for the Cox model. Statistics in Medicine, 28, 1982–1998. doi:10.1002/sim.3618 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Willson A. E., & Shuey K. M (2016). Life course pathways of economic hardship and mobility and midlife trajectories of health. Journal of Health and Social Behavior, 57, 407–422. doi:10.1177/0022146516660345 [DOI] [PubMed] [Google Scholar]
- Young R., & Johnson D. R (2015). Handling missing values in longitudinal panel data with multiple imputation. Journal of Marriage and the Family, 77, 277–294. doi:10.1111/jomf.12144 [DOI] [PMC free article] [PubMed] [Google Scholar]