Abstract
The main purpose of this study is to describe how negative emotions were investigated in the sphere of dermatological diseases, in order (1) to summarize literature trends about skin disorders and emotions, (2) to highlight any imbalances between the most studied and neglected emotions, (3) and to offer directions for future research. A computerized literature search provided 41 relevant and potentially eligible studies. Results showed that the study of emotions in skin disease is limited to Sadness/depression and Fear/anxiety. The emotions of Anger and Disgust have been poorly explored in empirical studies, despite they could be theoretically considered a vulnerability factor for the development of skin disorders and the dermatological extreme consequences, as negative emotionality toward self and the pathological skin condition. The bibliometric qualitative analysis with VOSViewer software revealed that the majority of the studies have been focused on the relationships between vitiligo and Sadness/depression, dermatitis and Fear/anxiety, psoriasis, and Anger, suggesting the need of future research exploring Disgust and, in general, a wider emotional spectrum.
Keywords: negative emotions, skin disorders, depression, anxiety, anger, disgust
Resumen.
El objetivo principal de este estudio fue describir cómo se han investigado las emociones negativas en el ámbito de las enfermedades dermatológicas, con el fin de (1) resumir las tendencias de la literatura sobre las enfermedades de la piel y las emociones, (2) para resaltar las diferencias entre las emociones más estudiados y las más descuidadas y (3) ofrecer direcciones para futuras investigaciones. Una búsqueda bibliográfica computarizada proporcionó 41 estudios relevantes y potencialmente elegibles. Los resultados mostraron que el estudio de las emociones en la enfermedad de la piel se limita a Tristeza/depresión y Miedo/ansiedad. Las emociones de la ira y el asco han sido poco exploradas en estudios empíricos, a pesar de que teóricamente podrían considerarse un factor de vulnerabilidad para el desarrollo de enfermedades de la piel y las consecuencias dermatológicas extremas, como la emocionalidad negativa hacia uno mismo y la condición patológica de la piel. El análisis cualitativo bibliométrico con el software VOSViewer reveló que la mayoría de los estudios se han centrado en las relaciones entre vitiligo y Tristeza/depresión, dermatitis y Miedo/ansiedad, psoriasis e Ira, lo que sugiere la necesidad de futuras investigaciones que exploren asco y, en general, un espectro emocional más amplio.
Palabras Clave: emociones negativas, enfermedades de la piel, depresión, ansiedad, ira, asco
1. Introduction
From the physiological point of view, the skin is an organ strictly linked to emotional activities: redness, pallor, sweating, itching can be consequences of somatic activation, expressing a range of affective feeling-states. The relationship between psychological distress and skin alterations has always been a topic of great interest for researchers and clinicians. Unlike many other organs in the body, the human epidermis has an immediate reaction to mental stress, so that several authors aimed to demonstrate the so-called “brain-skin connection” (Paus, Theoharides, & Arck, 2006; Arck et al., 2010). It was found that mental, physical, and emotional stress definitely affects the skin and this may depend on several reasons. In stressful conditions, in fact, hormones relapse encourages inflammation and the decreasing blood flow to the skin (Dhabhar, 2000), irritating the skin nerves and increasing inflammation or allergic reactions, with systemic alterations of neuroendocrine and immunological parameters (Pavlovic et al., 2008). Furthermore, skin recruits the immune system to fight, dysregulating the innate immune response and causing inflammations such as Rosacea, Acne, and Psoriasis (Yamasaki & Gallo, 2009). As a consequence, triggering a vicious circle, natural moisturizing factors, and plumping lipids production decline and skin healing, repair, and restoration processes are delayed (Eming, Krieg, & Davidson, 2007).
The connection between skin and mind has deep roots and is the object of a specific clinic and research field called Psychodermatology. Research hypothesis has arisen spontaneously on the basis of careful observation of clinical data in medical settings and active collaboration between dermatologists, psychiatrists and psychologists. In the last twenty years, a number of dermatological studies have shown that people affected by a skin disorder often have a related psychological problem. For example, Gupta and Gupta (2001) have observed that patients with dermatological diseases show high rates of comorbid Major Depressive Disorder (MDD), Obsessive Compulsive Disorder (OCD), Body Dysmorphic Disorder, Social Phobia, and Post-Traumatic Stress Disorder (PTSD), which required prescriptions for anxiolytic and antidepressant medications. Picardi, Abeni, Melchi, Puddu, and Pasquini (2000) showed that the prevalence of emotional disorders was even 25.2% in about 2500 outpatients of a dermatological clinic. More specifically, a prevalence of more than 30% was found in patients with acne, pruritus, urticaria and alopecia.
In the study carried on by Gieler, Niemeier, Kupfer, Brosig, and Schill (2001), a survey was sent to 69 dermatology hospitals. In nearly all dermatoses, with the exception of hyperhidrosis and seborrheic eczema, the authors found that the extent of emotional influences was increased, compared to a similar study performed ten years before. However, the most interesting result was the discovery of a subpopulation of about 23% of dermatology patients with psychosomatic disorders.
Fritzsche et al. (2001), using the ICD-10 criteria for the assessment of mental disorders, found mental, emotional, and behavioral disorders -of which the most frequent were mood and anxiety disorders- in 46% of 86 dermatological patients. Depression and anxiety, in fact, are mostly risk factors for several skin diseases, as can be seen in empirical studies on psoriasis vulgaris (Devrimci-Ozguven, Kundakci, Kumbasar, & Boyvat, 2000).
Furthermore, there are some review studies that have sought to establish relationships between psychiatric disorders and skin disorders. Buljan, Buljan, and Situm (2005), arguing that the treatment of psychodermatologic disorders is almost impossible without a holistic team approach involving psychiatrist, dermatologist and psychologist, proposed a review about psycho-dermatologic disorders, the psychosomatic disorders, primary psychiatric disorders, and secondary psychiatric disorders. The review conclusion is that psychopharmacologic treatment with anxiolytics, antidepressants, antipsychotics, and mood stabilizers can be prescribed by the dermatologist after consulting the psychiatrist.
Even Yadav, Narang, and Kumaran (2013) presented a comprehensive review of salient features and treatment updates in primary psychiatric dermatoses and also discussed the secondary psychiatric morbidity. The authors’ aim was to allow the dermatologist to be able to initiate basic pharmacotherapy, to know about various non-pharmacological treatments, such as psychotherapy, and the right time to refer the patient to the psychiatrist.
Again, Tareen and Tareen (2015) described how major affective disorders (such as major depression and bipolar disorders), anxiety spectrum disorders (such as social phobia and obsessive-compulsive disorder), and some commonly encountered personality disorders are frequently encountered in patients with skin conditions, often complicating the treatment plan and creating a viscous cycle where both disease processes keep perpetuating each other.
More recently, Krooks, Weatherall, and Holland (2017) discussed the etiology, epidemiology, clinical presentation, diagnosis, and first-line treatment of specific primary psychiatric causes of dermatologic conditions, writing a review, useful as a guide for dermatologists to use while prescribing atypical antipsychotics, selective serotonin reuptake inhibitors, and tricyclic antidepressants and/or cognitive behavioral therapy.
However, this literature review highlights some critical points. First of all, the common denominator is that these studies are psychiatric/medical guidelines, focused on the dermatological clinical practice and management, and not on psychological features or to the comprehension of such mechanisms. As stated by Marshall, Taylor, and Bewley (2016) “patients who present to a psycho-dermatology clinic usually believe they have a primary skin problem (though this is not always the case)” (p. 31). Hence, there is the need of a study taking into account not only the nosographic aspects, or specific skin disorders, but also the different types of skin disorders and affective components, by including the entire range of negative emotions, that is, sadness, fear, anger, and disgust.
In the comprehension of patient suffering it should be considered the link between skin, skin pathologies, emotions, emotion expression, and emotion pathology. Among skin disorders there is a psychosomatic quote. Several psychodynamics theories suggest that the affected skin represents the expression of a negative emotion that is difficult for the individual to differentiate and describe. However, the role played by emotions is still unclear. It has not been yet established if negative emotions can be considered a reaction to the pathological condition or if, as stable response patterns, they can increase the vulnerability for the development of skin diseases. To reach this purpose a literature review is necessary, in order to understand how negative emotions have been studied hereinbefore, and to plan future studies answering to this issue and helping clinicians to identify the most effective treatments, both dermatological and psychological, for these patients.
From these premises, the main aim of this study is to describe how negative emotions were investigated in the sphere of dermatological diseases, in order (1) to summarize literature trends about skin disorders and emotions, (2) to highlight any imbalances between the most studied and the most neglected emotions, (3) and to offer directions for future research.
2. Methods
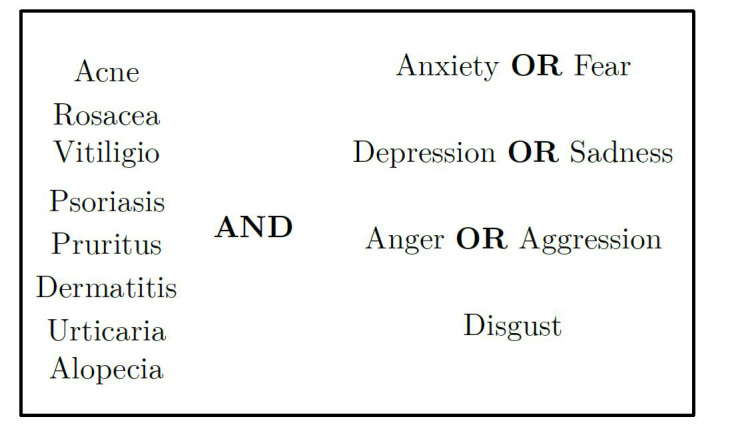
A computerized literature searches of each item contained in the ICD-10 classification for skin diseases -from code L00 to L99- has been conducted on three scientific article databases: Psyc-INFO, Web of Science, and PubMed; moreover, in order to obtain even the most obscure information, an electronic search on Google Scholar has been carried on. For many skin disorders, the search did not produce any relevant results to the field of emotions. Figure 1 shows some of the terms inserted on the literature search, representing the most popular results. Anyway, at the beginning of the research, each skin disorder has been associated with each emotion.
Figure 1. Literature search terms.
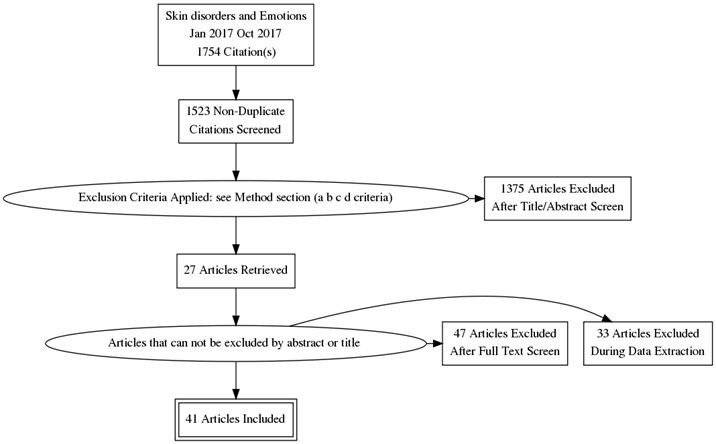
Search limits restricted the results to: 1) research articles published in English between 2000 and 2017 and identified as empirical, epidemiological or longitudinal studies; 2) researches conducted in a clinical sample; 3) measuring negative emotions such as sadness, disgust, anger and fear. As regards exclusion criteria, the search did not include: a) Studies on Quality of Life (681); b)
Studies on caregivers of skin disordered patients (315); c) Studies on children or adolescents (287); d) Dermatological review studies, book chapters, dissertation, and thesis (92). Following this second stage in the screening process, 41 studies provided relevant and potentially eligible information for coding. According to the recommendation of Moher and the Prisma Group (2009), Figure 2 shows the detailed flow chart with all research steps and selection criteria.
Figure 2. Systematic Review Flow Chart.
For each publication, data regarding authors name, year of publication, country of the study (population, instruments language), the skin disorders observed, the psychological instruments used, and the main results, were entered in a spreadsheet (MS Excel 5.0) to allow the construction of synthetic tables. To understand the relationship between skin and emotions we have divided the studies on the basis of the primary emotions considered: 1) sadness; 2) fear; 3) anger; 4) disgust. However, despite anxiety and depression are separate syndromes, they often co-occur. Hence, data of the studies that considered both the diseases have been grouped, to avoid duplicate, resulting in two tables. Finally, the qualitative data analysis was conducted using VOSviewer 1.6.1, a software tool for constructing and visualizing bibliometric networks based on data downloaded from bibliographic databases (Van Eck & Waltman, 2014). It produces a bubble map through the analyses of words reported in publications’ titles and abstracts. Each bubble represents a keyword or a phrase. The bubble size and color, and inter-Buble distance indicate keyword’s frequency, citation per publication (CPP) count, and frequency of co-occurrence or corresponding terms in publications, respectively (Van Eck & Waltman, 2014).
3. Results
3.1 Skin disorders, Sadness/Depression and Fear/Anxiety
From a clinical point of view, sadness is the typical emotion of loss, disappointment, separation, mourning. The intensity of sadness depends on the value that the indi-
vidual attributes to the loss, and the purposes which the loss incurred compromise. The more it is considered indispensable, irreplaceable and irretrievable what it lacks, the more intense and prolonged will be the emotional response of sadness (Lewis, Haviland-Jones, & Barrett, 2010). It is necessary to distinguish depression by “moments of sadness”, which may be present in the life of every individual and usually have fairly obvious causes and are characterized by a limited duration. Instead, depression and the states of melancholy mood usually are long lasting and accompanied by: a) low self-esteem; b) loss of interest and/or pleasure in activities that are normally pleasurable for the subject (anhedonia); c) lack of motivation. In fact, depression is contemplated in the international classifications of mood disorders (Wakefield & Demazeux, 2016). Conceptually, it is impossible to study the emotion of sadness as a primary emotion, as the existing literature was mainly interested and focused on the pathological expression of sadness, i.e., depression. Moreover, in the case of dermatological disorders there may be a moment of physiological sadness linked to the diagnosis, but the more interesting object is the pathological, prolonged, and pervasive sadness, because of the increased level of subjective suffering and psychological pain. To date, too little is known about the role played by this emotion. It is consolidated that the two conditions co-occur, but it is not clear whether the depression is the result of the failure to accept the diagnosis (i.e., a secondary disease) or if the depression, as pre-existing condition, could increase the vulnerability to the development of the somatic disorder.
A similar discussion regards the emotion of fear, an immediate response to danger and undoubtedly a close relative of anxiety. Both are the response to a “threat”. However, even though anxiety and fear are similar in their physiological manifestation (through physical symptoms such as rapid heartbeat, difficulty in breathing, sweating, tightness, etc.), they differ substantially: fear is an emotional reaction to a real danger, while anxiety is an emotional reaction to a perceived danger (Perusini & Fanselow, 2015). The studies analyzed refer to the latter category, that is, to the pathological fear activation (anxiety). Up to date, we can only hypothesize that anxiety may worsen the course of dermatological pathology or may negatively influence the outcome and management of the disease, which is often chronic. Moreover, is not established if the anxiety trait can predispose to the development of dermatological pathologies, although many of them have been found in correlation.
Table 1 represents the characteristics of the studies that explored Sadness/Depression and Fear/Anxiety in Skin Disorders. As stated, depression and anxiety often co-occur. We found 29 studies (only 8 measuring exclusively depression), which explored depression and anxiety in skin disordered patients. Studies increased in the last years, but are homogeneous in different continents such as Europe, Asia, and America, showing how the incidence of depression and anxiety are similar in different cultural and ethnic groups and also in the comparison between different skin disorders. However, it can be observed that the majority of the studies were focused on vitiligo and psoriasis (65.5%), and often the two groups are compared, with almost all studies reporting higher levels of depression and anxiety in favor of the psoriatic patients.
Table 1. Characteristics of the researches studying Sadness/Depression and Fear/Anxiety in Skin Disorders.
| Author | Country | Skin disorder | Sample | Measure | Results |
| Mattoo, Handa, Kaur, Gupta, and Malhotra (2001) | India | Vitiligo and Psoriasis | 113 patients with vitiligo (30.11±12.49) and 103 with psoriasis (40.91±14.26) | ICD-10 psychiatric diagnoses and General Health Questionnaire (GHQ) | Positive cases of depressive episode were 22% vs 29% in vitiligo and psoriasis, respectively. Depression, anxiety, and total psychopathology levels were similar in the two GHQ positive subgroups |
| Sharma, Koranne, and Singh(2001) | India | Vitiligo and Psoriasis | 30 untreated psoriasis and vitiligo patients aged 18-60 yrs | General Health Questionnaire (GHQ-H) | The prevalences of depression were 23.3% and 10% in psoriasis and vitiligo respectively and anxiety was observed in 3.3% of each group. |
| Esposito, Saraceno, Giunta, Maccarone, and Chimenti (2006) | Italy | Psoriasis | 2.391 patients | Center for Epidemiological Studies-Depression Scale (CES-D) questionnaire Depressive symptomatology was observed in 1.482/2.391 patients (62% overall) | |
| Engin, Uguz, Yilmaz, Özdemir, and Mevlitoglu (2008) | Turkey | Chronic idiopathic urticaria (CIU) | 73 patients with CIU, and 34 healthy subjects matched for age and sex | Beck Depression Inventory (BDI), the Beck Anxiety Inventory (BAI) | When compared with healthy controls, patients with CIU had significantly higher BDI and BA scores |
| Ahmed, Ahmed, and Nasreen (2007) | Pakistan | Vitiligo | 100 patients 15-60 years with a mean age of 24.6 years | Psychiatric Assessment Schedule (PAS) | Major depressive illness (15), was the most frequent psychiatric illness followed by generalized anxiety (10), mixed anxiety and depression, social phobia, agarophobia and sexual dysfunction |
| Tabolli et al. (2008) | Italy | Pemphigus vulgaris and pemphigus foliaceus | 58 patients of whom 47% < 50 years 53% >50 years | 36-item short form health survey (SF-36); SQ anxiety scale questionnaire; Clinical Depression Questionnaire | Patients with higher depression and anxiety had a more severe degree o mucocutaneous involvement |
| Ehsani, Toosi, Shahshahani, Arbabi, and Noormohammadpour (2009) | Iran | Neurotic excoriation, trichotillomania, delusion of parasitosis and dermatitis artefacta | 178 patients with psychocutaneous disorder (40.5± 15.6 years) | DSM-IV diagnostic criteria | Mood and anxiety disorders were common in patients with dermatitis artefacta, as patients with neurotic excoriation |
| Dieris-Hirche, Gieler, Kupfer, and Milch (2009) | Germany | Atopic Dermatitis (AD) | 62 adult atopic dermatitis patients and 62 healthy controls | HADS-D | A significantly higher level of suicidal ideation, anxiety and depression was shown among patients with atopic dermatitis |
| Abram, Silm, Maaroos, and Oona (2009) | Estonia | Rosacea | 70 consecutive patients (seekers) and 56 subjects with rosacea from population (non-seekers) | Mood Scale questionnaire and visual analogue scale (VAS) | Higher mean VAS scores were not related to severity of rosacea, but were associated with the presence of depressive symptoms among seekers. |
| Layegh, Arshadi, Shahriari, Pezeshkpour, and Nahidi (2010) | Iran | Psoriasis, acne, alopecia and vitiligo | 300 patients with a mean age of 26.55±10.81 years. | Beck depression questionnaire | The prevalence rate of clinical depression was found to be 47.4% in patients with acne; 69.4% in those with psoriasis; 70.1% in those suffering from vitiligo; 50% in diffuse alopecia areata; 60% in universalis alopecia areata; 100% in ophiasis alopecia areata and 68.3% in patients with localized alopecia areata. |
| Uhlenhake, Yentzer, and Feldman (2010) | North Carolina | Acne | Acne patients aged 18 and over | Total Resource Utilization BenchmarkOTM | Depression was two to three times more prevalent in acne patients than in the general population, with a reported 8.8% of acne patients having clinical depression. |
| Ghajarzadeh, Ghiasi, and Kheirkhah (2012) | Iran | psoriasis, vitiligo, and alopecia areata | 300 patients (100 with alopecia areata, 100 with psoriasis and 100 with vitiligo) | Beck Depression Inventory (BDI), SF-36 and Dermatology Life Quality Index (DLQI) | Significant correlation was found between DLQI and BDI in all disease groups (r = 0.44,P < 0.001). BDI scores were the highest in psoriasis group but this difference was not significant (P = 0.2). |
| Rashid et al. (2011) | Bangladesh | Vitiligo and Psoriasis | 50 patients with psoriasis 35.32±10.05 years and same number of patients with vitiligo 33.50±9.99 years and were compared | Diagnostic and Statistical Manual for Mental and Behavioural Disorders-Fourth Edition) DSM-IV | The proportion of major depressive disorders (MDD) was higher among psoriasis patients 15(30.0%) compared to vitiligo patients 04(8.0%). However, no statistical difference was found between two groups of patients in terms of anxiety disorders (8% in psoriasis and 12% in vitiligo patients). |
| Chan et al. (2012) | Singapore | Vitiligo | 145 vitiligo patients aged 21+ | Strucured questionnaire | Among the patients, 17.2% (n = 25) had been identified as depressed. |
| Alfani et al. (2012) | Italy | Alopecia Areata | 73 patients and 73 controls 35.2±9.2 and 35.1±9.1 years, respectively | Minnesota Multiphasic Personality Inventory (MMPI-2) | Some scales (i.e. Depression, Anxiety, Family relationships) were higher for patients with alopecia areata than for controls. |
| Al-Harbi (2013) | Saudi Arabia | Vitiligo | 308 vitiligo patients | Beck Depression Inventory Scale | According to the Beck Depression Scale, 54.5% were found to be depressed, most with mild depression. |
| Settineri, Guarneri, Saitta, Mento, and Cannavò (2013) | Italy | Seborrheic dermatitis and Psoriasis | Respectively: 33 with SD (39.85±15.45) and 36 psorisatic (41.11±13.72) years | Profile of Mood States (POMS) and the Toronto Alexithymia Scale TAS-20 | Two different depressive profiles emerged: psoriatic showed symptoms of major depression, SD patients to minor depression. |
| Sellami et al. (2014) | Tunisia | Alopecia areata (AA) | 50 patients-mean age 32.92 years | Hospital Anxiety and Depression scale questionnaire, Toronto Alexithymia scale 20, and Severity of Alopecia Tool. | Depression and anxiety were detected respectively in 38% and 62% of patients. |
| Duman, Ozdemir, Yucel, and Akin (2014) | Turkey | Pilonidal sinus | 205 patients: 107 operated with primary closure (26.4±4.5 years) and 98 Limberg flap reconstruction (28.3±4.8 years) | Beck Depression Inventory; Beck Anxiety Inventory; Short Form 36 | Mean Beck Depression Inventory (19±6.13 vs. 16±4.90 p < 0.001) and Beck Anxiety Inventory (19±6.27 vs. 16±4.90 p < 0.001) |
| Dalgard et al. (2015) | 13 countries | Infections of the skin and subcoutaneaous tissue | 3635 patients aged 47.2±17.9 years | Hospital Anxiety and Depression Scale | Clinical depression =10.1% Clinical Anxiety = 17.2% Suicidal Ideation = 12.7% |
| Pärna, Aluoja, and Kingo (2015) | Estonia | Dermatitis and Eczema | 40 patients with psoriasis, 40 with eczema, 40 with acne, 15 with seborrheic dermatitis and 40 healthy controls (M=38.9±14.5 ) | Emotional State Questionnaire (EST-Q); Dermatology Life Quality Index (DLQI); RAND-36-item HRQoL survey | Depression was similar in all dermatological groups. Anxiety was significantly higher in dermatological patients, compared to healthy controls (p = .005). |
| Kim et al. (2015) | Korea | Atopic Dermatitis (AD) | 1517 (19.8±1.0 years) | Korean Military Multiphasic Personality Inventory (KMPI) | The adjusted odds ratios for depression, anxiety, and somatization were significantly greater for individuals with AD compared with those without AD. |
| Cheng et al. (2015) | Taiwan | Atopic Dermatitis (AD) | 8208 (32.60±16.06years) | ICD-9 Diagnosis | Higher incidence of depressive disorder With AD=273(4.32)Without AD=48(0.74) <0.001 and Anxiety disorders With AD=180(2.83) Without AD=45(0.70) <0.001. |
| Konda et al. (2015) | India | Prurigo Nodularis (PN) | 39 patients with PN (27.87±17.6) and 39 age and gender matched healthy controls | Pruritus Grading Scale; Pittsburgh Sleep Quality Index; Hamilton rating scale for depression (HDRS) | Severity of depressive symptoms was significantly higher in PN patients (U = 350.5; p = 0.01). |
| Khattri, Bist, Arun, and Mehta (2015) | India | Vitiligo | 50 patients with vitiligo and 50 healthy controls,aged between 20 and 70 years old | DSM-IV Axis I Disorders (SCID-I), Hospital Anxiety Depression Scale (HADS), Rosenberg Self-Esteem Scale (RSES), Liebowitz Social Anxiety Scale (LSAS) and Sheehan Disability Scale (SDS) | In comparison to healthy controls, the rate of depression and anxiety was found to be higher and mean self-esteem score was found to be lower in the vitiligo group. There was no significant difference between groups in terms of social anxiety. |
| Egeberg, Hansen, Gislason, and Thyssen (2016) | Denmark | Rosacea | 30.725 and 24.712 patients with mild and moderate-tosevere rosacea > 18 years | Data on 4.632.341 Danish citizens | Mild and moderateto-severe rosacea increased the risk of both depression [IRR 1.89 (95% CI 1.82-1.96) and IRR 2.04 (95% CI 1.96-2.12)] and anxiety disorders [IRR 1.80 (95% CI 1.75-1.86) and IRR 1.98 (95% CI 1.91-2.05)]. |
| Halioua, Cribier, Frey, and Tan (2017) | UK, France, Germany and US | Rosacea | 807 (31.3±14.5 years) | Online survey of the general population over 18 years of age | Those with FS were more likely to avoid social situations (54.2% vs. 2.0%, p < 1.00E−10) and had a higher rate of depression (36.7% vs. 21.1%, p < 1.00E−10). |
| Wojtyna, Łakuta, Marcinkiewicz, Bergler-Czop, and Brzezinska-Wcisło (2017) | Poland | Psoriasis | 219 patients with psoriasis, aged 18-70 years | Beck Depression Inventory, the Appearance Schemas Inventory-Revised, the Berlin Social Support Scales, and the Distress Thermometer | The main contributors to depression were: female gender, beliefs about appearance and its salience to one’s self-worth, greater psychological distress, and lower levels of emotional social support. |
| Vernwal (2017) | India | Vitiligo | 100 vitiligo patients and 100 controls | Hospital Anxiety and Depression Scale | In comparison to healthy controls, the psychiatric morbidity was found to be significantly higher in the vitiligo group (62% v/s 25%). 37%, 18%, and 7% vitiligo patients suffered from Mixed anxiety and depressive disorder, Depressive disorder and Generalized anxiety disorder respectively. |
3.2 Skin disorders and Anger/Aggression
For most of the theories, anger is the typical reaction to both physical and psychological frustration and constriction. The causal relationship between frustration and anger is quite complex. Other factors seem in fact to be involved in the origins of anger emotion as, for example, the responsibility and the awareness attributed to the person or the situation that causes frustration or constriction (Averill, 2012). The emotion of anger can be defined as the reaction that follows a precise sequence of events: a) a state of need; b) an object (living or nonliving) that is opposed to the realization of the need; c) the attribution of intentionality to such object of opposing; d) a lack of fear toward the frustrating object; e) the strong intention to remove and attack the frustrating object; f) an act of aggression implemented through the attack (Boswell, 2016). Therefore, there are different kinds of anger and specifically three: anger directed toward others, self-directed or denied (Livingstone, Shepherd, Spears, & Manstead, 2016).
Table 2 shows the studies related to Anger/Aggression in Skin Disorders. The studies that have found the emotion of anger, in association with skin diseases, is quite low. Only 11 out of 41 studies (29%) addressed this emotion, finding that this is one of the emotions mostly experienced by people with psoriasis and atopic dermatitis, followed by urticaria and erythema, chronic idiopatic urticaria, acne and vitiligo.
Table 2. Characteristics of the researches studying Anger/Aggression in Skin Disorders.
| Author | Country | Skin disorder | Sample | Measure | Results |
|---|---|---|---|---|---|
| Sayar, Ugurad, Kural, and Acar (2000) | Turkey | Acne | 31 acne vulgaris patients and 25 controls | Beck Depression Inventory, State-Trait Anxiety Inventory, Rosenberg Self-Esteem Scale, and Spielberger State-Trait Anger Expression Inventory. | No significant difference was detected on anger-related subscales between the acne and control groups. |
| Conrad et al. (2008) | Germany | Chronic idiopathic urticaria (CIU) and psoriasis | 41 CIU patients 44 psoriasis patients and 49 healthy controls | Alexithymia (TAS-20), emotional distress (SCL-90-R) and anger (STAXI). | Anger was the only significant predictor of pruritus severity in CIU. |
| Linder et al. (2009) | Italy | Psoriasis | 323 patients (aged 18-85 years; mean -SD age 51.2 - 28.7 years) | Interview and a questionnaire developed by clinicians and researchers | Psoriasis elicited anger, annoyance at the inconvenience of the disease, and irritation in approximately 50% of the patients |
| Kossakowska, Ciescinska, Jaszewska, and Placek (2010) | Poland | Vitiligo and Psoriasis | 60 patients with psoriasis (n = 30) and vitiligo (n = 30) as well as healthy persons (n = 60) matched | Watson and Greer’s Courtauld Emotional Control Scale and Kossakowska’s Chronic Patients Questionnaire. | Psoriasis patients control negative emotions more intensively than healthy people. Vitiligo patients do not differ in the control of negative emotions compared with healthy subjects. |
| Sampogna, Tabolli, and Abeni (2012) | Italy | Psoriasias | 936 patients | Skindex-29 questionnaire | The emotions most frequently experienced were: shame, anger, Worry. |
| Takaki and Ishii (2013) | Japan | Atopic Dermatitis (AD) | 43 adult patients with AD, 32 adults with remission from AD, and 63 adults without AD 20-47 years | Anger expression trait scale (AX) | Results indicated a significant impact of anger suppression on depression, in patients with AD. |
| Altınöz, Taskıntuna, Altınöz, and Ceran (2014) | Turkey | Chronic spontaneous urticaria (CSU) and alopecia areata (AA) | 30 CSU 30 AA 30 controls | Hospital Anxiety and Depression Scale and Multi-Dimensional Anger Inventory | More of the CSU patients were observed to respond with excessive anger to most situations, to have high levels of anxiety anger and passive aggressive interpersonal Relationships. |
| Sarkar, Sarkar, Saha, and Sarkar (2014) | India | Psoriasis | Forty-eight patients of psoriasis and equal number of healthy controls | Self-reporting questionnaire-24 (SRQ-24) and skindex (A 61-item survey questionnaire) | the most common psychiatric morbidity in psoriasis patients was anger (58.3%) |
| Altunay and Demirci (2015) | Turkey | Pruritus | 40 patients with a mean age 46.55±13.20 years | State-Trait Anger Expression Index and the Mini International Neuropsychiatric Interview (M.I.N.I) | Pruritus duration was correlated with anger trait and anger-in subscale scores in all patients. |
| Aydin et al. (2017) | Turkey | Psoriasis | Eighty-five patients with psoriasis and 86 healthy controls | State-Trait Expression Inventory for Anger (STAXI) and Roserberg Self-esteem Scale (RSES) | Reduced self-esteem and increased anger levels are remarkable in psoriasis patients. |
| (Coneo, Thompson, & Lavda, 2017) | England | Dermathology patients | ninety-one participant | Optimism (LOT-R), perceptions of social support (SFSSQ) social acceptance, fear of negative Evaluation (FNE), appearance concern (CARVAL/ CARSAL), appearance discrepancy PADQ), social comparison (INCOMM) and wellbeing (HADS) on aggression levels (RAQ) | Anxiety was also found to have a significant positive relationship with aggression (β = 0.356, t = 2.564,p = 0.01). |
In particular, Conrad et al. (2008) measured alexithymia (TAS-20), emotional distress (SCL-90-R). and anger (STAXI) in skin-disordered patients, founding that that chronic idiopathic urticaria (CIU) and psoriasis are associated with personality-based difficulties in emotional regulation, particularly with regard to the feeling of anger. However, it remains unclear if anger is directed toward others, self-directed or denied. The high prevalence of alexithymia seems connected with difficulties in communicating anger and in both skin disorders, the relationship between pruritus as a major symptom of negative affectivity could explain anger towards self and others.
3.3 Skin Disorders and Disgust
Disgust is an emotion characterized by a feeling of nausea, revulsion, especially in respect of odors and flavors, and, figuratively speaking, moral repulsion, intolerance, hate with a strong psychological value. It is manifested by a behavior tending to remove something or someone, and from a physiological reaction, such as nausea and vomiting in response to dirt and contamination sensations (Lateiner & Spatharas, 2016).
Over the years, not many authors have given their contribution to the empirical study of the emotion of disgust, but several studies show that disgust has the function to keep us away from situations or substances which could be dangerous, or from anything that is abhorrent and dirty, including values, thoughts, people, and, in some cases, even the self (Yoder, Widen, & Russell, 2016). Although it can be assumed that disgust plays a key role in the perception of body image and dermatological disease, the studies on this topic are quite low.
Unfortunately, only one study addressed the emotion of disgust in patients with psoriasis. Lahousen et al. (2016), in fact, investigated the differences psoriasis patients and skin-healthy controls concerning appraisal of touching, shame and disgust in one hundred and seventyone patients with psoriasis and 171 skin healthy controls who completed the Touch-Shame-Disgust-Questionnaire (TSD-Q), obtaining that skin-related disgust and shame were significantly higher in psoriasis patients. The study of disgust is one of the most neglected, not only in the field of psychology and psychiatry, but also in its applications in the dermatological context, presenting a significantly low incidence even in the field of psycho-dermatology.
4. Qualitative Analysis
Thanks to VOSviewer has been possible to analyze a text that contained the main information of a paper i.e. the disease and the associated primary emotion studied. On the basis of data collected in the review of the forty-one studies, a list has been formed. Figure 3 shows the bibliographic landscapes of the studies about skin disorders and emotions. The more the colors are close to red, the higher their occurrence and the closer the words, the higher the co-occurrence.
Figure 3. Bibliometric landscape of primary emotions and skin diseases.
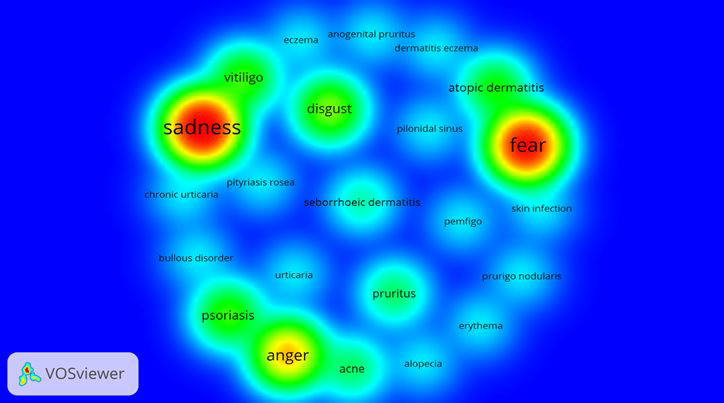
The qualitative analysis provides visual information on: 1) the proximity of vitiligo and sadness/depression; 2) the proximity of fear/anxiety and atopic dermatitis; 3) the proximity of psoriasis and anger; 4) the apparent independence of disgust.
This visual analysis remarks on the findings discussed: literature on emotions and skin diseases has been focused on specific emotions, neglecting others. In particular, the map highlights the imbalance between studies that addressed depression and anxiety and studies that considered anger and/or disgust. In fact, still little is known about the involvement of anger and its role as a predisposing factor and also as a secondary problem towards the dermatological pathology. Furthermore, the emotion of disgust is under-represented: in comparison to other emotions, disgust is the most neglected, despite it is undoubtedly involved. The individual can feel disgust against his/her body (self-disgust) or can believe that the other perceives him/her as disgusting.
5. Discussion
The present review study was aimed to describe in what way negative emotions were investigated in the sphere of dermatological diseases, in order to highlight any possible imbalances between the most studied and the most neglected emotions, to identify a possible association model between the type of dermatological condition and the emotion studied, and to offer cues for future research.
Clinical observation suggested that dermatological patients live an intense emotional activation. From the moment of the received diagnosis they have to face psychological difficulties and have to manage disease acceptance and therapy management. This can raise different reactions in the individual: from depression for the loss of health, to anxiety for symptoms worsening, to anger (why me?), until disgust towards pustule, desquamation, rash, in other terms, against his/her own skin and body. The loss of a healthy and attractive image can severely impair the relationships with the body image and with others. Studies on quality of life, despite interesting and useful, do not cover or explain the aspects more related to the inner emotional experience. To reach this purpose, i.e., to understand how negative emotions are declined among skin disordered patients, a review was necessary as a first step in the comprehension of the psychological functioning.
The present review suggests -despite taking into account that studies are published from one to two years after their actual implementation- an increasing interest, over the last five years, by authors who explored the role of emotions in skin diseases, or more likely their emotional consequences. It is increasingly evident the impact of the psychosomatic medicine, the collaboration between dermatologists, psychiatrists, and psychologists, and the vision of the disorder in the psyche-soma unit (Muscatello, Bruno, Scimeca, Pandolfo, & Zoccali, 2014; Rizzo et al., 2018). However, the interest on negative emotions in skin disorders reveals some contradiction and imbalance. For example, we observed that the exploration of the emotional aspects has been more successful for some diseases such as psoriasis, dermatitis and vitiligo. This may depend on the epidemiology of the disease and thus on the rarity or representativeness of the observations, or from a possible greater interest for the diseases in which the psychological implications are more observable. For example, the incidence of psoriasis in adults varies from 78.9/100,000 person-years in the United States to 230/100,000 person-years in Italy. The occurrence of psoriasis varies also according to age and geographic region, being more frequent in countries more distant from the equator and in the adult age range (Parisi, Symmons, Griffiths, & Ashcroft, 2013) while the worldwide incidence of pemphigus is 0.75-5 cases/1,000,000 per year. Most cases of PV in North America, Europe and Asia are sporadic, with a higher incidence among Ashkenazi Jews, with an estimate of 1.6 per 100,000 populations per year in Jerusalem (Femiano, 2007).
The imbalance of the epidemiology of skin diseases fails to explain the imbalance in the study of primary emotions, which was found rather inhomogeneous.
Most of the studies have shown consistent results. For example, we have found that: a) sadness was studied in terms of depression and, therefore, in its pathological manifestation and not physiological; b) most of the studies addressed the fear in terms of anxiety, or a reaction to a perceived danger; c) many of the studies that have studied depression have found an association with anxiety, as already consolidated in the literature.
While other studies raise some controversial issues. Results show that the emotion of disgust is considered involved in dermatological disorders by different authors, but is not sufficiently represented on the side of empirical exploration. In other words, the authors argue that disgust is undoubtedly associated with, for example, papulosquamous or bullous diseases as a theoretical assumption, but empirical studies on clinical samples and plausibly appropriate tools for measuring the emotion of disgust are almost completely unavailable (Settineri & Mento, 2014).
The study of the emotion of anger, on the other hand, resulted very limited. It becomes difficult to determine whether or not this emotion is involved in skin diseases, as it would suggest the clinical observation. The collected data must take into account a possible bias: when the emotion of anger appears in the studies cited, could be the result of variability due to chance (e.g., an upstream selection of the variable in the research design, a lack of publication of studies that disconfirm the involvement of anger in skin diseases, etc.). For these reasons, future studies on the role of anger and disgust in dermatological diseases would be advantageous.
6. Limitations
Of course, this review has also several limitations. Having included some reviews, it is possible that the number of studies dealing with depression and anxiety has been underestimated. However, this could slightly modify results, since depression and anxiety resulted as the most studied among skin problems.
On the contrary, some of the studies cited also analyzed the relationship between skin disorders and the feelings of shame or guilt. These emotions have been excluded because should need specific space of discussion and scientific deepening. In clinical practice, we observe that the patient is immersed in a mix of different emotions with regard to the dermatological problem, because it has an impact on the self-image and the social and relational sphere. Every dermatological disease has its particular features, some of them affect exposed body areas, such as face or neck, and can generate intense negative emotions not only towards self, but also against other leading to avoidance of exposure, fear of judgement, fear of intimacy, etc.
Besides, due to the disparity between the studies, but also to the heterogeneity of the dermatological disorders treated, it was not possible to conduct a meta-analysis. Unfortunately, statistical conclusions and comparisons are not applicable to this research. Hence, a problem emerges with respect to the comparison of results. This study has not mitigated the effects of measuring negative emotions through different tools, which span from structured interview to self-report scales or questionnaires vs. DSM-IV or ICD-10 diagnostic criteria. This makes the discussion a narrative reflection of a qualitative nature, supported by the visual analysis, as a bibliographic landscape.
Finally, the failure to consult of search engines (e.g., Scopus) most appropriate for this kind of study, may result in the exclusion of manuscripts useful for the development of the revision theme.
7. Conclusion
We believe the most innovative points are two. The first is that, to our knowledge, the present review considers the whole negative emotional spectrum, i.e., not only depression and anxiety, which are the most studied, but also anger and disgust. The second point is the application of an innovative method of bibliographic data analysis software (VOS), resulting in a graphical representation of the studies on the topic. This method allows to create a sort of map, a landscape that immediately suggests to the reader the “state of art”, arising new issues and future research cues.
Dermatology is an interesting research field, a preferential point of observation to understand the somatization mechanisms and the mind-body relationship. The link between emotional reactions and skin responses is the background of the success of techniques such as biofeedback, which allows visualizing the skin reactions to a series of stimuli (Shenefelt, 2010). Since the emotional reaction steps away from the skin (Damasio, 2003), the visualization of one’s emotional reactions can help the individual to recognize the importance of these reactions and to manage them more effectively.
In conclusion, as well as in many other fields of medicine, in which emotions intervene (Settineri, Rizzo, Liotta, & Mento, 2017; Mento, Le Donne, Crisafulli, Rizzo, & Settineri, 2017; Mento et al., 2015), the deepening of the neglected aspects can foster a better understanding of the skin disorder and can be the basis of therapeutic interventions increasingly targeted, such as biofeedback technique and psychotherapy based on emotion regulation and mindfulness based stress reduction.
8. Contributors
R.A. and B.A. conducted literature searches, analysis and wrote the manuscript.
Z.RA. and M.MRA. contributed to and have approved the final manuscript.
M.C. conceived the study and wrote the hypothesis.
9. Compliance with Ethical Standards
Funding. This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Conflict of Interest. The authors declare that there is no financial, general, and institutional conflict of interest regarding the publication of this article.
Ethical approval. This article does not contain any studies with human participants performed by any of the authors.
References
- Abram, K., Silm, H., Maaroos, H., & Oona, M. (2009). Subjective disease perception and symptoms of depression in relation to healthcare-seeking behaviour in patients with rosacea. Acta dermato-venereologica, 89 (5), 488-491. [DOI] [PubMed]; Abram K., Silm H., Maaroos H., Oona M. Subjective disease perception and symptoms of depression in relation to healthcare-seeking behaviour in patients with rosacea. Acta dermato-venereologica. 2009;89(5):488–491. doi: 10.2340/00015555-0716. [DOI] [PubMed] [Google Scholar]
- Ahmed, I., Ahmed, S., & Nasreen, S. (2007). Frequency and pattern of psychiatric disorders in patients with vitiligo. J Ayub Med Coll Abbottabad, 19 (3), 19-21. [PubMed]; Ahmed I., Ahmed S., Nasreen S. Frequency and pattern of psychiatric disorders in patients with vitiligo. J Ayub Med Coll Abbottabad. 2007;19(3):19–21. [PubMed] [Google Scholar]
- Alfani, S., Antinone, V., Mozzetta, A., Pietro, C., Mazzanti, C., Stella, P., & Abeni, D. (2012). Psychological status of patients with alopecia areata. Acta dermato-venereologica, 92 (3), 304-306. [DOI] [PubMed]; Alfani S., Antinone V., Mozzetta A., Pietro C., Mazzanti C., Stella P., Abeni D. Psychological status of patients with alopecia areata. Acta dermato-venereologica. 2012;92(3):304–306. doi: 10.2340/00015555-1239. [DOI] [PubMed] [Google Scholar]
- Al-Harbi, M. (2013). Prevalence of depression in vitiligo patients. Skinmed, 11 (6), 327-330. [PubMed]; Al-Harbi M. Prevalence of depression in vitiligo patients. Skinmed. 2013;11(6):327–330. [PubMed] [Google Scholar]
- Altınöz, A., Taşkıntuna, N., Altınöz, S., & Ceran, S. (2014). A cohort study of the relationship between anger and chronic spontaneous urticaria. Advances in therapy, 31 (9), 1000-1007. [DOI] [PubMed]; Altınöz A., Taşkıntuna N., Altınöz S., Ceran S. A cohort study of the relationship between anger and chronic spontaneous urticaria. Advances in therapy. 2014;31(9):1000–1007. doi: 10.1007/s12325-014-0152-6. [DOI] [PubMed] [Google Scholar]
- Altunay, I., & Demirci, G. (2015). The relationship of functional pruritus with anger and associated psychiatric disorders. Turkderm, 49 (A00101s1), 28-32.; Altunay I., Demirci G. The relationship of functional pruritus with anger and associated psychiatric disorders. Turkderm. 2015;49(A00101s1):28–32. [Google Scholar]
- Arck, P., Handjiski, B., Hagen, E., Pincus, M., Bruenahl, C., Bienenstock, J., & Paus, R. (2010). Is there a ‘gut-brain-skin axis’? Experimental dermatology, 19 (5), 401-405. [DOI] [PubMed]; Arck P., Handjiski B., Hagen E., Pincus M., Bruenahl C., Bienenstock J., Paus R. Is there a ‘gut-brain-skin axis’? Experimental dermatology. 2010;19(5):401–405. doi: 10.1111/j.1600-0625.2009.01060.x. [DOI] [PubMed] [Google Scholar]
- Averill, J. R. (2012). Anger and aggression: An essay on emotion. Springer Science & Business Media.; Averill J. R. Anger and aggression: An essay on emotion. Springer Science & Business Media; 2012. [Google Scholar]
- Aydin, E., Atis, G., Bolu, A., Aydin, C., Karabacak, E., Dogan, B., & Ates, M. (2017). Identification of anger and self-esteem in psoriasis patients in a consultation-liaison psychiatry setting: a case control study. Psychiatry and Clinical Psychopharmacology, 27 (3), 222-226.; Aydin E., Atis G., Bolu A., Aydin C., Karabacak E., Dogan B., Ates M. Identification of anger and self-esteem in psoriasis patients in a consultation-liaison psychiatry setting: a case control study. Psychiatry and Clinical Psychopharmacology. 2017;27(3):222–226. [Google Scholar]
- Boswell, J. (2016). Recognizing anger in clinical research and practice. Clinical Psychology: Science and Practice, 23 (1), 86-89.; Boswell J. Recognizing anger in clinical research and practice. Clinical Psychology: Science and Practice. 2016;23(1) [Google Scholar]
- Buljan, D., Buljan, M., & Situm, M. (2005). Psychodermatology: a brief review for clinicians. Psychiatria Danubina, 17 (1-2), 76-83. [PubMed]; Buljan D., Buljan M., Situm M. Psychodermatology: a brief review for clinicians. Psychiatria Danubina. 2005;17(1-2):76–83. [PubMed] [Google Scholar]
- Chan, M., Chua, T., Goh, B., Aw, C., Thng, T., & Lee, S. (2012). Investigating factors associated with depression of vitiligo patients in Singapore. Journal of clinical nursing, 21 (11-12), 1614-1621. [DOI] [PubMed]; Chan M., Chua T., Goh B., Aw C., Thng T., Lee S. Investigating factors associated with depression of vitiligo patients in Singapore. Journal of clinical nursing. 2012;21(11-12):1614–1621. doi: 10.1111/j.1365-2702.2011.03777.x. [DOI] [PubMed] [Google Scholar]
- Cheng, C., Hsu, J., Huang, K., Bai, Y., Su, T., Li, C., & Chen, M. (2015). Risk of developing major depressive disorder and anxiety disorders among adolescents and adults with atopic dermatitis: A nationwide longitudinal study. Journal of affective disorders, 178, 60-65. [DOI] [PubMed]; Cheng C., Hsu J., Huang K., Bai Y., Su T., Li C., Chen M. Risk of developing major depressive disorder and anxiety disorders among adolescents and adults with atopic dermatitis: A nationwide longitudinal study. Journal of affective disorders. 2015;178:60–65. doi: 10.1016/j.jad.2015.02.025. [DOI] [PubMed] [Google Scholar]
- Coneo, A., Thompson, A., & Lavda, A. (2017). The influence of optimism, social support and anxiety on aggression in a sample of dermatology patients: an analysis of cross-sectional data. British Journal of Dermatology, 176 (5), 1187-1194. [DOI] [PubMed]; Coneo A., Thompson A., Lavda A. The influence of optimism, social support and anxiety on aggression in a sample of dermatology patients: an analysis of cross-sectional data. British Journal of Dermatology. 2017;176(5):1187–1194. doi: 10.1111/bjd.15115. [DOI] [PubMed] [Google Scholar]
- Conrad, R., Geiser, F., Haidl, G., Hutmacher, M., Liedtke, R., & Wermter, F. (2008). Relationship between anger and pruritus perception in patients with chronic idiopathic urticaria and psoriasis. Journal of the European Academy of Dermatology and Venereology, 22 (9), 1062-1069. [DOI] [PubMed]; Conrad R., Geiser F., Haidl G., Hutmacher M., Liedtke R., Wermter F. Relationship between anger and pruritus perception in patients with chronic idiopathic urticaria and psoriasis. Journal of the European Academy of Dermatology and Venereology. 2008;22(9):1062–1069. doi: 10.1111/j.1468-3083.2008.02714.x. [DOI] [PubMed] [Google Scholar]
- Dalgard, F., Gieler, U., Tomas-Aragones, L., Lien, L., Poot, F., Jemec, G., & Evers, A. (2015). The psychological burden of skin diseases: a cross-sectional multicenter study among dermatological out-patients in 13 european countries. Journal of Investigative Dermatology, 135 (4), 984-991. [DOI] [PMC free article] [PubMed]; Dalgard F., Gieler U., Tomas-Aragones L., Lien L., Poot F., Jemec G., Evers A. The psychological burden of skin diseases: a cross-sectional multicenter study among dermatological out-patients in 13 european countries. Journal of Investigative Dermatology. 2015;135(4):984–991. doi: 10.1038/jid.2014.530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Damasio, A. (2003). Feelings of emotion and the self. Annals of the New York Academy of Sciences, 1001 (1), 253-261. [DOI] [PubMed]; Damasio A. Feelings of emotion and the self. Annals of the New York Academy of Sciences. 2003;1001(1):253–261. doi: 10.1196/annals.1279.014. [DOI] [PubMed] [Google Scholar]
- Devrimci-Ozguven, H., Kundakci, N., Kumbasar, H., & Boyvat, A. (2000). The depression, anxiety, life satisfaction and affective expression levels in psoriasis patients. Journal of the European Academy of dermatology and venereology, 14 (4), 267-271. [DOI] [PubMed]; Devrimci-Ozguven H., Kundakci N., Kumbasar H., Boyvat A. The depression, anxiety, life satisfaction and affective expression levels in psoriasis patients. Journal of the European Academy of dermatology and venereology. 2000;14(4):267–271. doi: 10.1046/j.1468-3083.2000.00085.x. [DOI] [PubMed] [Google Scholar]
- Dhabhar, F. (2000). Acute stress enhances while chronic stress suppresses skin immunity: the role of stress hormones and leukocyte trafficking. Annals of the New York Academy of Sciences, 917 (1), 876-893. [DOI] [PubMed]; Dhabhar F. Acute stress enhances while chronic stress suppresses skin immunity: the role of stress hormones and leukocyte trafficking. Annals of the New York Academy of Sciences. 2000;917(1):876–893. doi: 10.1111/j.1749-6632.2000.tb05454.x. [DOI] [PubMed] [Google Scholar]
- Dieris-Hirche, J., Gieler, U., Kupfer, J., & Milch, W. (2009). Suicidal ideation, anxiety and depression in adult patients with atopic dermatitis. Der Hautarzt; Zeitschrift fur Dermatologie, Venerologie, und verwandte Gebiete, 60 (8), 641-646. [DOI] [PubMed]; Dieris-Hirche J., Gieler U., Kupfer J., Milch W. Suicidal ideation, anxiety and depression in adult patients with atopic dermatitis. Der Hautarzt; Zeitschrift fur Dermatologie, Venerologie, und verwandte Gebiete. 2009;60(8):641–646. doi: 10.1007/s00105-009-1744-y. [DOI] [PubMed] [Google Scholar]
- Duman, K., Ozdemir, Y., Yucel, E., & Akin, M. (2014). Comparison of depression, anxiety and long-term quality of health in patients with a history of either primary closure or limberg flap reconstruction for pilonidal sinus. Clinics, 69 (6), 384-387. [DOI] [PMC free article] [PubMed]; Duman K., Ozdemir Y., Yucel E., Akin M. Comparison of depression, anxiety and long-term quality of health in patients with a history of either primary closure or limberg flap reconstruction for pilonidal sinus. Clinics. 2014;69(6):384–387. doi: 10.6061/clinics/2014(06)03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Egeberg, A., Hansen, P., Gislason, G., & Thyssen, J. (2016). Patients with rosacea have increased risk of depression and anxiety disorders: a Danish nationwide cohort study. Dermatology, 232 (2), 208-213. [DOI] [PubMed]; Egeberg A., Hansen P., Gislason G., Thyssen J. Patients with rosacea have increased risk of depression and anxiety disorders: a Danish nationwide cohort study. Dermatology. 2016;232(2):208–213. doi: 10.1159/000444082. [DOI] [PubMed] [Google Scholar]
- Ehsani, A., Toosi, S., Shahshahani, M., Arbabi, M., & Noormohammadpour, P. (2009). Psycho-cutaneous disorders: an epidemiologic study. Journal of the European Academy of Dermatology and Venereology, 23 (8), 945-947. [DOI] [PubMed]; Ehsani A., Toosi S., Shahshahani M., Arbabi M., Noormohammadpour P. Psycho-cutaneous disorders: an epidemiologic study. Journal of the European Academy of Dermatology and Venereology. 2009;23(8):945–947. doi: 10.1111/j.1468-3083.2009.03236.x. [DOI] [PubMed] [Google Scholar]
- Eming, S., Krieg, T., & Davidson, J. (2007). Inflammation in wound repair: molecular and cellular mechanisms. Journal of Investigative Dermatology, 127 (3), 514-525. [DOI] [PubMed]; Eming S., Krieg T., Davidson J. Inflammation in wound repair: molecular and cellular mechanisms. Journal of Investigative Dermatology. 2007;127(3):514–525. doi: 10.1038/sj.jid.5700701. [DOI] [PubMed] [Google Scholar]
- Engin, B., Uguz, F., Yilmaz, E., Özdemir, M., & Mevlitoglu, I. (2008). The levels of depression, anxiety and quality of life in patients with chronic idiopathic urticaria. Journal of the European Academy of Dermatology and Venereology, 22 (1), 36-40. [DOI] [PubMed]; Engin B., Uguz F., Yilmaz E., Özdemir M., Mevlitoglu I. The levels of depression, anxiety and quality of life in patients with chronic idiopathic urticaria. Journal of the European Academy of Dermatology and Venereology. 2008;22(1):36–40. doi: 10.1111/j.1468-3083.2007.02324.x. [DOI] [PubMed] [Google Scholar]
- Esposito, M., Saraceno, R., Giunta, A., Maccarone, M., & Chimenti, S. (2006). An italian study on psoriasis and depression. Dermatology, 212 (2), 123-127. [DOI] [PubMed]; Esposito M., Saraceno R., Giunta A., Maccarone M., Chimenti S. An italian study on psoriasis and depression. Dermatology. 2006;212(2):123–127. doi: 10.1159/000090652. [DOI] [PubMed] [Google Scholar]
- Femiano, F. (2007). Pemphigus vulgaris: recent advances in our understanding of its pathogenesis. Minerva stomatologica, 56 (4), 215-223. [PubMed]; Femiano F. Pemphigus vulgaris: recent advances in our understanding of its pathogenesis. Minerva stomatologica. 2007;56(4):215–223. [PubMed] [Google Scholar]
- Fritzsche, K., Ott, J., Zschocke, I., Scheib, P., Burger, T., & Augustin, M. (2001). Psychosomatic liaison service in dermatology. Dermatology, 203 (1), 27-31. [DOI] [PubMed]; Fritzsche K., Ott J., Zschocke I., Scheib P., Burger T., Augustin M. Psychosomatic liaison service in dermatology. Dermatology. 2001;203(1):27–31. doi: 10.1159/000051699. [DOI] [PubMed] [Google Scholar]
- Ghajarzadeh, M., Ghiasi, M., & Kheirkhah, S. (2012). Associations between skin diseases and quality of life: a comparison of psoriasis, vitiligo, and alopecia areata. Acta Medica Iranica, 50 (7), 511. [PubMed]; Ghajarzadeh M., Ghiasi M., Kheirkhah S. Associations between skin diseases and quality of life: a comparison of psoriasis, vitiligo, and alopecia areata. Acta Medica Iranica. 2012;50(7):511–511. [PubMed] [Google Scholar]
- Gieler, U., Niemeier, V., Kupfer, J., Brosig, B., & Schill, W. (2001). Psychosomatic dermatology in germany: a survey of 69 dermatologic clinics. Der Hautarzt; Zeitschrift fur Dermatologie, Venerologie, und verwandte Gebiete, 52 (2), 104-110. [DOI] [PubMed]; Gieler U., Niemeier V., Kupfer J., Brosig B., Schill W. Psychosomatic dermatology in germany: a survey of 69 dermatologic clinics. Der Hautarzt; Zeitschrift fur Dermatologie, Venerologie, und verwandte Gebiete. 2001;52(2):104–110. doi: 10.1007/s001050051273. [DOI] [PubMed] [Google Scholar]
- Gupta, M., & Gupta, A. (2001). The use of antidepressant drugs in dermatology. Journal of the European Academy of Dermatology and Venereology, 15 (6), 512-518. [DOI] [PubMed]; Gupta M., Gupta A. The use of antidepressant drugs in dermatology. Journal of the European Academy of Dermatology and Venereology. 2001;15(6):512–518. doi: 10.1046/j.1468-3083.2001.00278.x. [DOI] [PubMed] [Google Scholar]
- Halioua, B., Cribier, B., Frey, M., & Tan, J. (2017). Feelings of stigmatization in patients with rosacea. Journal of the European Academy of Dermatology and Venereology, 31 (1), 163-168. [DOI] [PubMed]; Halioua B., Cribier B., Frey M., Tan J. Feelings of stigmatization in patients with rosacea. Journal of the European Academy of Dermatology and Venereology. 2017;31(1):163–168. doi: 10.1111/jdv.13748. [DOI] [PubMed] [Google Scholar]
- Khattri, S., Bist, J., Arun, A., & Mehta, A. (2015). Clinical correlates of vitiligo with depression and anxiety: A comparative study in patients and their caregivers. International Journal, 3 (1), 200-205.; Khattri S., Bist J., Arun A., Mehta A. Clinical correlates of vitiligo with depression and anxiety: A comparative study in patients and their caregivers. International Journal. 2015;3(1):200–205. [Google Scholar]
- Kim, S., Hur, J., Jang, J., Park, H., Hong, C., Son, S., & Chang, K. (2015). Psychological Distress in Young Adult Males with Atopic Dermatitis: A Cross-Sectional Study. Medicine, 94 (23). [DOI] [PMC free article] [PubMed]; Kim S., Hur J., Jang J., Park H., Hong C., Son S., Chang K. Psychological Distress in Young Adult Males with Atopic Dermatitis: A Cross-Sectional Study. Medicine. 2015;94(23) doi: 10.1097/MD.0000000000000949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Konda, D., Chandrashekar, L., Rajappa, M., Kattimani, S., Thappa, D., & Ananthanarayanan, P. (2015). Serotonin and interleukin-6: Association with pruritus severity, sleep quality and depression severity in prurigo nodularis. Asian journal of psychiatry, 17, 24-28. [DOI] [PubMed]; Konda D., Chandrashekar L., Rajappa M., Kattimani S., Thappa D., Ananthanarayanan P. Serotonin and interleukin-6: Association with pruritus severity, sleep quality and depression severity in prurigo nodularis. Asian journal of psychiatry. 2015;17:24–28. doi: 10.1016/j.ajp.2015.07.010. [DOI] [PubMed] [Google Scholar]
- Kossakowska, M., Cieścińska, C., Jaszewska, J., & Placek, W. (2010). Control of negative emotions and its implication for illness perception among psoriasis and vitiligo patients. Journal of the European Academy of Dermatology and Venereology, 24 (4), 429-433. [DOI] [PubMed]; Kossakowska M., Cieścińska C., Jaszewska J., Placek W. Control of negative emotions and its implication for illness perception among psoriasis and vitiligo patients. Journal of the European Academy of Dermatology and Venereology. 2010;24(4):429–433. doi: 10.1111/j.1468-3083.2009.03432.x. [DOI] [PubMed] [Google Scholar]
- Krooks, J., Weatherall, A., & Holland, P. (2017). Review of epidemiology, clinical presentation, diagnosis, and treatment of common primary psychiatric causes of cutaneous disease. Journal of Dermatological Treatment , ( just-accepted), 1-45. [DOI] [PubMed]; Krooks J., Weatherall A., Holland P. Review of epidemiology, clinical presentation, diagnosis, and treatment of common primary psychiatric causes of cutaneous disease. Journal of Dermatological Treatment. 2017;(just-accepted):1–45. doi: 10.1080/09546634.2017.1395389. [DOI] [PubMed] [Google Scholar]
- Lahousen, T., Kupfer, J., Gieler, U., Hofer, A., Linder, M., & Schut, C. (2016). Differences Between Psoriasis Patients and Skin-healthy Controls Concerning Appraisal of Touching, Shame and Disgust. Acta dermato-venereologica, 96 (217), 78-82. [DOI] [PubMed]; Lahousen T., Kupfer J., Gieler U., Hofer A., Linder M., Schut C. Differences Between Psoriasis Patients and Skin-healthy Controls Concerning Appraisal of Touching, Shame and Disgust. Acta dermato-venereologica. 2016;96(217):78–82. doi: 10.2340/00015555-2373. [DOI] [PubMed] [Google Scholar]
- Lateiner, D., & Spatharas, D. (2016). The ancient emotion of disgust. Oxford University Press.; Lateiner D., Spatharas D. The ancient emotion of disgust. Oxford University Press; 2016. [Google Scholar]
- Layegh, P., Arshadi, H., Shahriari, S., Pezeshkpour, F., & Nahidi, Y. (2010). A comparative study on the prevalence of depression and suicidal ideation in dermatology patients suffering from psoriasis, Acne, Alopecia areata and Vitiligo. Iranian Journal of Dermatology, 13 (4), 106-111.; Layegh P., Arshadi H., Shahriari S., Pezeshkpour F., Nahidi Y. A comparative study on the prevalence of depression and suicidal ideation in dermatology patients suffering from psoriasis, Acne, Alopecia areata and Vitiligo. Iranian Journal of Dermatology. 2010;13(4):106–111. [Google Scholar]
- Lewis, M., Haviland-Jones, J., & Barrett, L. E. (2010). Handbook of emotions. Guilford Press.; Lewis M., Haviland-Jones J., Barrett L. E. Handbook of emotions. Guilford Press; 2010. [Google Scholar]
- Linder, D., Dall’Olio, E., Gisondi, P., Berardesca, E., De Gennaro, E., Pennella, A., & Girolomoni, G. (2009). Perception of disease and doctor-patient relationship experienced by patients with psoriasis. American journal of clinical dermatology, 10 (5), 325-330. [DOI] [PubMed]; Linder D., Dall’Olio E., Gisondi P., Berardesca E., De Gennaro E., Pennella A., Girolomoni G. Perception of disease and doctor-patient relationship experienced by patients with psoriasis. American journal of clinical dermatology. 2009;10(5):325–330. doi: 10.2165/11311190-000000000-00000. [DOI] [PubMed] [Google Scholar]
- Livingstone, A. G., Shepherd, L., Spears, R., & Manstead, A. S. (2016). “fury, us”: Anger as a basis for new group self-categories. Cognition and Emotion, 30 (1), 183-192. [DOI] [PubMed]; Livingstone A. G., Shepherd L., Spears R., Manstead A. S. “fury, us”: Anger as a basis for new group self-categories. Cognition and Emotion. 2016;30(1):183–192. doi: 10.1080/02699931.2015.1023702. [DOI] [PubMed] [Google Scholar]
- Marshall, C., Taylor, R., & Bewley, A. (2016). Psychodermatology in Clinical Practice: Main Principles. Acta dermato-venereologica, 96 (217), 30-34. [DOI] [PubMed]; Marshall C., Taylor R., Bewley A. Psychodermatology in Clinical Practice: Main Principles. Acta dermato-venereologica. 2016;96(217):30–34. doi: 10.2340/00015555-2370. [DOI] [PubMed] [Google Scholar]
- Mattoo, S., Handa, S., Kaur, I., Gupta, N., & Malhotra, R. (2001). Psychiatric morbidity in vitiligo and psoriasis: a comparative study from india. The Journal of dermatology, 28 (8), 424-432. [DOI] [PubMed]; Mattoo S., Handa S., Kaur I., Gupta N., Malhotra R. Psychiatric morbidity in vitiligo and psoriasis: a comparative study from india. The Journal of dermatology. 2001;28(8):424–432. doi: 10.1111/j.1346-8138.2001.tb00004.x. [DOI] [PubMed] [Google Scholar]
- Mento, C., Le Donne, M., Crisafulli, S., Rizzo, A., & Settineri, S. (2017). Bmi at early puerperium: body image, eating attitudes and mood states. Journal of Obstetrics and Gynaecology, 37 (4), 428-434. [DOI] [PubMed]; Mento C., Le Donne M., Crisafulli S., Rizzo A., Settineri S. Bmi at early puerperium: body image, eating attitudes and mood states. Journal of Obstetrics and Gynaecology. 2017;37(4):428–434. doi: 10.1080/01443615.2016.1250727. [DOI] [PubMed] [Google Scholar]
- Mento, C., Piraino, B., Rizzo, A., Vento, R., Rigoli, L., Moschella, E., & Settineri, S. (2015). Affective control and life satisfaction in thalassemics. International Journal of Psychological Research, 8 (1), 90-97.; Mento C., Piraino B., Rizzo A., Vento R., Rigoli L., Moschella E., Settineri S. Affective control and life satisfaction in thalassemics. International Journal of Psychological Research. 2015;8(1):90–97. [Google Scholar]
- Muscatello, M., Bruno, A., Scimeca, G., Pandolfo, G., & Zoccali, R. (2014). Role of negative affects in pathophysiology and clinical expression of irritable bowel syndrome. World Journal of Gastroenterology: WJG, 20 (24), 7570. [DOI] [PMC free article] [PubMed]; Muscatello M., Bruno A., Scimeca G., Pandolfo G., Zoccali R. Role of negative affects in pathophysiology and clinical expression of irritable bowel syndrome. World Journal of Gastroenterology: WJG. 2014;20(24):7570–7570. doi: 10.3748/wjg.v20.i24.7570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parisi, R., Symmons, D., Griffiths, C., & Ashcroft, D. (2013). Global epidemiology of psoriasis: a systematic review of incidence and prevalence. Journal of Investigative Dermatology, 133 (2), 377-385. [DOI] [PubMed]; Parisi R., Symmons D., Griffiths C., Ashcroft D. Global epidemiology of psoriasis: a systematic review of incidence and prevalence. Journal of Investigative Dermatology. 2013;133(2):377–385. doi: 10.1038/jid.2012.339. [DOI] [PubMed] [Google Scholar]
- Paus, R., Theoharides, T., & Arck, P. (2006). Neuroimmunoendocrine circuitry of the ‘brain-skin connection’. Trends in immunology, 27 (1), 32-39. [DOI] [PubMed]; Paus R., Theoharides T., Arck P. Neuroimmunoendocrine circuitry of the ‘brain-skin connection’. Trends in immunology. 2006;27(1):32–39. doi: 10.1016/j.it.2005.10.002. [DOI] [PubMed] [Google Scholar]
- Pavlovic, S., Daniltchenko, M., Tobin, D., Hagen, E., Hunt, S., Klapp, B., & Peters, E. (2008). Further exploring the brain-skin connection: stress worsens dermatitis via substance P-dependent neurogenic inflammation in mice. Journal of Investigative Dermatology, 128 (2), 434-446. [DOI] [PubMed]; Pavlovic S., Daniltchenko M., Tobin D., Hagen E., Hunt S., Klapp B., Peters E. Further exploring the brain-skin connection: stress worsens dermatitis via substance P-dependent neurogenic inflammation in mice. Journal of Investigative Dermatology. 2008;128(2):434–446. doi: 10.1038/sj.jid.5701079. [DOI] [PubMed] [Google Scholar]
- Perusini, J., & Fanselow, M. (2015). Neurobehavioral perspectives on the distinction between fear and anxiety. Learning & Memory, 22 (9), 417-425. [DOI] [PMC free article] [PubMed]; Perusini J., Fanselow M. Neurobehavioral perspectives on the distinction between fear and anxiety. Learning & Memory. 2015;22(9):417–425. doi: 10.1101/lm.039180.115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Picardi, A., Abeni, D., Melchi, C., Puddu, P., & Pasquini, P. (2000). Psychiatric morbidity in dermatological outpatients: an issue to be recognized. British Journal of dermatology, 143 (5), 983-991. [DOI] [PubMed]; Picardi A., Abeni D., Melchi C., Puddu P., Pasquini P. Psychiatric morbidity in dermatological outpatients: an issue to be recognized. British Journal of dermatology. 2000;143(5):983–991. doi: 10.1046/j.1365-2133.2000.03831.x. [DOI] [PubMed] [Google Scholar]
- Pärna, E., Aluoja, A., & Kingo, K. (2015). Quality of life and emotional state in chronic skin disease. Acta Derm Venereol, 95, 312-316. [DOI] [PubMed]; Pärna E., Aluoja A., Kingo K. Quality of life and emotional state in chronic skin disease. Acta Derm Venereol. 2015;95:312–316. doi: 10.2340/00015555-1920. [DOI] [PubMed] [Google Scholar]
- Rashid, M., Mullick, M., Jaigirdar, M., Ali, R., Nirola, D., Salam, M., & Ahsan, M. (2011). Psychiatric Morbidity in Psoriasis and Vitiligo in Two Tertiary Hospitals in Bangladesh. Bangabandhu Sheikh Mujib Medical University Journal, 4 (2), 88-93.; Rashid M., Mullick M., Jaigirdar M., Ali R., Nirola D., Salam M., Ahsan M. Psychiatric Morbidity in Psoriasis and Vitiligo in Two Tertiary Hospitals in Bangladesh. Bangabandhu Sheikh Mujib Medical University Journal. 2011;4(2):88–93. [Google Scholar]
- Rizzo, A., Muscatello, M., Autunno, M., Borgese, C., Pandolfo, G., Zoccali, R., & Bruno, A. (2018). Negative emotions in headache patients. Recenti progressi in medicina, 109 (7), 393-397. [DOI] [PubMed]; Rizzo A., Muscatello M., Autunno M., Borgese C., Pandolfo G., Zoccali R., Bruno A. Negative emotions in headache patients. Recenti progressi in medicina. 2018;109(7):393–397. doi: 10.1701/2955.29709. [DOI] [PubMed] [Google Scholar]
- Sampogna, F., Tabolli, S., & Abeni, D. (2012). Living with psoriasis: prevalence of shame, anger, worry, and problems in daily activities and social life. Acta dermato-venereologica, 92 (3), 299-303. [DOI] [PubMed]; Sampogna F., Tabolli S., Abeni D. Living with psoriasis: prevalence of shame, anger, worry, and problems in daily activities and social life. Acta dermato-venereologica. 2012;92(3):299–303. doi: 10.2340/00015555-1273. [DOI] [PubMed] [Google Scholar]
- Sarkar, S., Sarkar, A., Saha, R., & Sarkar, T. (2014). Psoriasis and psychiatric morbidity: a profile from a tertiary care centre of Eastern India. Journal of family medicine and primary care, 3 (1), 29. [DOI] [PMC free article] [PubMed]; Sarkar S., Sarkar A., Saha R., Sarkar T. Psoriasis and psychiatric morbidity: a profile from a tertiary care centre of Eastern India. Journal of family medicine and primary care. 2014;3(1):29–29. doi: 10.4103/2249-4863.130267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sayar, K., Ugurad, I., Kural, Y., & Acar, B. (2000). The psychometric assessment of acne vulgaris patients. Dermatology and Psychosomatics/Dermatologie und Psychosomatik, 1 (2), 62-65.; Sayar K., Ugurad I., Kural Y., Acar B. The psychometric assessment of acne vulgaris patients. Dermatology and Psychosomatics/Dermatologie und Psychosomatik. 2000;1(2):62–65. [Google Scholar]
- Sellami, R., Masmoudi, J., Ouali, U., Mnif, L., Amouri, M., Turki, H., & Jaoua, A. (2014). The relationship between alopecia areata and alexithymia, anxiety and depression: a case-control study. Indian journal of dermatology, 59 (4), 421. [DOI] [PMC free article] [PubMed]; Sellami R., Masmoudi J., Ouali U., Mnif L., Amouri M., Turki H., Jaoua A. The relationship between alopecia areata and alexithymia, anxiety and depression: a case-control study. Indian journal of dermatology. 2014;59(4):421–421. doi: 10.4103/0019-5154.135525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Settineri, S., Guarneri, F., Saitta, A., Mento, C., & Cannavò, S. (2013). Depression profiles in skin disorders. Open Journal of Psychiatry, 3 (1).; Settineri S., Guarneri F., Saitta A., Mento C., Cannavò S. Depression profiles in skin disorders. Open Journal of Psychiatry. 2013;3(1) [Google Scholar]
- Settineri, S., & Mento, C. (2014). Questionnaire of Disgust. Mediterranean Journal of Clinical Psychology, 2 (1).; Settineri S., Mento C. Questionnaire of Disgust. Mediterranean Journal of Clinical Psychology. 2014;2(1) [Google Scholar]
- Settineri, S., Rizzo, A., Liotta, M., & Mento, C. (2017). Clinical Psychology of Oral Health: The Link Between Teeth and Emotions. SAGE Open, 7 (3), 2158244017728319.; Settineri S., Rizzo A., Liotta M., Mento C. Clinical Psychology of Oral Health: The Link Between Teeth and Emotions. SAGE Open. 2017;7(3):2158244017728319–2158244017728319. [Google Scholar]
- Sharma, N., Koranne, R., & Singh, R. (2001). Psychiatric morbidity in psoriasis and vitiligo: a comparative study. The Journal of dermatology, 28 (8), 419-423. [DOI] [PubMed]; Sharma N., Koranne R., Singh R. Psychiatric morbidity in psoriasis and vitiligo: a comparative study. The Journal of dermatology. 2001;28(8):419–423. doi: 10.1111/j.1346-8138.2001.tb00003.x. [DOI] [PubMed] [Google Scholar]
- Shenefelt, P. (2010). Psychological interventions in the management of common skin conditions. Psychology research and behavior management, 3 (51). [DOI] [PMC free article] [PubMed]; Shenefelt P. Psychological interventions in the management of common skin conditions. Psychology research and behavior management. 2010;3(51) doi: 10.2147/prbm.s7072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tabolli, S., Mozzetta, A., Antinone, V., Alfani, S., Cianchini, G., & Abeni, D. (2008). The health impact of pemphigus vulgaris and pemphigus foliaceus assessed using the Medical Outcomes Study 36-item short form health survey questionnaire. British Journal of Dermatology, 158 (5), 1029-1034. [DOI] [PubMed]; Tabolli S., Mozzetta A., Antinone V., Alfani S., Cianchini G., Abeni D. The health impact of pemphigus vulgaris and pemphigus foliaceus assessed using the Medical Outcomes Study 36-item short form health survey questionnaire. British Journal of Dermatology. 2008;158(5):1029–1034. doi: 10.1111/j.1365-2133.2008.08481.x. [DOI] [PubMed] [Google Scholar]
- Takaki, H., & Ishii, Y. (2013). Sense of coherence, depression, and anger among adults with atopic dermatitis. Psychology, health & medicine, 18 (6), 725-734. [DOI] [PubMed]; Takaki H., Ishii Y. Sense of coherence, depression, and anger among adults with atopic dermatitis. Psychology, health & medicine. 2013;18(6):725–734. doi: 10.1080/13548506.2013.766353. [DOI] [PubMed] [Google Scholar]
- Tareen, R., & Tareen, A. (2015). Dermatology practice and psychiatric disorders. Journal of Alternative Medicine Research, 7 (1), 47.; Tareen R., Tareen A. Dermatology practice and psychiatric disorders. Journal of Alternative Medicine Research. 2015;7(1):47–47. [Google Scholar]
- Uhlenhake, E., Yentzer, B., & Feldman, S. (2010). Acne vulgaris and depression: a retrospective examination. Journal of cosmetic dermatology, 9 (1), 59-63. [DOI] [PubMed]; Uhlenhake E., Yentzer B., Feldman S. Acne vulgaris and depression: a retrospective examination. Journal of cosmetic dermatology. 2010;9(1):59–63. doi: 10.1111/j.1473-2165.2010.00478.x. [DOI] [PubMed] [Google Scholar]
- Van Eck, N., & Waltman, L. (2014). Visualizing bibliometric networks. In Y. Ding, R. Rousseau, & D. Wolfram (Eds.), Measuring Scholarly Impact: Methods and practice. New York, NY: Springer International Publishing, pp. 285-320.; Van Eck N., Waltman L. Visualizing bibliometric networks. In: Ding Y, Rousseau R, Wolfram D, editors. Measuring Scholarly Impact: Methods and practice. New York, NY: Springer International Publishing; 2014. pp. 285–320. [Google Scholar]
- Vernwal, D. (2017). A study of anxiety and depression in Vitiligo patients: New challenges to treat. European Psychiatry, 41, S321.; Vernwal D. A study of anxiety and depression in Vitiligo patients: New challenges to treat. European Psychiatry. 2017;41:S321–S321. [Google Scholar]
- Wakefield, J., & Demazeux, S. (2016). Sadness or Depression? International Perspectives on the Depression Epidemic and Its Meaning. Springer.; Wakefield J., Demazeux S. Sadness or Depression? International Perspectives on the Depression Epidemic and Its Meaning. Springer; 2016. [Google Scholar]
- Wojtyna, E., Łakuta, P., Marcinkiewicz, K., Bergler-Czop, B., & Brzezińska-Wcisło, L. (2017). Gender, body image and social support: Biopsychosocial determinants of depression among patients with psoriasis. Acta dermato-venereologica, 97 (1), 91-97. [DOI] [PubMed]; Wojtyna E., Łakuta P., Marcinkiewicz K., Bergler-Czop B., Brzezińska-Wcisło L. Gender, body image and social support: Biopsychosocial determinants of depression among patients with psoriasis. Acta dermato-venereologica. 2017;97(1):91–97. doi: 10.2340/00015555-2483. [DOI] [PubMed] [Google Scholar]
- Yadav, S., Narang, T., & Kumaran, M. (2013). Psychodermatology: A comprehensive review. Indian Journal of Dermatology, Venereology, and Leprology, 79 (2), 176. [DOI] [PubMed]; Yadav S., Narang T., Kumaran M. Psychodermatology: A comprehensive review. Indian Journal of Dermatology, Venereology, and Leprology. 2013;79(2):176–176. doi: 10.4103/0378-6323.107632. [DOI] [PubMed] [Google Scholar]
- Yamasaki, K., & Gallo, R. (2009). The molecular pathology of rosacea. Journal of dermatological science, 55 (2), 77-81. [DOI] [PMC free article] [PubMed]; Yamasaki K., Gallo R. The molecular pathology of rosacea. Journal of dermatological science. 2009;55(2):77–81. doi: 10.1016/j.jdermsci.2009.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yoder, A., Widen, S., & Russell, J. (2016). The word disgust may refer to more than one emotion. Emotion, 16 (3), 301. [DOI] [PubMed]; Yoder A., Widen S., Russell J. The word disgust may refer to more than one emotion. Emotion. 2016;16(3):301–301. doi: 10.1037/emo0000118. [DOI] [PubMed] [Google Scholar]