Abstract
At the height of the COVID-19 crisis in the Netherlands a shortness of intensive care beds was looming. Dutch professional medical organizations asked a group of ethicists for assistance in drafting guidelines and criteria for selection of patients for intensive care (IC) treatment in case of absolute scarcity, when medical selection criteria would no longer suffice. This article describes the Dutch context, the process of drafting the advice and reflects on the role of ethicists and lessons learned. We argue that timely interaction between clinical and ethical expertise is necessary since the distinction between medical and non-medical considerations is not as clearcut as sometimes assumed. Furthermore, pragmatic considerations related to the specifics of an epidemic are of importance, for example, in relation to prioritizing health care workers. As a consequence, any protocol already present before the pandemic would need alterations to fit the current situation. The ‘fair innings’ criterion we proposed, rephrased as an argument of intergenerational solidarity, was considered reasonable by professionals as well as patient organizations. While it is desirable to draft ethical guidelines in ‘peacetime’ as a matter of pandemic preparedness, the pressure of an actual crisis facilitates decision-making, although it will also complicate a more democratic approach.
Introduction
The COVID-19 epidemic reached the Netherlands in the beginning of March 2020. Notwithstanding initial social distancing measures, the number of COVID-19 patients increased steadily, and within weeks hospitals in certain regions were overwhelmed. A quickly established national coordination structure to relocate and distribute patients could not prevent that shortness of intensive care units (ICUs) was looming. It was hoped that a quick expansion (as far as reasonably possible) of critical care capacity and more strict patient selection based on medical criteria would be sufficient to deal with the increased demand. Yet, how to deal with a situation where physicians would find themselves unable to treat all patients who required intensive care to survive?
In the Netherlands, as in other countries, no ready-to-use protocols were available at the start of the outbreak (Antommaria et al., 2020). The Dutch Association of Medical Specialists (FMS) felt they needed help to come up with fair guidelines for this non-medical triage. They asked the Royal Dutch Medical Association (KNMG) for assistance, and the KNMG invited five ethicists—the authors of this article—to help draft such guidelines. Four of us also have a medical background (MS and SvdV majored in medicine, DW has been a general practitioner and MdV is a pediatrician); the fifth (MV) is well versed in public health.
In this article, we describe the Dutch context, the process of drafting the advice and the final result. We focus on some controversies, notably our own role during the process and indicate some lessons learned.
The Dutch Context
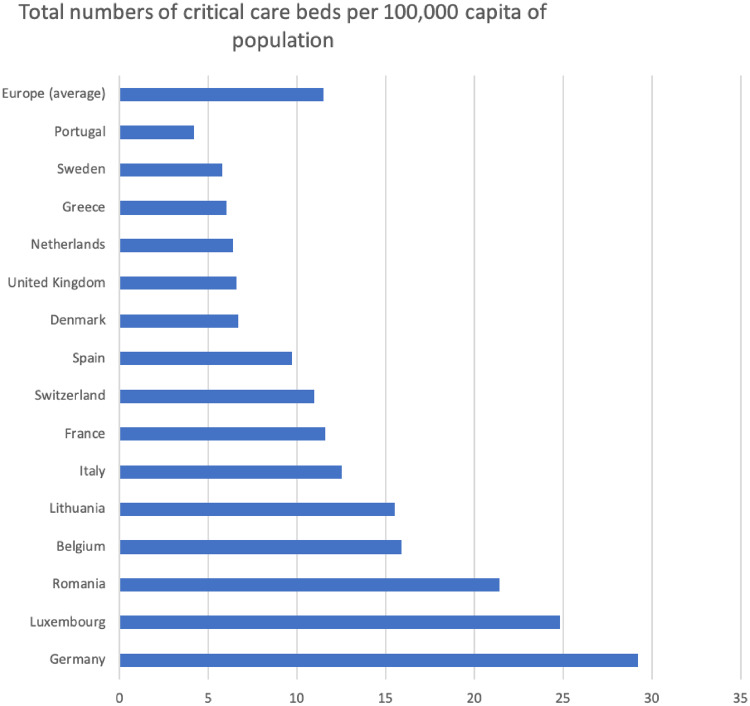
Even though official numbers of ICU capacity need to be treated with caution because not every country uses the same definitions, it is clear that the Netherlands have a low capacity compared to other European countries: 6.4 beds per 100,000 inhabitants. As shown in Figure 1, the average number in European countries is 11.5 beds; Germany has around 30, Luxemburg 25, Belgium approximately 15 and France 11.5 (Rhodes et al., 2012).
Figure 1.
Numbers of critical care beds corrected for size of population (per 100,000 inhabitants) for European countries (Rhodes et al., 2012).
In normal circumstances this low number appears sufficient and ICU scarcity in the Netherlands is rare. The Dutch health care system has a relatively strong focus on efficiency, and maintaining a high surplus capacity in intensive care departments involves major investments that could also be used in other health care domains. Moreover, it might be that Dutch physicians are more reluctant than their colleagues in other countries to send patients to intensive care. Dutch doctors see ICU treatment as an invasive and sometimes harmful treatment that imposes severe burdens on patients—also in the long run—that should only be offered to patients who have a reasonable prospect to benefit (Fogteloo, 2020). Moreover, death on ICU is not seen as a good death, but as something that should be avoided, and this may also play a role in discussions with patient and family when further treatment options are considered (Abarshi et al., 2009). Costs are not an issue for individual treatment decisions; in the Netherlands medically necessary care is covered by the (obligatory) health insurance for all inhabitants.
Soon after the start of the COVID-19 epidemic it became clear that the Dutch capacity would not be sufficient to treat all patients who would be needing an ICU bed.
A centralized system was set up to distribute patients over hospitals in the country, so that regions with a low incidence would share the burdens of more affected regions. Furthermore, hospitals succeeded in doubling the ICU capacity within a few weeks, shifting much capacity and resources from regular care to intensive care. This resulted in a capacity of 13 ICU beds per 100,000 inhabitants—a major achievement but still far below the normal capacity in countries such as Luxemburg and Germany. ICU doctors and nurses made clear that a further expansion was impossible due to lack of qualified staff. At that point, the situation that not all eligible patients could be served became a terrible, but realistic prospect.
As a first step toward stricter triage protocols, Dutch Society of Intensive Care (NVIC) formulated various levels of increasingly strict medical criteria for patients to be admitted to the ICU (NVIC (Nederlandse Vereniging voor Intensive Care), 2020). Exclusion criteria were formulated in line with the CHEST Consensus Statement (Christian et al., 2014), based on low probability of survival and short life expectancy, such as ‘severe trauma with expected >90% mortality rate’, or ‘end-stage organ failure with life expectancy <1 year’. However, the possibility remained that even those stricter criteria would not be sufficient to allocate the scarce resources and it was expected that a next step involved patient selection on the basis of criteria that would be arbitrary from a medical point of view. At that point in time we were asked to offer further guidance.
Process
The KNMG organized a first videoconference in which they explained the problem and gave insight into the existing (medical) protocols and the stepwise approach to increasingly strict medical triage. They stressed the need for speedy work, since the situation was worsening quickly.
An initial in-depth discussion of possible criteria and subsequent email exchange led to a first version of our ethical advice on triage guidelines within 2 days. This draft was sent to representatives of the ethics departments of each of the eight Dutch medical schools. They were given 24 hours to comment on the draft and most responded within that time frame. The draft received general support and after a few adjustments a second draft was discussed with representatives of the FMS. Their feedback resulted in further adaptations and within a week after the first meeting our ethical advice together with a first draft of a guideline for ‘triage on non-medical grounds’ written by the FMS and the ethicists of KNMG based on our advice, was sent to the Dutch Health Inspectorate. The Inspectorate has a legal role in maintaining quality of care and the FMS felt that the Inspectorate’s support was essential to ascertain that physicians would not have to fear litigation if they actually did perform triage on non-medical grounds. The Inspectorate wanted information on the views of societal stakeholders and therefore asked the KNMG to consult with a number of societal parties (associations of elderly, patient associations and other professional organizations). Interestingly, the consultations conducted with the KNMG did not give rise to major critique, so no significant adaptations appeared necessary. Simultaneously, the guideline was brought on par with various other medical guidelines dealing with triage in other settings (nursing homes, ER, etc.) and several weeks after the first videoconference, the draft protocol was offered to the Inspectorate and sometime later also to the Dutch Minister of Health.
The Advice
One thing was clear in the discussions from the outset: we were to offer guidance for a scenario that everyone abhorred and wanted to avoid by all means. Triage on non-medical grounds would be a true tragedy since it implied that patients who could potentially benefit from ICU treatment were to be denied this treatment. Ethical guidance at best could aim at helping physicians to make the ‘least worst’ decisions. Any set of criteria we would propose would involve some degree of contingency and it was also clear that at some point no substantive grounds for allocation might be available and that then the fairest approach would be to defer to a randomized procedure for allocating beds, i.e. a lottery. But before that, in our view, it was possible to come with some more substantive guidance for triage decisions. We agreed on several basic ethical notions (Table 1).
Table 1.
Basic ethical notions as endorsed in the guideline
Basic ethical notions for triage
|
The most fundamental notion was that all human beings have equal worth, which we considered a basis for holding that many personal features should be irrelevant for triage decisions, such as ethnicity, gender, social or legal status or wealth. Moreover, we rejected selection based on mental and physical impairment and (prior) quality of life indices, from the principle that every human being has equal moral worth and every life is worth saving. Medical criteria like the clinical frailty score (CFS) (De Geer et al., 2020; Guidet et al., 2020), had already been used as a factor to determine probability of survival in earlier selection steps, implying there would be no remaining relevant medical grounds for triage on the basis of impairments at this stage. At that point, experienced quality of life is irrelevant. We also considered judgments about ‘personal responsibility for illness’ or ‘own fault’ to be irrelevant for ICU admission, both for principled reasons (people should not have to pay in this way for what went wrong in their lives) and for practical reasons: it would be impossible, in the hectic situation of an outbreak, to determine ‘guilt’ in any fair way.
We were reluctant to prioritize health workers because one of the main arguments—the utilitarian consideration that serving health care workers first might enable them to continue their life-saving work—seemed rather irrelevant for ICU settings in the COVID-19 crisis. Once in need of ICU treatment, a patient needs months to recover from COVID-19 and is not expected to return to work in the short term. Eventually we did suggest some form of prioritization of people working in health care; not for reasons of utility but as a matter of desert given the increased and sometimes unavoidable exposure to the virus in their professional (life-saving) work. This consideration would be particularly relevant if these health care workers (including cleaning and transport personnel) did not have sufficient personal protection.
We also agreed on the basic idea of fair innings that younger persons have a stronger claim to life-saving interventions, but gave it the specific form as explained below. Finally, the criteria we proposed should not be used to compare patients already admitted to patients waiting for intensive care, although we did leave room for reevaluating the prospects of patients in ICU, which might lead to withdrawal of intensive care for medical reasons.
Our final advice is summarized in Table 2.
Table 2.
Final guidance on COVID-19 pandemic ICU triage
Final advice
|
Evaluation
There has been much discussion in past decades, as well as during the current COVID-19 crisis about the justification of triage criteria (Truog et al., 2006; Verweij, 2009; Kirby, 2010; Kaposy and Khraishi, 2012; Emanuel et al., 2020). A reasonable justification has both substantive (are there morally relevant grounds for selecting patients?) as well as procedural (what is a fair process to come to a triage protocol?) elements. In pluralist societies chances are high that we will disagree about principles that should govern rationing (Daniels, 2000) although there are various ways to find overlap and divergence between different normative approaches (Verweij, 2009). In this article, we reflect on the process toward a triage protocol, specifically on our own role in it and on what we have learned. We elaborate on six points.
Should Medical Ethics Offer ‘Fair’ Guidance That Tidies Up Questionable Political Choices from the Past?
Some of our colleagues thought this was an example of ‘wheeling in the ethicist’ for problems that should not have occurred in the first place. In the Netherlands there is much emphasis on efficiency in health care and, as a result of that, the ICU capacity is simply too small to cope with extreme circumstances. If this was a matter of too much efficiency-thinking and insufficient political foresight, should ethicists lend themselves to tidy things up?
We agree that pandemic preparedness—and especially its ethical implications—could have been better, and we elaborate on that below. We do not agree with the assumption that bioethicists should not offer guidance in dilemmas that are the result of questionable policy choices from the past. Many ethical dilemmas can be avoided if timely action or precaution is taken or if more investments have been made; but that is not a reason to forego an advisory role when the dilemma does occur. Moreover, depending on the severity of the crisis, excessive scarcity could even occur in countries that were better prepared in terms of their ICU capacity, like Germany. Leaving it to doctors to ‘clear the rubbish’ and declining their request for ethical advice, would in our opinion not have been right.
For that matter, the assumption that in normal times there is insufficient over-capacity in the Netherlands—can also not be embraced without further analysis. Maintaining extra ICU capacity in normal times has opportunity costs and may well lead to other shortages elsewhere in the health care system.
Should Ethical Deliberation about Triage Criteria Not Be Part of Pandemic Preparedness to Avoid the (Ad Hoc) Pressures during a Crisis?
Another criticism raised by others as well as by ourselves concerns timing. Ideally, one would think, such controversial policies are not developed in the heat of a crisis but as a matter of pandemic preparedness. This would have many advantages: there is less time pressure, it may be easier to involve different stakeholders and politicians, and, given the lack of knowledge about the nature of the next pandemic and who will be at highest risk, deliberation can be more impartial as it occurs behind a ‘veil of ignorance’; not always the elderly are the highest risk group; the Spanish Flu, for example, especially hit hard among young adults. Moreover, it was put forward that public discussions about strict triage would cause additional anxiety among the most vulnerable groups (for COVID-19: elderly, chronically ill patients, persons with obesity).
In 2012, 3 years after the H1N1-pandemic, a Dutch bioethics think tank had issued a report outlining the most important ethical issues and possibilities with the urgent advice to the Minister of Health not to postpone these discussions until a new epidemic came along (CEG Centrum voor Ethiek en Gezondheid, 2012). Unfortunately, this was exactly what happened: the report sank into oblivion only to resurface when COVID-19 appeared.
Interestingly, during the process we started to see the benefits of ethical deliberation during crisis. We met much more consensus and support for controversial arguments and concrete proposals than we had expected. The assumption that it would be easier to agree on allocation principles in peacetime, when no immediate interests are threatened, thus might not be the whole truth. Moreover, one can question the legitimacy of such general principles that are meant to guide choices in a crisis, if stakeholders have limited foresight of what the principles will actually imply in an actual crisis.
Finally, every epidemic or other disaster will be unpredictable to some extent, raising unpredictable ethical issues. For example, prioritizing health care staff is usually justified by their usefulness in combatting the disaster—in this case, however, duration of ICU admission and rehabilitation are so long, that this argument failed.
Of course, bioethical reflection in pandemic preparedness planning is of high importance, and the ethical reports and literature we had at our disposal proved highly useful for our deliberation. Our experiences, however, show that tailored ethical guidance must and can be made in the heat of a crisis.
Should One Accept Primacy of Medical Considerations for Triage Decisions?
There is yet another aspect to timing that requires critical reflection. We were asked to offer ethical guidance for triage decisions in case all (evidence-based) medical grounds for triage would have been exhausted. In fact, the NVIC had already written and updated a pandemic triage protocol in which infrastructure and medical triage criteria were formulated. We were called in when the doctors thought they would soon be at the end of their wits—not before. This conveys a view on triage decision-making in which ethical expertise has no place as long as medical criteria can still play a role in patient selection. This assumption is deeply problematic for several reasons.
First of all, it suggests a relatively clear distinction between situations where medical decisions can be all evidence-based, and situations where medical evidence offers insufficient ground for further patient selection. Arguably, this distinction is seldom clear cut.
Second, and much more fundamental, it suggests that medical criteria are relatively uncontroversial or even morally neutral (or at least beyond moral doubt) and that value judgments and ethical reasoning especially become relevant when strictly medical judgments are exhausted. This assumption does not hold given that medicine is a deeply value-laden practice anyway. But in case medical practice is approaching excessive scarcity and triage becomes necessary—even triage on still purely medical grounds—medicine itself adopts a different normative framework. Indeed, the (strictly medical) protocol of the NVIC emphasized that it offered a roadmap from focusing on optimal care for each individual patient to optimal medical care for the population as a whole. This is a controversial value-laden judgment indeed, in which ethical guidance seems appropriate. Moreover, saving most lives is only one of several possible ways to give substance to optimal medical care for the population—one could also aim to protect as many life years as possible, or include quality and not just quantity of life. Although we think saving most lives is a reasonable interpretation of efficiency in this context, this is not a self-evident ethical choice (Verweij, 2009).
Moreover, by giving primacy to medical considerations in order to save most lives, a particular position is taken in the fair-chances/best outcomes tradeoff (Daniels, 1993). Applying strictly medical criteria in triage decisions to attain optimal effects may imply that some groups lose all prospect to possible life-saving treatment. This can be considered inequitable: after all, if one belongs to a high-risk group in which it will be more difficult to be treated effectively, it does not imply that one would have no chance to benefit from intensive care at all. A full focus on medical grounds for efficient use of resources even runs the risk to broaden health inequalities and social injustices, given that determinants of ill-health and risk factors often cluster in groups that are socially deprived. Indeed, in the USA the COVID-19 pandemic shows a higher mortality among African-American men (Garg et al., 2020).
Although we acknowledge there was a risk that our ‘late arrival’ legitimized a primacy of purely medical considerations focusing on ‘best outcomes’, we succeeded in changing some earlier decisions on medical criteria. We helped to discard the idea to use age (e.g. >80 or even >70) as an absolute exclusion criterion, and we managed to ascertain that the CFS would not be used for non-elderly persons, as this might lead to undue discrimination of persons with preexisting mental or physical impairments.
Fair Innings or Discrimination of the Elderly?
Another lesson is the way we felt we had to reframe the ‘fair innings’ argument. Inspired by the Maryland community-based triage policy (Biddison et al., 2019), we argued that age as such should not be a criterion, but a large enough difference in age between patients who might benefit should. In our view, using the terminology of ‘generations’ captured this best, as it can be used to appeal to intergenerational solidarity. Indeed, during the first weeks of the outbreak, many elderly citizens stated that they would be prepared to give up their claim to an ICU bed if that could save the life of a younger person. At the same time, the mere mentioning of ‘age’ as a possible criterium also led to public and political agitation and accusations of age discrimination. However, during the consultation round with, among others, various patient groups and elderly citizens, it appeared that the ‘generations’ argument was well-received and thought justifiable, once properly explained and openly discussed amongst their constituency.
The Importance of Practicality
As mentioned above, it was the first time in the recent history of our country that these issues had to be discussed under the actual threat of absolute scarcity. Our advice therefore had be concrete and feasible. Earlier deliberations, such as the 2012 report mentioned above, had offered general considerations at best, but no clear practical steps to be followed (CEG Centrum voor Ethiek en Gezondheid, 2012). During our deliberations with physicians, every step in the protocol was related to the actual practice, including the concrete infrastructure and distribution of the ICU care in the Netherlands. This had some unexpected consequences.
For example, we stipulated that in a situation of absolute shortage, there should be no priority for pandemic victims over regular patients. The same non-medical criteria would have to apply to COVID-19 and non-COVID-19 patients alike. However, in practice there are COVID-19 and non-COVID-19 ICU units that face different levels of scarcity, so at one moment in time different criteria might apply to COVID-19 and non-COVID-19 patients. In order to treat those two groups as equal as possible, enough—but not too many—ICU beds should be reserved for non-COVID patients.
The specific features of this epidemic, especially the long admissions and protracted recovery after ICU, led to another new element: the usual argumentation about priority for health care workers and other so-called essential professions could no longer be based on their usefulness in fighting the consequences of the pandemic. Such priority could only be justified by appeal to the fact that health care workers had faced higher personal risks, in their work for the benefit of all patients. While health care workers do not run a bigger risk than many others as long as they are well-protected, the shortages of protective materials in the current crisis made a difference here. We argued that therefore only priority should be given to health care workers with frequent COVID-19 patient contacts and who had insufficient access—due to scarcity—to personal protection materials.
Should These Decisions Not Be Made in a Public Sphere and in a Democratic Process?
A triage protocol should not only be based on reasonable principles suggested by bioethicists but ideally also be the outcome of a politically legitimate process (Daniels, 2000). Our hope was that for that reason final decision regarding triage criteria in absolute scarcity would receive political support. In our advisory role we consistently argued that a final protocol would need to be endorsed by government to ascertain political legitimacy and democratic accountability, but we realized that this would be an almost impossible problem for politicians to take a stance on. For that reason, the consultation of various societal groups, as instigated by the health inspectorate and carried out by the KNMG, was especially worthwhile and we consider it as contributing to the legitimacy of the process.
In practice, attempts to get support from the Inspectorate and the Minister of Health led to a postponement of publication of the protocol of more than a month. At the beginning of the pandemic the complete parliament had supported a motion that ruled out triage on the basis of absolute age limits. Also after several discussions and negotiations, the Minister of Health remained critical of the protocol’s reference to age as a relevant consideration. Notwithstanding his view, mid-June 2020, the medical associations KNMG and FMS published the protocol, establishing its status as a valid professional guideline. The Inspectorate has called for a professional and social debate about the protocol, in order to consider decisions in line with it as satisfying standards of ‘good medical practice’ during times of a crisis. The medical associations see the current publication also as open for a societal debate that might lead to adjustments in the future. The publication received a relatively favorable coverage in newspapers and other media, as a first step in this debate.
Conclusion
Looking back on the process of drafting the triage guidelines, we can conclude several things. First, timely interaction between clinical and ethical expertise is necessary. This could and should have happened earlier. Medical grounds and ethical grounds for triage should not be separated, and this is illustrated by our experience with the process of alignment between the medical and non-medical guidelines. We were able to make some difference and offer guidance in the medical guidelines. By giving our advice and discussing it with representatives of the medical associations we helped to prevent an exclusion criterion in terms of absolute age that the doctors were considering, and we managed to assure that the CFS would not be used for non-elderly persons. Second, we feared that the predominant susceptibility of the elderly for COVID-19 would make fair innings especially controversial. However, there was a lot of support for the intergenerational solidarity argument and the related relative age criterion even from representatives of elderly associations.
Third, writing advice with this immense impact needs the (ad hoc) pressure during a crisis to come up with concrete, practicable, clear and unambiguous criteria to allow for procedurally just triage in the whole country. Without this pressure it is hard to believe that the painful choices that had to be made, would actually be made. Nor could the criteria have been geared to the specifics of this unique situation. While this illustrates that ‘peacetime’ ethical deliberations may not be best suited to arrive at such guidelines, the urgency and political sensitivity of the subject in the middle of a crisis complicates public democratic decision-making and hence raises questions of legitimacy.
During the discussions about the protocol, the threat of absolute scarcity gradually lessened. In fact, the horror scenario of triage on non-medical grounds has only been nearby in the south of the Netherlands, while the pressure in other parts of the country was still limited. On a national level, at most ¾ of the maximally expandable ICU capacity was in use during the peak of the crisis. Openly debating the protocol in society and parliament seemed less and less urgent and we feared that in the end the protocol would not be published at all. The medical associations, however, were determined to publish it as a professional guideline.
In the coming months political and societal debates will continue and this might result in adjustments, or a completely different protocol in the future. For now, however, there is a protocol in place that does offer guidance in a possible next wave in the pandemic. At the same time, the prospect that the protocol might become practice in the future is abhorred by proponents and opponents alike.
Acknowledgements
The authors are grateful for the intellectual and organizational support from KNMG ethicists Gert van Dijk, Antina de Jong and Krista Tromp.
Conflict of Interest
None declared.
Contributor Information
Marcel Verweij, Philosophy Group, Wageningen University.
Suzanne van de Vathorst, Medical Ethics, Philosophy and History of Medicine, Erasmus MC.
Maartje Schermer, Medical Ethics, Philosophy and History of Medicine, Erasmus MC.
Dick Willems, Amsterdam UMC.
References
- Abarshi E., Onwuteaka-Philipsen G., Donker G., Echteld M., Van den Block L., Deliens L. (2009). General Practitioner Awareness of Preferred Place of Death and Correlates of Dying in a Preferred Place: A Nationwide Mortality Follow-Back Study in the Netherlands. Journal of Pain and Symptom Management, 38, 568–577. [DOI] [PubMed] [Google Scholar]
- Antommaria A. H. M., Gibb T. S., McGuire A., Wolpe P. R., Wynia M. K., Applewhite M. K., Caplan A., Diekema D. S., Hester D. M., Lehmann L. S., McLeod-Sordjan R., Schiff T., Tabor H. K., Wieten S. E., Eberl J. T.; Task Force of the Association of Bioethics Program Directors (2020). Ventilator Triage Policies during the COVID‐19 Pandemic at U.S. Hospitals Associated with Members of the Association of Bioethics Program Directors. Annals of Internal Medicine, doi: 10.7326/M20‐1738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Biddison E. L. D., Faden R., Gwon H. S., Mareiniss D. P., Regenberg A. C., Schoch-Spana M., Schwartz J., Toner E. S. (2019). Too Many Patients. A Framework to Guide Statewide Allocation of Scarce Mechanical Ventilation during Disasters. Chest, 155, 848–854. [DOI] [PubMed] [Google Scholar]
- CEG Centrum voor Ethiek en Gezondheid (2012). Rechtvaardige selectie bij een pandemie [Fair Selection in Case of a Pandemic]. Den Haag: Center for Ethics and Health.
- Christian M. D., Sprung C. L., King M. A., Dichter J. R., Kissoon N., Devereaux A. V., Gomersall C. D. (2014). Triage: Care of the Critically Ill and Injured during Pandemics and Disasters: CHEST Consensus Statement. Chest, 146 (4 Suppl), e61S–e74S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daniels N. (1993). Rationing Fairly: Programmatic Considerations. Bioethics, 7, 224–233. [DOI] [PubMed] [Google Scholar]
- Daniels N. (2000). Accountability for Reasonableness. Establishing a Fair Process for Priority Setting is Easier than Agreeing on Principles. BMJ, 321, 1300–1301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Geer L., Fredrikson M., Tibblin A. O. (2020). Frailty Predicts 30-Day Mortality in Intensive Care Patients: A Prospective Prediction Study. European Journal of Anaesthesiology, doi: 10.1097/EJA.0000000000001156. [DOI] [PubMed] [Google Scholar]
- Emanuel E. J., Persad G., Upshur R., Thome B., Parker M., Glickman A., Zhang C., Boyle C., Smith M., Phillips J. P. (2020). Fair Allocation of Scarce Medical Resources in the Time of COVID-19. The New England Journal of Medicine, 382, 2049–2055. [DOI] [PubMed] [Google Scholar]
- Fogteloo M. (2020). Wie Krijgt Dat Schaarse Intensive Care Bed? De Groene Amsterdammer, 8 April 2020.
- Garg S., Kim L., Whitaker M., O’Halloran A., Cummings C., Holstein R., Prill M., Chai S. J., Kirley P. D., Alden N. B., Kawasaki B., Yousey-Hindes K., Niccolai L., Anderson E. J., Openo K. P., Weigel A., Monroe M. L., Ryan P., Henderson J., Kim S., Como-Sabetti K., Lynfield R., Sosin D., Torres S., Muse A., Bennett N. M., Billing L., Sutton M., West N., Schaffner W., Talbot H. K., Aquino C., George A., Budd A., Brammer L., Langley G., Hall A. J., Fry A. (2020). Hospitalization Rates and Characteristics of Patients Hospitalized with Laboratory-Confirmed Coronavirus Disease 2019—COVID-NET, 14 States, March 1–30, 2020. Morbidity and Mortality Weekly Report, 69, 458–464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guidet B., de Lange D. W., Boumendil A., Leaver S., Watson X., Boulanger C., Szczeklik W., Artigas A., Morandi A., Andersen F., Zafeiridis T., Jung C., Moreno R., Walther S., Oeyen S., Schefold J. C., Cecconi M., Marsh B., Joannidis M., Nalapko Y., Elhadi M., Fjølner J., Flaatten H; for the VIP2 Study Group (2020). The Contribution of Frailty, Cognition, Activity of Daily Life and Comorbidities on Outcome in Acutely Admitted Patients over 80 Years in European ICUs: The VIP2 Study. Intensive Care Medicine, 46, 57–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaposy C., Khraishi S. (2012). A Relational Analysis of Pandemic Critical Care Triage Protocols. International Journal of Feminist Approaches to Bioethics, 5, 70–90. [Google Scholar]
- Kirby J. (2010). Enhancing the Fairness of Pandemic Critical Care Triage. Journal of Medical Ethics, 36, 758–761. [DOI] [PubMed] [Google Scholar]
- NVIC (Nederlandse Vereniging voor Intensive Care) (2020). Draaiboek Pandemie Deel 1 [Protocol Pandemics, Part 1]. Versie 1. Netherlands Association of Intensive Care.
- Rhodes A., Ferdinande P., Flaatten H., Guidet B., Metnitz P. G., Moreno R. P. (2012). The Variability of Critical Care Bed Numbers in Europe. Intensive Care Med, 38, 1647–1653. [DOI] [PubMed] [Google Scholar]
- Truog R. D., Brock D. W., Cook D. J., Danis M., Luce J. M., Rubenfeld G. D., Levy M. M; Task Force on Values, Ethics, and Rationing in Critical Care (VERICC) (2006). For the Task Force on Values, Ethics, and Rationing in Critical Care (VERICC) (2006). Rationing in the Intensive Care Unit. Critical Care Medicine, 34, 958–963. [DOI] [PubMed] [Google Scholar]
- Verweij M. (2009). Moral Principles for Allocating Scarce Medical Resources in an Influenza Pandemic. Journal of Bioethical Inquiry, 6, 159–169. [Google Scholar]