Figure 2.
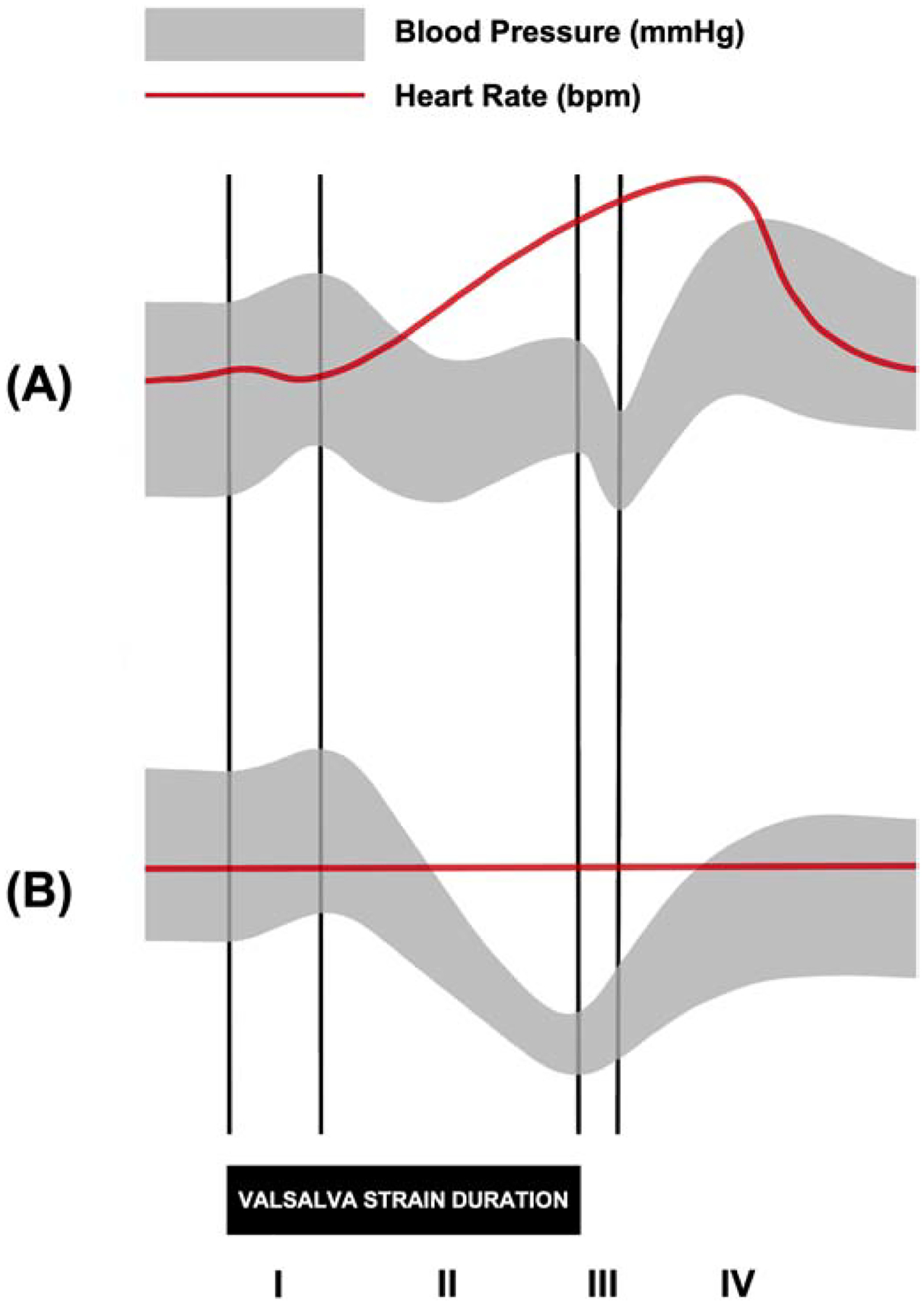
Representative blood pressure (BP) and heart rate (HR) tracings during the Valsalva maneuver in (A) healthy subjects and (B) patients with neurogenic orthostatic hypotension. The Valsalva maneuver is used to evaluate the sympathetic and parasympathetic responses of the baroreflex as an individual forcibly exhales at maximum pressure (~40 mmHg) for 15 seconds. Those with intact autonomic nervous system function are expected to exhibit a specific pattern of physiological responses to the Valsalva maneuver that can be divided into four phases: (I) the mechanical increase in intrathoracic pressure causes a brief increase in BP and decrease in HR; (II, early) the reduction in venous return causes a decrease in stroke volume and BP; (II, late) the baroreflex is activated by the decrease in BP, causing a sympathetically-mediated increase in BP and HR; (III) the pulmonary vascular refills with blood upon termination of the Valsalva maneuver, causing a decrease in BP; (IV) the sudden increase in venous return leads to a compensatory decrease in HR and increase in BP that overshoots baseline BP due to residual sympathetic activity. In patients with impaired autonomic function, as in neurogenic orthostatic hypotension, there is a lack of late phase II BP increase and BP overshoot in phase IV recovery.
