Abstract
Objective
To analyse the remodelling and recovery of a relocated intravitreal injection (IVI) service with an adapted treatment regimen in a tertiary referral centre during a nationwide lockdown with initial cancellation of all non-emergency treatments caused by the COVID-19 pandemic.
Methods and analysis
For this retrospective observational study at Hanusch Hospital, Vienna, between 16 March 2020 and 5 May 2020, we conducted an analysis of an appointment booking system based on prioritisation incorporating disease class, severity and fellow eye status by evidence-based impact on irreversible structural impairment and survey data from telephone interviews. Recapture time was defined as the time-to-discard the backlog of patients in need for treatment. Non-attendance was stratified as treatment refusal for personal reasons and non-attendance due to lockdown-related restrictions.
Results
Of the 1109 patients, 241 (21.7%) were considered as highly urgent, 269 (24.3%) as urgent, 402 (36.2%) as semiurgent and 197 (17.8%) as non-urgent. Recapture time was 15 days for highly urgent patients, 22 days for urgent patients, 43 days for semiurgent patients and 46 days for non-urgent patients. The proportion of patients who refused treatment due to personal reasons was 5.2%, with a mean age of 82.4 years; 29 patients (2.6%) could not attend due to lockdown-related restrictions.
Conclusion
By streamlining treatment based on urgency as well as increasing the number of bilateral IVI, recapture time was fast. We could provide a safe treatment environment for healthcare professionals and patients after resetting the injection service outside of the hospital with increased levels of protection.
Keywords: degeneration, macula, neovascularisation, retina
Key messages.
What is already known about this subject?
The COVID-19 pandemic has affected all aspects of clinical practice, and nationwide lockdowns have become the main approach to flatten the curve of new infections.
What are the new findings?
A consequent triage system based on hierarchical prioritisation based on urgency minimises treatment delay for all patients in need for intravitreal treatment and allows adapted continuation of care; further survey analysis of reasons for non-attendance and treatment refusal for personal reasons provides more insight on the implemented changes.
How might these results change the focus of research or clinical practice?
The strategies undertaken can be refined and may serve as a blueprint in case of a second wave and help identifying those patients not being able to attend the injection clinics, thus helping to improve treatment and service strategies.
Introduction
As of 29 June 2020, a novel coronavirus, termed SARS-CoV2, has accounted for around 10.1 million cases of disease globally. Since the first reports of the virus in Wuhan, China, on 31 December 2019,1 the disease has spread globally, and the coronavirus disease now commonly named COVID-19 was declared an Emergency of international concern on 30 January 2020 and a pandemic on 11 March.2 3
The first cases of COVID-19 in Austria, an Italian couple travelling to work in Austria from Bergamo, Italy, were recorded on 25 February 2020 in Innsbruck.4
The Tyrolean ski resort of Ischgl soon after was identified as a COVID-19 hotspot, and the disease has spread remarkably fast throughout Europe.5 On 13 March, the Austrian government announced the temporary closure of universities and schools, and on 16 March, restaurants were closed, and public gatherings were banned. Austrian citizens were only allowed to leave their homes for necessary professional activities, groceries and to assist other people, especially the elderly, and the government introduced restrictions for outdoor activities.6 7
The Hanusch Hospital in Vienna is a tertiary referral centre for ophthalmology with a highly frequented medical retina service, conducting more than 13 000 intravitreal injections (IVIs) in 2019. In the evening of 14 March 2020, the medical director announced a hold to all non-emergency surgery and elective inpatient admissions until the end of April to all departmental leads. Our centre was dedicated to non-CoVID-19 related care; thus, patients with confirmed COVID-19 related disease would be transferred to other hospital services. Safety measurements at our hospital were installed overnight; all but two entrances were closed, and healthcare professionals were separated from patients and had to pass a symptom check including temperature measurements. Patients were screened in a separate triage system including full personal protection equipment (PPE) for healthcare professionals and isolation capacities if needed. IVIs of anti-vascular endothelial growth factor (VEGF) agents for neovascular age-related macular degeneration (nvAMD) and selected retinal vascular diseases including central retinal vein occlusion (CRVO) are not considered elective surgery as, despite the threat of sight impairment in the case of treatment deferral, they do not fulfil the criteria of emergency treatments.8 As injection appointments were among the first elective procedures to be deferred, a progressive backlog accumulated day by day. By 15 March 2020, the ophthalmology department split into three teams to ensure maintenance of care in case of an infection of team members.
To restart the injection service, several tasks needed to be addressed: first, a triage system was agreed to classify patients with respect to the urgency of planned treatments similar to other subspecialties. Second, a new injection location had to be found outside of the hospital to protect this COVID-19 free environment, and third, patients had to be contacted by phone or, if not available, by information letters and should be rescheduled. After intense logistics, a dedicated injection room with a spacious waiting area to avoid crowding was established in a satellite clinic about 6 km away from the hospital. With a rapidly escalating global need for PPE, protection for doctors and nurses, as well as protection for the administrative staff had to be transferred, and examination rooms had to be relocated. After 8 days, on 24 March, the first IVI in lockdown was administered to patients.
In this article, we aim to analyse the response to the COVID-19 pandemic in our injection service, including survey data from telephone interviews providing insights on triage mechanisms and patient acceptance and learning points for a looming second wave.
Materials and methods
With every day of standstill, the numbers of patients awaiting their injections were increasing. The risk of sight loss due to treatment deferral is influenced by several factors: disease entity, visual acuity (VA) levels, laterality and VA levels in fellow eyes. To address these factors, triage criteria to establish an urgency grading for all patients receiving anti-VEGF IVI were proposed by the head of department and the medical retina service lead and were communicated to all team members. Patients were called by doctors and informed about the changed location of the injection service and new appointment dates. If a patient could not be reached, the next of kin would be contacted; if unsuccessful, information letters were sent to the patients via postal service. A backlog register with daily back-ups was set forth including patient name, date of birth, triage grade, prelockdown injection date, new injection date and telephone call notes including reasons for non-attendance for all patients from 16 March 2020. The new protocols were explained to the patients, and a verbal consent to proceed with the planned date was obtained. Patients, who could not attend or refused treatment for personal reasons, were called after 2 weeks and offered another appointment. Triage was stopped at the point in time, when all previously rescheduled patients could be injected as initially planned and no further delay of treatment was observed.
Urgency triage criteria
The following classification was applied to all patients after an electronic medical record review with additional optical coherence tomography (OCT) image analysis if needed.
Grade 1 consisted of patients with nvAMD or CRVO in one eye, with a VA in the fellow eye below 20/60 Snellen; treatment for these patients was considered to be highly urgent. Grade 2 consisted of patients with bilateral nvAMD or bilateral CRVO and a VA in both eyes above 20/60 Snellen, or patients with nvAMD in one eye and a VA in the fellow eye between 20/60 and 20/40 Snellen; treatment for these patients was considered as urgent. Grade 3 included patients with nvAMD or CRVO and a VA in the fellow eye greater or equal to 20/32 Snellen; treatment was considered as semiurgent. Grade 4 comprised patients with diabetic macular oedema (DMO), macular oedema secondary to branch retinal vein occlusion, pseudophakic macular oedema secondary to intraocular surgery or age-related macular degeneration (AMD) with a VA below 20/400 in the affected eye; treatment was considered as non-urgent. The triage criteria are summarised in table 1.
Table 1.
Triage criteria
| Grade 1: highly urgent | Patients with neovascular age-related macular degeneration (nvAMD) or central retinal vein occlusion (CRVO) in one eye, with a visual acuity (VA) in the fellow eye below 20/60 Snellen. |
| Grade 2: urgent | Patients with bilateral nvAMD or bilateral CRVO and a VA in both eyes above 20/60 Snellen or patients with nvAMD in one eye and a VA in the fellow eye between 20/60 and 20/40 Snellen. |
| Grade 3: semiurgent | Patients with nvAMD or CRVO and a VA in the fellow eye greater or equal to 20/32 Snellen. |
| Grade 4: urgent | Patients with diabetic macular oedema, macular oedema secondary to branch retinal vein occlusion, pseudophakic macular oedema secondary to intraocular surgery or age-related macular degeneration with a VA below 20/400 in the affected eye. |
Injection room relocation
To enter the new injection room with adjacent administrative area in a satellite clinic, all patients had to undergo symptom screening including temperature check and received face masks at the entrance. Teams consisted of an ophthalmologist conducting the IVI, assisting nurses and administrative personnel. To keep the contact time with the healthcare professionals at an acceptable minimum, patients were asked a standardised questionnaire about recent deterioration in VA or new onset of symptoms (figure 1). Only in case of a positive answer, a slit lamp examination was performed. The PPE during the injection procedure for the healthcare professionals consisted of a surgical mask, gloves and frequent hand disinfection; administrative staff members were protected via screens and surgical masks. Slit lamps were adapted with protection screens. Appointment booking was extended to 15 min slots per patient, and waiting rooms were adapted accordingly to guarantee distancing for patients.
Figure 1.
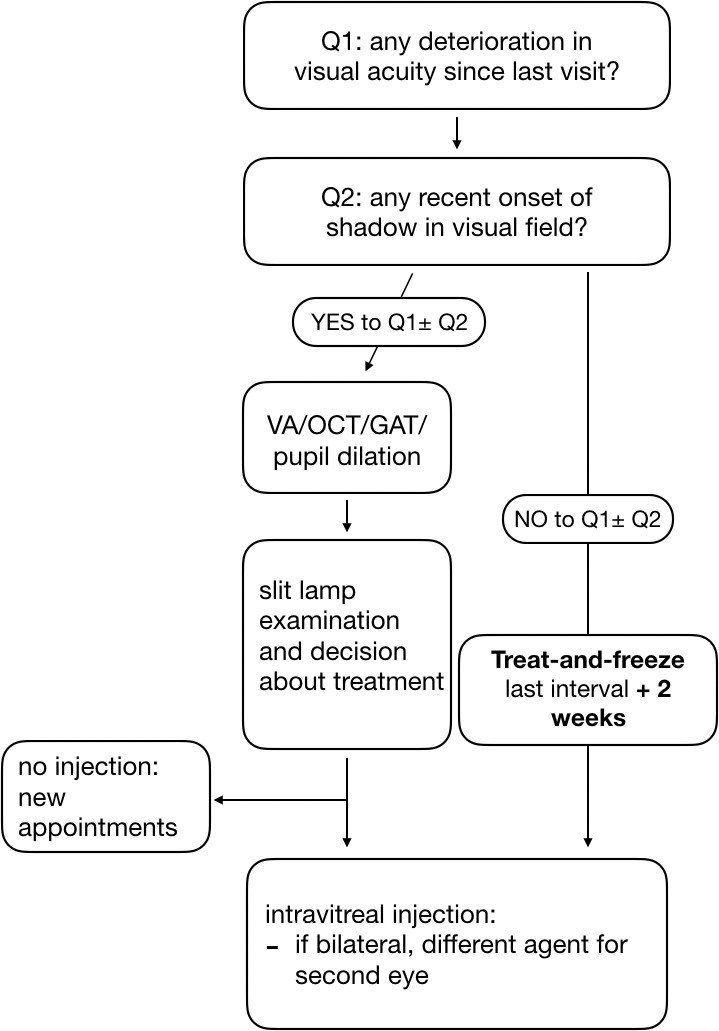
Flow chart of treat-and-freeze regime for IVI with limited patient–doctor exposure to minimise the risk of infection during the COVID-19 pandemic. Patients, who had a new onset of symptoms or deterioration in their visual acuity (VA) would receive an optical coherence tomography (OCT) scan, Goldmann applanation tonometry (GAT) and a dilated fundus examination. All other patients would receive an IVI without routine examination, and the retreatment interval was extended by 2 weeks with respect to their previous treatment interval. IVI, intravitreal injection.
Treatment protocol
Following a survey of Austrian medical retinal key decision makers and clinical leads, an adapted treatment protocol was established at our institution. The standard treatment regime in place prior to the COVID-19 pandemic was a treat-and-extend regimen for patients with nvAMD or macular oedema secondary to retinal vein occlusions and a pro re nata regime for DMO. The proposed treatment protocol named treat-and-freeze is summarised in figure 1. It consisted of several key points: first, a standardised questionnaire was asked to identify patients with potential deterioration or retinal detachment symptoms who would be examined with VA assessment, OCT, Goldmann applanation tonometry and dilated fundus exam. If eligible for treatment, patients would then receive an IVI, and the retreatment interval would be determined by the medical retina specialist. All other patients would receive an IVI without further pupil dilation, and the interval would be subsequently extended by 2 weeks for the next appointment with the outlook of maintaining the interval, unless changes were reported. Second, bilateral injections were offered for all patients who were under a treat-and-extend regime to both eyes, and treatment intervals were adjusted to the eye with the shorter interval. To minimise the risk of endophthalmitis or toxic reactions, different agents were used in the two eyes and a single surgical cover covering both eyes for bilateral injections was used as recommended in guidelines.9 10 If bilateral treatment implicated a change of agents for one eye, patients were reconsented. Patients refusing bilateral treatment in one session would receive the injection in the eye with the better prognosis; the other eye would be downgraded and rescheduled. Injection clinic patient lists were screened for patients awaiting bilateral injections the following day to plan accordingly.
Patient and public involvement
This research was done without patient involvement. Patients were not invited to comment on the study design and were not consulted to develop patient-relevant outcomes or interpret the results. Patients were not invited to contribute to the writing or editing of this document for readability or accuracy.
Results
Urgency triage
A total of 1109 patients were included in our analysis from 16 March 2020 to 5 May 2020. Grade 1, defined as high urgency, consisted of 241 (21.7%) patients. Grade 2, including all urgent patients, consisted of 269 (24.3%) patients, grade 3, incorporating all semiurgent patients, consisted of 402 (36.2%) patients and grade 4, including all non-urgent patients, comprised 197 patients (17.8%). The mean age of all patients was 77.5 years (median 79 years) and was equally distributed in all grades; all results are summoned in table 2.
Table 2.
Summary of patient characteristics
| All | Grade 1: highly urgent | Grade 2: urgent | Grade 3: semiurgent | Grade 4: non-urgent | |
| Patients (n) | 1109 | 241 | 269 | 402 | 197 |
| Bilateral IVI | 147 | ||||
| Recapture date | 30 April 2020 | 30 March 2020 | 6 April 2020 | 27 April 2020 | 30 April 2020 |
| Recapture time (days) | 46 | 15 | 22 | 43 | 46 |
| Age (mean) | 77.47 | 77.35 | 77.37 | 77.40 | 77.30 |
| NA – total (mean age), n (%) | 29 (86.00) | 8 (92.00) | 5 (86.00) | 11 (86.00) | 5 (77.00) |
| NA – outside Austria, n (%) | 10 (87.50) | 4 (89.00) | 3 (83.00) | 1 (92.00) | 2 (74.00) |
| NA – poor general health, admitted to hospital or recent surgery, n (%) | 9 (89.00) | 2 (93.50) | 0 (0.00) | 5 (86.00) | 2 (84.50) |
| NA – treatment received elsewhere (private practice or hospital eye service), n (%) | 2 (67.50) | 0 (0.00) | 0 (0.00) | 2 (67.50) | 0 (0.00) |
| NA – under quarantine, n (%) | 5 (82.00) | 2 (87.00) | 1 (80.00) | 2 (85.00) | 0 (0.00) |
| NA – in retirement home, n (%) | 3 (94.00) | 0 (0.00) | 1 (86.00) | 1 (94.00) | 1 (95.00) |
| Treatment refusal for personal reasons, n (mean age) | 58 (82.43) | 13 (86.38) | 9 (82.00) | 23 (84.35) | 11 (74.91) |
| Proportion of patients refusing treatment per grading (%) | 5.2 | 5.4 | 3.3 | 5.7 | 5.6 |
IVI, intravitreal injection; NA, non-attendance.
Treatment delay and recapture time
Two factors were causing the backlog of patients in need for IVIs: the deferral period of 8 days caused by the necessity to relocate the injection service away from a site where all elective procedures had been stopped and a reduced injection capacity in the new location caused by safety measurements to avoid crowding of patients in the waiting area. We adapted a new booking system based on the urgency grading. As a first step, only those patients with appointments for a particular day and a high urgency defined as grade 1 would keep their appointments, and all other patients were cancelled. The available, yet reduced slots were filled in with patients from the backlog register and a high urgency grade. Once all patients with grade 1 could be booked for appointments, we then continued the same procedure for all patients with grades 1 and 2, and after successful booking, proceeded with grades 3 and 4. The time-to-discard the backlog of patients awaiting their treatments was defined as recapture time. For all grades, the recapture time was 46 days and was achieved on 30 April. Grade 1, defined as highly urgent, had a recapture time of 15 days; all patients defined as grade 1 could receive treatment without any delay after 30 March. Recapture time for grade 2 was 22 days and was achieved on 6 April; for grades 3 and 4, recapture time was 43 days and 46 days, respectively, and was achieved on 27 April and 30 April.
Non-attendance and treatment refusal
During the lockdown, social distancing for all was considered to be paramount in order to flatten the curve. In times of unprecedented measures like travel restrictions, planned patient attendance in this cohort was of high interest, as treatment slots were limited. Thus, patients were called and briefly informed about the new injection modalities and surveyed whether they planned to attend, and if not, their motives were recorded and documented. In total, 29 patients with a mean age of 86.0 years announced that they could not attend their injection appointments. Ten patients could not attend, as they were outside of Austria, and 13 patients were unable to receive treatment due to poor general health, admission to hospital or because of recent surgical procedures. Four patients had sought treatment either in private practice or at other hospital eye services. Five patients could not attend as they were under quarantine due to COVID-19 exposure or infection, and four patients could not attend as they were residents in retirement homes.11
Patients would also refuse to be treated for personal reasons. In these situations, they were called after 2 weeks and were asked again whether they had reconsidered receiving treatment with anti-VEGF IVI. In total, 58 patients with a mean age of 82.4 years refused treatment for their macular disease, which represents a proportion of 5.2% of all patients: 13 patients with grade 1 (mean age 86.4, 5.4% of patients with grade 1), 9 patients with grade 2 (mean age 82.0, 3.3% of patients with grade 2), 23 patients with grade 3 (mean age 84.4, 5.7% of patients with grade 3) and 11 patients with grade 4 (mean age 74.9, 5.6% of patients with grade 4) decided not to attend the injection clinics for personal reasons, usually being very worried of getting infected when leaving the house. These patients have been contacted repeatedly to provide an opportunity for treatment as the numbers of infections have started to decline and the lockdown was stopped, leading to a gradual opening of services.
Discussion
A fast remodelling of injection pathways combined with an efficient triage is necessary to ensure continuation of treatment for those with sight-threatening macular diseases during a pandemic caused by this contagious virus. By adapting all necessary protection proceedings for both healthcare professionals and patients as well as streamlined treatment based on urgency, we could effectively recapture the time lost due to an essential lockdown in the early nationwide response to COVID-19. Although almost all patients receiving treatment in our injection service are at higher risk to develop a more severe form of COVID-19 due to their age, patient acceptance of the measures taken were high, and treatment refusal was only at 5.2%.
The COVID-19 pandemic has put ophthalmologists across the world under pressure from several sides. Early anecdotal reports hinted that among the specialties in medicine, ophthalmologists were at higher risk of being infected by SARS-Cov2.12–14 Whereas cataract surgery is considered elective surgery and may be postponed in times of crisis, deferral of anti-VEGF injections for nvAMD can lead to loss of vision that cannot be recovered.15 COVID-19 is causing a higher mortality in the elderly, which may be contributed to higher incidences of comorbidities.[16 17 The mean age of patients analysed in this study is 77.5 years and highlights the fact that protection of this cohort from infection with SARS-Cov2 is paramount. The urgency of anti-VEGF treatment is not considered to be equal in nvAMD, macular oedema secondary to retinal vein occlusion and DMO.8 Austria was hit by the pandemic earlier than Germany, the UK or the USA, hence guidance from professional organisations was scarce and daily updates were of great help.18–20 Nevertheless, the grading system used in our centre was already established and ongoing by the start of the newly established injection service on 24 March.
In hindsight, the number of new COVID-19 infections in Austria peaked on 26 March, when 1063 patients were tested positive.21 As the nationwide curve seemed to flatten in the following days, patients in our centre with high urgency could receive IVI without any delay from 30 March onwards. Almost half of the patients affected by the lockdown and resulting remodelling of the service (46%) were considered to be either highly urgent or urgent. To be able to provide ongoing care for these patients under intensified protection and extended time slots, we had to adjust our service and would like to highlight two important factors: first, the delay of patients with diseases that are considered less urgent like DMO in the urgent phase,22 23 and second, preferred bilateral IVI application if possible. When comparing the number of bilateral injections during the observation period from 24 March to 5 May to a similar period prior to the remodelling phase (2 February to 13 March), we conducted 150 bilateral IVI compared with 22 bilateral IVI prior to the COVID-19 crisis. The combination of increasing bilateral injections and a hierarchical prioritisation provided enough slots for patients to be treated accordingly in the urgent phase. By achieving a fast recovery, we could then start to rebook patients, who were graded as semiurgent or non-urgent, without compromising safety of both patients and healthcare professionals. After 46 days, we were able to continue to book all patients as previously planned. We have deliberately decided to defer steroid injections in the first weeks based on our triage criteria and have offered them to patients in selected cases after the lockdown was eased.
Although the treat-and-freeze protocol as used in our service during the lockdown has proven to be effective, as it has helped to limit face-to-face exposure and time at the injection service, the absence of OCT guidance, however, has limits. Patients, who may have developed small signs of activity as small intraretinal haemorrhages, might not be aware of any visual changes at presentation yet would have been extended by 2 weeks. However, bilateral treatment in eyes with different disease activity needs careful triage, and undertreatment has to be avoided. The use of this protocol, until proven otherwise, is indeed limited to times of need.
How patients have responded to this crisis is of great interest. As we were reaching out to all our patients via telephone to inform them about the new appointment dates, we could survey 29 patients for their reasons of non-attendance. These were caused either by travel restrictions, patients being unwell or under quarantine or residents in retirement homes who were affected by lockdown more extensively as several COVID-19 hotspots were located in these facilities.24 Understandably, patients also refused to attend our injection service based in a satellite clinic, when media reporting of high risks of infection was ubiquitous. Interestingly, the rates of treatment refusal were lower than reported in other countries, where, for example, anecdotal reports of no-show rates of 25% have pushed clinical leaders to arrange to reach out to patients in their homes.25 Of the 1109 patients included in our analysis, only 58 patients with a mean age of 82.4 years decided to reject treatment for personal reasons. When stratifying by urgency grades, the mean age of patients declining attendance was higher than the average age in high-urgent to semiurgent groups and lower than average in the non-urgent group. This could be explained by the fact that the non-urgent group includes patients with DMO who are of younger age but also more prone to suffer from comorbidities than those suffering from nvAMD.
A limitation of our study is the retrospective observational nature of the analysis. Three doctors were in charge of the backlog register and conducted the phone interviews. Further studies are warranted to identify the impact of this pandemic on the treatment of macular diseases.
For the foreseeable future, our clinics may continue to change at a rapid pace. Researchers across the globe are streamlining efforts to find potential vaccine candidates.26 With a second wave looming, lessons learnt from the lockdown may prove their value, as a subsequent partial or complete lockdown may or may not be necessary in the upcoming winter.27 Hospital providers need to anticipate and engage with high levels of flexibility to provide care with maximum patient and physician safety, and short audit cycles will be essential to be able to care for all our patients in need, regardless of urgency.
Acknowledgments
The authors would like to thank Siegfried K Wagner for helping with language editing.
Footnotes
Contributors: All listed authors contributed to the conception or design of the work; or the acquisition, analysis or interpretation of data for the work; drafted or revised the work critically for important intellectual content; and finally approved this version to be published and agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. JoH and OF are responsible for the overall content as guarantors.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent for publication: Not required.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: All data relevant to the study are included in the article.
References
- 1.Huang C, Wang Y, Li X, et al. . Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020;395:497–506. 10.1016/S0140-6736(20)30183-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Statement on the second meeting of the International Health Regulations Emergency Committee regarding the outbreak of novel coronavirus (2019-nCoV), 2005. Available: https://www.who.int/news-room/detail/30-01-2020-statement-on-the-second-meeting-of-the-international-health-regulations-(2005)-emergency-committee-regarding-the-outbreak-of-novel-coronavirus-(2019-ncov) [Accessed 21 May 2020].
- 3.WHO Director-General’s opening remarks at the media briefing on COVID-19. Available: https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19-11-march-2020 [Accessed 21 May 2020].
- 4.Rourke A, Farrer M, Marsh S, et al. . Europe on alert as four more Covid-19 deaths reported in Italy – as it happened, 2020. Available: http://www.theguardian.com/world/live/2020/feb/25/coronavirus-live-updates-outbreak-latest-news-italy-italia-deaths-symptoms-china-stocks-wall-street-dow-jones-economy-falls [Accessed 21 May 2020].
- 5.Mikhail J. Coronavirus: Wie Skiort Ischgl zur europäischen Brutstätte wurde - WELT, 2020. Available: https://www.welt.de/wissenschaft/article206592389/Coronavirus-Wie-Skiort-Ischgl-zur-europaeischen-Brutstaette-wurde.html [Accessed 21 May 2020].
- 6.Verordnung gemäß § 2 Z 1 des COVID-19-Maßnahmengesetzes. Available: https://www.sozialministerium.at/dam/jcr:640e8f8d-f4ca-4fd7-bdd8-93b5c2e2c52a/BGBLA_2020_II_98%20(3).pdf [Accessed 21 May 2020].
- 7.Landesregierung A der T. Quarantäneverordnung für alle 279 Tiroler Gemeinden. Available: https://www.tirol.gv.at/meldungen/meldung/artikel/quarantaeneverordnung-fuer-alle-279-tiroler-gemeinden/ [Accessed 21 May 2020].
- 8.Guidance for anti-VEGF intravitreal injections during the COVID-19 pandemic. Available: https://www.springermedizin.de/covid-19/guidance-for-anti-vegf-intravitreal-injections-during-the-covid-/17923100?fulltextView=true [Accessed 25 May 2020]. [DOI] [PMC free article] [PubMed]
- 9.The Royal College of Ophthalmologists - Ophthalmic Service Guidance Intravitreal injection therapy. Available: https://www.rcophth.ac.uk/wp-content/uploads/2018/02/Intravitreal-Injection-Therapy-August-2018-2.pdf [Accessed 23 May 2020].
- 10.Grzybowski A, Told R, Sacu S, et al. . 2018 update on intravitreal injections: Euretina expert consensus recommendations. Ophthalmologica 2018;239:181–93. 10.1159/000486145 [DOI] [PubMed] [Google Scholar]
- 11.RIS - Betretungsverbot für Besucherinnen und Besucher von Krankenanstalten, Wohn- und Pflegeheimen sowie Pflegestationen - Landesrecht konsolidiert Wien, Fassung vom 26.05.2020. Available: https://www.ris.bka.gv.at/GeltendeFassung.wxe?Abfrage=LrW&Gesetzesnummer=20000600 [Accessed 26 May 2020].
- 12.Zhou Y, Zeng Y, Tong Y, et al. . Ophthalmologic evidence against the interpersonal transmission of 2019 novel coronavirus through conjunctiva. medRxiv 2020. [Google Scholar]
- 13.Charters L. Researchers find low risk of COVID-19 transmission in tears. Available: https://www.ophthalmologytimes.com/article/researchers-find-low-risk-covid-19-transmission-tears-0 [Accessed 25 May 2020].
- 14.2019-nCoV transmission through the ocular surface must not be ignored. The Lancet 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Richard G, Monés J, Wolf S, et al. . Scheduled versus pro re NatA dosing in the view trials. Ophthalmology 2015;122:2497–503. 10.1016/j.ophtha.2015.08.014 [DOI] [PubMed] [Google Scholar]
- 16.Liu K, Chen Y, Lin R, et al. . Clinical features of COVID-19 in elderly patients: a comparison with young and middle-aged patients. J Infect 2020;80:e14–18. 10.1016/j.jinf.2020.03.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chen J, Qi T, Liu L, et al. . Clinical progression of patients with COVID-19 in Shanghai, China. J Infect 2020;80:e1–6. 10.1016/j.jinf.2020.03.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Coronavirus COVID-19 « dog. Available: https://www.dog.org/?cat=288 [Accessed 25 May 2020].
- 19.American Academy of Ophthalmology Important coronavirus updates for ophthalmologists, 2020. Available: https://www.aao.org/headline/alert-important-coronavirus-context [Accessed 25 May 2020].
- 20.The Royal College of Ophthalmologists - Medical Retinal Management Plan during COVID-19. Available: https://www.rcophth.ac.uk/wp-content/uploads/2020/03/Medical-Retinal-Management-Plan-during-COVID-19-UPDATED-300320-1-3.pdf [Accessed 25 May 2020].
- 21.Amtliches Dashboard COVID19. Available: https://info.gesundheitsministerium.at/dashboard.html?l=en [Accessed 25 May 2020].
- 22.Bressler NM, Beaulieu WT, Glassman AR, et al. . Persistent macular thickening following Intravitreous aflibercept, bevacizumab, or ranibizumab for Central-Involved diabetic macular edema with vision impairment: a secondary analysis of a randomized clinical trial. JAMA Ophthalmol 2018;136:257–69. 10.1001/jamaophthalmol.2017.6565 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Schmidt-Erfurth U, Lang GE, Holz FG, et al. . Three-Year outcomes of individualized ranibizumab treatment in patients with diabetic macular edema: the restore extension study. Ophthalmology 2014;121:1045–53. 10.1016/j.ophtha.2013.11.041 [DOI] [PubMed] [Google Scholar]
- 24.Zach K. Coronavirus: Ausbruch in vier Wiener Pensionistenheimen. kurier.at, 2020. Available: https://kurier.at/chronik/wien/coronavirus-ausbruch-in-vier-wiener-pensionistenheimen/400792283 [Accessed 25 May 2020].
- 25.Mobile clinics and home visits for optimal retinal care in Israel - EuroTimes, 2020. Available: https://www.eurotimes.org/mobile-clinics-and-home-visits-for-optimal-retinal-care-in-israel/ [Accessed 25 May 2020].
- 26.Thanh Le T, Andreadakis Z, Kumar A, et al. . The COVID-19 vaccine development landscape. Nat Rev Drug Discov 2020;19:305–6. 10.1038/d41573-020-00073-5 [DOI] [PubMed] [Google Scholar]
- 27.BBC News Could there be a second wave? Available: https://www.bbc.com/news/av/52739484/coronavirus-could-there-be-a-second-wave [Accessed 25 May 2020].


