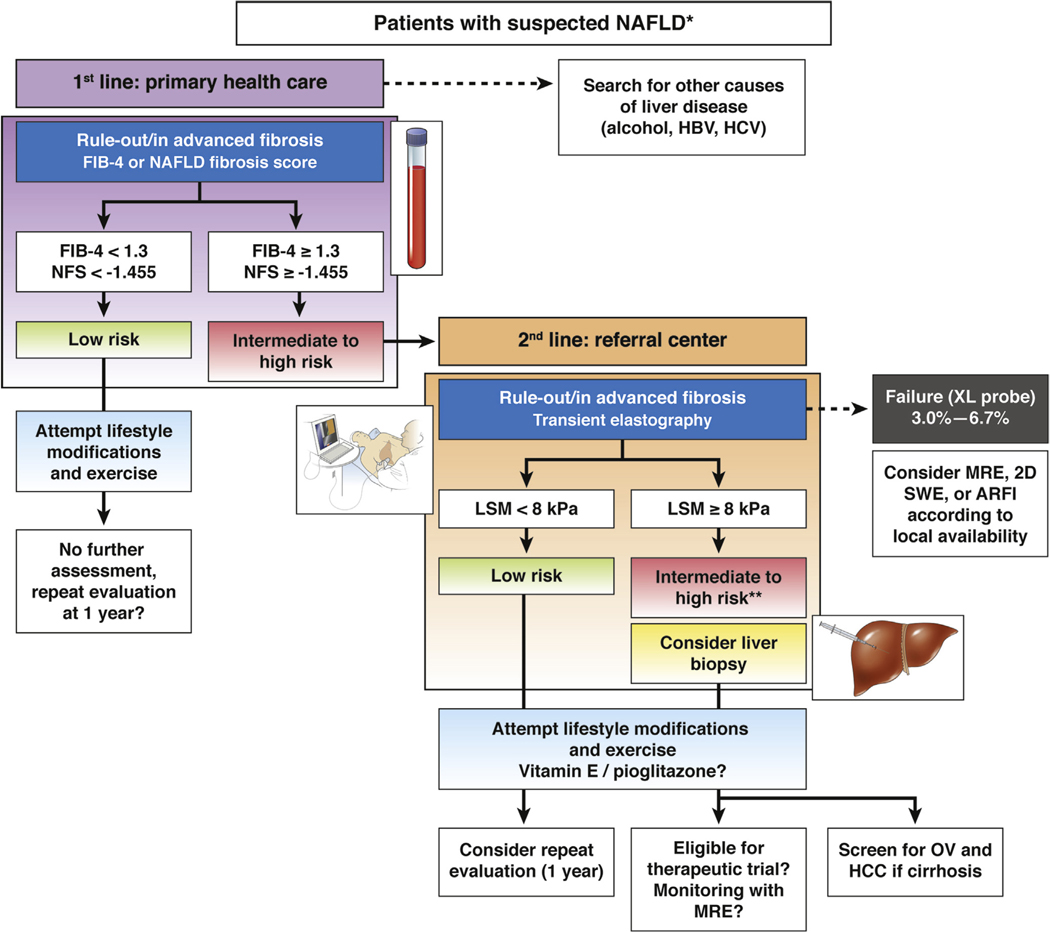
Figure 1.
A suggested algorithm for the use of noninvasive tests for risk stratification of patients with suspected NAFLD in clinical practice. *Suspicion of NAFLD is based on the presence of steatosis on ultrasound or abnormal liver tests (transaminases/γ-glutamyltransferase) in patients with risk factors (obesity, type 2 diabetes, or metabolic syndrome). Significant alcohol consumption and secondary causes of steatosis should be excluded. The proposed algorithm is based on expert opinion. The choice of noninvasive tools should be sequential, guided by local availability and the context of use: in primary health care setting, simple inexpensive and widely available serum biomarkers, such as FIB-4 or NFS, with high negative predictive value (88%−95%) for ruling out advanced fibrosis should be used as first-line. Patients with low risk (FIB-4 <1.3 or NAFLD Fibrosis score < −1.455; 55 to 58% of cases) do not need further assessment. They should be offered lifestyle modifications and exercise. Those with intermediate (FIB-4 = 1.3 to 3.25 or NFS = −1.455 to 0.672; 30% of cases) and high risk (FIB-4 >3.25 or NFS >0.672; 12%–15% of cases, positive predictive value 75%–90%) of having advanced fibrosis should be addressed to a referral center for LSM, using TE, in fasting condition, using M-probe for patients with skin-liver capsule distance <25 mm otherwise with the XL-probe. Patients at low risk of having advanced fibrosis (LSM <8 kPa; NPV 94%–100%) should be considered for a repeat evaluation within 1 year. Those with intermediate (LSM = 8–10 kPa) or high risk (LSM ≥10 kPa, PPV 47%–70%) of having advanced fibrosis should be considered for liver biopsy. However, confounders for liver stiffness should be carefully excluded to minimize the risk of false positive results. **Also patented serum biomarkers (FibroTest, Fibrometer, or ELF) could be considered in patients with intermediate risk according to local availability. In case of TE failure, alternative such as SWE/ARFI, MRE (particularly when BMI >35 kg/m2) may be considered according to local availability. In any case, all patients should be offered lifestyle modifications and exercise. As recommended by recent European Association for the Study of the Liver or American Association for the Study of Liver Diseases clinical practice guidelines, vitamin E (in non-diabetics) and pioglitazone may be considered in these patients. Also patients with cirrhosis should be screened for esophageal varices (OV) and hepatocellular carcinoma (HCC). In those with a liver biopsy, follow-up during treatment of LSM, using MRE, is the most promising noninvasive approach but requires further validation. NPV, negative predictive value; PPV, positive predictive value.