Background: A subset of patients with coronavirus disease 2019 (COVID-19) will develop acute respiratory distress syndrome and require mechanical ventilation. Studies suggest that many patients with COVID-19 and acute respiratory distress syndrome experience a cytokine storm characterized by fever; hyperferritinemia; and a massive release of inflammatory cytokines, including interleukin-6, tumor necrosis factor-α, and monocyte chemoattractant proteins (1). These findings led to the hypothesis that biological agents targeting specific cytokine or inflammatory pathways may improve the respiratory outcomes of patients with the most severe forms of COVID-19 (2).
Objective: To describe a patient with COVID-19 and overt hemophagocytic syndrome whose response to treatment was consistent with this hypothesis.
Case Report: A 51-year-old man who had received a kidney transplant was referred to our intensive care unit for cough, fever, and shortness of breath leading to the presumptive diagnosis of COVID-19. On day 1, acute respiratory failure required mechanical ventilation and prone positioning. Therapy with dexamethasone (5 mg twice daily), ceftriaxone (2 g/d), and spiramycin (1.5 million units 3 times daily) was initiated. Tacrolimus and mycophenolate mofetil were withdrawn. On day 2, the patient developed refractory multiorgan failure characterized by an inflammatory state, heart failure, stage 3 acute-on-chronic kidney injury, acute liver failure, nonregenerative anemia, thrombocytopenia, and lactic acidosis. The C-reactive protein level was 262 mg/L, and the ferritin level was 52 005 μg/L. We considered a diagnosis of hemophagocytic syndrome because the patient had underlying immunosuppression; fever of 39 °C; a serum ferritin level above 6000 μg/L; a hemoglobin level below 92 g/L; a platelet count below 110 × 109 cells/L; high levels of serum triglycerides; and aspartate aminotransferase with an HScore of 253, which indicated that the probability of having hemophagocytic syndrome was 99.5% (3). Bone marrow aspiration and liver biopsy confirmed the presence of hemophagocytosis (Figure). Polymerase chain reaction identified severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) in bronchoalveolar fluid (cycle threshold 21) and blood.
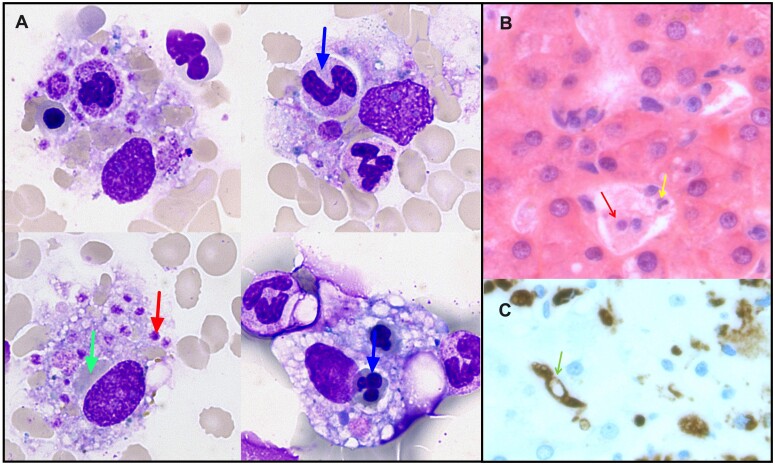
Figure.
Bone marrow and liver hemophagocytosis in a kidney transplant recipient with COVID-19.
COVID-19 = coronavirus disease 2019. A. Hemophagocytosis of polymorphonuclear neutrophils (yellow arrow), erythrocytes (green arrow), and platelets (red arrow) by activated macrophages in the bone marrow aspirate. May–Grünwald–Giemsa staining, original magnification × 1000. B. Kupffer cell hypertrophy and hyperplasia with hemophagocytosis of polymorphonuclear neutrophils (yellow arrow) and lymphocytes (red arrow) in the liver (hematoxylin–eosin staining). C. CD68 immunostaining of the liver biopsy (brown staining: activated macrophages with hemophagocytosis of erythrocytes [green arrow]).
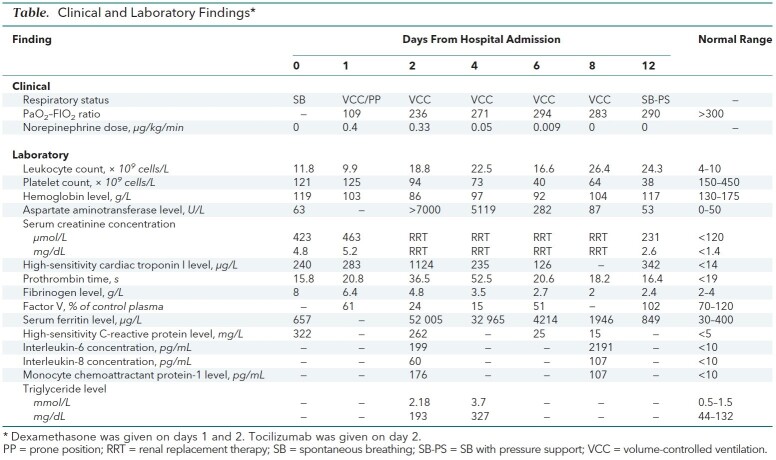
Given the salutary effects of interleukin-6 receptor inhibition in the treatment of secondary hemophagocytic syndromes (4) and chimeric antigen receptor T cell–related cytokine release syndromes (5), we treated the patient with tocilizumab (8 mg/kg intravenously, once) as salvage therapy, instead of etoposide, and we withdrew dexamethasone. Tocilizumab administration was followed by dramatic improvement of the respiratory, hemodynamic, and liver conditions and correction of the ferritin levels (Table). Three days after tocilizumab administration, we observed normalization of circulating levels of CD3- CD16+ CD56+ natural killer cells and effector CD8+ CD56+ and CD8+ CD57+ perforin-positive, granzyme-positive T cells.
Table. Clinical and Laboratory Findings*.
Discussion: In this report, we describe an immunocompromised patient with COVID-19 and a related hemophagocytic syndrome whom we treated with tocilizumab. The cytokine storm and multiorgan failure rapidly reversed, and the patient made a speedy recovery. On hospital day 30, the patient was breathing spontaneously with protective tracheotomy, and rehabilitation is ongoing. On the basis of this experience, we suggest that clinicians who have similar patients consider using drugs that inhibit interleukin-6 to treat these patients while waiting for the results of the randomized controlled trials that are now evaluating tocilizumab in patients with COVID-19 and respiratory failure.
Biography
Acknowledgment: The authors thank Dr. Emmanuel Treiner, Prof. Jacques Izopet, Dr. François Vergez, and Prof. Jannick Selves for their help in obtaining accurate immunology, pathology, and virology analyses in the context of the COVID-19 crisis.
Disclosures: Disclosures can be viewed at www.acponline.org/authors/icmje/ConflictOfInterestForms.do?msNum=L20-0419.
Corresponding Author: Stanislas Faguer, MD, PhD, Département de Néphrologie et Transplantation d'organes, Unité de Réanimation, INSERM U1048 (équipe 12, I2MC), Hôpital Rangueil, 1, avenue Jean Poulhes, 31059 Toulouse Cedex, France; e-mail, faguer.s@chu-toulouse.fr.
Footnotes
This article was published at Annals.org on 18 May 2020.
References
- 1. doi: 10.1016/S0140-6736(20)30183-5. Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497-506. [PMID: 31986264] doi:10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed]
- 2. doi: 10.1016/j.ijantimicag.2020.105954. Zhang C, Wu Z, Li JW, et al. The cytokine release syndrome (CRS) of severe COVID-19 and interleukin-6 receptor (IL-6R) antagonist tocilizumab may be the key to reduce the mortality. Int J Antimicrob Agents. 2020:105954. [PMID: 32234467] doi:10.1016/j.ijantimicag.2020.105954. [DOI] [PMC free article] [PubMed]
- 3. doi: 10.1002/art.38690. Fardet L, Galicier L, Lambotte O, et al. Development and validation of the HScore, a score for the diagnosis of reactive hemophagocytic syndrome. Arthritis Rheumatol. 2014;66:2613-20. [PMID: 24782338] doi:10.1002/art.38690. [DOI] [PubMed]
- 4. doi: 10.1002/hon.2174. Faguer S, Vergez F, Peres M, et al. Tocilizumab added to conventional therapy reverses both the cytokine profile and CD8+Granzyme+ T-cells/NK cells expansion in refractory hemophagocytic lymphohistiocytosis [Letter]. Hematol Oncol. 2016;34:55-7. [PMID: 25312407] doi:10.1002/hon.2174. [DOI] [PubMed]
- 5. doi: 10.1097/CCM.0000000000002053. Fitzgerald JC, Weiss SL, Maude SL, et al. Cytokine release syndrome after chimeric antigen receptor T cell therapy for acute lymphoblastic leukemia. Crit Care Med. 2017;45:e124-e131. [PMID: 27632680] doi:10.1097/CCM.0000000000002053. [DOI] [PMC free article] [PubMed]