Abstract
Objective
To review the available literature concerning the effectiveness of the COVID-19 diagnostic tools.
Background
With the absence of specific treatment/vaccines for the coronavirus COVID-19, the most appropriate approach to control this infection is to quarantine people and isolate symptomatic people and suspected or infected cases. Although real-time reverse transcription-polymerase chain reaction (RT-PCR) assay is considered the first tool to make a definitive diagnosis of COVID-19 disease, the high false negative rate, low sensitivity, limited supplies and strict requirements for laboratory settings might delay accurate diagnosis. Computed tomography (CT) has been reported as an important tool to identify and investigate suspected patients with COVID-19 disease at early stage.
Key findings
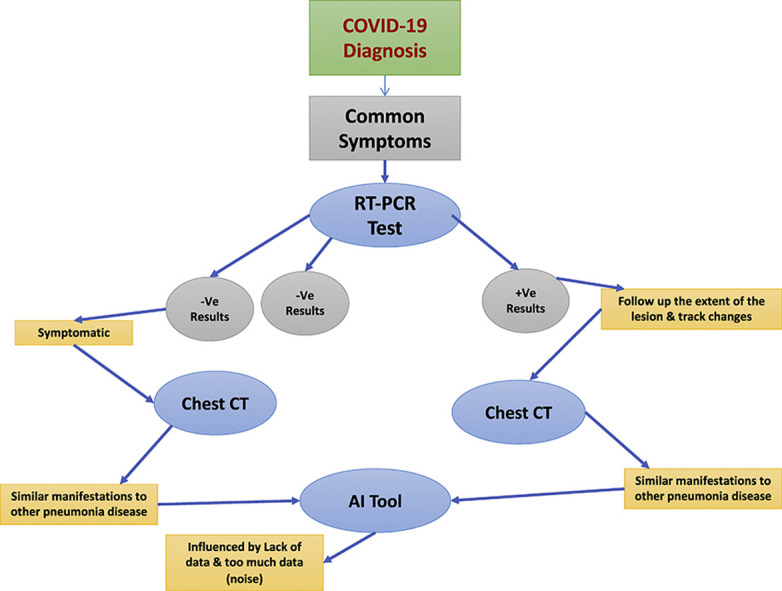
RT-PCR shows low sensitivity (60–71%) in diagnosing patients with COVID-19 infection compared to the CT chest. Several studies reported that chest CT scans show typical imaging features in all patients with COVID-19. This high sensitivity and initial presentation in CT chest can be helpful in rectifying false negative results obtained from RT-PCR. As COVID-19 has similar manifestations to other pneumonia diseases, artificial intelligence (AI) might help radiologists to differentiate COVID-19 from other pneumonia diseases.
Conclusion
Although CT scan is a powerful tool in COVID-19 diagnosis, it is not sufficient to detect COVID-19 alone due to the low specificity (25%), and challenges that radiologists might face in differentiating COVID-19 from other viral pneumonia on chest CT scans. AI might help radiologists to differentiate COVID-19 from other pneumonia diseases.
Implication for practice
Both RT-PCR and CT tests together would increase sensitivity and improve quarantine efficacy, an impact neither could achieve alone.
Keywords: CT scan, RT-PCR, Ground-glass opacification, Consolidation, Crazy-paving, Artificial intelligence
Graphical abstract
Introduction
Cases of an unidentified form of viral pneumonia were first reported in Wuhan city, Hubei province, China, in December 2019.1 In the following weeks, this unknown virus gradually spread across the whole world.2 On January 7, 2020, a scientific research institution in China announced that the viral pneumonia was a novel coronavirus (SARS-COV-2), later it was called COVID-19 by the World Health Organization (WHO).3 According to Worldometer (2020), as of August 31, 2020, there had been 25,416,807 confirmed cases, 851,102 reported deaths and 17,724,602 recovered individuals across the world.4
The mortality rate of COVID-19 is lower than that of the coronaviruses severe acute respiratory syndrome (SARS) and Middle East respiratory syndrome (MERS).5, 6, 7 However, COVID-19 is highly transmissible and rapidly spread, as it can be transmitted by respiratory droplets and contact. The common symptoms observed in patients with COVID-19 are fever, cough, severe headache, myalgia and fatigue.8, 9, 10 However, infection by other viruses such as influenza A or B can cause similar symptoms to COVID-19, which may make it difficult to distinguish COVID-19 from other infections, especially during flu season.11 The incubation period for COVID-19 infection is typically 1–14 days and might extend up to 24 days.12, 13, 14 The health conditions of most COVID-19 patients are mild, but they can become severe, especially among elderly people or those with underlying diseases, such as chronic lung or cardiovascular disease.15, 16, 17, 18, 19 To date, there is no evidence of any effective treatment for patients with COVID-19.16 Due to the lack of specific vaccines and drugs for COVID-19, it is essential to detect and manage the disease at an early stage to immediately isolate people who are confirmed to be infected with COVID-19 from healthy people.19, 20, 21, 22, 23, 24
According to the guidelines for the diagnosis of COVID-19 published by the Chinese government, real-time reverse transcription-polymerase chain reaction (RT-PCR) assay is considered the first tool in COVID-19 diagnosis.25 However, delayed sample collection, poor kit performance, limited supplies and strict requirements for laboratory settings might delay accurate diagnosis.21, 22, 23, 24, 25, 26 This indicates that patients with COVID-19 may not be detected and receive appropriate treatment, which could increase the risk of spread of the infection among a larger population.27 It is not about the test itself; it is often about when and how the test samples are collected from infected people, and whether these samples are prepared and transported properly.28
Diagnostic imaging such as computed tomography (CT) has played an important role in the diagnosis and management of patients with COVID-19.29 , 30 CT of the chest is a routine scanning technique for pneumonia diagnosis. It can be used for the diagnosis of COVID-19, as well as to follow up the extent of lesions and track any changes in patients whose RT-PCR assays and plain radiographic images were negative.20 , 31, 32, 33 Several studies reported that a CT of the chest shows typical imaging features in nearly all patients with COVID-19.11 , 34, 35, 36 Hung et al. and Xie et al. (2020) highlight that similar imaging features were also detected in patients whose RT-PCR assays were negative.1 , 37
Artificial intelligence (AI), an emerging technology in the field of diagnostic imaging, has contributed to improving diagnosis and prognosis of several diseases, such as pneumonia.38 A research team showed the potential of AI in supporting the diagnosis of COVID-19 in patients with COVID-19 when trained on CT images, achieving a high sensitivity and specificity (90%).39 , 40 By conducting a comprehensive review of published studies and the experience of diagnosing patients with coronavirus, the aim of this article is to review the effectiveness of the available COVID-19 diagnostic tools.
RT-PCR assay and CT scans in the diagnosis of COVID-19
The standard method of COVID test is RT-PCR, and the test sample can be collected via nasopharyngeal swab or oropharyngeal swab.41, 42, 43 The RT-PCR is a genetic test combining reverse transcription of Ribonucleic acid (RNA) into complementary Deoxyribonucleic acid (DNA), and amplification of specific DNA targets using RT-PCR.44 Although the RT-PCR test remains the reference standard in making a definitive diagnosis of COVID-19 infection,45 , 46 this test has rigorous laboratory specifications and takes a long time to report results.30 , 37 Several studies found that the initial RT-PCR results for patients with COVID-19 infection were false-negatives.1 , 37 These false-negative findings cannot be ignored, especially for those symptomatic people suspected to be infected with COVID-19.
CT scans of the chest are used as a routine test to diagnose pneumonia; therefore, this may be useful in diagnosing COVID-19.21 , 47 Unenhanced high resolution CT (HRCT) of the chest is acquired during a single breath-hold. CT images are then reconstructed and transmitted for subsequent interpretation and diagnosis.48 Ai et al. (2020) conducted a study to evaluate the value and consistency of chest CT scans in the diagnosis of COVID-19 and found that the majority of patients (98%, n = 56/57) had initial positive chest CT scans before or within six days of the initial positive RT-PCR findings.21 This is in line with other studies; they found that positive diagnoses of COVID-19 were available three days earlier with chest CT scans than with RT-PCR assay.30, 31, 32, 33, 34, 35, 36, 37 This indicates that chest CT scans can play a role in rapidly detecting the infection at an early stage.
Several studies have reported that chest CT scans show typical radiographic features in all patients with COVID-19.1 , 37 , 49 The National Health Commission of China reported that chest CT is of a great value in diagnosing COVID-19, monitoring disease progression and evaluating treatment plans.25 Lee et al. (2020) claim that most of the clinics in China currently prefer to use CT compared to other investigation tools. This preference might stem from the accessibility of CT units in China, CT's ability to diagnose patients at an early stage, concerns associated with other tests specificity and the lack of virus-testing kits.50 However, the American College of Radiology (ACR) is against the use of chest CT as a first-line investigation tool to diagnose patients with suspected COVID-19 disease.51 This might be due to the low specificity of CT in differentiating COVID-19 from other similar illnesses. Similarly the Royal College of Radiologists (RCR) stated that CT does have a well-established role in the assessment of patients presenting with severe respiratory distress, particularly those that deteriorate clinically. However, they confirmed that CT should not be used as a diagnostic assessment of patients with suspected coronavirus infection.52 Further challenges related to hygiene may also be another reason for not considering CT as a sole diagnostic tool for patients with COVID-19. This includes managing ventilation, airflow, and sanitising and cleaning the scanner rooms in radiology departments.25 , 53
Recent studies have revealed that RT-PCR has low sensitivity (60–71%) in diagnosing patients with COVID-19 infection compared to the CT chest.37 , 54 , 55 Fang et al. (2020) referred to the high sensitivity of CT chest (98%) compared to that of RT-PCR tests (71%).55 This is in line with the findings of Xie et al. (2020), who evaluated 167 patients and found that 3% (n = 5) of the patients showed initially negative RT-PCR nasopharyngeal and/or throat swabs but simultaneously showed positive results in chest CT scans.37 This finding was supported by Huang et al. (2020), who found that a laboratory test showed a normal white blood cells count with a negative RT-PCR assay; however, a chest CT scan showed multiple peripheral ground-glass opacities (GGO) in the lingual segments.1 Such false-negative results may be attributed to the low viral load in test samples and/or laboratory errors,37 , 55 and it might be necessary to retest the patient. However, test kits are in short supply or are unavailable in some places.54 Therefore, some hospitals have started to use chest CT scans as a primary tool to diagnose COVID-19, though the ACR advises radiographers and radiologists to apply extreme precaution in this practice.51
In a study by Xie et al. (2020), it was found that all patients presented characteristic CT image features of COVID-19 at an early stage, including GGO and/or mixed GGO and mixed consolidation, confirmed by positive RT-PCR assay during the isolation period.37 Shi et al. (2020) highlighted that symptomatic patients might show changes in chest CT scans prior to obvious symptom onset.56 Shi and colleagues indicated that following up with chest CT scans might aid the continuous monitoring of disease changes during treatment.56 In their study, Wu et al. (2020) found that most of the patients had mild symptoms and high temperatures; however, the lung manifestations on their chest CT scans were serious. They highlighted the role of chest CT scans in evaluating the severity of COVID-19 infection.57
In contrast, Guan et al. (2020) and Chuang et al. (2020) respectively found that 20% (n = 230/1099) and 14% (n = 3/21) of patients with clinical symptoms and positive RT-PCR findings had normal chest CT findings.8 , 20 Similar results were found by Yang et al. (2020).46 Although chest CT scans can show higher sensitivity in COVID-19 diagnosis than RT-PCR assay, Pan et al. (2020) and Fang et al. (2020) refer to the low specificity of chest CT scans.55 , 58 This is reinforced by Ai et al. (2020), who found that chest CT scans had low specificity (25%) in a recent study of 1,014 patients with COVID-19.21 This may stem from the difficulties that radiologists face in distinguishing between COVID-19 and other diseases on chest CT scans. Additionally, Li and Xia (2020) found that two patients confirmed to be infected with COVID-19 did not have CT features typical of COVID-19.30, 31, 32, 33, 34, 35, 36, 37 This indicates that the differential diagnosis of COVID-19 should be considered when patients present with a fever and cough of unknown origin. It was also advised that all radiologists should familiarise themselves with the typical COVID-19 findings on chest CT scans.45 , 54 Furthermore, radiologists should pay attention while interpreting CT images and be able to differentiate the features of patients with COVID-19 from motion artefacts as some of these patients may face difficulties in following the breathing instructions during CT scans.30 The above studies may suggest that chest CT imaging alone is not sufficient to exclude the diagnosis of COVID-19. Therefore, early chest CT scans combined with other investigation tools, such as RT-PCR assay, may still be required.
Features of COVID-19 in CT imaging
During the early stages of COVID-19 infection, chest x-rays may not be sensitive enough to detect these changes.59 , 60 CT on the other hand, has better sensitivity for the detection of early or mild disease.20 , 62 Focusing on the many faces of COVID-19 for better recognition and accurate diagnosis is always recommended.60 , 62 Below, typical and relatively atypical CT manifestations of COVID-19 will be reviewed to identify the potential imaging features of COVID-19.
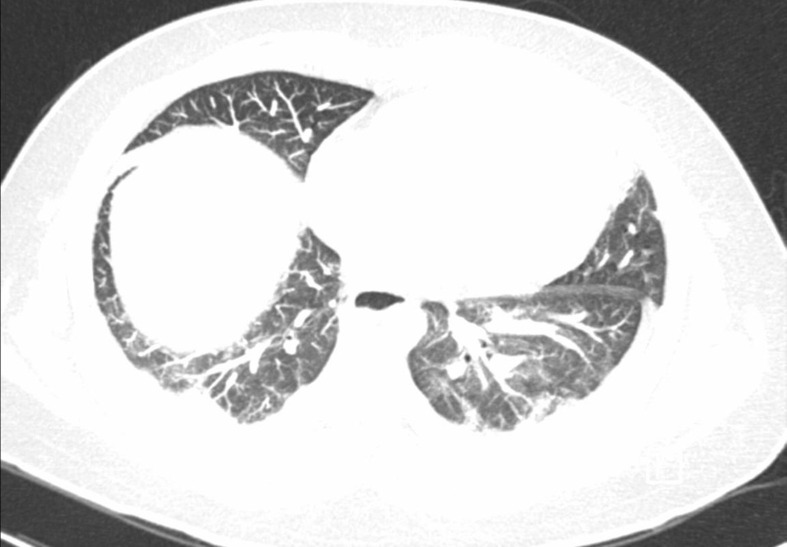
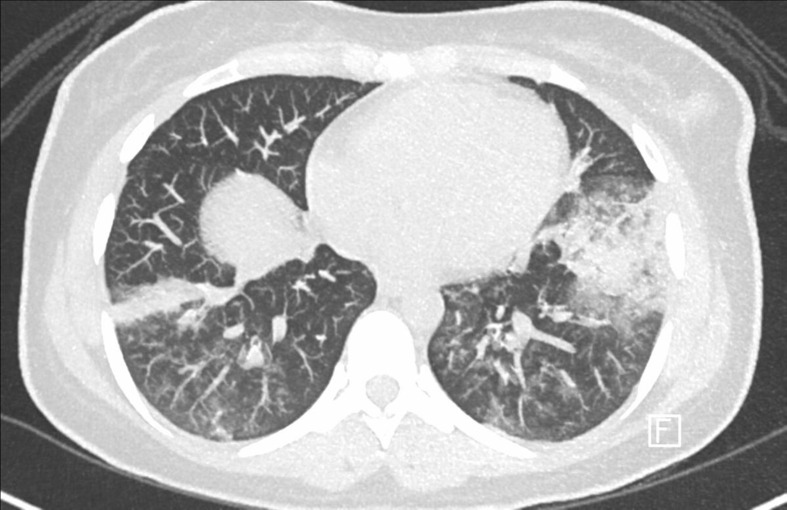
GGO is the most common feature.29 , 49 , 63 It is a hazy increase in attenuation that appears in a variety of interstitial and alveolar processes with preservation of the bronchial and vascular margins.64 Consolidation is another typical feature of COVID-19, which is an area of opacification obscuring the margins of vessels and airway walls.57 , 65 GGO with single or multiple focal lesions with or without consolidation in the posterior and peripheral lung segments that are distributed bilaterally is a common feature (Figure 1, Figure 2 ). GGO with reticular or interlobular septal thickening in a typical ‘crazy-paving’ pattern is often observed, while pure consolidation is relatively less common.58, 59, 60 , 65 A recent study showed that the most frequent CT abnormalities observed in patients with COVID-19 were GGO (73/80 cases, 91%), consolidation (50/80 cases, 63%) and interlobular septal thickening (47/80, 59%). Most of the patients had multiple lesions, with an average of 12 ± 6 lung segments involved.57
Figure 1.
Lower bilateral peripheral consolidations and ground-glass opacities in keeping with the clinical diagnosis of clinical history provided of COVID-19.
Figure 2.
Bilateral mainly basilar peripheral patchy consolidative opacities associated with bilateral basilar ill-defined ground-glass opacities.
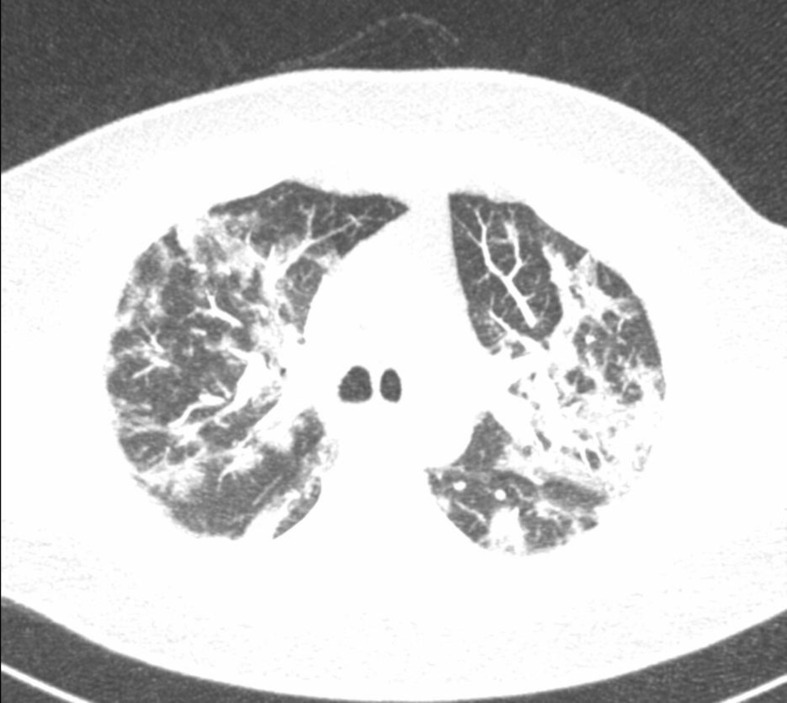
CT imaging features of COVID-19 can differ in various stages and patients.66 In an early phase, GGO with single or multiple lesions can be found along the sub-pleural areas or bronchi.11 These lesions have nodular or patchy appearance, with thickened blood vessels passing through the GGO. Thickened interlobular and interlobular septa along with halo signs are also seen.67 As per published studies, the percentage of this finding occurrence ranges between 14 and 98% (Fig. 3 ).67 , 68 However, this range significantly increases in the short-term re-examination, where more denser lesions can be seen.58 Consequently, crazy paving appearance may be noticed due to the lobular septal thickening and reflecting interstitial lesions.67
Figure 3.
Upper and lower lobe coalescent patchy perilobular ground-glass airspace opacities.
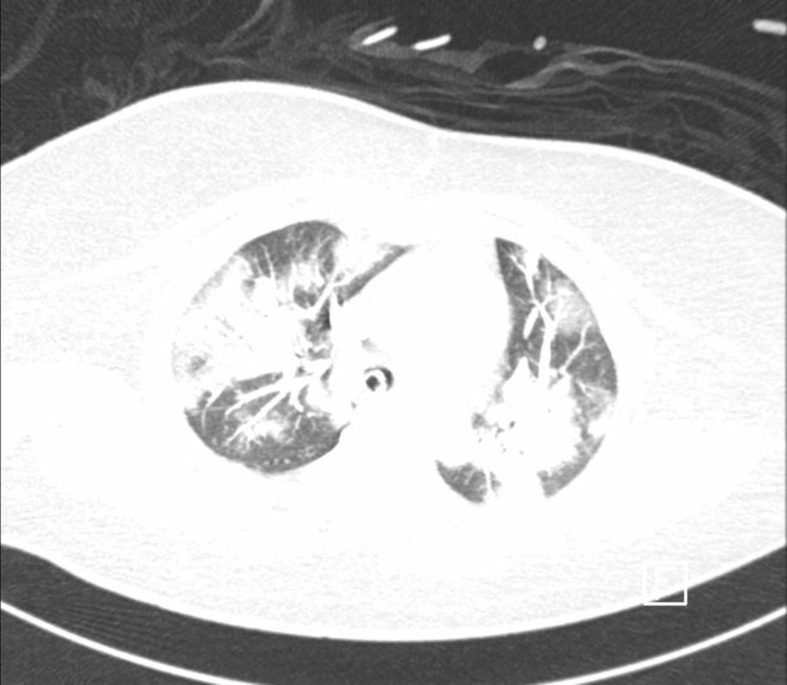
In severe patients, bilateral multifocal consolidation can be seen, partially fused into massive consolidation with small pleural effusions and even presenting with ‘white lung’.59 Two weeks after onset, lung involvement has been shown to gradually increase to consolidation.61 Within 1–3 weeks, this GGO could progress to or co-exist with consolidations.56 With a longer time interval, more consolidative lesions can be seen between symptom onset and the CT scan, especially in patients older than 50 years old,65 suggesting that this feature can be used as an alert in patient management.66 After 3–14 days of re-examination and as the disease progresses, an increase in the range of GGO patches and consolidation can be observed (Fig. 4 ). The middle and lower lung regions and the posterior lung area are where this progression is mainly distributed.11 , 61 Patients may have single-lobe or multiple-lobe involvement. A study by Y. Pan et al. (2020) found that 30.2% and 44.4% of patients had only one lobe involved and all lobes involved, respectively. ‘White lung’ is when diffused lesions are seen in the lungs and their density increases significantly. White lung indicates that the patient's condition has worsened because it seriously affects the lung function.61
Figure 4.
Multifocal bilateral airspace opacities that are more consolidation than ground glass and patchy peripheral distribution, which is related to patient's laboratory proven COVID-19.
It is worth noting that several other CT imaging features can also be observed as the number of COVID-19 cases increases, including air bronchogram, airway and pleural changes, fibrosis, vascular enlargement, air bubble signs, nodules, halo signs, lymphadenopathy, and pericardial effusion.66 The percentages of these manifestations occurrence vary widely, therefore, radiologists should be aware while interpreting the CT images for COVID-19 patients to avoid misdiagnosis with typical viral pneumonia and should always link between symptoms and CT features.
Artificial intelligence (AI) combined with CT imaging in COVID-19 diagnosis
Recently, notable advancements have been made in using AI in the diagnostic imaging field.69, 70, 71, 72, 73, 74 Ardila et al. (2019) highlighted that AI can exceed the performance of human experts in medical imaging diagnosis.75 A few studies in the literature have examined the use of AI in COVID-19 diagnosis, although most of them are preprint version of scientific articles that have not been peer-reviewed, thus highlighting the need for further investigation. Kermany et al. (2018) and Rajaraman et al. (2018) referred to the use of AI (deep learning) in detecting bacterial and viral pneumonia in the chest.76 , 77 Two years later, a deep learning (DL) system was developed by Shan et al. (2020), and they found that with the DL the percentage of infection (POI) of lung lobes and bronchopulmonary segments can be automatically calculated and were clinically relevant with the severity of pneumonia. They highlighted the importance of this system in quantifying the changes in the follow-up CT scans of COVID-19 patients and evaluating how the infection progresses under different forms of clinical management.78 This was reinforced by Wang et al. (2020), who used a DL approach to extract the imaging features for COVID-19. They found that the sensitivity and specificity of this method were 74% and 67% respectively.29 However, a common weakness of the above studies was the relatively low number of collected CT images from patients, which may not be representative of all COVID-19 patients. A further study was conducted by Li et al. (2020), who collected 4,536 CT images, and designed and evaluated a three-dimensional (3D) deep learning model to diagnose COVID-19 infections in chest CT scans. This model showed high sensitivity (90%) and specificity (96%) in detecting COVID-19.79
Jin et al. (2020) conducted a large-scale study (n = 756) subjects, 496 COVID-19 positives and 260 negatives to compare the diagnostic performance of an AI system with that of five radiologists. It was found that the AI system achieved high sensitivity (94%), specificity (95.47%) and diagnostic accuracy, which was comparable to that of experienced radiologists (94.7% sensitivity).69 This parallels with the findings of Chen et al. (2020), who found similar performance between a COVID-19 diagnosis system and an expert radiologist; however, it is important to note that the AI system in this study was validated based upon a small dataset (n = 19 confirmed COVID-19 patients) and one radiologist.80 It was found that high classification results were achieved for coronavirus versus non-coronavirus patients with 98.2% sensitivity and 92.2% specificity.81 A similar result was reported by Xu et al. (2020); however, it is interesting to note that the diagnostic certainty of the AI system was evaluated by creating confidence scores of these forecasts.82 A deep learning approach can assist radiologists in diagnosing COVID-19 and can automatically extract lesions within CT images, as indicated by Song et al. (2020) and Bai et al. (2020).65 , 83, 84, 85, 86 Bai et al. (2020) indicated that the DL tool achieved a prediction area under curve (AUC) of 0·938 by combining the clinical data and the CT data.83
AI systems, especially deep learning, have been proposed to process and analyse medical imaging data such as chest CT to assist radiologists and physicians to improve diagnosis performance. The AI offers radiologists an opportunity to save time and maximise productivity especially when required to examine a lot of cases.87 Bai et al. (2020) assessed the performance of radiologists in differentiating COVID-19 from other viral pneumonia on chest CT.88 It was found that radiologists achieved high specificity and moderate sensitivity in distinguishing COVID-19 from other viral pneumonia on chest CT. A further interesting study was conducted by Bai et al. (2020) to assess radiologists' performance with and without AI assistance in distinguishing coronavirus versus non-coronavirus patients. The authors found that radiologists attained a higher accuracy (90%), sensitivity (88%) and specificity (91%) with AI assistance.89 This suggests the potential role for the AI system to improve radiologists' routine workflow and diagnostic outcomes related to COVID-19. It is worth noting that all the above studies were retrospective, and prospective studies might be required to further validate AI system in real time to assist physicians’ diagnosis.
As can be seen, AI systems can be used in conjunction with chest CT images and patient history (age, gender, clinical information, blood test, symptoms and possible contact with infected people) to improve the detection of the infection. The AI systems helps to segment the exact infected area of the patient's lung from the chest CT and quantify the volume with respect to the total volume of the lung.28 This information might guide the physician in decision-making related to treatment options. The AI system can offer a second opinion to the physician in patients who had normal chest CT or those showing non-specific findings, in order to achieve high sensitivity, specificity and accuracy in COVID-19 diagnosis and management.
The above studies indicate that AI systems could be used to screen and diagnose quickly a great volume of patients with suspected COVID-19, which could lead to accurate discrimination between bacterial pneumonia and viral pneumonia (COVID-19) and decrease unnecessary delays. However, radiologists who are not familiar with such systems may face challenges in getting used to them, which might be problematic because COVID-19 is spreading rapidly. In addition, as most deep learning systems require experts to annotate the lesions in the CT images for disease detection, this will require time and effort from radiologists, which might be considered a big challenge due to the current radiologist shortages in some countries.90 Naude (2020) indicate that the use of AI systems are impeded by a lack of data, and by too much data. These limitations require a careful balance between data privacy and public health, and rigorous human–AI interface. It is unlikely that these will be tackled in the current time; more diagnostic data needs to be gathered to train AI and save lives.40 The topic of the role of AI in the diagnosis and management of COVID-19 remains open for further investigation.
Conclusion
This review of the available literature on COVID-19 provides insights into the value of CT scan in diagnosing and controlling this infection. Although in some studies chest CT scans have shown high sensitivity in diagnosing COVID-19 compared to RT-PCR tests, chest CT scans alone are not sufficient to detect COVID-19 and can be useful complement to other tools for diagnosing patients with COVID-19 and tracking their prognosis. CT scans can be used as a staging tool to assess the complications of COVID-19 on patients' lungs. The CT findings for patients with COVID-19 show that the infection has mixed and diverse features. The presence of GGO with single or multiple lesions suggests that the disease is in an early stage, while bilateral multifocal consolidation can be seen in an advanced stage. As COVID-19 has similar manifestations to other pneumonia diseases, several AI systems have been proposed and developed in order to differentiate COVID-19 from other pneumonia diseases.
Conflict of interest statement
No conflict of interest.
References
- 1.Huang P., Liu T., Huang L., Liu H., Lei M., Xu W., et al. Use of chest CT in combination with negative RT-PCR assay for the 2019 novel coronavirus but high clinical suspicion. Radiology. 2020 Apr;295(1):22–23. doi: 10.1148/radiol.2020200330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Phan L., Nguyen T., Luong Q., Nguyen T., Nguyen H., Le H.Q., et al. Importation and human-to-human transmission of a novel coronavirus in Vietnam. N EngI J Med. 2020 Feb 27;382(9):872–874. doi: 10.1056/NEJMc2001272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.World Health Organisation (WHO) Coronavirus disease 2019 (COVID-19) Situation Report – 28. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200217-sitrep-28-covid-19.pdf?sfvrsn=a19cf2ad_2 Available from:
- 4.World Meter Corona Virus Update (Live) https://www.worldometers.info/coronavirus/ Available from:
- 5.Guarner J. Three emerging coronaviruses in two decades: the story of SARS, MERS, and now COVID-19. Clin Infect Dis. 2020;153(4):420–421. doi: 10.1093/ajcp/aqaa029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rajgor D., Lee M., Archuleta S., Bagdasarian N., Quek S. The many estimates of the COVID-19 case fatality rate. Lancet Infect Dis. 2020 doi: 10.1016/S1473-3099(20)30244-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sun Q., Qiu H., Huang M., Yang Y. Lower mortality of COVID-19 by early recognition and intervention: experience from Jiangsu Province. Ann Intensive Care. 2020;10(1):1–4. doi: 10.1186/s13613-020-00650-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chen H., Guo J., Wang C., Luo F., Yu X., Zhang W., et al. Clinical characteristics and intrauterine vertical transmission potential of COVID-19 infection in nine pregnant women: a retrospective review of medical records. Lancet. 2020;395(10226):809–815. doi: 10.1016/S0140-6736(20)30360-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Singhal T. A review of coronavirus disease-2019 (COVID-19) Indian J Pediatr. 2020;87(4):281–286. doi: 10.1007/s12098-020-03263-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tian S., Hu N., Lou J., et al. Characteristics of COVID-19 infection in Beijing. J Infect Dis. 2020;80(4):401–404. doi: 10.1016/j.jinf.2020.02.018. 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zhao W., Zhong Z., Xie X., Yu Q., Liu J. Relation between chest CT findings and clinical conditions of coronavirus disease (COVID-19) pneumonia: a multicenter study. AJR. 2020;214(5):1072–1077. doi: 10.2214/AJR.20.22976. [DOI] [PubMed] [Google Scholar]
- 12.Hui D., Azhar E., Madani T., Ntoumi F., Kock R., Dar O., et al. The continuing 2019-nCOVID epidemic threat of novel coronaviruses to global health-The latest 2019 novel coronavirus outbreak in Wuhan, China. J Infect. 2020;91(2020):264–266. doi: 10.1016/j.ijid.2020.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lauer S., Grantz K., Bi Q., Jones F., Zheng Q., Meredith H., et al. The incubation period of coronavirus disease 2019 (COVID-19) from publicly reported confirmed cases: estimation and application. Ann Intern Med. 2020;172(9):577–582. doi: 10.7326/M20-0504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lei S., Jiang F., Su W., Chen C., Chen J., Mei W., et al. Clinical characteristics and outcomes of patients undergoing surgeries during the incubation period of COVID-19 infection. EClinicalMedicine. 2020;54(8):2–3. doi: 10.1016/j.eclinm.2020.100331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gardner W., States D., Bagley N. The coronavirus and the risks to the elderly in long-term care. J Soc Policy. 2020;10(1080):1–6. doi: 10.1080/08959420.2020.1750543. [DOI] [PubMed] [Google Scholar]
- 16.Ioannidis J., Axfors C., Contopoulos-Ioannidis D. Population-level COVID-19 mortality risk for non-elderly individuals overall and for non-elderly individuals without underlying diseases in pandemic epicenters. medRxiv. 2020 doi: 10.1101/2020.04.05.20054361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Armitage R., Nellums L. COVID-19 and the consequences of isolating the elderly. Lancet Public Health. 2020;5(5):256–261. doi: 10.1016/S2468-2667(20)30061-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kliger A., Silberzweig J. Mitigating risk of COVID-19 in dialysis facilities. Clin J Am Soc Nephrol. 2020;15(5):707–709. doi: 10.2215/CJN.03340320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pascarella G., Strumia A., Piliego C., Bruno F., Buono R., Costa F., et al. COVID-19 diagnosis and management: a comprehensive review. J Intern Med. 2020 doi: 10.1111/joim.13091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Guan W., Ni Z., Hu Y., Liang W., Ou C., He J., et al. Clinical characteristics of 2019 novel coronavirus infection in China. medRxiv. 2020 doi: 10.1101/2020.02.06.20020974. [DOI] [Google Scholar]
- 21.Ai T., Yang Z., Hou H., Zhan C., Chen C., Lv W., et al. Correlation of chest CT and RT-PCR testing in coronavirus disease 2019 (COVID-19) in China: a report of 1014 cases. Radiology. 2020 doi: 10.1148/radiol.2020200642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Yang Y., Yang M., Shen C., Wang F., Yuan J., Li J., et al. Evaluating the accuracy of different respiratory specimens in the laboratory diagnosis and monitoring the viral shedding of 2019-nCoV infections. medRxiv. 2020 doi: 10.1101/2020.02.11.20021493. [DOI] [Google Scholar]
- 23.Jin Y., Yang H., Ji W., Wu W., Chen S., Zhang W., et al. Virology, epidemiology, pathogenesis, and control of COVID-19. Viruses. 2020;12(4):372–388. doi: 10.3390/v12040372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Alanagreh L., Alzoughool F., Atoum M. The human coronavirus disease COVID-19: its origin, characteristics, and insights into potential drugs and its mechanisms. Pathogens. 2020;9(5):33–41. doi: 10.3390/pathogens9050331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Chinese government The diagnostic and treatment protocol of COVID-19. http://www.gov.cn/zhengce/zhengceku/2020-02/19/content_5480948.htm Available from:
- 26.Wang X., Tan L., Wang X., Lu Y., Cheng L., Sun Z., et al. Comparison of nasopharyngeal and oropharyngeal swabs for SARS-CoV-2 detection in 353 patients received tests with both specimens simultaneously. Int J Infect Dis. 2020;94(2020):107–109. doi: 10.1016/j.ijid.2020.04.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Esposito A., Palmisano A., Scotti G., Morelli M., Vignale D., Cobelli F., et al. Why is chest CT important for early diagnosis of COVID-19? Prevalence matters. medRxiv. 2020 doi: 10.1101/2020.03.30.20047985. [DOI] [Google Scholar]
- 28.King Abdullah university of science and technology (KAUST) Using AI to understand the pathogenesis of COVID-19. https://www.kaust.edu.sa/en/news/using-ai-to-understand-the-pathogenesis-of-covid-19 Available from:
- 29.Wang S., Kang B., Ma J., Zeng X., Xiao M., Guo J., et al. A deep learning algorithm using CT images to screen for Corona Virus Disease (COVID-19) medRxiv. 2020 doi: 10.1101/2020.02.14.20023028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Li Y., Xia L. Coronavirus Disease 2019 (COVID-19): role of chest CT in diagnosis and management. AJR. 2020;214(6):1280–1286. doi: 10.2214/AJR.20.22954. [DOI] [PubMed] [Google Scholar]
- 31.Bai H., Hsieh B., Xiong Z., Halsey K., Choi J., Tran T., et al. Performance of radiologists in differentiating COVID-19 from viral pneumonia on chest CT. Radiology. 2020;10(20):8–23. doi: 10.1148/radiol.2020200823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Dai W., Zhang H., Yu J., Xu H., Chen H., Luo S., et al. CT imaging and differential diagnosis of COVID-19. Can Assoc Radiol J. 2020;71(2):195–200. doi: 10.1177/0846537120913033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Raptis C., Hammer M., Short R., Shah A., Bhalla S., Bierhals A., et al. Chest CT and coronavirus disease (COVID-19): a critical review of the literature to date. AJR. 2020;16(20):1–4. doi: 10.2214/AJR.20.23202. [DOI] [PubMed] [Google Scholar]
- 34.Salehi S., Abedi A., Balakrishnan S., Gholamrezanezhad A. Coronavirus disease 2019 (COVID-19): a systematic review of imaging findings in 919 patients. AJR. 2020;10(5):1–7. doi: 10.2214/AJR.20.23034. [DOI] [PubMed] [Google Scholar]
- 35.Caruso D., Zerunian M., Polici M., Pucciarelli F., Polidori T., Rucci C., et al. Chest CT features of COVID-19 in Rome, Italy. Radiology. 2020 doi: 10.1148/radiol.2020201237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Zhu Y., Liu Y., Li Z., Kuang J., Li X., Yang Y., et al. Clinical and CT imaging features of 2019 novel coronavirus disease (COVID-19) J Infect Dis. 2020 doi: 10.1016/j.jinf.2020.02.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Xie X., Zhong Z., Zhao W., Zheng C., Wang F., Liu J. Chest CT for typical 2019-nCoV pneumonia: relationship to negative RT-PCR testing. Radiology. 2020 doi: 10.1148/radiol.2020200343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bullock J., Luccioni A., Pham K., Lam C., Oroz M. Mapping the landscape of artificial intelligence applications against COVID-19. medarXiv. 2020 https://arxiv.org/abs/2003.11336 [Google Scholar]
- 39.Li L., Qin L., Xu Z., Yin Y., Wang X., Kong B., et al. Artificial intelligence distinguishes COVID-19 from community acquired pneumonia on chest CT. Radiology. 2020 doi: 10.1148/radiol.2020200905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Naudé W. Artificial Intelligence against COVID-19: An early review. https://papers.ssrn.com/sol3/papers.cfm?abstract_id=3568314 Available from:
- 41.Wang D., Hu B., Hu C., Zhu F., Liu X., Zhang J., et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus–infected pneumonia in Wuhan, China. Jama. 2020;323(11):1061–1069. doi: 10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.LeBlanc J., Heinstein C., MacDonald J., Pettipas J., Hatchette T., Patriquin G. A combined oropharyngeal/nares swab is a suitable alternative to nasopharyngeal swabs for the detection of SARS-CoV-2. J Clin Virol. 2020;128(2020):1–4. doi: 10.1016/j.jcv.2020.104442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kojima N., Turner F., Slepnev V., Bacelar A., Deming L., Kodeboy S., et al. Self-collected oral fluid and nasal swabs demonstrate comparable sensitivity to clinician collected nasopharyngeal swabs for covid-19 detection. medRxiv. 2020 doi: 10.1101/2020.04.11.20062372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Jawerth N. How is the COVID-19 Virus Detected using Real Time RT-PCR? https://www.iaea.org/newscenter/news/how-is-the-covid-19-virus-detected-using-real-time-rt-pcr Available from:
- 45.Yang W., Cao Q., Qin L., Wang X., Cheng Z., Dai A., et al. Clinical characteristics and imaging manifestations of the 2019 novel coronavirus disease (COVID-19): a multi-center study in Wenzhou city, Zhejiang, China. J Infect. 2020;80(4):388–393. doi: 10.1016/j.jinf.2020.02.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Yang W., Yan F. Patients with RT-PCR confirmed COVID-19 and normal chest CT. Radiology. 2020;295(2):1–2. doi: 10.1148/radiol.2020200702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Dai H., Zhang X., Xia J., Zhang T., Shang Y., Huang R., et al. High-resolution chest CT features and clinical characteristics of patients infected with COVID-19 in Jiangsu, China. Int J Infect Dis. 2020;95(2020):106–112. doi: 10.1016/j.ijid.2020.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Shi F., Wang J., Shi J., Wu Ziyan, Wang Q., Tang Z., et al. Review of artificial intelligence techniques in imaging data acquisition, segmentation and diagnosis for covid-19. IEEE Trans BIOMED. 2020 doi: 10.1109/RBME.2020.2987975. [DOI] [PubMed] [Google Scholar]
- 49.Chung M., Bernheim A., Mei X., Zhang N., Huang M., Zeng X., et al. CT imaging features of 2019 novel coronavirus (2019-nCoV) Radiology. 2020;295(1):202–207. doi: 10.1148/radiol.2020200230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Lee E., Ng M., Khong P.L. COVID-19 pneumonia: what has CT taught us? Lancet Infect Dis. 2020;20(4):384–385. doi: 10.1016/S1473-3099(20)30134-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.American College of Radiology ACR Recommendations for the use of Chest Radiography and Computed Tomography (CT) for Suspected COVID-19 Infection. https://www.acr.org/Advocacy-and-Economics/ACR-Position-Statements/Recommendations-for-Chest-Radiography-and-CT-for-Suspected-COVID19-Infection Available from:
- 52.The Royal College of Radiologists The role of CT in patients suspected with COVID-19 infection. https://www.rcr.ac.uk/college/coronavirus-covid-19-what-rcr-doing/clinical-information/role-ct-chest/role-ct-patients Available from:
- 53.General Office of National Health Committee Office of State Administration of Traditional Chinese Medicine. Notice on the issuance of a program for the diagnosis and treatment of novel coronavirus (2019-nCoV) infected pneumonia (trial sixth edition) http://yzs.satcm.gov.cn/zhengcewenjian/2020-02-19/13221.html Available from:
- 54.Kanne J., Little B., Chung J., Elicker B., Ketai L. Essentials for radiologists on COVID-19: an update—radiology scientific expert panel. Radiology. 2020 doi: 10.1148/radiol.2020200527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Fang Y., Zhang H., Xie J., Lin M., Ying L., Pang P., et al. Sensitivity of chest CT for COVID-19: comparison to RT-PCR. Radiology. 2020 doi: 10.1148/radiol.2020200432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Shi H., Han X., Jiang N., Cao Y., Alwalid O., Gu J., et al. Radiological findings from 81 patients with COVID-19 pneumonia in Wuhan, China: a descriptive study. Lancet Infect Dis. 2020;20(4):425–434. doi: 10.1016/S1473-3099(20)30086-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Wu J., Wu X., Zeng W., Zeng W., Guo D., Fang Z., et al. Chest CT findings in patients with coronavirus disease 2019 and its relationship with clinical features. Invest Radiol. 2020;55(5):257–261. doi: 10.1097/RLI.0000000000000670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Pan F., Ye T., Sun P., Gui S., Liang B., Li L., et al. Time course of lung changes on chest CT during recovery from 2019 novel coronavirus (COVID-19) pneumonia. Radiology. 2020;295(3):215–221. doi: 10.1148/radiol.2020200370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Zu Z., Jiang M., Xu P., Chen W., Ni Q., Lu G., et al. Coronavirus disease 2019 (COVID-19): a perspective from China. Radiology. 2020 doi: 10.1148/radiol.2020200490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Ng M., Lee E., Yang J., Yang F., Li X., Wang H., et al. Imaging profile of the COVID-19 infection: radiologic findings and literature review. Radiology: Cardiothorac Imag. 2020 Feb 13;2(1):200–234. doi: 10.1148/ryct.2020200034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Pan Y., Guan H., Zhou S., Wang Y., Li Q., Zhu T., et al. Initial CT findings and temporal changes in patients with the novel coronavirus pneumonia (2019-nCoV): a study of 63 patients in Wuhan, China. Eur Radiol. 2020;30(5):3306–3309. doi: 10.1007/s00330-020-06731-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Paul N., Roberts H., Butany J., Chung T., Gold W., Mehta S., et al. Radiologic pattern of disease in patients with severe acute respiratory syndrome: the Toronto experience. Radiographics. 2004;24(2):553–563. doi: 10.1148/rg.242035193. [DOI] [PubMed] [Google Scholar]
- 63.Kay F., Abbara S. The many faces of COVID-19: spectrum of imaging manifestations. Radiology. 2020;2(1):1–6. doi: 10.1148/ryct.2020200037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Ye Z., Zhang Y., Wang Y., Huang Z., Song B. Chest CT manifestations of new coronavirus disease 2019 (COVID-19): a pictorial review. Eur Radiol. 2020;19(20):1–9. doi: 10.1007/s00330-020-06801-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Song F., Shi N., Shan F., Zhang Z., Shen J., Ling H., et al. Emerging 2019 novel coronavirus (2019-nCoV) pneumonia. Radiology. 2020;295(1):210–217. doi: 10.1148/radiol.2020200274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Franquet T. Imaging of pulmonary viral pneumonia. Radiology. 2011;260(1):18–39. doi: 10.1148/radiol.11092149. [DOI] [PubMed] [Google Scholar]
- 67.Li M., Lei P., Zeng B., Li Z., Yu P., Fan B., et al. Coronavirus disease (COVID-19): spectrum of CT findings and temporal progression of the disease. Acad Radiol. 2020;27(5):603–608. doi: 10.1016/j.acra.2020.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Li K., Wu J., Wu F., Guo D., Chen L., Fang Z., et al. The clinical and chest CT features associated with severe and critical COVID-19 pneumonia. Invest Radiol. 2020;55(6):327–331. doi: 10.1097/RLI.0000000000000672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Jin C., Chen W., Cao Y., Xu Z., Tan Z., Zhang X., et al. Development and evaluation of an AI system for COVID-19 diagnosis. medRxiv. 2020 doi: 10.1101/2020.03.20.20039834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Hosny A., Parmar C., Quackenbush J., Schwartz L., Aerts H. Artificial intelligence in radiology. Nat Rev Cancer. 2018;18(8):500–510. doi: 10.1038/s41568-018-0016-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Tang A., Tam R., Cadrin-Chênevert A., Guest W., Chong J., Barfett J., et al. Canadian Association of Radiologists white paper on artificial intelligence in radiology. Can Assoc Radiol J. 2018;69(2):120–135. doi: 10.1016/j.carj.2018.02.002. [DOI] [PubMed] [Google Scholar]
- 72.Thrall J., Li X., Li Q., Cruz C., Do S., Dreyer K., et al. Artificial intelligence and machine learning in radiology: opportunities, challenges, pitfalls, and criteria for success. J Am Coll Radiol. 2018;15(3):504–508. doi: 10.1016/j.jacr.2017.12.026. [DOI] [PubMed] [Google Scholar]
- 73.Kong B., Wang X., Bai J., Gao F., Cao K., Xia J., et al. Learning tree-structured representation for 3D coronary artery segmentation. Comput Med Imag Graph. 2020;80(20):10–18. doi: 10.1016/j.compmedimag.2019.101688. [DOI] [PubMed] [Google Scholar]
- 74.Rao B., Zohrabian V., Cedeno P., Saha A., Pahade J., Davis M. Utility of artificial intelligence tool as a prospective radiology peer Reviewer—detection of unreported intracranial hemorrhage. Acad Radiol. 2020 doi: 10.1016/j.acra.2020.01.035. [DOI] [PubMed] [Google Scholar]
- 75.Ardila D., Kiraly A., Bharadwaj S., Choi B., Reicher J., Peng L., et al. End-to-end lung cancer screening with three-dimensional deep learning on low-dose chest computed tomography. Nat Med. 2019;25(6):954–961. doi: 10.1038/s41591-019-0447-x. [DOI] [PubMed] [Google Scholar]
- 76.Kermany D., Goldbaum M., Cai W., Valentim C., Liang H., Baxter S., et al. Identifying medical diagnoses and treatable diseases by image-based deep learning. Cell. 2018;172(5):1122–1131. doi: 10.1016/j.cell.2018.02.010. [DOI] [PubMed] [Google Scholar]
- 77.Rajaraman S., Candemir S., Kim I., Thoma G., Antani S. Visualization and interpretation of convolutional neural network predictions in detecting pneumonia in pediatric chest radiographs. Appl Sci. 2018;8(10):1715. doi: 10.3390/app8101715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Shan F., Gao Y., Wang J., Shi N., Han M., Xue Z., et al. Lung infection quantification of covid-19 in ct images with deep learning. arXiv 2020: arXiv:2003.04655. 2020 [Google Scholar]
- 79.Li L., Qin L., Xu Z., Yin Y., Wang X., Kong B., et al. Artificial intelligence distinguishes covid-19 from community acquired pneumonia on chest ct. Radiology. 2020 doi: 10.1148/radiol.2020200905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Chen J., Wu L., Zhang J., Zhang L., Gong D., Zhao Y., et al. Deep learning-based model for detecting 2019 novel coronavirus pneumonia on high-resolution computed tomography: a prospective study. medRxiv. 2020 doi: 10.1101/2020.02.25.20021568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Gozes O., Frid-Adar M., Greenspan H., Browning P., Zhang H., Ji W., et al. Rapid ai development cycle for the coronavirus (covid-19) pandemic: initial results for automated detection & patient monitoring using deep learning ct image analysis. arXiv:2003.05037. 2020 [Google Scholar]
- 82.Xu X., Jiang X., Ma C., Du P., Li X., Lv S., et al. Deep learning system to screen coronavirus disease 2019 pneumonia. arXiv:2002.09334. 2020 doi: 10.1016/j.eng.2020.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Bai X., Fang C., Zhou Y., Bai S., Liu Z., Chen Q., et al. Predicting COVID-19 malignant progression with AI techniques. Lancet. 2020 doi: 10.1101/2020.03.20.20037325. [DOI] [Google Scholar]
- 84.Maghdid H., Asaad A., Ghafoor K., Sadiq A., Khan M. Diagnosing COVID-19 pneumonia from X-ray and CT images using deep learning and transfer learning algorithms. arXiv:2004.00038. 2020 [Google Scholar]
- 85.Huang L., Han R., Ai T., Yu P., Kang H., Tao Q., et al. Serial quantitative chest ct assessment of covid-19: deep-learning approach. Radiology. 2020;2(2):20–75. doi: 10.1148/ryct.2020200075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Gozes O., Frid-Adar M., Sagie N., Zhang H., Ji W., Greenspan H. Coronavirus detection and analysis on chest ct with deep learning. arXiv:2004.02640. 2020 [Google Scholar]
- 87.Nguyen T.T. Artificial intelligence in the battle against coronavirus (COVID-19): a survey and future research directions. https://www.researchgate.net/profile/Thanh_Nguyen372/publication/340487417_Artificial_Intelligence_in_the_Battle_against_Coronavirus_COVID-19_A_Survey_and_Future_Research_Directions/links/5ec928a2458515626cc328f9/Artificial-Intelligence-in-the-Battle-against-Coronavirus-COVID-19-A-Survey-and-Future-Research-Directions.pdf Available from:
- 88.Bai H., Hsieh B., Xiong Z., Halsey K., Choi J., Tran T., et al. Performance of radiologists in differentiating COVID-19 from viral pneumonia on chest CT. Radiology. 2020 doi: 10.1148/radiol.2020200823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Bai X., Wang R., Xiong Z., Hsieh B., ChangK, Halsey K., et al. AI augmentation of radiologist performance in distinguishing COVID-19 from pneumonia of other etiology on chest CT. Radiology. 2020 doi: 10.1148/radiol.2020201491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Zheng C., Deng X., Fu Q., Zhou Q., Feng J., Ma H., et al. Deep learning-based detection for COVID-19 from chest CT using weak label. medRxiv. 2020 doi: 10.1101/2020.03.12.20027185. [DOI] [Google Scholar]