Abstract
Purpose
In response to the coronavirus disease 2019 pandemic, current Association of American Medical Colleges guidelines discourage away rotations, posing significant challenges for attracting students to radiation oncology (RO). This is particularly concerning for medical students underrepresented in medicine (UIM) due to the potential of widening existing disparities in applicant and workforce composition. To proactively address this, we created a Radiation Oncology Intensive Shadowing Experience (RISE) to expose UIM students to the field of RO.
Methods and Materials
Key stakeholders within the residency program, including both UIM faculty and residents with experience in health disparities and medical education, designed a 1-week virtual RISE intended for fourth year UIM students recruited through established national organizations serving UIM medical students. A 1-week disease-specific curriculum was developed using 4 components: (1) foundational exposure to RO, (2) didactic teaching, (3) mentorship opportunities, and (4) a capstone experience. Mentorship was continuously weaved through the experience by attendings, peer resident mentors, and a UIM resident panel to optimize exposure.
Results
RISE was successfully initiated at 2 academic medical centers with 12 UIM students enrolled through August. Anonymized pre- and postclerkship surveys were developed for students, residents, and faculty involved in RISE to evaluate participants’ satisfaction, resident and attending time burden, and perceptions of program effectiveness.
Conclusions
We created a unique virtual RO shadowing experience for UIM students to address a critical gap in exposure to RO, heightened by the corona virus disease 2019 pandemic, with the goal of improving diversity, equity, and inclusion in our field.
Introduction
The novel coronavirus disease 2019 (COVID-19) pandemic has affected medical education with suspension of on-site clinical rotations per the Association of American Medical Colleges (AAMC).1 In response, radiation oncology (RO) residency programs have created virtual clinical opportunities to address gaps in medical education.2,3 However, at the time of this publication, there were few available clerkships for medical students unaffiliated with a home residency program. Current AAMC guidelines discourage away rotations for the 2020 to 2021 academic year, except in circumstances where students lack access to clinical experiences within their home institution.4 These guidelines pose challenges for minority students underrepresented in medicine (UIM) as they are approximately 40% less likely than their non-Hispanic white counterparts to attend a medical school with an affiliated RO department.5 This lack of access to formal away rotations also affects associated benefits that could strengthen an application, including letters of recommendation, research opportunities, and networking.
To our knowledge, there are limited formal programs with a potential to improve workforce diversity in RO.6 Data on residency composition indicate that black, Hispanic, and American Indian/Alaska natives/native Hawaiians/Pacific Islanders make up 11.7% of applicants and 8.1% of RO residents.7,8 Given the interest in training a diverse and culturally competent workforce, the medical profession has advocated for deliberate efforts through pipeline recruitment.9 Herein, we describe a proactive approach to mitigate the effect of COVID-19 on senior UIM medical students through a Radiation Oncology Intensive Shadowing Experience (RISE). The goal of RISE is to provide clinical exposure, didactic teaching, mentorship, and networking opportunities for UIM trainees, allowing for promotion of diversity, equity, and inclusion in RO.
Methods and Materials
Using Kern’s 6 steps of curriculum design,10 key stakeholders with experience in medical education and health disparities were assembled from 3 Northeastern academic medical centers. Members included the residency program director, medical student clerkship directors, and residents, including those from UIM groups. The group reviewed COVID-related restrictions imposed on the residency program and identified the needs of both the program and of UIM students, highlighting the current deficiencies in education, followed by a problem-centered approach to identify solutions. Due to external time constraints, an abbreviated needs assessment was undertaken by stakeholders via a focused group discussion to identify the ideal learning environment for students, review existing resources, and highlight barriers to reform. A strategic planning session was pursued to develop specific goals and objectives for a 1-week virtual curriculum (Table 1).
Table 1.
Sample medical student schedule for 1-week RISE
| Monday | Tuesday | Wednesday | Thursday | Friday |
|---|---|---|---|---|
| 8:00-9:00 AM Resident AM conference |
8:00-9:00 AM Resident AM conference |
8:00-9:00 AM Resident AM conference |
8:00-9:00 AM Resident AM conference |
8:00-9:00 AM Resident AM conference |
| 9:00-10:00 AM Virtual panel with UIM RO residents and attendings |
9:00-11:00 AM Peer resident mentor IROC sessions 1 and 2 – introduction and CT simulation |
9:00-10:00 AM Virtual experience of CT simulation – introduction to the role of radiation therapist |
9:00-10:00 AM IROC sessions 5 and 6 – physics & QA |
9:00-10:00 AM IROC session 7 – RO emergencies |
| 10:00-12:00 AM Virtual meet and greet with attending and didactic teaching on disease site topic |
11:00-12:00 AM Virtual patient consultation |
10:00-11:00 AM IROC session 4–plan evaluation |
10:00-11:00 AM Virtual follow-up visits with attending |
10:00-10:30 AM Final capstone prep resident mentor |
| 12:00-1:00 PM Virtual department chart rounds |
12:00-1:00 PM Disease site-specific tumor board |
11:00-1:00 PM Virtual MR-LINAC live treatment |
11:00-12:00 PM Academic time |
12:00-12:30 PM Capstone presentation & conversation – disease-specific topic |
| 1:00-2:00 PM Preconsultation virtual patient interview |
1:00-2:00 PM IROC session 3 – contouring |
1:00-2:00 PM Virtual on treatment visits with attending |
1:00-2:00 PM Peer resident meeting: Prep for capstone presentation |
1:00-2:00 PM Meeting with attending to debrief the week and discuss research opportunities |
| 2:00-3:00 PM Virtual consult with attending |
2:00-3:00 PM Peer resident meeting: Consult note writing and introduction to e-contour platform with contouring practice |
2:00-3:00 PM Virtual dosimetry session and plan review with attending |
2:00-4:00 PM Academic time (finish Power Point for capstone presentation on disease site topic) |
2:00-3:00 PM Peer resident meeting: Applying to RO & wrap-up |
Abbreviations: CT = computed tomography; IROC = Introductory Radiation Oncology Curriculum; LINAC = linear accelerator; MR = magnetic resonance; QA = question and answer; RISE = Radiation Oncology Intensive Shadowing Experience; RO = radiation oncology; UIM = underrepresented in medicine.
The 4 key components of the RISE curriculum include (1) exposure to RO through virtual attendance of department chart rounds and tumor boards; virtual exposure to simulations, contouring, and treatment planning; and patient encounters via secure cloud-based telemedicine; (2) knowledge through didactic teaching; (3) mentorship opportunities through formal exposure to site-specific attendings and resident mentor and via informal exposures through a UIM panel during the virtual experience; and finally, (4) a capstone presentation. These components encompass the goals and objectives of RISE, including the formation of longitudinal relationships with resident and faculty mentors, and provide an intensive virtual experience to UIM students unduly affected by rotation limitations during COVID-19. To ensure quality content, the previously validated Introductory Radiation Oncology Curriculum was used for core knowledge.11,12 Participation in this 1-week intensive experience was designed to be limited to senior UIM medical students based on the AAMC definition.13 Recruitment was through established organizations, including the Student National Medical Association, Latino Medical Student Association, and the Asian Pacific American Medical Student Association, and advertisement on social media platforms.
Mentorship and networking experiences with 1 to 2 site-specific attendings, a resident, and a UIM resident panel were weaved throughout the experience. Finally, a case-based capstone presentation leveraged the students’ visibility in the department and highlighted the knowledge acquired during the week.
Results
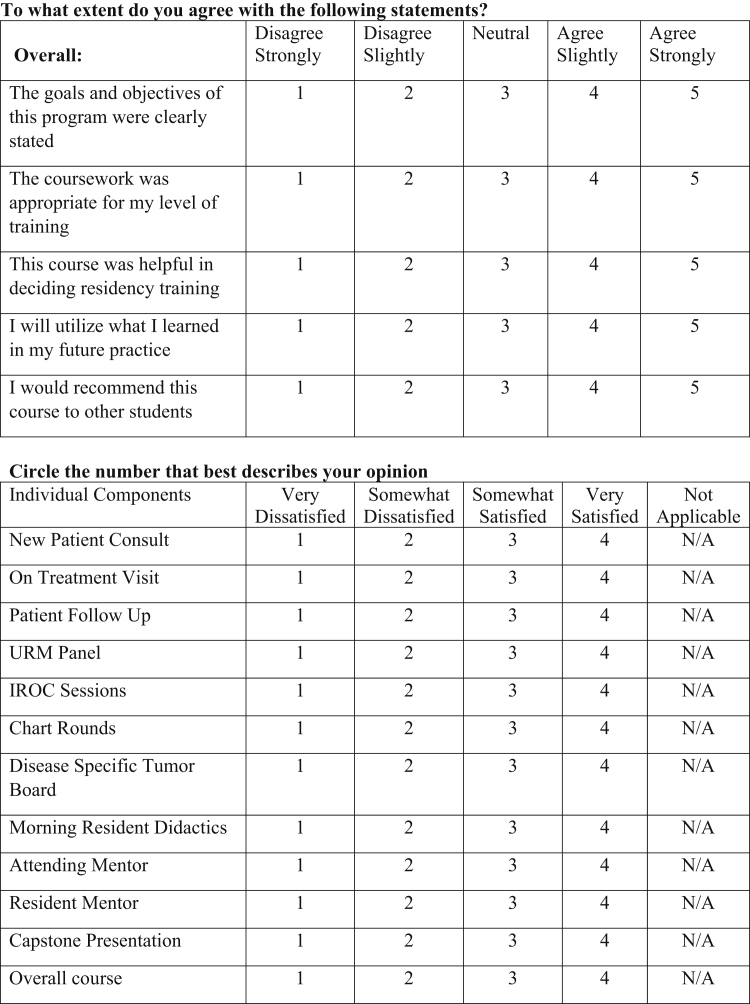
RISE was successfully implemented at 2 academic medical centers, with the first UIM medical student starting within 6 weeks from program conception. There was department-wide buy-in from leadership and 12 students were registered through the end of summer. Anonymized pre- and postclerkship surveys were developed for RISE student participants with questions on demographics, exposure to and experience with RO, and objective knowledge-based questions previously validated as part of the Introductory Radiation Oncology Curriculum curriculum11 (Fig 1). A brief survey was also designed for the faculty and resident mentors to evaluate the utility and time burden.
Figure 1.
Sample questions from medical student survey regarding evaluation of 1-week Radiation Oncology Intensive Shadowing Experience (RISE).
Discussion
To our knowledge, this is the only virtual RO shadowing experience specifically targeting UIM students. This addresses a critical gap in resources, exposure, diversity, and inclusion initiatives in RO. Our program, as part of a major medical cancer center, is uniquely positioned to provide students with a variety of learning opportunities and state-of-the-art technologies not widely available. One potential limitation is the short duration, condensing a traditional 4-week medical school rotation into 1 week. Although this is more compact, the virtual platform, intensive structure, and tailored single service mentorship allow students to spend more time with faculty mentors and build stronger connections while providing flexibility for filling empty time with educational experiences. Our curriculum includes educational activities previously reported by medical students as deciding factors for specialty and previously validated among RO residents for learning.14, 15, 16 The week-long experience, with designated faculty and peer resident mentors, aims to provide medical students the opportunity to build new career networks and establish collaborations for future projects, strengthening their residency applications.17 It also allows participants to interact with trainees of similar backgrounds and interests, shown to influence residency selection in UIM students.18
On a national scale, the COVID-19 pandemic has revealed a long known yet underaddressed epidemic of socioeconomic and health disparities within marginalized communities.19 In medical education, COVID-19 has influenced guidelines that may affect students who have historically been underrepresented in competitive specialties and could be deterred from applying due to limited access to rotations. We have harnessed this opportunity to create a curriculum that promotes diversity and inclusion. It also has applications beyond COVID-19, and based on our experience we hope other RO departments, with institution-specific adaptations, will use the RISE program to address similar obstacles in recruiting UIM students.
Footnotes
Sources of support: This work had no specific funding.
Disclosures: Dr Zietman reports a stipend from Elsevier as the editor-in-chief of International Journal of Radiation Oncology, Biology, and Physics, which is outside the submitted work. Dr Nguyen reports personal fees from COTA, Astellas, Bayer, Janssen, Ferring, Augmenix, Dendreon, Blue Earth Diagnostics, and Boston Scientific, and grant funding from Astellas, Bayer and Janssen, all outside the submitted work.
References
- 1.Important guidance for medical students on clinical rotations during the coronavirus (COVID-19) outbreak. AAMC. https://www.aamc.org/news-insights/press-releases/important-guidance-medical-students-clinical-rotations-during-coronavirus-covid-19-outbreak Available at:
- 2.Pollom E, Sandhu N, Frank J, et al. Continuing medical student education during the COVID19 pandemic: Development of a virtual radiation oncology clerkship [e-pub ahead of print]. Adv Radiat Oncol. https://doi.org/10.1016/j.adro.2020.05.006. Accessed June 16, 2020. [DOI] [PMC free article] [PubMed]
- 3.Kahn J. ROECSG 2020 – Virtual medical student radiation oncology elective in the COVID-19 era. Oral presentation on May 16, 2020. Available at: https://www.youtube.com/watch?v=WHQsBzhhogM&feature=youtu.be. Accessed May 16, 2020.
- 4.Final report and recommendations for medical education institutions of LCME-accredited, U.S. osteopathic, and non-U.S. medical school applicants. https://www.aamc.org/system/files/2020-05/covid19_Final_Recommendations_05112020.pdf Available at:
- 5.Chapman C.H., Hwang W.T., Deville C. Diversity based on race, ethnicity, and sex, of the US radiation oncology physician workforce. Int J Radiat Oncol Biol Phys. 2013;85:912–918. doi: 10.1016/j.ijrobp.2012.08.020. [DOI] [PubMed] [Google Scholar]
- 6.American Society for Radiation Oncology https://www.astro.org/Patient-Care-and-Research/Research/Funding-Opportunities/ASTRO-Minority-Summer-Fellowship-Award Available at:
- 7.Castillo-Page L. Association of American Medical Colleges; 2016. Diversity in Medical Education: Facts & Figures 2016.https://www.aamcdiversityfactsandfigures2016.org/report-section/section-1/ Available at: Accessed October 18, 2020. [Google Scholar]
- 8.Pandharipande P.V., Mercaldo N.D., Lietz A.P. Identifying barriers to building a diverse physician workforce: A national survey of the ACR membership. J Am Coll Radiol. 2019;16:1091–1101. doi: 10.1016/j.jacr.2019.05.008. [DOI] [PubMed] [Google Scholar]
- 9.Jones R.D., Chapman C.H., Holliday E.B. Qualitative assessment of academic radiation oncology department chairs' insights on diversity, equity, and inclusion: Progress, challenges, and future aspirations. Int J Radiat Oncol Biol Phys. 2018;101:30–45. doi: 10.1016/j.ijrobp.2018.01.012. [DOI] [PubMed] [Google Scholar]
- 10.Thomas P.A., Kern D.E., Hughes M.T., Chen B.Y. 3rd ed. Johns Hopkins University Press; Baltimore, MD: 2016. Curriculum Development for Medical Education a Six-Step Approach. [Google Scholar]
- 11.Jimenez RB, Johnson A, Padilla L, et al. The impact of an introductory radiation oncology curriculum (IROC) for radiation oncology trainees across the United States and Canada [e-pub ahead of print]. Int J Radiat Oncol Biol Phys. https://doi.org/10.1016/j.ijrobp.2020.02.015. Accessed June 16, 2020. [DOI] [PubMed]
- 12.Golden D.W., Braunstein S., Jimenez R.B. Multi-institutional implementation and evaluation of a curriculum for the medical student clerkship in radiation oncology. J Am Coll Radiol. 2016;13:203–209. doi: 10.1016/j.jacr.2015.06.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Underrepresented in Medicine Definition AAMC. https://www.aamc.org/what-we-do/mission-areas/diversity-inclusion/underrepresented-in-medicine Available at:
- 14.McKillip R.P., Kauffmann G., Chmura S.J. Structured radiation oncology clerkship curricula: Evaluating the effect on residency applicant knowledge of radiation oncology. J Am Coll Radiol. 2018;15:1330. doi: 10.1016/j.jacr.2018.05.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sidiqi B.U., Gillespie E.F., Lapen K. Patterns and perceptions of “away” rotations among radiation oncology residency applicants. Int J Radiat Oncol Biol Phys. 2020;107:1007–1011. doi: 10.1016/j.ijrobp.2020.04.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gunther J.R., Jimenez R.B., Yechieli R.L. Introductory radiation oncology curriculum: Report of a national needs assessment and multi-institutional pilot implementation. Int J Radiat Oncol Biol Phys. 2018;101:1029–1038. doi: 10.1016/j.ijrobp.2018.04.020. [Correction appears in Int J Radiat Oncol Biol Phys. 2018;102:1602] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sayan M., Ohri N., Lee A. The impact of formal mentorship programs on mentorship experience among radiation oncology residents from the northeast. Front Oncol. 2019;9:1369. doi: 10.3389/fonc.2019.01369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lightfoote J.B., Deville C., Ma L.D. Diversity, inclusion, and representation: It is time to act. J Am Coll Radiol. 2016;13:1421–1425. doi: 10.1016/j.jacr.2016.08.008. [DOI] [PubMed] [Google Scholar]
- 19.Smith J.A., Judd J. COVID-19: Vulnerability and the power of privilege in a pandemic. Health Prom J Austral. 2020;31:158. doi: 10.1002/hpja.333. [DOI] [PMC free article] [PubMed] [Google Scholar]