Abstract
AIM
To provide a detailed description of the natural history of persistent subretinal fluid (SRF) after successful repair of rhegmatogenous retinal detachment (RRD) and its association with visual outcome.
METHODS
This was a prospective long-term follow-up for eyes undergoing scleral buckling (SB) surgery for macula-off RRD. Examinations were carried out preoperatively and postoperatively at 1, 3, 6, 9 and 12mo, until persistent SRF had completely resolved. One month postoperatively, optical coherence tomography (OCT) was used to classify SRF into three patterns: bleb-like loculated (BL), shallow-diffused (SD), and multiple blebs (MB). Serial OCT imaging was used to evaluate morphological changes in SRF until its complete disappearance. Patients were divided into two groups depending on the presence or absence of persistent SRF.
RESULTS
A total of 59 patients (59 eyes) were included. There were no statistical differences between two groups at baseline, except for the proportion of patients with high myopia and a younger age. One month after surgery, OCT detected persistent SRF in 49 eyes (83.1%). The 3 morphological patterns of SRF were observed in 27 eyes (55.1%) with BL, 13 eyes (26.5%) with SD, and 9 eyes (18.4%) with MB. The mean time for complete absorption differed significantly across the three SRF patterns (F=8.097, P=0.001), which was 8.8±6.1, 20.1±12.1, and 16.7±10.2mo in BL, SD, and MB, respectively. In 9 of the 13 eyes with SD, the pattern transformed into MB type. In cases involving MB, the size and number of blebs decreased gradually until they had been completely absorbed. Eyes with persistent SRF were more likely to demonstrate disruption of the ellipsoid zone (49.0% vs 10%, P=0.034). The final best-corrected visual acuity of two groups was 0.37±0.11 (with SRF) vs 0.34±0.12 (without SRF) logMAR (P=0.499), respectively.
CONCLUSION
High preoperative myopia and younger age are associated with persistent SRF. BL is the most commonly observed pattern with the shortest duration and gradually disappeared. Most cases involving SD SRF transform into MB type during resolution. The size and number of the MBs decrease gradually until they were completely absorbed. The absence of persistent SRF may contribute to slow visual recovery in the short-term but does not influence the final visual outcome.
Keywords: subretinal fluid, rhegmatogenous retinal detachment, optical coherence tomography, visual acuity
INTRODUCTION
Persistent subretinal fluid (SRF) is a common condition that refers to remnants of SRF between the sensory retina and the retinal pigment epithelium (RPE), even after ophthalmic confirmation that the retina has been reattached and that all retinal breaks have been sealed. By applying optical coherence tomography (OCT), a highly-sensitive and non-invasive diagnostic technique, previous studies showed that the incidence of persistent SRF varied widely, from 9% to 94%[1]–[5]. This level of variation is thought to be related to differences in study design, baseline patient demographics and characteristics, and surgical procedures. Previous studies have also reported that persistent SRF occurred in >50% of patients with rhegmatogenous retinal detachment (RRD) and treated by scleral buckling (SB), compared to 0 to 20% of patients treated by pars plana vitrectomy[1]–[2]. Research has also shown that younger patients[6], and those with a macula-off status[7], have higher incidence rates of postoperative SRF and delayed absorption.
It is commonly known that it can take several months for SRF to completely resolve, and that persistent SRF may affect visual recovery, reduce central vision, and cause metamorphopsia[8] and the loss of depth perception. It remains uncertain as to whether persistent SRF influences the final visual outcome; some authors consider that SRF is associated with visual loss[3],[9]–[10], while others do not[4],[11]–[12]. It is possible that these contradictory viewpoints relate to a variety of factors including small sample sizes, short follow-up periods, inappropriate case selection, and a failure to quantify the extent of SRF.
Three distinct patterns of SRF have been identified: bleb-like (BL), shallow-diffused (SD), and multiple blebs (MB). A previous study showed that the specific pattern of SRF involved represents an independent predictor for visual outcome postoperatively[3]. We hypothesized that the pattern of SRF, and the size and number of SRF blebs, might represent important determinants for persistent SRF. Furthermore, we considered that tracing the natural course of SRF blebs until their complete absorption may help to clarify the pathophysiological mechanisms underlying persistent SRF.
This prospective research study had three specific aims. First, we assessed the incidence, related factors, and time taken for fluid absorption in cases with persistent SRF. Second, we aimed to provide a detailed description of three distinct SRF patterns and explain how these change during persistent SRF absorption. Finally, we investigated how SRF might cause changes in macular structure and quantified how such events might be associated with visual outcome. Because of the likelihood of delayed absorption in cases of macula-involved retinal detachment (RD), we only included patients with macula-off RRD.
SUBJECTS AND METHODS
Ethical Approval
This was a prospective long-term follow-up study of patients who underwent SB surgery for primary uncomplicated macula-off RRD with detectable peripheral breaks. All aspects of the study were approved by the Baoding First Central Hospital Ethics Committee and conducted in accordance with the Declaration of Helsinki. Informed consent was acquired from all patients using a form that had been approved by the Institutional Review Board.
The study was carried out between January 1, 2015 and January 1, 2017 at the Department of Ophthalmology, Baoding First Central Hospital, China, and involved 59 consecutive eyes. Patients were included if they had macula-off RRD with good visibility, aged 18y or older, treated with SB alone, and achieved successful retinal reattachment. The exclusion criteria were as follows: 1) previous vitreoretinal surgery; 2) re-detachment during follow-up; 3) uveitis; 4) retinal vascular diseases (e.g., diabetic retinopathy, vascular occlusive diseases); 5) retinal dystrophies; 6) pre-existing macular pathological features (e.g., macular hole, age-related macular degeneration, macular edema, vitreomacular traction syndrome, or epiretinal membrane); 7) a follow-up period <6mo.
For each patient, we examined both eyes preoperatively and postoperatively (at 1, 3, 6, 9, and 12mo). If the SRF had been completely resorbed by the 12-month timepoint, then no further follow-up was required. In cases with no or delayed absorption, patients were routinely followed-up every 3mo to evaluate morphological changes until the persistent SRF had completely resolved. At each timepoint, patients received a complete ophthalmological examination, including best-corrected visual acuity (BCVA), slit-lamp biomicroscopy, and intraocular pressure (IOP). OCT was performed periodically to assess the natural resolution of SRF. Images were captured after administering mydriatic eye drops. Subjects were divided in two groups based on whether or not they had been diagnosed with persistent SRF (defined as a clear space between the sensory retina and the RPE when evaluated 1mo after SB surgery). SRF was detected with a macular Carl Zeiss Meditech Cirrus HD-OCT 5000 (Zeiss, Oberkochen, Germany).
Data Collection
Prior to surgery, we acquired a range of demographic and clinical data, including age, sex, medical and ophthalmic history, refractive error (high myopia defined as a preoperative spherical equivalent of -6 D or more), BCVA, IOP, lens status, macular status (determined by preoperative OCT), the duration and extent of detachment, the number and location of breaks, and previous ophthalmic operations. During surgery, we recorded whether SRF drainage was performed, and whether any additional interventions were performed for subretinal blebs. Postoperatively, patients underwent BCVA testing at each follow-up visit, and the anatomical status of the retina was evaluated by OCT.
Surgical Technique
All SB surgeries were conducted by one experienced retinal surgeon (Gu ZH). Prior to elective surgery, each patient underwent a complete physical examination. The selection of the surgical procedure was made at the surgeon's discretion. The time elapsed from a definitive diagnosis to surgery ranged from 2 to 4d. If patients were admitted on a Friday, Saturday, or during a holiday period, then they received surgery the following week day. All patients received surgery with a 5.0-mm-wide silicone sponge segmental buckle. During surgery, we applied cryotherapy to retinal tears and areas of degeneration. We then placed a radially, or circumferentially, oriented silicone sponge to block the retinal tear. SRF drainage was performed if necessary, but was a rare event in our series of cases. We also applied intraocular tamponade if required.
Optical Coherence Tomography
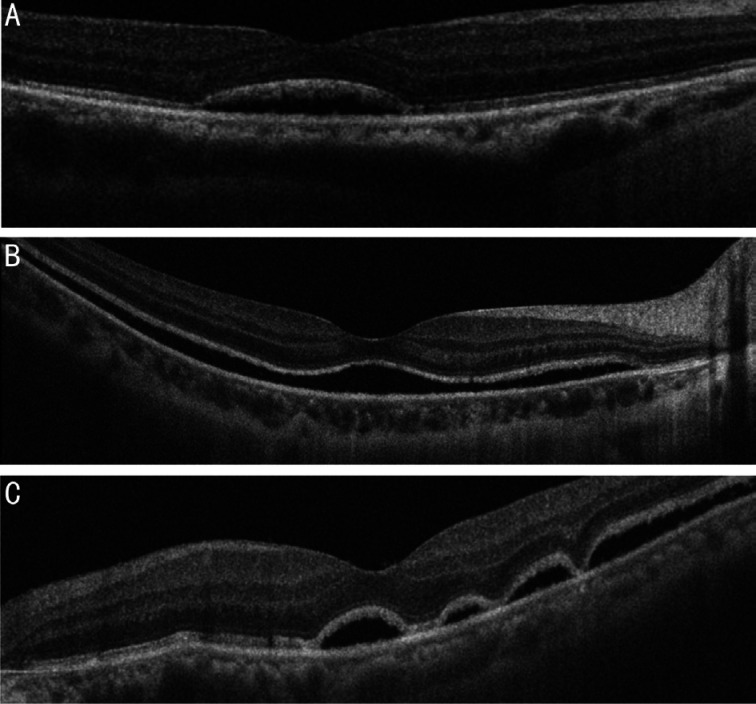
OCT scans were evaluated by two independent graders (Li LY and Zhang YL), who were blinded to clinical data. Any disagreement between the two graders was settled by a third grader (Chen S). For each patient, we carried out a series of periodic OCT scans during follow-up. These data allowed us to investigate the natural course of subretinal blebs and morphological changes in the retinal structure. We recorded a range of postoperative OCT parameters, including the presence and patterns of persistent SRF, the presence of an epiretinal membrane, and the presence of cystoid macular edema. We also assessed the integrity of the ellipsoid zone (EZ), and the external limiting membrane (ELM). ‘Damage’ was defined as a disruption or loss of integrity. Using OCT data acquired at the 1-month timepoint, we classified persistent SRF into three patterns: BL, SD, and MB (Figure 1). The BL type was defined as a single, confined, discrete bleb of fluid. The SD type was defined as an extension of sub-macular fluid over the fovea with a margin extending beyond the edge of a 6 mm scan. MB SRF was defined as the presence of more than three bleb-like sub-RDs. We evaluated serial morphological changes in SRF during follow-up until the SRF had completely disappeared.
Figure 1. Three patterns of SRF on OCT: BL (A), SD (B), and MB (C).
Statistical Analysis
All statistical analyses were performed using Statistical Package for the Social Sciences software version 25 (IBM Corp., Armonk, NY, USA). Qualitative parameters are presented as frequencies and percentages, while quantitative parameters are presented as means and standard deviations. BCVA was converted to the logarithm of the minimal angle of resolution (logMAR) before statistical analysis. We allocated logMAR values for counting fingers (logMAR=2.5), hand movements (logMAR=2.7), and light perception (logMAR=3.0). Differences in categorical data were analyzed using Chi-squared tests, or Fisher's exact tests for small samples. Unpaired t-tests, or the Mann-Whitney rank-sum test, were used to compare continuous data between eyes with and without persistent SRF. Paired t-tests were used to compare visual function across different timepoints, and repeated measures analysis of variance was used to compare baseline BCVA with mean BCVA at each follow-up visit. P<0.05 was considered statistically significant.
RESULTS
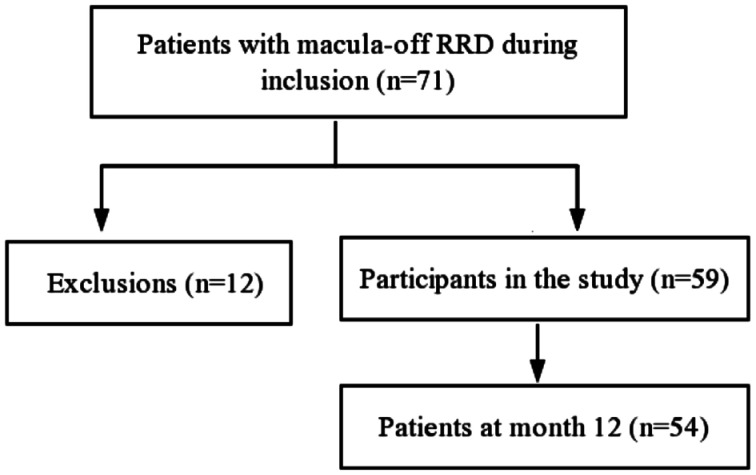
A total of 71 patients with primary macula-off RRD were treated during the study period, and all achieved complete retinal reattachment following SB surgery. Twelve patients were subsequently excluded due to pre-existing retinal or macular disease (n=6), previous eye trauma (n=2), and previous vitreoretinal surgery (n=1); three other patients were excluded because the follow-up period was <6mo. Finally, 59 patients (59 eyes) were included in the final analysis; 54 patients (54 eyes) were followed-up for at least 12mo (Figure 2).
Figure 2. Flow chart showing patient inclusion/exclusion.
Of the 59 patients, 32 (54.2%) were male and 27 (45.8%) were female. The mean patient age was 45.2±11.0y (range: 18 to 70y), and the mean follow-up duration was 15.6±7.2mo (range: 9 to 48mo). The mean time elapsed between symptom onset and surgery was 14.7±11.6d (range: 5 to 90d). In total, 52 (88.1%) eyes were phakic and 7 (11.9%) were pseudophakic. Only one patient underwent cataract surgery during the follow-up period. RD occurred in 8 (13.6%), 31 (52.5%), 18 (30.5%), and 2 (3.4%) eyes, with one, two, three, and four quadrants of RRD, respectively. Only 6 patients received intraoperative SRF drainage.
OCT was performed 1mo after surgery for retinal reattachment and identified persistent SRF in 49 of the 59 eyes (83.1%) of patients with macula-off RRD. At 3, 6, 9, and 12mo after SB surgery, OCT scans revealed sub-foveal fluid in 69.5%, 50.8%, 35.6%, and 30.5% of cases, respectively. Eighteen eyes with persistent SRF at 12mo were routinely followed-up every 3mo. At the 24-month follow-up timepoint, 6 cases (10.2%) still showed SRF on OCT imaging. SRF resolution was eventually observed in all but one case. The mean time to complete SRF absorption was 13.2±10.0mo (range: 3 to 30mo). None of the cases showing an absence of SRF at the 1-month follow-up timepoint showed SRF at any subsequent follow-up visit.
A comparison of the characteristics of the patient groups with and without persistent SRF is shown in Table 1. The persistent SRF group featured a significantly higher proportion of eyes with preoperative high myopia (46.9% vs 10%, P=0.038). Patients with persistent SRF were also significantly younger than those without persistent SRF (43.5±10.2 vs 53.5±11.1y, P=0.008). There were no significant differences between the two groups in terms of sex, lens status, number of breaks, the duration of detachment, or the extents of RD and SRF drainage.
Table 1. A comparison of characteristics between groups of patients with and without persistent SRF.
| Parameter | Overall (n=59 eyes) | Persistent SRF (n=49 eyes) | SRF absent (n=10 eyes) | P |
| Sex, n (%) | ||||
| Male | 32 (54.2) | 26 (53.1) | 6 (60) | 0.688a |
| Female | 27 (45.8) | 23 (56.9) | 4 (40) | |
| Age, y | 45.2±11.0 | 43.5±10.2 | 53.5±11.1 | 0.008b |
| Laterality, n (%) | ||||
| Right eye | 31 (52.5) | 26 (53.1) | 5 (50) | 0.860a |
| Left eye | 28 (47.5) | 23 (56.9) | 5 (50) | |
| Lens status, eyes n (%) | ||||
| Phakic | 52 (88.1) | 43 (87.8) | 9 (90) | 0.662a |
| Pseudophakic | 7 (11.9) | 6 (12.2) | 1 (10) | |
| Detachment duration (d) | 14.7±11.6 | 14.8±12.3 | 14.3±7.1 | 0.911b |
| Quadrants of RRD | 2.2±0.73 | 2.3±0.73 | 2.0±0.67 | 0.261b |
| Breaks number | 1.4±0.53 | 1.5±0.54 | 1.3±0.48 | 0.365b |
| High myopia (%) | 24 (40.7) | 23 (46.9) | 1 (10) | 0.038a |
| SRF drainage (%) | 6 (10.2) | 5 (10.2) | 1 (10) | 1.0a |
| BCVA, logMAR | 1.25±0.29 | 1.25±0.30 | 1.24±0.26 | 0.915b |
BCVA: Best-corrected visual acuity; logMAR: Logarithm of minimal angle of resolution; RRD: Rhegmatogenous retinal detachment; SRF: Subretinal fluid. aChi-squared tests or Fisher's exact test; bt-test.
mean±SD
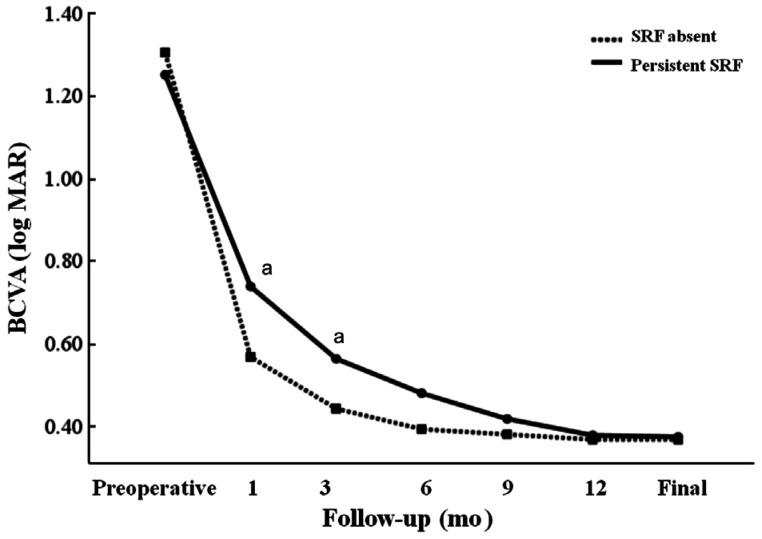
There were no significant differences in preoperative BCVA when compared between eyes with and without SRF (P=0.915); mean preoperative BCVA at baseline was 1.25±0.29 logMAR. After surgery, BCVA was 0.71±0.21 logMAR at 1mo, 0.53±0.16 logMAR at 3mo, 0.45±0.16 logMAR at 6mo, 0.40±0.15 logMAR at 9mo, 0.37±0.12 logMAR at 12mo, and 0.36±0.11 logMAR at the final postoperative follow-up visit. Compared with baseline, BCVA showed significant improvement at all follow-up visits (P<0.0001). There was no significant difference between the groups in terms of the change in BCVA (P=0.093). The BCVA of patients with SRF at 1mo (0.73±0.21 vs 0.57±0.16 logMAR, P=0.022) and 3mo (0.55±0.17 vs 0.43±0.08 logMAR, P=0.029), was significantly worse than that in patients without SRF. No significant differences were detected in postoperative BCVA values between groups at 6mo, or any of the subsequent follow-up visits. Similarly, there were no significant differences between groups in terms of final BCVA (0.37±0.11 vs 0.34±0.12 logMAR, P=0.499). The longitudinal changes in BCVA are shown in Figure 3.
Figure 3. Changes in BCVA during follow-up after SB surgery for patients with macula-off RRD.
The mean preoperative BCVA values at baseline were 1.25±0.30 logMAR and 1.24±0.26 logMAR in eyes with and without SRF, respectively. Subgroup analysis between groups of patients with and without SRF showed that the mean BCVA in the SRF group was significantly worse than patients without SRF at the 1- and 3-month follow-up timepoints (P=0.022 and 0.029, respectively). However, there were no significant differences throughout the rest of the follow-up period (P=0.081 at 6mo, P=0.272 at 9mo, P=0.829 at 12mo, and P=0.499 at the final visit). aP<0.05.
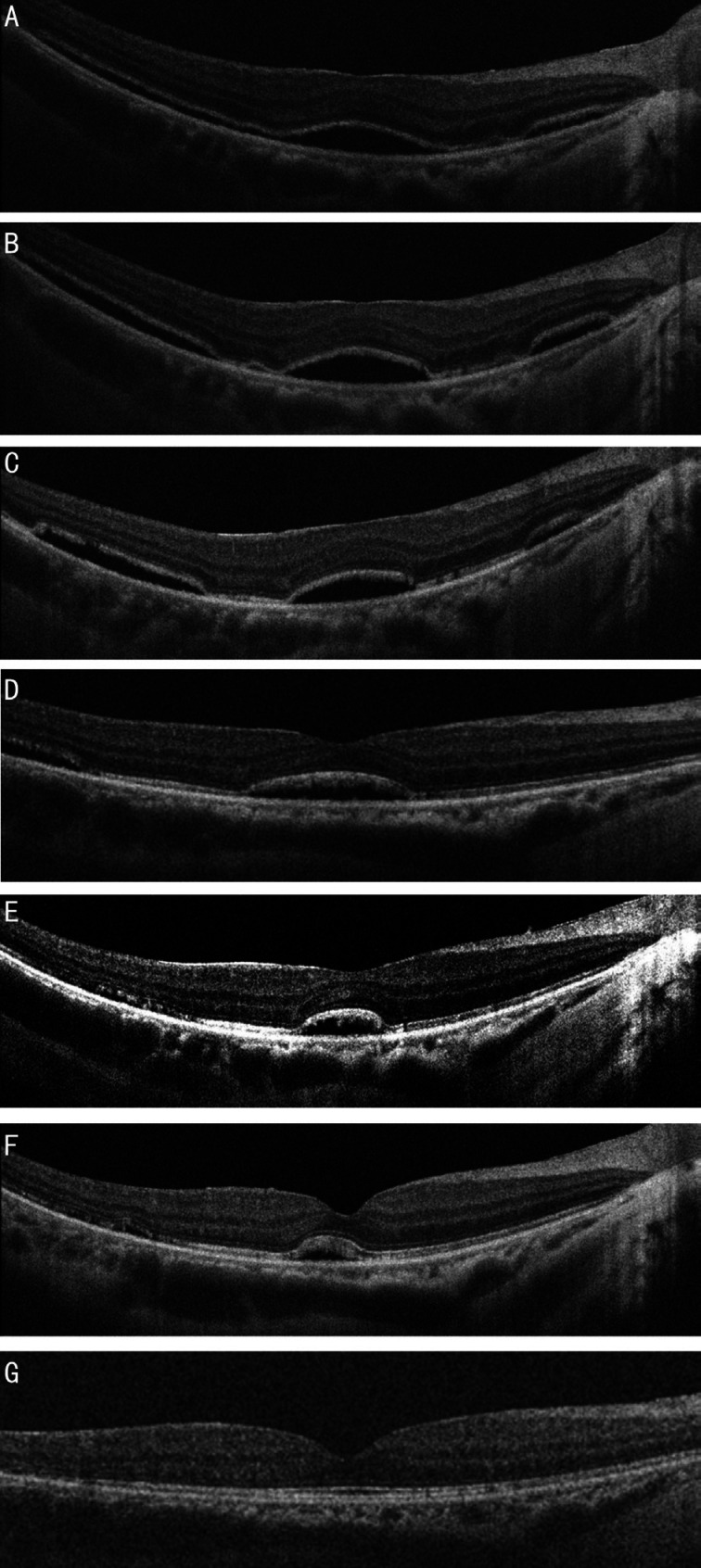
In eyes with persistent SRF, 27 (55.1%) eyes showed BL, 13 (26.5%) eyes showed SD, and 9 (18.4%) had MB. Cumulative persistence curves across the different types of SRF are shown in Figure 4. Over longitudinal follow-up, the mean time for complete absorption differed significantly among the three SRF patterns (F=8.097, P=0.001). BL SRF was less persistent than the other two forms (both P<0.05). In the sub-group of patients with BL SRF, we observed gradual resolution within a mean period of 8.8±6.1mo (range: 3 to 21mo). BL SRF was completely absorbed within 12 and 24mo after SB surgery in 22 and 4 cases, respectively. Two cases with complete absorption of SRF at 9mo, and 1 case without resolution, were lost to follow-up after 12mo. There was no significant difference in the duration of SRF when compared between the diffused and MB patterns. In 9 of the 13 eyes with diffused SRF, the pattern transformed into the MB type and completely resolved during follow-up. Another 3 cases of diffused SRF showed partial attachment from the periphery to the center of the retina during SRF absorption. The mean time to complete absorption of SD SRF was 20.1±12.1mo (range: 6 to 30mo). One case of diffused SRF showed subretinal fibrosis with long-standing RRD without absorption at the final follow-up at 4y. Figure 5 depicts a representative case showing the natural evolution of diffused SRF after SB surgery. The size and number of blebs gradually decreased until they had been completely absorbed. The mean time to complete absorption of MB was 16.7±10.2mo (range: 6 to 30mo). None of the eyes examined showed an increase of SRF during the period of observation. We evaluated the influence of SRF patterns on final BCVA and found that there were no significant differences among the three types (P=0.27).
Figure 4. Cumulative persistence curves of the three SRF patterns.
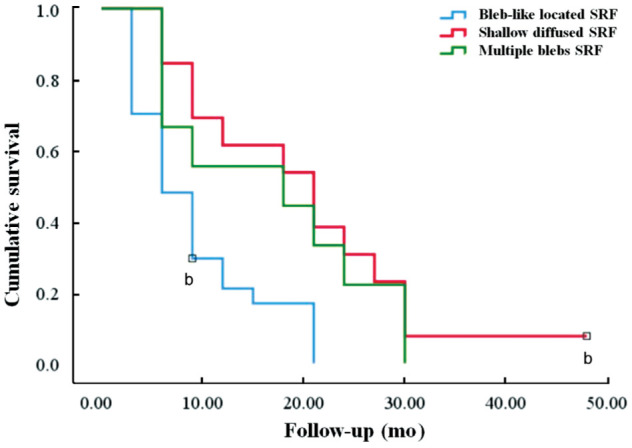
bCensored cases.
Figure 5. The natural evolution of SD SRF after SB surgery.
Images represent serial OCT images showing the natural course of a 41-year-old patient with SD SRF after SB surgery for macula-off RRD. A: Diffused SRF was observed 1mo after surgery. BCVA was 0.7 logMAR. B: Three months after surgery, the SRF pattern had transformed from the diffuse type to the MB type, with discontinuous retinal reattachment. BCVA was 0.7 logMAR. C: Six months after surgery, the width of the SRF had decreased. BCVA was 0.6 logMAR. D: Nine months after surgery, the width and number of blebs had decreased, BCVA was 0.4 logMAR. E: Twelve months after surgery, the blebs showed gradual regression, leaving a single bleb. BCVA was 0.3 logMAR. F: Fifteen months after surgery, the width of the single bleb SRF had decreased. BCVA was 0.3 logMAR. G: Complete resolution of bleb SRF was confirmed 18mo after surgery. BCVA was 0.2 logMAR.
The most frequent postoperative finding on OCT was disruption of the EZ and ELM. One month after surgery, postoperative EZ was disrupted in 25 (36.2%) eyes, while ELM integrity was disrupted in 14 (23.7%) patients. Eyes with persistent SRF were more likely to show disruption of the EZ (49.0% vs 10%, P=0.034). As the volume of SRF decreased, most patients showed gradual restoration of the EZ and ELM integrity during follow-up. A small proportion of cases showed progressive EZ disruption. At the final follow-up visit, 4 (6.8%) patients still showed disruption of EZ and ELM. Epiretinal membranes were detected in 3 of the 59 (5.1%) eyes, and macular edema was observed in 6 (10.2%) eyes.
DISCUSSION
Persistent SRF is a very common finding after successful SB surgery for macula-off RRD. Of the 59 eyes investigated in this study, 49 (83.1%) of patients with macula-off RRD showed persistent SRF 1mo after SB surgery, this finding is in line with previous reports. For example, Benson et al[5] performed OCT and identified persistent SRF in 82.5% of patients with macula-off RRD when evaluated 6wk after surgery. Similarly, Chantarasorn et al[4] reported an SRF incidence of 78.6% when evaluated 6wk after surgery. According to previous studies, persistent SRF can often be present for long periods of time before it is absorbed[2],[9],[13]. Our longitudinal follow-up showed that the mean duration of time required for complete SRF absorption was 13.2±10.0mo. However, OCT imaging showed clear evidence of SRF in 30% of cases 12mo after surgery, persistent SRF was eventually absorbed in all cases except one; one young male patient, with subretinal fibrosis and a 3-month history of 3 RRD, showed diffused SRF without absorption at his final follow-up visit, 4y after surgery. The long duration of SRF in this patient suggested that the condition was multifactorial, since the presence of SRF did not influence postoperative BCVA, we did not attempt to carry out additional procedures.
We investigated the relationships between a range of clinical factors and the presence or absence of SRF after surgery. We found that a younger age, and high myopia, may be associated with persistent SRF. Kim et al[6] also reported that a younger age was associated with persistent loculated SRF; however, the factors underlying this association remain unclear. We speculate that persistent SRF in younger patients may be related to the composition of the SRF itself. In younger patients, the vitreous is usually less liquefied and more viscous[14]. Mimouni et al[13] recently reported that SRF was significantly associated with high myopia, and suggested that a thinner and more degenerated RPE, as well as other features of chorioretinal atrophy, may be related to reduced pumping capabilities, thus restricting fluid resorption. Other factors, such as phakia and long-standing detachment, have also been linked with persistent SRF; however, our current results showed no significant associations with these variables.
It remains controversial as to whether SRF affects postoperative BCVA. Some researchers propose that persistent SRF may delay visual recovery but has no influence on the final outcome[11]. Our results are consistent with Seo et al[11] in that persistent SRF within 12mo of SB surgery for macula-off RRD may delay visual recovery but does not cause visual loss. All of our patients showed good but slow recovery in terms of the BCVA. Group comparisons further showed that the presence of persistent SRF after surgery did not correlate with final BCVA. In addition, BCVA values in patients with SRF at 1 and 3mo after surgery were worse than in patients without SRF. At the 6-month follow-up, there was no significant difference between the two groups in terms of visual outcome. Furthermore, the resolution of SRF was clearly associated with an improvement in visual acuity. However, some authors arrived at contradictory conclusions, and suggested that persistent SRF can influence visual outcome. For example, Benson et al[15] reported that SRF was associated with worse visual acuity at 6wk follow-up, we consider that these discrepancies were related to small sample sizes, and/or short follow-up periods. In addition, some studies utilized macula-on and macula-off conditions to calculate visual outcomes, thus reducing specificity. When comparing the speed of BCVA improvement between groups of patients with and without persistent SRF, we observed slower recovery in the group with SRF. Although persistent SRF may have influenced visual recovery over the short-term, it did not influence the final visual outcome.
By investigating the morphology of postoperative SRF, we identified three distinct patterns of SRF: BL, SD, and MB. More than half of the cases with persistent SRF (55.1%) showed the BL pattern. By comparing the different types of SRF, we identified that patients with BL located SRF required a shorter duration of time for fluid reabsorption compared with the two other types of SRF. SD SRF, and MB, tended to persist for a longer period of time. At the 24mo follow-up visit, all cases of BL SRF had been absorbed. We further found that it can take in excess of one year for the complete resolution of SD SRF and MB. At the 24mo follow-up visit, 10.2% of patients still possessed SRF. This suggested that the anatomical recovery of the retina may occur in a uniform manner. With increasing time after surgery, the SRF showed serial changes in morphology. For example, the width of the SRF blebs decreased gradually during the follow-up period until complete absorption. These findings were consistent with a recent retrospective study that described a progressive reduction in the width of SRF blebs over time[16]. Most cases of SD SRF that showed transformation into the MB type also featured either discontinuous or partial reattachment of the retina; subsequently, the extent of the SRF gradually reduced until it had been completely absorbed. In patients showing MB, we found that the size and number of blebs decreased gradually until they had been completely absorbed. It is likely that the speed of SRF absorption is associated with a range of factors, including volume, composition, viscosity, and the anatomical recovery of the RPE. Previous studies have identified high concentrations of a range of large molecules in long-standing cases of persistent SRF, including proteins, glycosaminoglycans, and cellular debris[17]–[18]. Other studies have identified the active transport of SRF from the subretinal space into the choroidal circulation via the RPE following surgery[19]. Experimental animal models have also demonstrated the irregular anatomical recovery of photoreceptor RPE apposition following retinal reattachment[20]. This finding may support the hypothesis that retinal reattachment may allow the RPE pumps to recover, thus increasing the absorptive capacity of the RPE, and thus inducing active absorption. It is also possible that the width of the SRF blebs may dictate the speed at which fluid is absorbed.
Our analyses revealed no significant differences between the incidences of the three types of SRF in relation to patient age, high myopia, lens status, or the location and extent of the RD. In a previous study, Kim et al[6] found that multiple SRF blebs were particularly prevalent in younger patients, but this was not replicated in our study. Furthermore, we did not find any significant differences in final visual outcomes for the three different patterns of SRF.
Retinal reattachment allows the restoration of photoreceptors; this process has been shown to be significantly associated with visual outcomes[21]. Another group reported that visual outcomes are strongly correlated with EZ integrity[22]. In the present study, the proportion of eyes with persistent SRF showing disruption in the EZ decreased from 36.2% at the 1-month visit, to 6.8% by the final follow-up visit. In contrast, the proportion of eyes with EZ disruption was 10% in the group of patients without persistent SRF, although this resolved by the final follow-up visit. A previous 5-year follow-up study, conducted by Rashid et al[23], concluded that disruption in the photoreceptor layer soon after surgery may eventually resolve. In the present study, we found that eyes with persistent SRF were more likely to demonstrate EZ and ELM disruption at the final follow-up visit. Although persistent SRF did not influence the final visual outcome, it was capable of causing harmful effects on the photoreceptors. Consequently, we recommend the active removal of as much SRF as possible.
This prospective study provides a detailed description of the patterns of persistent SRF, and determined how these patterns are associated with the natural time-course of SRF absorption following the repair of macula-involving RRD. Several limitations should be taken into consideration when interpreting our results. First, it is possible that the true incidence of SRF is higher than reported herein because OCT cannot scan peripheral areas of the retina. Second, we evaluated visual outcomes by measuring BCVA. Additional studies, incorporating other imaging modalities, such as fundus fluorescein angiography and microperimetry, are now needed to further elucidate how persistent SRF can be resolved and to elucidate the functional implications of these changes after RRD treatment. Third, we did not perform OCT until 1mo after surgery. Future studies should investigate the status of SRF at a much earlier timepoint as structural changes in the retina may be related to SRF resolution, and final visual function. Finally, patients without persistent SRF after the 12-month follow-up visit underwent OCT at 3-month intervals. Therefore, it is not possible to ascertain exactly when the SRF was completely absorbed.
In summary, this prospective study found a high incidence of SRF in patients following surgery for macula-off RRD, and that the SRF could be classified into three distinctive patterns. We also described the natural course of SRF and investigated its association with visual outcome in patients who underwent successful SB surgery for macula-off RRD. Persistent loculated SRF was identified in 83.1% of patients with macula-off RRD. Preoperative high myopia, and younger age, were significantly associated with persistent SRF. BL SRF was the most commonly identified pattern following successful SB surgery; this form also had the shortest duration. We also traced the natural course of SRF blebs until their complete absorption. BL SRF gradually disappeared as SRF volume decreased. Most cases with SD SRF showed transformation into MB SRF blebs over time. Furthermore, the size and number of MB SRF blebs decreased gradually until they were completely absorbed. Although the incidence and mean time duration required for complete SRF absorption were different across the three different patterns of SRF, there was a gradual recovery of visual acuity over time, and the specific pattern of SRF had no influence on final visual outcome. Finally, there was a gradual restoration in defects of the EZ and ELM during the course of SRF resolution throughout the follow-up period.
Acknowledgments
Conflicts of Interest: Fu Y, None; Chen S, None; Gu ZH, None; Zhang YL, None; Li LY, None; Yang N, None.
REFERENCES
- 1.Kim YK, Woo SJ, Park KH, Yu YS, Chung H. Comparison of persistent submacular fluid in vitrectomy and scleral buckle surgery for macula-involving retinal detachment. Am J Ophthalmol. 2010;149(4):623–629.e1. doi: 10.1016/j.ajo.2009.11.018. [DOI] [PubMed] [Google Scholar]
- 2.Huang CM, Fu T, Zhang TH, Wu XY, Ji Q, Tan RL. Scleral buckling versus vitrectomy for macula-off rhegmatogenous retinal detachment as accessed with spectral-domain optical coherence tomography: a retrospective observational case series. BMC Ophthalmol. 2013;13:12. doi: 10.1186/1471-2415-13-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ricker LJ, Noordzij LJ, Goezinne F, Cals DW, Berendschot TT, Liem AT, Hendrikse F, La Heij EC. Persistent subfoveal fluid and increased preoperative foveal thickness impair visual outcome after macula-off retinal detachment repair. Retina. 2011;31(8):1505–1512. doi: 10.1097/IAE.0b013e31820a6910. [DOI] [PubMed] [Google Scholar]
- 4.Chantarasorn Y, Oellers P, Eliott D. Choroidal thickness is associated with delayed subretinal fluid absorption after rhegmatogenous retinal detachment surgery. Ophthalmol Retina. 2019;3(11):947–955. doi: 10.1016/j.oret.2019.05.009. [DOI] [PubMed] [Google Scholar]
- 5.Benson SE, Schlottmann PG, Bunce C, Xing W, Charteris DG. Optical coherence tomography analysis of the macula after scleral buckle surgery for retinal detachment. Ophthalmology. 2007;114(1):108–112. doi: 10.1016/j.ophtha.2006.07.022. [DOI] [PubMed] [Google Scholar]
- 6.Kim YK, Ahn J, Woo SJ, Hwang DJ, Park KH. Multiple subretinal fluid blebs after successful retinal detachment surgery: incidence, risk factors, and presumed pathophysiology. Am J Ophthalmol. 2014;157(4):834–841. doi: 10.1016/j.ajo.2013.12.030. [DOI] [PubMed] [Google Scholar]
- 7.Kim JM, Lee EJ, Cho GE, Bae K, Lee JY, Han G, Kang SW. Delayed absorption of subretinal fluid after retinal reattachment surgery and associated choroidal features. Korean J Ophthalmol. 2017;31(5):402–411. doi: 10.3341/kjo.2016.0033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Borowicz D, Nowomiejska K, Nowakowska D, Brzozowska A, Toro MD, Avitabile T, Jünemann AG, Rejdak R. Functional and morphological results of treatment of macula-on and macula-off rhegmatogenous retinal detachment with pars plana vitrectomy and sulfur hexafluoride gas tamponade. BMC Ophthalmol. 2019;19(1):118. doi: 10.1186/s12886-019-1120-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wolfensberger TJ, Gonvers M. Optical coherence tomography in the evaluation of incomplete visual acuity recovery after macula-off retinal detachments. Graefes Arch Clin Exp Ophthalmol. 2002;240(2):85–89. doi: 10.1007/s00417-001-0410-6. [DOI] [PubMed] [Google Scholar]
- 10.Theodossiadis PG, Georgalas IG, Emfietzoglou J, Kyriaki TE, Pantelia E, Gogas PS, Moschos MN, Theodossiadis GP. Optical coherence tomography findings in the macula after treatment of rhegmatogenous retinal detachments with spared macula preoperatively. Retina. 2003;23(1):69–75. doi: 10.1097/00006982-200302000-00011. [DOI] [PubMed] [Google Scholar]
- 11.Seo JH, Woo SJ, Park KH, Yu YS, Chung H. Influence of persistent submacular fluid on visual outcome after successful scleral buckle surgery for macula-off retinal detachment. Am J Ophthalmol. 2008;145(5):915–922. doi: 10.1016/j.ajo.2008.01.005. [DOI] [PubMed] [Google Scholar]
- 12.Mao JB, Lin JJ, Yu XT, Cheng D, Chen YQ, Tao JW, Wu HF, Jiang L, Zhang Y, Shen LJ. Comparison of persistent submacular fluid in different preoperative macular status after vitrectomy for rhegmatogenous retinal detachment. Int J Ophthalmol. 2018;11(11):1796–1801. doi: 10.18240/ijo.2018.11.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mimouni M, Jaouni T, Ben-Yair M, Almus S, Derman L, Ehrenberg S, Almeida D, Barak Y, Zayit-Soudry S, Averbukh E. Persistent loculated subretinal fluid after rhegmatogenous retinal detachment surgery. Retina. 2020;40(6):1153–1159. doi: 10.1097/IAE.0000000000002565. [DOI] [PubMed] [Google Scholar]
- 14.Abouzeid H, Becker K, Holz FG, Wolfensberger TJ. Submacular fluid after encircling buckle surgery for inferior macula-off retinal detachment in young patients. Acta Ophthalmol. 2009;87(1):96–99. doi: 10.1111/j.1755-3768.2008.01196.x. [DOI] [PubMed] [Google Scholar]
- 15.Benson SE, Schlottmann PG, Bunce C, Xing W, Charteris DG. Optical coherence tomography analysis of the macula after vitrectomy surgery for retinal detachment. Ophthalmology. 2006;113(7):1179–1183. doi: 10.1016/j.ophtha.2006.01.039. [DOI] [PubMed] [Google Scholar]
- 16.Gharbiya M, Malagola R, Mariotti C, Parisi F, de Vico U, Ganino C, Grandinetti F. Spectral-domain optical coherence tomography analysis of persistent subretinal fluid after scleral buckling surgery for macula-off retinal detachment. Eye (Lond) 2015;29(9):1186–1193. doi: 10.1038/eye.2015.113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Quintyn JC, Brasseur G. Subretinal fluid in primary rhegmatogenous retinal detachment: physiopathology and composition. Surv Ophthalmol. 2004;49(1):96–108. doi: 10.1016/j.survophthal.2003.10.003. [DOI] [PubMed] [Google Scholar]
- 18.Veckeneer M, Derycke L, Lindstedt EW, van Meurs J, Cornelissen M, Bracke M, van Aken E. Persistent subretinal fluid after surgery for rhegmatogenous retinal detachment: hypothesis and review. Graefes Arch Clin Exp Ophthalmol. 2012;250(6):795–802. doi: 10.1007/s00417-011-1870-y. [DOI] [PubMed] [Google Scholar]
- 19.Negi A, Marmor MF. The resorption of subretinal fluid after diffuse damage to the retinal pigment epithelium. Invest Ophthalmol Vis Sci. 1983;24(11):1475–1479. [PubMed] [Google Scholar]
- 20.Immel J, Negi A, Marmor MF. Acute changes in RPE apical morphology after retinal detachment in rabbit. A SEM study. Invest Ophthalmol Vis Sci. 1986;27(12):1770–1776. [PubMed] [Google Scholar]
- 21.Karacorlu M, Sayman Muslubas I, Hocaoglu M, Arf S, Ersoz MG. Correlation between morphological changes and functional outcomes of recent-onset macula-off rhegmatogenous retinal detachment: prognostic factors in rhegmatogenous retinal detachment. Int Ophthalmol. 2018;38(3):1275–1283. doi: 10.1007/s10792-017-0591-6. [DOI] [PubMed] [Google Scholar]
- 22.Kang HM, Lee SC, Lee CS. Association of spectral-domain optical coherence tomography findings with visual outcome of macula-off rhegmatogenous retinal detachment surgery. Ophthalmologica. 2015;234(2):83–90. doi: 10.1159/000381786. [DOI] [PubMed] [Google Scholar]
- 23.Rashid S, Pilli S, Chin EK, Zawadzki RJ, Werner JS, Park SS. Five-year follow-up of macular morphologic changes after rhegmatogenous retinal detachment repair: Fourier domain OCT findings. Retina. 2013;33(10):2049–2058. doi: 10.1097/IAE.0b013e3182891e81. [DOI] [PMC free article] [PubMed] [Google Scholar]