Abstract
Introduction
Social prescribing aims to address social determinants of health, which account for 80%–90% of health outcomes, but the evidence base behind it is limited due to a lack of data linkingsocial prescribing activity and outcomes.
Methods and analysis
The objective of the quantitative component of this feasibility studyisto identify the characteristics of individuals who receive social prescriptions and describe the use and estimate the impact of social prescribing; the latter will be done on a homeless subgroup. We will use the Oxford Royal College of General Practitioners (RCGP) Research and Surveillance Centre (RSC) primary care sentinel network, whose general practicescover a population of over 4 000 000 patients. Social prescribing data will be extracted onall recorded patients for 5 years up to 31 January 2020. The objective for the qualitative component of the study isto explore approaches to understand the contextual factors that will have influenced our quantitative findings to identify mechanisms to encourage adoption of social prescribing in primary care while improving data quality. Itwill comprise up to three 90–120 minute advisory group meetings for six to eight participants. Participants will be recruited based on their experience of delivering primary care within Oxfordshire and Surrey. The advisory group outputs will be analysed using framework analysis and will be used to create a survey instrument consisting of statements that surveyees, who will consist of primary care practitioners within the RCGP RSC, can agree or disagree with.
Ethics and dissemination
All RCGP RSC data are pseudonymised at the point of data extraction. No personally identifiable data are required for this investigation. This protocol follows the Good Reporting of a Mixed Methods Study checklist. The study results will be published in a peer-reviewed journal and the dataset will be available to other researchers.
Keywords: social prescribing, health informatics, primary care, social determinants of health
Strengths and limitations of this study.
A key strength of this feasibility study is that it uses an established and nationally representative sentinel network, The Royal College of General Practitioners Research Surveillance Centre, which provides access to a large sample of real-world evidence data that has a high level of data completeness.
The practical and feasible approaches identified through our project could be adopted by National Health Service Digital and rolled out nationally across England, yielding information to improve our understanding of the current use and impact of social prescribing and also help to elucidate the best practice for social prescribing.
A limitation is that though nationally representative, because general practitioner practices participate on a voluntary basis, there is slight under-representation of practices with more deprived patients, which means there may be some selection bias.
Another limitation is that the identification of patient output and outcome metrics will be restricted by primary care clinical codes (ie, Readv2, CTV3), which do not always align directly with the output and outcome metrics of interest.
Introduction
It is well established that 80%–90% of health outcomes are linked social determinants of health including health-related behaviours, socioeconomic and environmental factors.1
Societies that enable all citizens to play a full and useful role in the social, economic and cultural life of their society will be healthier than those where people face insecurity, exclusion and deprivation.2
Since the 19th century, there have been initiatives such as social medicine3 and community health4 designed to address these social determinants of health at individual and community levels. There are subtle differences between these initiatives but they all largely focus on needs that remain unaddressed in traditional biomedical models.
Social prescribingis a more recent initiative that has been developed to address social determinants of health. Social prescriptions have been used for several years across European countries. National Health Service (NHS) England defines social prescribing as ‘a way of linking patients in primary care with sources of support within the community to help improve their health and well-being’.5 Social prescriptions are varied and include activities focused on health, education, skills development, sports and leisure/art activities. If used well, they can help to deliver several benefits to individuals and health and care systems including5: giving a route for health and care systems to address social determinants of health; promoting self-care; support job creation by funnelling resources to local Voluntary, Community and Social Enterprise organisations; building stronger communities; reducing service utilisation including general practitioner (GP) appointments, secondary care referrals and accident and emergency attendances.
A wide variety of approaches are included within the umbrella of social prescriptions. A 2017 systematic review6 indicated that while there have been 15 studies into the effects of social prescriptions, none were of sufficient quality to allow a strong recommendation for their use. Since 2017, studies using quantitative and qualitative methods have been done to determine the impact of social prescribing but most of these studies have had small sample sizes that may not have been representative of the full breadth of individuals receiving social prescriptions.7 8 More robust evidence is required to strategically inform the development of social prescriptions and to establish social prescriptions as an evidence-based intervention that clinicians feel comfortable in regularly using.
A major barrier to the generation of evidence that could facilitate evaluation of social prescribing is the lack of data on what social prescribing activity is taking place and the outcomes delivered for people taking up social prescribing. This stems from the lack of standardisation of recording, a limited list of formal codes associated with social prescribing as well as likely variation in the uptake, use and quality of data recorded by clinicians.
To address these barriers and overcome some of the challenges faced with other studies, we propose a feasibility study using a large nationally representative dataset of English general practice to enable us to test approaches to understand the use and impact of social prescriptions. English general practice is an ideal location to assess the feasibility of measuring the uptake and impact of social prescribing. English general practices have a registration-based system (one patient registered with a single practice) and are highly computerised.9 Computerised medical record (CMR) systems have been widely used for measuring quality and outcomes in general practice. Where data are likely to be complex, as we anticipate in this study, ontologies provide a formal method to specify how we will measure the uptake and impact of social prescribing.10 11
We can readily access a nationally representative sample of data through the Oxford Royal College of General Practitioners Research Surveillance Centre (RCGPRSC) sentinel network. The RSC is one of the longest established primary care sentinel networks in Europe, currently consisting of over 1000 generalresearch ready practices and covering a population of over 4 000 000 patients, who are broadly representative of the English population.12 13 The RCGPRSC’s dataset consists of twice weekly pseudonymised coded extracts of general practice electronic health record (EHR) data from all major clinical systems.12 13 Finally, England is also an ideal location for this feasibility study because there is a strong national push to promote social prescribing as a mechanism to improve patient and population outcomes while optimising resource utilisation (box 1).
Box 1. Social prescribing in the English context.
Social prescribing is part of National Health Service (NHS) England’s commitment, as highlighted in the NHS England Long-Term Plan,31 to make personalised care business as usual across the health and care system. In January 2019, as part of its Universal Personalised Care Plan,32 NHS England announced a major expansion of social prescribing, as one of six components of the comprehensive model of personalised care. NHS England has produced a standard model, the link worker model, of social prescribing in partnership with stakeholders and it has created reference guidance33 34 that provides advice on implementing this link worker model.
To begin to address the gap in the evidence base around social prescriptions, NHS England worked with commissioners, practitioners, providers, evaluators and other stakeholder groups to create a consensus Common Outcomes Framework (COF)15 on what outcomes and outputs should be measured to demonstrate the impact of social prescribing. Feedback from a wide range of stakeholders (including social prescribing connector schemes, primary care staff, local authorities, local NHS, voluntary, community and social enterprises organisations, academics, researchers, public health leaders and other government agencies) was collected to inform the COF. The reference guide encourages the use of SNOMED codes to record social prescribing in patient records as well as the patient activation measure and the Office of National Statistics (ONS) well-being Measure to capture outcomes being delivered to patients.
Aim
This feasibility study will enable us to test approaches to understand the use and impact of social prescriptions.
Objectives
Our objectives encompass the exploration of the development of measurement tools, measuring use and impacts as well as feeding back on variation between practices which may be the result of data quality as well as variation in care.
To identify the characteristics of the individuals who are provided, or decline social prescriptions and the patient and health service outcomes related to their social prescription, the latter of which will be done on a subgroup of individuals recorded as being homeless.
To develop a taxonomy and ontology to capture social prescribing referrals and interventions made in primary care
To report inter practice variation and to explore opportunities to improve data quality and the quality of social prescribing in primary care.
To explore the feasibility and willingness of primary care practitioners, including GPs and link workers, to routinely collect data (eg, uptake, service use, health/well-being measures) and to use it to evaluate impact of the social prescribing link worker model.
Methods and analysis
Study design
This feasibility study will enable us to test approaches to understand the use and impact of social prescriptions. Our study follows the Good Reporting of a Mixed Methods Study checklist.14 The study protocol combines qualitative and quantitative methods and will explore how the RCGP RSC can be used to establish the baseline of existing data, understand outcomes delivered and to explore approaches that can be used to understand and influence how link-worker based models are being implemented in English general practices.
The quantitative methods (WP1) will use the RCGP RSC database to test approaches to identify the use and impact of social prescribing.12 13 The qualitative methods (WP2) comprise advisory group meetings that will be carried out with individuals with experience of primary care, which will be used to inform the design of a survey that will be disseminated to a wider group of primary care practitioners within the RCGP RSC. WP2 will help us explore approaches tounderstand the contextual factors that will have influenced our quantitative findings with the goal of identifying mechanisms to encourage adoption of social prescribing in primary care while improving data quality.
Study setting and sample
For WP1, we will use the sample of over 1000 nationally representative GP practices contained within the RCGP RSC.12 13 For WP2, we will approach and recruit people in person and through existing departmental contacts within the University of Oxford and University of Surrey Departments of Primary Care as well as through our contacts within primary care networks in Oxfordshire and Surrey, where members of our study team work. Individuals will be recruited if they haveany experience working within primary care (which will include GPs, practice nurses, allied health professionals and link workers)and are within travelling distance of the University of Oxford or the University of Surrey to attend advisory group meetings on our premises or via a virtual platform if circumstances do not permit face to face meetings (eg, because of COVID-19).
Data collection and data management
Data collection from volunteer RCGP RSC practices
For this project, we propose to use the RCGP RSC sentinel network. The RCGP RSC was established in 1967 and comprises CMRs of pseudonymised data received from over 1000 primary care practices across England, covering a population of over 4 000 000 currently registered patients.12 13
RCGP RSC data are registration based, so that every patient is registered with only one practice at a time with each patient having a unique patient identifier, the NHS number. The NHS number enables the transition of a patient’s medical record to another practice when he/she moves to a different location and for the patient’s data to link with secondary care and other datasets.9 Although within this study we will use pseudonymised NHS number throughout following RCGP RSC processes.
CMR data in UK primary care are captured primarily within two EHR systems which use Read and CTV3 codes; both systems, however, will be transitioning to SNOMED CT. Read, CTV3 and SNOMED CT codes are used to collate data for primary care including diagnoses, processes of care, prescriptions and results from laboratory-based data.
We will extract and analyse coded data from primary care practices for 5 years up to 31 January 2020. The data extract will include all instances of use of the codes highlighted in table 1, which were derived from the NHS Outcomes Framework for social prescribing.15
Table 1.
NHS Common Outcomes Framework (COF) for social prescribing codes
| Readv2 | CTV3 | SNOMED CT | Term description |
| 9NSE. | 9NSE. XaaEA |
871691000000100 | Social prescribing offered (finding) |
| 8IEp. | 8IEp. XaaEB |
871711000000103 | Social prescribing declined (situation) |
| 8T09. | 8T09. XaaEC |
871731000000106 | Referral to social prescribing service (procedure) |
| XagOR | 1084281000000109 | Signposting to social prescribing service (procedure) | |
| 8BAf. |
8BAf. XaQvz |
515721000000104 | Social prescribing for mental health (regime/therapy) |
NB: codes in italics are not in the COF but will be included in the data extract.
NHS, National Health Service.
We will also explore other ways of capturing information on the use of social prescribing through the use of a social prescribing ontology. Ontologies are frequently used in healthcare for modelling the semantics of medical concepts and to facilitate exchange of medical data between different healthcare service providers.16 The social prescribing ontology will be underpinned by a taxonomy based on concepts associated with social prescribing practices and the well-being of social prescribing recipients. The primary purpose of the taxonomy and ontology is to harmonise data sources containing measures and indicators of social prescribing across various parts of the health system (figure 1).
Figure 1.
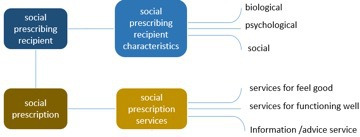
Upper level design of the social prescribing ontology.
The taxonomy will cover several key concepts derived from the five ways to well-being model proposed by the New Economics Foundation17 as well as Wilkinson and Marmot’s2 work on social factors related to health. The concepts will include social gradient, stress, early life, social exclusion, work/unemployment, social support, addiction, food, transport, ethnic inequalities, health inequalities at older ages, neighbourhood housing and health, sexual behaviours. The ontology will describe these key concepts used within social prescribing. The social prescribing recipient will have one of more characteristics that would qualify them as a social prescribing recipient. In the ontology, these characteristics will be organised according to the biopsychosocial model.18 The healthcare provider will consider these characteristics and decide if a social prescription will be beneficial. The social prescription will enable the social prescribing recipient to access one or more social prescription services. In addition to the services relevant to these concepts, we have also included an additional category, ‘information/advice service’ which includes a range of services that do not fit directly within the scope of original conceptual model of well-being or social factors related to health, but have an indirect effect on well-being.
The social prescribing ontology has been implemented according to the web ontology language within the Protégé ontology development environment and hosted on the BioPortal ontology repository.19
Advisory groups and surveys
Advisory groups
The advisory groups will comprise up to eight participants and will adopt methods and best practice normally used for focus groups20 and will last between 90 and 120 min. The moderator will introduce the discussion topics, monitor the group dynamics to ensure views from all participants are adequately represented and to ensure all discussion topics are covered. A second moderator will take detailed notes of the discussion and help the moderator to keep to time. The advisory groups will be recorded and transcribed verbatim.21
The discussion topics were agreed in consultation with the NHS England personalised care team working on social prescribing. The key topics will include:
Understanding if and how social prescribing schemes are being used by primary care and how social prescribing activity is currently being recorded.
Understanding link worker-based models of social prescribing (including: estimation of investment in social prescribing schemes; estimation of number of link workers; referral process and pathways, eg, who refers into the scheme; estimation of average amount of time link workers spend with patients; estimation of community groups referred to and numbers of volunteers; nature of community groups referred to; estimation of number of personalised support plans co-produced with people receiving support).
Understanding if there a change in morale of primary care staff.
Exploring views on the impact of these different models on patients (eg, through measures like the Patient Activation Measure (PAM) and ONS well-being measure) and primary care (eg, number of GP appointments, prescriptions for patients, number of secondary referrals).
Exploring approaches that could be used to support primary care to improve data quality and recording of data related to social prescribing, including outcome and output metrics outlined in the NHS England Social Prescriptions Common Outcomes Framework (COF).
Surveys
We will use the findings from the advisory groups to develop an online survey to capture the degree of consensus with our advisory group findings. The surveys will be sent to primary care practitioners within the RCGP RSC and include statements for respondents to agree or disagree with. There will also be an opportunity for the respondents to explain why they agree or disagree with a statement.
Data management
Where available, the following output and outcome information derived from the social prescribing COF15 will be analysed for the study:
Output metrics
Characteristics of people referred: age, disability, gender reassignment, marriage or civil partnership, pregnancy and maternity, race, religion or belief, sex, sexual orientation.
Referral criteria such as long-term conditions or receipt of social care packages.
Outcome metrics: impact on patients and health and care system
PAMs.
ONS well-being measures.
GP consultations.
Accident and Emergency (A&E) attendance.
Hospital bed days.
Number of medication prescriptions.
Data analysis
Statistical and modelling analysis
Descriptive statistics will be used to report the findings and will focus on two key domains:
Social prescription use: Use of social prescribing will be identified using the codes listed in table 1 as well as through the use of a social prescribing ontology. We will explore the use of both approaches individually and in combination to identify the method that works best.
Social prescription impact: We will explore methods to determine the impact of social prescribing by focusing on individuals recorded as being homeless, which is a subgroup that the RCGP RSC team is working with for other projects:
-
We will first identify individuals who have received a social prescription and who are recorded as being homeless. We will then explore methods to determine the details of the social prescription(s) they have received from the existing RCGP RSC data (eg, frequency, adherence, type of social prescription).
Where available, we will attempt identify any additional clinical conditions of the individuals referred.
-
Where available, we will attempt to identify the characteristics of people referred (see output metrics above).
We will attempt to identify matched cohorts of homeless people with similar characteristics but who did not receive a social prescription.
Where available, identify the outcomes (see outcome metricsabove) for both cohorts of homeless people.
The goal of these analyses will be to explore if the RCGP RSC can be used to accurately capture the use and impact of social prescribing.
Analysis of advisory groups
QSR NVivo V.11 and Microsoft Excel will be used to organise and analyse advisorygroup meeting outputs.22We will use Framework Analysis, a well-established approach to observe similarities, discrepancies and inter-relationships among the data.23 Framework Analysis consists of a five-step process including24:
Familiarisation: reading the transcripts, reflecting on the research question and keeping notes of potential ideas and recurring concepts.
Identifying a thematic framework: using a priori knowledge of the literature as well as the concepts from the first step to create a framework/index to sort the new material into a descriptive list of concepts that will be refined to represent the diversity, centrality and dynamics of participants’ attitudes.
Indexing: systematically applying the framework to the data, using a numerical system that will link them directly to the index. A second analyst will also use the framework to test the transparency of the method and compare his/her assumptions with the first analyst’s.
Charting: the indexes will be used to create thematic charts, which will include a refined summary of major subjects that will have emerged in order to provide a more abstract view of the data.
Mapping and interpretation: interpreting the data as a whole.
For the survey, summary statistics will be used to describe the results based on key themes interrogated in the survey. The outputs of the survey will be used to identify opportunities and barriers at multiple levels:
Individual stakeholder level.
GP practice level.
Regional level.
Survey results will be used to inform the survey design for a larger and subsequent study.
Patient and public involvement
No patients or public were involved in the development of the research question or design of this study. For the advisory group meetings, the GP practices we engage with for this study will be asked to invite patients who would be willing toserve on our advisory group and/or anonymously comment on the advisory group themes, as per National Institutes of Health Research (NIHR) Involve guidelines.25
Project management
The feasibility study will be a collaborative project led by AJ and SdeL, with Simon de Lusignan serving as the principal investigator. RCGP and NHS England will be collaborators and will oversee the project in collaboration with the principal investigator. The research and information governance framework for RCGP RSC sits within the University of Surrey’s formal frameworks for information and research governance. The project team is supported by IT services dedicated to the Faculty and to the Department of Clinical and Experimental Medicine. Our secure analysis servers are optimised for routine healthcare data processing, to provide faster deliveries for our projects.
Ethics and dissemination
Ethics
For WP1, consent will not be required for these data and we will not process data for people where opt-out codes are present, which is currently 2.74%.26 The data will be pseudonymised and encrypted before uploading to the Clinical Informatics Research Group secure server. Personal data will not be identifiable. This study is considered to be an ‘Audit of current practice’ when tested against the Health Research Authority/Medical Research Council ‘Is my study research’ tool and, therefore, does not require specific ethical approval.27 Approval for use of the data was acquired from the RCGP RSC Study Approval Committee.
Data extractions will be conducted in accordance with the Clinical Informatics and Health Outcomes Research Group’s standard operating procedures for data extraction, pseudonymisation and transfer described previously.28
Pseudonymisation, the standard approach for protecting patient’s privacy defined by the European Data Protection Supervisor,29 involves the removal of all personal identifiers from data—such as name, date of birth. To minimise the risk of reidentification, all strong identifiers (in this study, NHS number) are removed and data are kept encrypted during transfer and are stored on a secure network that meets NHS Information Governance standards.29 For this study we need, for example, to be able to link outcome and output metrics (see below) associated with the patient before and after receiving a social prescription. Pseudonymisation allows us to do this without knowing any of the strong personal identifiers of that individual. All data processing and analysis in the present proposed study will be conducted within the secure IT environment of the Clinical Informatics and Health Outcomes Research Group, at the University of Surrey. The information security policies and procedures of the Research Group have been approved by the NHS Digital as meeting the Data Security and Privacy standards psuedonymising as close to sources as possible. If patients have opted out of record sharing, we will not analyse their data.
For WP2 where participants in the advisory group meetings are serving as advisors rather than research participants, University of Surrey Self-Assessment for Governance and Ethics30 assessment indicated that a further ethics and governance application was not necessary for the analyses linked to this part of the feasibility study.
Dissemination
The outputs from our research will highlight and capture findings linked to our four objectives, namely:
An analysis of social prescribing use across the RCGP RSC.
An analysis of the NHS COF social prescribing codes versus the codes from our ontology.
An overview of approaches used to determine how the impact of social prescribing could be estimated from different analytical approaches.
An analysis highlighting the findings from our advisory group meetings about different social prescribing models used by practitioners and their willingness to use routine data collection to improve data quality and the outcomes that could be delivered by social prescribing.
The outputs from the research will be disseminated primarily through peer-reviewed papers in high-impact journals within the domains of primary care and health and care systems. We will also present findings at relevant seminars and conferences.
Discussion
Our feasibility study aims to enable us to test approaches to understand the use and impact of social prescriptions. We look to achieve this aim through several objectives including: reporting baseline levels of social prescription utilisation and the patients within practices who are provided social prescriptions; establishing a social prescribing taxonomy/ontology that can capture social prescribing referrals and interventions made in primary care; establishing what data can be made available to practices to highlight inter practice variation; establishing what data can be used to enable future evaluation of social prescribing; exploring approaches to understand the contextual factors that will have influenced our quantitative findings and which can inform the design and development of a more effective taxonomy/ontology for social prescribing; and ultimately helping us understand and encourage adoption of social prescribing in primary care while improving data quality. For the quantitative analyses, we will focus on the specific subgroup of those who are homeless to better understand how they can be identified through the RCGP RSC and to explore whether we can identify the interventions they received and the outcomes delivered to them.
Below we outline several strengths of our study and as well as some limitations which we hope to overcome.
Strengths
The key strength of this feasibility study is that is uses an established and nationally representative sentinel network. The practices within the sentinel network are nationally representative and they provide access to a sample of real world evidence data to quantify current national use of social prescribing. Further to this, the large sample size of this representative dataset and the high-level data completeness of the data are particular strengths of the RCGP RSC dataset.
We think that the introduction of a standard methodology for adoption and delivery of social prescribing by GP practices could increase the chances of being able to show benefits. Furthermore, the recording of detailed information on social prescribing (including type, treatment duration, costs and outcomes) is also needed to facilitate the adoption and improvement in the use of social prescriptions. The practical and feasible approaches identified through our project could be adopted by NHS Digital and rolled out nationally across England, yielding information to improve our understanding of the current use and impact of social prescribing and also help to elucidate best practice for social prescribing. Furthermore, our findings could also serve as a source of information for other countries looking to introduce social prescribing into their health and care systems.
Limitations
Though nationally representative, because GP practices participate on a voluntary basis, there is slight underrepresentation of practices with more deprived patients,13 which means there may be some selection bias. Furthermore, identification of patient output and outcome metrics will be restricted by primary care clinical codes (ie, Read, CTV3), which do not always align directly with the output and outcome metrics of interest. Finally, because of the limited number of people we can recruit for the advisorygroup meetings and survey, the experiences of the primary care practitioners we recruit for WP2 will be limited and may not be able to capture the contextual factors experienced by the entire sentinel network.
We will report additional strengths and limitations identified while undertaking the study in the final manuscript.
Conclusion
This feasibility study will enable us to test approaches to understand the use and impact of social prescriptions. Once established, we plan on using our approaches to create a dashboard for GP practices to understand their use of social prescriptions in near real time.
Supplementary Material
Acknowledgments
Practices and patients of the Royal College of General Practitioners Research and Surveillance Centre (RCGP RSC), who allowed their pseudonymised clinical medical records to be used for this study.
Footnotes
Twitter: @Lusignan_S
Contributors: AJ, HL, UH, LM, FF, IY and SdL were involved in the design of the study protocol; AJ, HL, LM, VTB and SdL were involved in writing and reviewing the manuscript.
Funding: This work was commissioned by the Royal College of General Practitioners and NHS England.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Patient consent for publication: Not required.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Hood CM, Gennuso KP, Swain GR, et al. . County health rankings: relationships between determinant factors and health outcomes. Am J Prev Med 2016;50:129–35. 10.1016/j.amepre.2015.08.024 [DOI] [PubMed] [Google Scholar]
- 2.The WHO Social determinants of health: the solid facts. 2nd edn, 2019. http://www.euro.who.int/__data/assets/pdf_file/0005/98438/e81384.pdf [Google Scholar]
- 3.Han DS, Bae S-S, Kim D-H, et al. . Origins and evolution of social medicine and contemporary social medicine in Korea. J Prev Med Public Health 2017;50:141–57. 10.3961/jpmph.16.106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.A discussion document on the concept and principles of health promotion. Health Promot Int 1986;1:73–6. 05; 10.1093/heapro/1.1.73 [DOI] [PubMed] [Google Scholar]
- 5.NHS England Social prescribing and community-based support: Summary guide [Internet]. Available: https://www.england.nhs.uk/wp-content/uploads/2019/01/social-prescribing-community-based-support-summary-guide.pdf [Accessed 12 Apr 2019].
- 6.Bickerdike L, Booth A, Wilson PM, et al. . Social prescribing: less rhetoric and more reality. A systematic review of the evidence. BMJ Open 2017;7:e013384. 10.1136/bmjopen-2016-013384 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Carnes D, Sohanpal R, Frostick C, et al. . The impact of a social prescribing service on patients in primary care: a mixed methods evaluation. BMC Health Serv Res 2017;17:835. 10.1186/s12913-017-2778-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Woodall J, Trigwell J, Bunyan A-M, et al. . Understanding the effectiveness and mechanisms of a social prescribing service: a mixed method analysis. BMC Health Serv Res 2018;18:604. 10.1186/s12913-018-3437-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.de Lusignan S, van Weel C. The use of routinely collected computer data for research in primary care: opportunities and challenges. Fam Pract 2006;23:253–63. 10.1093/fampra/cmi106 [DOI] [PubMed] [Google Scholar]
- 10.de Lusignan S. In this issue: ontologies a key concept in informatics and key for open definitions of cases, exposures, and outcome measures. J Innov Health Inform 2015;22:170. 10.14236/jhi.v22i2.170 [DOI] [PubMed] [Google Scholar]
- 11.Liaw S-T, Taggart J, Yu H, et al. . Integrating electronic health record information to support integrated care: practical application of ontologies to improve the accuracy of diabetes disease registers. J Biomed Inform 2014;52:364–72. 10.1016/j.jbi.2014.07.016 [DOI] [PubMed] [Google Scholar]
- 12.de Lusignan S, Correa A, Smith GE, et al. . RCGP research and surveillance centre: 50 years' surveillance of influenza, infections, and respiratory conditions. Br J Gen Pract 2017;67:440–1. 10.3399/bjgp17X692645 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Correa A, Hinton W, McGovern A, et al. . Royal College of general practitioners research and surveillance centre (RCGP RSC) sentinel network: a cohort profile. BMJ Open 2016;6:e011092. 10.1136/bmjopen-2016-011092 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.O'Cathain A, Murphy E, Nicholl J. The quality of mixed methods studies in health services research. J Health Serv Res Policy 2008;13:92–8. 10.1258/jhsrp.2007.007074 [DOI] [PubMed] [Google Scholar]
- 15.NHS England Social prescribing and community-based support: Summary guide [Internet]. Available: https://www.england.nhs.uk/publication/social-prescribing-and-community-based-support-summary-guide/ [Accessed cited 2020 Jan 26].
- 16.Liyanage H, Krause P, De Lusignan S. Using ontologies to improve semantic interoperability in health data. J Innov Health Inform 2015;22:309–15. 10.14236/jhi.v22i2.159 [DOI] [PubMed] [Google Scholar]
- 17.Aked JO, Marks N, Cordon CO, et al. . Five ways to wellbeing: a report presented to the Foresight Project on communicating the evidence base for improving people’s well-being. London: new economics foundation, 2008. [Google Scholar]
- 18.Engel GL. The clinical application of the biopsychosocial model. Am J Psychiatry 1980;137:535–44. 10.1176/ajp.137.5.535 [DOI] [PubMed] [Google Scholar]
- 19.Bioportal Social prescribing ontology [Internet]. Available: https://bioportal.bioontology.org/ontologies/SOCPRES [Accessed 26 Jan 2020].
- 20.Kitzinger J. Qualitative research. introducing focus groups. BMJ 1995;311:299–302. 10.1136/bmj.311.7000.299 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care 2007;19:349–57. 10.1093/intqhc/mzm042 [DOI] [PubMed] [Google Scholar]
- 22.Zamawe FC. The implication of using NVivo software in qualitative data analysis: evidence-based reflections. Malawi Med J 2015;27:13–15. 10.4314/mmj.v27i1.4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gale NK, Heath G, Cameron E, et al. . Using the framework method for the analysis of qualitative data in multi-disciplinary health research. BMC Med Res Methodol 2013;13:117. 10.1186/1471-2288-13-117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ritchie J, Lewis J. Qualitative research practice: a guide for social science students and researchers. London: Sage, 2013. [Google Scholar]
- 25.National Institutes of Health Research INVOLVE: Briefing notes for researchers:public involvement in NHS, public health and social care research [Internet]. Available: https://www.invo.org.uk/wp-content/uploads/2014/11/9938_INVOLVE_Briefing_Notes_WEB.pdf [Accessed 30 Apr 2020].
- 26.NHS Digital National data opt-out, March 2019 [Internet]. Available: https://digital.nhs.uk/data-and-information/publications/statistical/national-data-opt-out/march-2019/ndop-mar19 [Accessed 30 Apr 2020].
- 27.Health Research Authority Is my study research? [Internet]. Available: http://www.hra-decisiontools.org.uk/research/ [Accessed 26 Jan 2020].
- 28.de Lusignan S, Borrow R, Tripathy M, et al. . Serological surveillance of influenza in an English sentinel network: pilot study protocol. BMJ Open 2019;9:e024285. 10.1136/bmjopen-2018-024285 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.de Lusignan S, Metsemakers JF, Houwink P, et al. . Routinely collected general practice data: goldmines for research? A report of the European Federation for medical informatics primary care informatics Working Group (EFMI PCIWG) from MIE2006, Maastricht, the Netherlands. Inform Prim Care 2006;14:203–9. 10.14236/jhi.v14i3.632 [DOI] [PubMed] [Google Scholar]
- 30.University of Surrey Welcome to SAGE: Self-Assessment for Governance and Ethics [Internet]. Available: https://surrey.onlinesurveys.ac.uk/sage-1 [Accessed 26 Jan 2020].
- 31.NHS England NHS Long Term Plan [Internet]. Available: https://www.longtermplan.nhs.uk/ [Accessed 26 Jan 2020].
- 32.NHS England Delivering universal personalised care [Internet]. Available: https://www.england.nhs.uk/personalisedcare/upc/ [Accessed 26 Jan 2020].
- 33.NHS England Social prescribing link workers [Internet]. Available: https://www.england.nhs.uk/publication/social-prescribing-link-workers/ [Accessed 26 Jan 2020].
- 34.Public Health England Social prescribing: applying All Our Health [Internet]. Available: https://www.gov.uk/government/publications/social-prescribing-applying-all-our-health/social-prescribing-applying-all-our-health [Accessed 26 Jan 2020].
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


