Abstract
The objective of this study is to assess the potential role of Emergency Department (ED) for early detection of mental disorders. Two cohorts (6,759 subjects aged 14 to 24 accessing ED, 165 subjects with mental disorders) were matched by ID and merged. Primary outcome was the proportion of individuals accessing ED before receiving a diagnosis of mental disorder in Mental Health Service (MHS). Secondary outcomes were age of first access to ED in subjects later accessing to MHS, and time from first ED access to receiving a diagnosis of mental disorder at MHS. We assessed whether gender, severity of ED presentation, and number of ED accesses predicted primary outcome. Almost half of individuals who later developed mental disorders (49.7%) accessed ED before access to MHS. Mean age of first ED contact among those later accessing to MHS was 17.34 (2.1), and ED access preceded access to MHS by 3.68 (2.11) years. Gender and severity of ED presentation were not associated with the access to MHS, while higher number of ED accesses was associated with later access to MHS (OR range: 1.17-1.36, p<0.05). Despite its limitations, the present study suggests ED might represent a contact point for individuals who later access to MHS. Future early detection programs should involve ED in their outreach and screening approaches. Additional studies are needed to assess if subjects earlier accessing to ED are at risk-of-developing or already suffer from a mental disorder, and to validate screening instruments specifically designed for ED.
Key words: Mental disorders, early detection, prevention, emergency department, prediction, adolescent psychiatry, pathway to care
Introduction
Schizophrenia, bipolar disorder, and depressive disorders, but also anxiety and eating disorders are neuroprogressive conditions evolving through a clinical staging model (Berk et al., 2017; Cosci & Fava, 2013; de la Fuente- Tomas et al., 2019; Millan et al., 2016). Within this framework it is evident that 75% of mental disorders arise during the adolescence or early adulthood with onset by age 24 (Tortella-Feliu et al., 2019). The need for integrated preventive approaches that encompass both child and adolescents and adult psychiatry have become a major area of interest of modern healthcare systems (O’Brien, 1991). In fact, mental health of young people has been defined a “global public-health challenge”, given that its correlates extend to lower educational achievements, higher risk of violence, poor reproductive and sexual health (Patel, Flisher, Hetrick, & McGorry, 2007). Prevention of mental disorders might also translate into better outcomes for physical health. To improve outcomes of mental disorders it is pivotal to adopt early intervention approaches that integrate primary (e.g. general practitioners) and secondary (e.g. psychiatric units) care settings (Arango et al., 2018; Bauer et al., 2018; Conus, Macneil, & Mcgorry, 2014; Firth et al., 2019; Fusar- Poli, McGorry, & Kane, 2017; Patton et al., 2016). Within this context, the role of Emergency Departments (ED) in prevention of mental disorders has been quite neglected to date. While a growing yet limited body of evidence has shown that interventions in ED can be effective in preventing suicide, (Boudreaux et al., 2016; Miller et al., 2017) the vast majority of available literature focuses on individuals who were already affected with mental disorders (Babeva, Hughes, & Asarnow, 2016). Subjects with mental disorder can require emergent medical assessment, due for instance to panic symptoms mimicking and hard to distinguish from neurologic, cardiac, or respiratory conditions, (Foldes-Busque et al., 2019; Greenslade, Hawkins, Parsonage, & Cullen, 2017) which are frequent in mental disorder (Correll et al., 2017; Firth et al., 2019). Also, it has been reported that subjects with mental disorders despite accounting for a portion as small as 4% of subject accessing to ED overall, (Barratt et al., 2016) are among frequent-users of ED, (Moulin, Evans, Xing, & Melnikow, 2018) and mental disorder is highly underestimated in ED (Nager, Pham, Grajower, & Gold, 2017). However, to the best of authors' knowledge, no preventive approach against mental illness has been developed in ED setting, apart from suicide prevention. Several studies have reported high rates of suicide attempts in patients accessing ED, (Canner, Giuliano, Selvarajah, Hammond, & Schneider, 2018; Doshi, Boudreaux, Wang, Pelletier, & Camargo, 2005; Olfson, Gameroff, Marcus, Greenberg, & Shaffer, 2005; Ting, Sullivan, Boudreaux, Miller, & Camargo, 2012) with some studies investigating preventive approaches for suicide in ED (Ranney et al., 2016; Ranney et al., 2018). The fact that ED has been neglected to date in the field of mental illness prevention is particularly concerning given that current early detection strategies identify only a small proportion of individuals who will later develop mental disorders. For instance, recent studies have found that only 5% of individuals who will later develop psychosis are detected during their at risk stage (Fusar-Poli, 2017b; Fusar-Poli, Rutigliano et al., 2017).
Given the aforementioned, the main aim of the present study was to assess the proportion of individuals with mental disorder who accessed ED ahead of their access to Mental Health Service (MHS). The secondary aim was to measure the age of first access to ED in subjects later accessing to MHS, the amount of time between first ED access and subsequent access to MHS. One further aim was to identify predictors of access to MHS. Our hypotheses were that a substantial proportion of individuals who develop mental disorder seek help in ED before accessing to MHS, and that factors associated with mental disorder in adults, namely severe presentation and number of accesses, are already there and predict subsequent mental disorder in adolescents and young adults.
Methods
Study design
Exploratory cohort study, based on the matching of two retrospective cohorts of individuals. The smaller cohort included 165 patients aged 14 to 24 years old receiving a diagnosis of any mental disorder between 2007 and 2016 in Padua (MHS). The larger cohort included 6,759 subjects aged 14 to 24 years old accessing ED of Padua University Hospital in the same period. On the resulting cohort, we measured primary outcome (i.e. the proportion of individuals accessing ED before MHS). Then, we created a second matched cohort of individuals accessing ED, either with (108) or without (6,651) MHS access. On this second cohort we measured secondary outcomes (see below). The flow-chart of cohort matching is represented in Figure 1. The study adhered to Declaration of Helsinki, and all subjects signed informed consent on the use of anonymized aggregate data for research purposes.
Primary and secondary outcome
Primary outcome was the proportion of individuals accessing ED before access to MHS and receiving a diagnosis of mental disorder, as defined by clinical interview according to ICD-10 criteria. Secondary outcomes were i) the mean age of first ED access in individuals with mental disorders, ii) the time between the first ED access and first access to MHS. We also assessed the role of two predictors on primary outcome, namely triage code as an indicator of severity of clinical ED presentation (ranging from white – lowest severity to red - highest severity with potential life-threatening course), and number of ED accesses.
Data analysis
The proportion of individuals referring to ED before access to MHS (primary outcome), the mean age of first ED referral of subjects later receiving a diagnosis of mental disorder, and the time between the first ED referral and access to MHS, were calculated with descriptive statistics.
Whether triage code, and number of ED accesses predicted subsequent access to MHS was investigated with Generalized Linear Models (GLM). We selected white code (least severe) as reference category for triage code. Gender was used as covariate. We randomly selected a control group (subjects not developing mental disorder among those accessing to ED) with sample size equal to the one developing mental disorder. To replicate results and avoid selection bias, we randomly selected 10 different control samples, and run the same analyses 10 times across different control groups to warrant results replicability and validation. Given the relevant number of multiple analyses, we corrected each p value, applying a False Discovery Rate (FDR) correction. All analyses were run by UG, by means of the R statistical software (R Foundation for Statistical Computing, Vienna, n.d.).
Results
The cohort of 165 individuals aged 14 to 24 developing mental disorder, was composed by 5 subjects with substance-related disorders [ICD-10 F10.0(1), F10.5(1), F11.9(1), F19.9(2)], 23 subjects with schizophrenia spectrum disorders [F20.0(1), F20.3(1), F20.8(2), F20.9(1), F21(1), F23.2(3), F23.3(1), F25.2(2), F25.8(1), F25.9(3), F28(1), F29(6)], 15 with bipolar affective disorder [F31.0(1), F31.1(1), F31.2(1), F31.5(1), F31.9(11)], 35 with depressive episode or depressive disorder [F32.0(1), F32.1(3), F32.2(7), F32.3(6), F32.8(1), F32.9(5), F33.0(2), F33.1(3), F33.3(5), F33.9(1), F39(1)], 75 with neurotic, stress-related, and somatoform disorders [F40.2(1), F41.0(11), F41.1(4), F41.9(22), F42.0(2), F42.8(3), F42.9(1), F43.0(1), F43.1(5), F43.2(23), F44.8(1), F48.9(1)], 1 with non-organic sleep disorder (F51.0(1)), 11 with disorders of personality and adult behavior [F60.3(5), F60.5(1), F60.8(1), F60.9(1), F63.0(1), F63.8(1)].
Of these 165 individuals, 65,45% (108) accessed to ED (either before or after access to MHS), and 82 (49,7%) did it before receiving a diagnosis of mental disorder at MHS (primary outcome).
Of these 82 individuals, 41% had ICD-10 criteria anxiety disorders, 22% had depressive disorders, 13% had schizophrenia spectrum disorders, 7 % had bipolar disorder, 7 % had personality disorders, others had other conditions (8%) including substance-related disorders, obsessive-compulsive disorders, tic disorder, conduct disorders, or adjustment disorders.
Among the 82 subjects accessing to ED before receiving a diagnosis of mental disorder at MHS, the mean age of first ED referrals was 17.34 [standard deviation (SD)=2.1] years old, and the average time from first ED referral to diagnosis of mental disorder was 3.68 (SD=2.11) years. Descriptions of the matched cohort, primary outcome and secondary outcomes are reported in Table 1.
Number of accesses to ED predicted subsequent mental disorder onset among subjects aged 15 to 24 years old, namely those with more ED accesses had increased likelihood of developing mental disorder, after adjusting for gender (OR = 1.17 to 1.36, p values <0.05 across all validation samples) (see Table 2).
Severity of clinical presentation, and specifically yellow over white triage code predicted subsequent onset of mental disorder in four out of ten random samples (OR = 2.84 to 4.62, p value <0.05 after FDR correction). However, the significant finding did not hold true in six out of ten random samples after FDR correction, not meeting replicability criteria (see Table 3).
Figure 1.
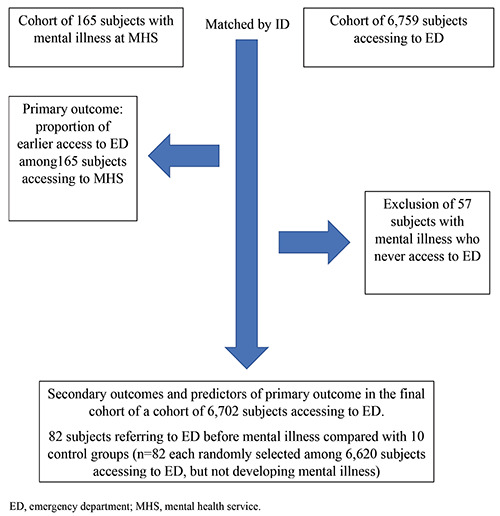
Flow-chart of cohort matching and study design.
Discussion
Data from the present cohort study suggest that half the patients later accessing to MHS and receiving a diagnosis of mental disorder accessed to ED earlier. Importantly, they accessed to ED between three and a half and four years before access to MHS. Moreover, the present data show that multiple ED referrals is associated with the subsequent access to MHS, regardless of gender. The clinical presentations of individuals accessing ED can range from mild to severe and indistinguishable from that of the general population.
The core result of this study is that half the patients later accessing to MHS for a diagnosis of mental disorders access ED three to four years ahead of the onset of their disorder, on average. This finding should be interpreted cautiously in the context of a naturalistic study where confounders could not systematically be assessed. Some subjects accessing to ED before MHS might have been already affected by mental disorder, while other might have been at-risk of developing mental illness.
Table 1.
Characteristics of a cohort of subjects aged 14 to 24 years old referring to Emergency Department before developing mental disorder: primary, secondary outcome, and other characteristics.
| Primary outcome (n=165) | ||
| Proportion of subjects accessing to ED before MHS | 82/165 (49.7%) | |
| Secondary outcomes (n=82) | ||
| Mean age at first access to Emergency Department (mean, SD) | 17.34 (2.1%) | |
| Years from ED access to mental disorder onset | 3.68 (2.11%) | |
| Other characteristics (n=82) | ||
| Mean age at first referral to mental health service | 21.43 (2.11%) | |
| Mean number of referrals | 4.07 (7.05%) | |
| Gender % | F=56; M=44 | |
| Red triage code % | 7 | |
| Yellow triage code % | 41 | |
| Green triage code % | 15 | |
| White triage code % | 37 |
ED, emergency department; MHS, mental health service.
Table 2.
Multivariate regression assessing whether number of referrals to ED predicted subsequent mental disorder onset across 10 samples.
| Predictor | Sample 1 | Sample 2 | Sample 3 | Sample 4 | Sample 5 | Sample 6 | Sample 7 | Sample 8 | Sample 9 | Sample 10 |
|---|---|---|---|---|---|---|---|---|---|---|
| Gender (M) | 1,03ns | 1,03ns | 0,9ns | 0,66ns | 0,93ns | 0,9ns | 1,14ns | 0,8ns | 0,81ns | 0,67ns |
| (0,54-1.94) | (0,24-1,98) | (0,48-1,7) | (0,38-1,24) | (0,5-1,75) | (0,48-1,7) | (0,6-2,16) | (0,42-1,5) | (0,43-1,53) | (0,38-1,26) | |
| ED referrals | 1,2* | 1,36* | 1,17* | 1,2* | 1,17* | 1,17* | 1,17* | 1,17* | 1,22* | 1,24* |
| (1.05-1.41) | (1,14-1,7) | (1,04-1,36) | (1,05-1,4) | (1,04-1,35) | (1,04-1,36) | (1,04-1,36) | (1,04-1,36) | (1,07-1,45) | (1,08-1,48) |
*, p<0.05; ns, non-significant; p-values are corrected for False Discovery Rate (FDR).
Table 3.
Multivariate regression assessing whether severity of clinical presentation to ED predicted subsequent mental disorder onset across 10 samples.
| Predictor | Sample 1 | Sample 2 | Sample 3 | Sample 4 | Sample 5 | Sample | Sample | Sample 8 | Sample 9 | Sample 10 |
|---|---|---|---|---|---|---|---|---|---|---|
| Gender (M) | 0,95ns | 0,97ns | 0,88ns | 0,58ns | 0,92ns | 0,88ns | 1,08ns | 0,77ns | 0,79ns | 0,64ns |
| (0,49-1,84) | (0,51-1,84) | (0,47-1,63) | (0,31-1,1) | (0,49-1,71) | (0,47-1,63) | (0,57-2,06) | (0,41-1,46) | (0,42-1,48)( | (0,34-1,22) | |
| Green triage code | 2,85ns | 2,51ns | 1,53ns | 1,11ns | 0,86ns | 1,89ns | 3,34ns | 1,75ns | 1,88ns | 1,81ns |
| (reference=white) | (1,06-8,01) | (0,93-7,08) | (0,59-3,98) | (0,45-2,73) | (0,34-2,11) | (0,95-3,84) | (1,17-10,48) | (0,68-4,54) | (0,72-4,99) | (0,7-4,7) |
| Yellow triage code | 4,62* | 2,84* | 1,89ns | 2,52ns | 1,39ns | 2,11ns | 2,45ns | 3,05* | 2,35ns | 3,09* |
| (reference=white) | (2,2-10,16) | (1,4-5,88) | (0,95-3,84) | (1,22-5,3) | (0,69-2,81) | (0,55-8,87) | (1,23-4,98) | (1,48-6,44) | (1,17-4,82) | (1,5-6,55) |
| Red triage code | 3,78ns | 2,49ns | 2,11ns | 2,06ns | 1,68ns | 1,53ns | 3,33ns | 2,45ns | 2,32ns | 2,36ns |
| (reference=white) | (0,93-18,95) | (0,66-10,44) | (0,55-8,87) | (0,54-8,72) | (0,44-7,14) | (0,59-3,98) | (0,81-16,7) | (0,65-10,3) | (0,61-9,76)( | (0,62-9,96) |
*, p<0.05; ns, non-significant; p-values are corrected for False Discovery Rate (FDR).
For the former group of patients, this study suggests that several young patients might have a long duration of untreated illness (three to four years). Should the access to ED be related to symptoms of mental illness, or should symptoms of mental disorders had been already present at that time, the average duration largely exceeds international recommendations aiming at reducing duration of untreated illness to be kept below three months, for instance (for psychosis) (Bertolote & McGorry, 2005). Our findings are valuable in ecological validity because they report on realworld data that reflect the local clinical routine, and might confirm there is an global mismatch between the recommended standards (three months of untreated illness) and their fulfillment (Cotter, Zabel, French, & Yung, 2017). This is particularly problematic in the case of individuals who present with sporadic features that resemble mental disorders but that spontaneously remit, such as in young individuals with acute and transient psychotic symptoms, (Minichino et al., 2019) who may frequently develop persisting mental disorders after seeking help at ED (Rutigliano et al., 2018). The present data are also in line with the limited evidence available to date on the role of ED in the early diagnosis and intervention of mental disorders. Data from a similar study conducted in Canada showed that around 50% of young individuals receive their index diagnosis of psychosis in ED (yet previous contacts may have occurred in other contexts) (Anderson et al., 2013). Moreover, a previous systematic review on pathway to care of patients with first-episode psychosis showed that for the vast majority the first contact was a physician, and frequently from emergency services (Anderson, Fuhrer, & Malla, 2010). While those studies confirm the relevance of the role of ED in early detection, data from the present study provide additional evidence, suggesting that index access to ED occurs earlier than index diagnosis of mental disorder, and that subsequent mental disorder can be suspected in particular in subjects aged between 17 and 18, and with repeated accesses, according to data of the present study. There is a large body of evidence converging on the association between duration of untreated illness and poor clinical outcome. In particular it has been shown that duration of untreated psychosis correlates with poor general symptomatic outcome, severity of positive and negative symptoms, not achieving remission and poor social functioning and global outcome, according to a metaanalysis (Penttilä, Jaäskel̈ainen, Hirvonen, Isohanni, & Miettunen, 2014). Solid evidence has shown that early intervention services are the gold-standard to improve outcome of early stages psychoses (Correll et al., 2018) (yet a lot remains to be done in the long-term) (Rutigliano et al., 2018). However, a recent meta-analysis indicates that to reduce the duration of untreated psychosis is it essential to intervene early and to detect young people during their clinical high risk stage, (Fusar-Poli, 2017a) i.e. before they receive an established diagnosis of mental disorder (Oliver et al., 2018).
Regarding the second group of individuals, namely those not already affected by mental illness when accessing to ED, ED could have worked as a detection setting for clinical high-risk group of subjects. In fact, early intervention services at the time of a first episode of mental disorder may not succeed in lowering the duration of untreated illness (Penttilä et al., 2014). Real-world data have shown services for individuals experiencing a clinical high risk stage can optimize the effectiveness of early intervention services for reducing the duration of untreated psychosis and other outcomes (Fusar-Poli, Diaz- Caneja, et al., 2016). For example individuals accessing to early intervention for psychosis via preventive services compared with those with standard referral spend fewer days in hospital, have a shorter duration of untreated illness, lower frequency of admission, and importantly even a lower likelihood of compulsory admission (which also implies cost-reduction) (Cheung, Roper, & Purdon, 2014) in the 24 months following referral (Fusar-Poli, Diaz-Caneja, et al., 2016). However, while it is clear that intervening at the time of the first onset of clinical high risk stage is much needed, the rate-limiting step towards is the ability to detect most individuals who are at risk and who will later develop mental disorders (van Os & Guloksuz, 2017). Recent empirical studies have shown that only a low proportion of individuals who will later develop psychosis would be detected during their clinical high risk stage, ahead of the onset of their disorder. Because of this, preventive services might be largely ineffective in detecting subjects at risk for psychosis with later transition to psychosis (Fusar-Poli, Sullivan, Shah, & Uhlhaas, 2019). This is further complicated by the intrinsic shortcomings of outreaching activities implemented by preventive services, which dilute the prognostic accuracy of the assessment interviews employed in this field (Fusar-Poli, Schultze-Lutter, et al., 2016; Pelizza et al., 2019; Yung et al., 2005). Since around half of patients later developing a mental disorder earlier access to ED, and since ED is a clinical context with pretest risk enrichment (HR 1.42 to develop psychosis compared with general population), (Fusar-Poli, Rutigliano, et al., 2016) it should be strongly involved in mental disorder prevention services. This manuscript contributes to the available knowledge in this area by suggesting that ED could be included in innovative detection programs for young individuals at risk of developing mental disorders. Leveraging our findings, it is possible to recommend that future prevention services should always incorporate a network of primary and mental healthcare agencies. In this perspective, the present study shows that the rates of young individuals developing any type of mental disorder who earlier referred to ED is high (almost 50%), possibly suggesting a window for improving early detection.
According to our data, subjects at risk of developing mental disorder apparently can present with any severity of clinical presentation, from mild to severe. Hence, while repeated ED access can potentially be used to identify subjects at risk, the severity of clinical presentation is unlikely to be of value to distinguish at risk individuals from those not at risk. These findings can inform future research in the development of a quick and usable instrument to screen for emerging mental disorders and detect individuals at risk among subjects aged 14 to 24, specifically designed for ED. Ideally such instrument should be quick to use, and ideally trans-diagnostic, (Fusar-Poli, Solmi, et al., 2019) to detect subjects at risk for mental disorder without adding additional logistic burden on ED. While such instruments are being developed across the world, (Downey & Zun, 2018; Nager et al., 2017) these have not yet received the empirical validation that is necessary to implement them in clinical routine.
Several reasons might contribute as barriers to mental healthcare, directing subjects at risk of mental disorders towards ED instead of MHS. First, self-stigma, overall stigma and discrimination in particular, are a barrier to access to care, and have been shown to correlate with longer duration of untreated illness (Kular et al., 2019).
Subjects may be prone to avoid mental-health connoted clinical contexts, may minimize functioning impairment or unspecific symptoms, and may wait to seek for help until more acute signs or symptoms manifest. ED might work as a unique opportunity for early detection and treatment of mental disorder given that subjects may not show help-seeking behavior in other than ED contexts, and given that once acute symptoms with the associated distress resolve, they may resume the usual habits avoiding mental health professionals, and neglecting they are in need of help.
The present work might also have some points of strength. First, we provide evidence from real-world data, which could be informative for eventual future clinical implementation of (real world) evidence-based services. Second, we have a-priori set a strict significance threshold, adding on top of FDR corrected p-value threshold, the replication of significant findings across 10 random samples as significance condition.
The present study has several limitations. First, we were unable to exclude mental disorder onset and subsequent psychiatric treatment was offered in other than national health service setting, such as private practice. Second, the sample size of subjects developing mental disorder after ED referral was relatively small, with 165 individuals with mental ill health, only 82 of whom attended the ED prior to diagnosis) and the research was only carried out in one region of Italy. On the contrary, sample size accessing to ED was dramatically higher than the small sample size accessing to MHS. As such, the analyses investigating the association between candidate predictors and outcomes in this study should be further replicated by future studies. Third, subjects might have accessed to ED for reasons unrelated to mental disorders’ symptoms. However, none of the subjects were admitted in medical units after ED access, excluding medical urgencies underlying reason for ED access. Fourth, the overall prevalence of subjects referring to MHS after ED was low, indicating the need for lean and fast self-rated screening instruments to be implemented in ED, as a long, time- and resource-consuming tool would not be costeffective.
Conclusions
In conclusion, we show that around half of the patients later developing mental disorders between age 15 and 24 contact ED on average 3-4 before their onset of mental disorders. Despite relevant limitations, results of thi exploratory study might suggest that involving ED in this network of services outreached by early intervention campaigns could translate into an improved detection for at risk individuals and reduced duration of untreated illness. We also show that mental disorder screening should be administered to subjects aged between 17 and 18, referring to ED multiple times, regardless gender, and severity of clinical presentation.
Highlights
Around one out of two patients aged 15 to 24 later accessing to mental health service for a mental disorder accesses to emergency department earlier.
On average three to four years pass between access to emergency department and access to mental health service.
Repeated accesses to emergency department predict later diagnosis of mental disorder.
References
- Arango C, Díaz-Caneja CM, McGorry PD, et al. (2018). Preventive strategies for mental health. The Lancet Psychiatry, 5(7), 591-604. doi:10.1016/S2215-0366(18)30057-9 [DOI] [PubMed] [Google Scholar]
- Anderson KK, Fuhrer R, Malla AK. (2010). The pathways to mental health care of first-episode psychosis patients: A systematic review. Psychological Medicine, 40(10), 1585-1597. doi:10.1017/S0033291710000371 [DOI] [PubMed] [Google Scholar]
- Anderson KK, Fuhrer R, Wynant W, Abrahamowicz M, Buckeridge DL, Malla A. (2013). Patterns of health services use prior to a first diagnosis of psychosis: The importance of primary care. Social Psychiatry and Psychiatric Epidemiology, 48(9), 1389-1398. doi:10.1007/s00127-013-0665-3 [DOI] [PubMed] [Google Scholar]
- Babeva K, Hughes JL, Asarnow J. (2016). Emergency Department Screening for Suicide and Mental Health Risk. Current Psychiatry Report, 18(11), 100. doi:10.1007/s11920-016-0738-6 [DOI] [PubMed] [Google Scholar]
- Barratt H, Rojas-García A, Clarke K, et al. (2016). Epidemiology of Mental Health Attendances at Emergency Departments: Systematic Review and Meta-Analysis. Abe T, ed. PLoS One, 11(4), e0154449. doi:10.1371/journal.pone.0154449 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bauer M, Andreassen OA, Geddes JR, et al. Areas of uncertainties and unmet needs in bipolar disorders: clinical and research perspectives. The Lancet Psychiatry, 5(11), 930-939. doi:10.1016/S2215-0366(18)30253-0 [DOI] [PubMed] [Google Scholar]
- Berk M, Post R, Ratheesh A, et al. (2017). Staging in bipolar disorder: from theoretical framework to clinical utility. World Psychiatry, 16(3), 236-244. doi:10.1002/wps.20441 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bertolote J, McGorry P. (2005). Early intervention and recovery for young people with early psychosis: Consensus statement. The British Journal of Psychiatry, 187(48), s116-s119. doi:10.1192/bjp.187.48.s116 [DOI] [PubMed] [Google Scholar]
- Boudreaux ED, Camargo CA, Arias SA, et al. (2016). Improving Suicide Risk Screening and Detection in the Emergency Department. American Journal of Preventive Medicine, 50(4), 445-453. doi:10.1016/j.amepre.2015.09.029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Canner JK, Giuliano K, Selvarajah S, Hammond ER, Schneider EB. (2018). Emergency department visits for attempted suicide and self harm in the USA: 2006-2013. Epidemiology and Psychiatric Sciences, 27(1), 94-102. doi:10.1017/ S2045796016000871 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheung D, Roper L, Purdon SE. (2014). Pathways to (specialized) care: Patient costs and contacts en route to a first-episode psychosis clinic. Early Intervention in Psychiatry, 8(4), 375-381. doi:10.1111/eip.12093 [DOI] [PubMed] [Google Scholar]
- Conus P, Macneil C, Mcgorry PD. (2014). Public health significance of bipolar disorder: Implications for early intervention and prevention. Bipolar Disorder, 16(5), 548-556. doi:10.1111/bdi.12137 [DOI] [PubMed] [Google Scholar]
- Correll CU, Galling B, Pawar A, et al. (2018). Comparison of early intervention services vs treatment as usual for earlyphase psychosis: A systematic review, meta-analysis, and meta-regression. JAMA Psychiatry, 75(6), 555-565. doi:10.1001/jamapsychiatry.2018.0623 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Correll CU, Solmi M, Veronese N, et al. (2017). Prevalence, incidence and mortality from cardiovascular disease in patients with pooled and specific severe mental illness: a large-scale meta-analysis of 3,211,768 patients and 113,383,368 controls. World Psychiatry, 16(2). doi:10.1002/ wps.20420 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cosci F, Fava GA. (2013). Staging of mental disorders: Systematic review. Psychotherapy and Psychosomatics, 82(1), 20-34. doi:10.1159/000342243 [DOI] [PubMed] [Google Scholar]
- Cotter J, Zabel E, French P, Yung AR. (2017). Prolonged duration of untreated psychosis: a problem that needs addressing. Early Intervention in Psychiatry, 11(3), 263-268. doi:10.1111/ eip.12308 [DOI] [PubMed] [Google Scholar]
- de la Fuente-Tomas L, Sánchez-Autet M, García-Álvarez L, et al. (2019). Clinical staging in severe mental disorders; bipolar disorder, depression and schizophrenia. Revista de Psiquiatria Salud Mental, 12(2), 106-115. doi:10.1016/j.rpsm.2018. 08.002 [DOI] [PubMed] [Google Scholar]
- Doshi A, Boudreaux ED, Wang N, Pelletier AJ, Camargo CA. (2005). National study of US emergency department visits for attempted suicide and self-inflicted injury, 1997-2001. Annals of Emergency Medicine, 46(4), 369-375. doi:10.1016/j.annemergmed.2005.04.018 [DOI] [PubMed] [Google Scholar]
- Downey LVA, Zun LS. (2018). Identifying Undiagnosed Pediatric Mental Illness in the Emergency Department. Pediatric Emergency Care, 34(2), e21-e23. doi:10.1097/PEC. 0000000000001151 [DOI] [PubMed] [Google Scholar]
- Firth J, Siddiqi N, Koyanagi A, et al. (2019). The Lancet Psychiatry Commission: a blueprint for protecting physical health in people with mental illness. The Lancet Psychiatry, 6(8), 675-712. doi:10.1016/S2215-0366(19)30132-4 [DOI] [PubMed] [Google Scholar]
- Foldes-Busque G, Denis I, Poitras J, Fleet RP, Archambault P, Dionne CE. (2019). A closer look at the relationships between panic attacks, emergency department visits and non-cardiac chest pain. Journal of Health Psychology, 24(6), 717-725. doi:10.1177/1359105316683785 [DOI] [PubMed] [Google Scholar]
- Fusar-Poli P. (2017a). Extending the benefits of indicated prevention to improve outcomes of first-episode psychosis. JAMA Psychiatry, 74(7), 667-668. doi:10.1001/jamapsychiatry.2017.1009 [DOI] [PubMed] [Google Scholar]
- Fusar-Poli P. (2017b). The Clinical High-Risk State for Psychosis (CHR-P), Version II. Schizophrenia Bullettin, 43(1), 44-47. doi:10.1093/schbul/sbw158 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fusar-Poli P, Díaz-Caneja CM, Patel R, et al. (2016). Services for people at high risk improve outcomes in patients with first episode psychosis. Acta Psychiatrica Scandinavica 133(1), 76-85. doi:10.1111/acps.12480 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fusar-Poli P, McGorry PD, Kane JM. (2017). Improving outcomes of first-episode psychosis: an overview. World Psychiatry, 16(3), 251-265. doi:10.1002/wps.20446 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fusar-Poli P, Rutigliano G, Stahl D, et al. (2017). Development and Validation of a Clinically Based Risk Calculator for the Transdiagnostic Prediction of Psychosis. JAMA Psychiatry, 74(5), 493-500. doi:10.1001/jamapsychiatry.2017.0284 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fusar-Poli P, Schultze-Lutter F, Cappucciati M, et al. (2016). The Dark Side of the Moon: Meta-analytical Impact of Recruitment Strategies on Risk Enrichment in the Clinical High Risk State for Psychosis. Schizophrenia Bulletin, 42(3), 732-743. doi:10.1093/schbul/sbv162 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fusar-Poli P, Solmi M, Brondino N, et al. (2019). Transdiagnostic psychiatry: a systematic review. World Psychiatry, 18(2), 192-207. doi:10.1002/wps.20631 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fusar-Poli P, Sullivan SA, Shah JL, Uhlhaas PJ. (2019). Improving the Detection of Individuals at Clinical Risk for Psychosis in the Community, Primary and Secondary Care: An Integrated Evidence-Based Approach. Front Psychiatry, 10, 774. doi:10.3389/fpsyt.2019.00774 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenslade JH, Hawkins T, Parsonage W, Cullen L. (2017). Panic Disorder in Patients Presenting to the Emergency Department With Chest Pain: Prevalence and Presenting Symptoms. Heart, Lung and Circulation, 26(12), 1310-1316. doi:10.1016/j.hlc.2017.01.001 [DOI] [PubMed] [Google Scholar]
- Kular A, Perry BI, Brown L, et al. (2019). Stigma and access to care in first-episode psychosis. Early Intervention in Psychiatry, 13(5), 1208-1213. doi:10.1111/eip.12756 [DOI] [PubMed] [Google Scholar]
- Miller IW, Camargo CA, Arias SA, et al. (2017). Suicide prevention in an emergency department population: The EDsafe study. JAMA Psychiatry, 74(6), 563-570. doi:10.1001/jamapsychiatry.2017.0678 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Minichino A, Rutigliano G, Merlino S, et al. (2019). Unmet needs in patients with brief psychotic disorders: Too ill for clinical high risk services and not ill enough for first episode services. European Psychiatry, 57, 26-32. doi:10.1016/j.eurpsy.2018. 12.006 [DOI] [PubMed] [Google Scholar]
- Moulin A, Evans EJ, Xing G, Melnikow J. (2018). Substance use, homelessness, mental illness and medicaid coverage: A setup for high emergency department utilization. The Western Journal of Emergency Medicine, 19(6), 902-906. doi:10.5811/ westjem.2018.9.38954 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nager AL, Pham PK, Grajower DN, Gold JI. (2017). Mental Health Screening among Adolescents and Young Adults in the Emergency Department. Pediatric Emergency Care, 33(1), 5-9. doi:10.1097/PEC.0000000000000529 [DOI] [PubMed] [Google Scholar]
- O’Brien JD. (1991). Current prevention concepts in child and adolescent psychiatry. American Journal of Psychotherapy. 45(2), 261-268. doi:10.1176/appi.psychotherapy.1991.45.2.261 [DOI] [PubMed] [Google Scholar]
- Olfson M, Gameroff MJ, Marcus SC, Greenberg T, Shaffer D. (2005). Emergency treatment of young people following deliberate self-harm. Archives of General Psychiatry, 62(10), 1122-1128. doi:10.1001/archpsyc.62.10.1122 [DOI] [PubMed] [Google Scholar]
- Oliver D, Davies C, Crossland G, et al. (2018). Can We Reduce the Duration of Untreated Psychosis? A Systematic Review and Meta-Analysis of Controlled Interventional Studies. Schizophrenia Bulletin, 44(6), 1362-1372. doi:10.1093/ schbul/sbx166 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patel V, Flisher AJ, Hetrick S, McGorry P. (2007). Mental health of young people: a global public-health challenge. Lancet, 369(9569), 1302-1313. doi:10.1016/S0140-6736(07)60368-7 [DOI] [PubMed] [Google Scholar]
- Patton GC, Sawyer SM, Santelli JS, et al. (2016). Our future: a Lancet commission on adolescent health and wellbeing. Lancet, 387(10036), 2423-2478. doi:10.1016/S0140-6736(16)00579-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pelizza L, Azzali S, Paterlini F, et al. (2019). Screening for psychosis risk among help-seeking adolescents: Application of the Italian version of the 16-item prodromal questionnaire (iPQ-16) in child and adolescent neuropsychiatry services. Early Intervention in Psychiatry, 13(4), 752-760. doi: 10.1111/eip.12554 [DOI] [PubMed] [Google Scholar]
- Penttilä M, Jaäskel̈ainen E, Hirvonen N, Isohanni M, Miettunen J. (2014). Duration of untreated psychosis as predictor of long-term outcome in schizophrenia: Systematic review and meta-analysis. The British Journal of Psychiatry, 205(2), 88-94. doi:10.1192/bjp.bp.113.127753 [DOI] [PubMed] [Google Scholar]
- R Foundation for Statistical Computing Vienna AU. Available from: https://www.Rorg/. [Google Scholar]
- Ranney ML, Freeman JR, Connell G, et al. (2016). A Depression Prevention Intervention for Adolescents in the Emergency Department. Journal of Adolescent Health, 59(4), 401-410. doi:10.1016/j.jadohealth.2016.04.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ranney ML, Pittman SK, Dunsiger S, et al. Emergency department text messaging for adolescent violence and depression prevention: A pilot randomized controlled trial. Psychological Services, 15(4), 419-428. doi:10.1037/ ser0000193 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rutigliano G, Merlino S, Minichino A, et al. (2018). Long term outcomes of acute and transient psychotic disorders: The missed opportunity of preventive interventions. European Psychiatry, 52, 126-133. doi:10.1016/j.eurpsy.2018.05.004 [DOI] [PubMed] [Google Scholar]
- Tortella-Feliu M, Fullana MA, Pérez-Vigil A, et al. (2019). Risk factors for posttraumatic stress disorder: An umbrella review of systematic reviews and meta-analyses. Neuroscience and Biobehavioral Reviews, 107, 154-165. doi:10.1016/j. neubiorev.2019.09.013 [DOI] [PubMed] [Google Scholar]
- van Os J, Guloksuz S. (2017). A critique of the “ultra-high risk” and “transition” paradigm. World Psychiatry, 16(2), 200-206. doi:10.1002/wps.20423 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yung AR, Yung AR, Pan Yuen H, et al. (2005). Mapping the Onset of Psychosis: The Comprehensive Assessment of At-Risk Mental States. Australian and New Zealand Journal of Psychiatry, 39(11-12), 964-971. doi:10.1080/j.1440-1614.2005.01714.x [DOI] [PubMed] [Google Scholar]


