Abstract
Background
Online physical activity interventions can be an effective strategy for weight loss. However, there is a lack of systematic reviews examining the relationship between intervention usage (dose) and participants' response to online physical activity interventions for weight loss. It remains unclear whether certain usage metrics (e.g. login frequency, percent of content accessed) would be associated with improvements in behavioral outcomes. Understanding the dose-response relationship for online physical activity interventions for weight loss would be important for designing and evaluating future interventions.
Objective
1) Review the methods used to assess intervention usage and 2) to explore the association between intervention usage metrics and outcomes for online physical activity interventions for weight-loss.
Methods
We conducted a systematic review following the PRISMA guidelines to examine the dose-response relationship of online-based interventions targeting physical activity. We used the following keywords: web OR internet OR online OR eHealth AND physical activity OR exercise, AND engagement OR dose OR dose-response OR usage AND obesity OR weight*. Peer-reviewed articles published between 2006 and 2019 were included.
Results
A total of five articles met the inclusion criteria. The mean intervention length was 10 ± 6 months (range 2–30 months). The usage metrics were total number of logins, login frequency, and usage of online tools. All usage metrics reported were found to be related to outcomes in physical activity interventions for weight-loss.
Conclusion
Our findings suggest that usage metrics for online physical activity interventions for weight-loss included login frequency, login duration, and use of online tools. Increased intervention usage appeared to be associated with an improvement in participant's weight, physical activity behaviors, and intervention retention. Future research should examine innovative ways to maintain intervention usage throughout the intervention.
Keywords: Online physical activity intervention, Dose-response, Usage, Weight-loss, Systematic review
Highlights
-
•
There are few studies examining the dose-response relationship of online physical activity interventions for weight-loss
-
•
Usage metrics for evaluating dose-response relationships included login frequency, login duration and use of online tools
-
•
Most usage metrics reflected time spent interacting with an intervention but not the quality of interaction
-
•
Increased intervention usage appeared to be associated with improvements in outcomes
-
•
Further studies examining usage metrics are needed to better understand dose-response relationship
1. Introduction
Obesity is the leading risk factor for type 2 diabetes, cardiovascular disease, and mortality (Patrick et al., 2011). Currently, 42.4% percent of individuals living in the United States are overweight or obese (Hales et al., 2020). Lifestyle changes such as regular physical activity is an important modifiable risk factor to combat obesity. However, the World Health Organization (2016) estimates more than 80% of adolescents and 23% of adults do not meet the requirement of 150 min of moderate-to-vigorous physical activity (MVPA) per week. This has led to a growing demand for public health agencies to develop and implement scalable physical activity programs to combat obesity and promote weight-loss.
Recent studies have shown that online physical activity interventions for weight-loss can be a scalable and effective method to increase physical activity, and promote weight-loss (Marcus et al., 2007; Alley et al., 2018; Liu et al., 2019; Liu et al., 2018; Nolan et al., 2018). These studies used an online platform that promoted physical activity to support weight-loss. Advantages of these online physical activity interventions for weight-loss include the potential of reaching a large number of participants, and improved program delivery flexibility (e.g. provide participants convenience by enabling them to access program content at anytime and anywhere) (White et al., 2004). Despite these advantages, persistent usage of online-based interventions is a concern (Eysenbach, 2005). Previous studies have reported that usage of online-based interventions dropped under 50% within one to two month after starting the program (Geraghty et al., 2013; Edney et al., 2019; Wangberg et al., 2008). Low intervention usage may not necessarily mean that participants have not improved their target behavior. It is possible that participants have gained the necessary motivation and skills from the intervention before completing the intervention. This may lead the participants to spend less time interacting with the intervention content (Eysenbach, 2005; Christensen and Mackinnon, 2006; Fleming et al., 2018). It is also likely that participant engagement decreased as a result of a lack of interest in the intervention design (Couper et al., 2010). Thus, this has prompted recent studies to examine the relationship between intervention usage and outcome, also known as the dose-response relationship.
Online-based interventions enable researchers to collect objective measures of intervention usage including log-in frequency, percentage of content viewed, and time spent per log-in. Previous studies examining the dose-response relationship between usage and intervention outcomes for eating disorder, depression, and smoking cessions found that an increase in intervention usage led to improved outcomes (Donkin et al., 2011). Currently, there is a lack of systematic reviews examining the dose-response relationship for online physical activity interventions for weight-loss. Therefore, this study's objectives are to 1) review the methods used to assess intervention usage and 2) explore the association between intervention usage metrics and outcomes for online physical activity interventions for weight-loss.
2. Methods
This review was conducted according to the PRISMA guidelines (Liberati et al., 2009). The parameters of the search strategy were first defined to include articles from January 1st, 2006 to June 1st, 2019. Academic Search Premier, Cochrane Central Register of Controlled Trials, Health Source: Nursing/Academic Edition, MEDLINE with Full Text, PsycARTICLES, PsycINFO were searched systematically with the following terms: web OR Internet OR online OR eHealth AND physical activity OR exercise, AND engagement OR dose OR dose-response OR usage AND obesity OR weight*. We performed a backward reference search of the articles found and included any articles that met the inclusion criteria.
2.1. Eligibility criteria
The title and abstract of identified studies were reviewed to make initial exclusions. Studies were selected for review if they met the following inclusion criteria: published in a peer-reviewed journal, participants were enrolled in an online physical activity intervention for weight-loss, collected objective measures of intervention usage data throughout the intervention, and evaluated the dose-response relationship. The online physical activity can be either explicitly or as part of a multicomponent lifestyle behavior intervention. Studies that met the above criteria were read fully to determine if they were suitable to include in our review. This review focused only on online-based delivered interventions and excluded in-person interventions. However, interventions were included if they had both an online and an in-person component.
2.2. Quality analysis
The study quality of the five publications were evaluated by the authors (NS, SL) using the Quality Assessment of Relevant Studies tool created by the Effective Public Health Practice Project (EPHPP) (Thomas et al., 2004); this tool allows for the assessment of both internal and external validity of a study. Studies were given a strong, moderate, or weak rating after being assessed based on six sub-categories: 1) Selection bias 2) Study design 3) Confounders 4) Blinding 5) Data collection methods 6) Withdrawals and dropouts. If a study receives at least four strong ratings and no weak ratings it is given a strong global rating. If a study has less than four strong ratings and one weak rating it is given a moderate global rating. Lastly, a study is given a weak global rating if it has two or more weak ratings. The quality assessment enabled us to flag any low-quality studies in order to reduce the risk of bias in our review (Background: Development and Use of Study Quality Assessment Tools, 2020).
2.3. Coding of study characteristics
Key study characteristics were extracted for this review. Factors were extracted that were believed to be important for review and captured the relationship between usage and outcomes. These factors consisted of an intervention/program design, study sample size, data related to study quality (i.e., selection bias, confounders, data collection methods), usage metrics (e.g. login frequency, login duration), and their association with intervention outcomes. Additionally, studies were coded using Michie et al. (2013) hierarchically clustered techniques for reporting behavior change interventions to determine behavior change techniques implemented.
2.4. Data synthesis
The review used descriptive data to summarize the various types of intervention usage metrics for online-based weight-loss interventions aimed to promote physical activity. All usage metrics were sorted by frequency to identify usage metrics reported in the literature. We identified whether certain usage metrics of online interventions were significantly associated with changes in study outcomes for each study and combined the observations into a matrix table. We sorted by frequency to evaluate which usage metrics were reflective of changes in the study outcomes.
3. Results
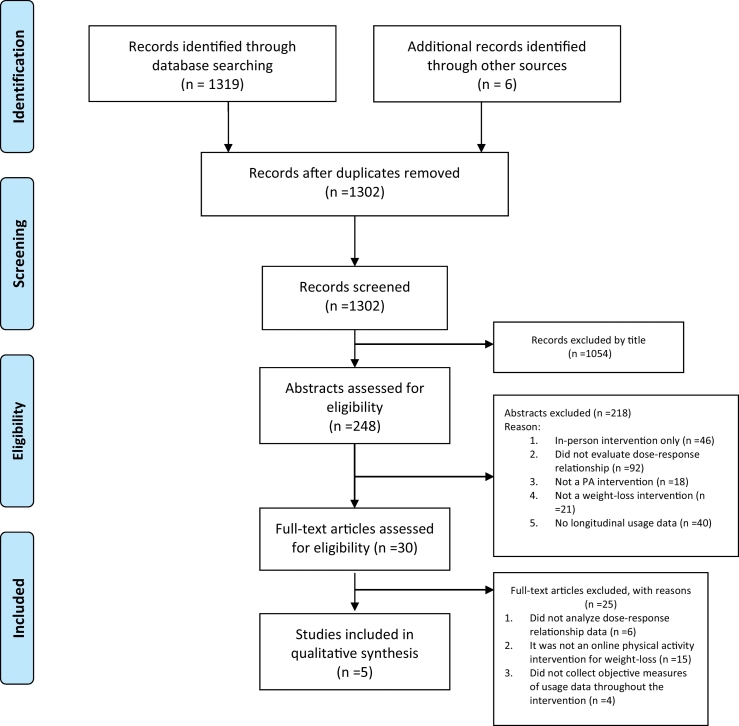
During the initial database search, 1302 relevant articles were identified. Particularly, 1054 articles were excluded based on the title, Following title elimination 248 articles were excluded because the intervention was not delivered online (n = 46), articles did not evaluate dose-response (n = 92), articles were not a physical activity intervention (n = 18) articles were not a weight-loss intervention (n = 21), or the article contained no longitudinal usage data (n = 40). Thirty full-text articles were screened in full. Twenty-five articles were eliminated because they did not analyze a dose-response relationship (n = 6), they were not an online physical activity intervention for weight-loss (n = 15), they did not collect objective measures of usage data throughout the intervention (n = 4). Five articles met our inclusion criteria. Article selections are shown in Fig. 1.
Fig. 1.
PRISMA flow diagram (Liberati et al., 2009).
3.1. Study characteristics
Scores for each quality assessment component (e.g. confounder, withdrawals and dropouts, data collection, and/or the analysis categories) for the five studies are listed in Table 1. Two studies received a “strong” global quality rating (Patrick et al., 2011; Funk et al., 2010); the remaining three studies were considered “moderate” (Maher et al., 2015; Hurling et al., 2006; Wilson et al., 2019).
Table 1.
Global assessment of studies identified in systematics search.a
| Author | Selection bias | Study design | Confounders | Blinding | Data collection method | Withdrawals | Global rating |
|---|---|---|---|---|---|---|---|
| Funk et al., 2010 | Strong | Strong | Strong | Moderate | Strong | Moderate | Strong |
| Hurling et al., 2006 | Moderate | Strong | Moderate | Moderate | Strong | Weak | Moderate |
| Maher et al., 2015 | Strong | Strong | Weak | Moderate | Strong | Strong | Moderate |
| Patrick et al., 2011 | Moderate | Strong | Strong | Moderate | Strong | Strong | Strong |
| Wilson et al., 2019 | Strong | Strong | Weak | Moderate | Strong | Moderate | Moderate |
Global assessment is based on quality assessment of relevant studies tool (Thomas et al., 2004).
Study characteristics are summarized in Table 2. The average intervention duration was 10 ± 6 months (range 2–30 months). Of the five studies selected, four implemented an online-based intervention platform (Patrick et al., 2011; Funk et al., 2010; Hurling et al., 2006; Wilson et al., 2019), and one utilized mobile phones (Maher et al., 2015). Four of the studies (Patrick et al., 2011; Funk et al., 2010; Hurling et al., 2006; Wilson et al., 2019) were primarily self-guided and involved no contact between participants and researchers (Patrick et al., 2011; Funk et al., 2010; Hurling et al., 2006; Wilson et al., 2019). However, one study involved inter-participant interactions via online communications such as chat forums (Maher et al., 2015). One of the online-based programs included a face-to-face component for half of the intervention period where the researchers met with the participants and delivered the intervention (Wilson et al., 2019).
Table 2.
Characteristics of studies identified in systematics search.a
| Study\country | Intervention duration, mode of delivery | Sample size (N), participant age | Intervention behavior change curricula | Cluster label | Behavior change techniques | Usage metrics |
|---|---|---|---|---|---|---|
|
Funk et al., 2010 United States |
Duration: 30 months Mode of delivery: Online |
N = 348, 55.7 years (SD 8.5) |
|
|
|
total logins: 107 (range 52, 143) Total time on website: 433 (range 236, 792) Use of online tools
Forum visits • Messages read: 54 (range 14, 152) • Posts made: 1 (range 0, 4) |
|
Hurling et al., 2006 United Kingdom |
Duration: 10-weeks Mode of delivery: Online |
N = 75, 35 years (range 23–54) |
|
|
|
Login frequency per week: 1.4 times |
|
Maher et al., 2015 Australia |
Duration: 50 days Mode of delivery: Mobile |
N = 110, 35.6 years (SD 12.4) |
|
|
|
Total logins: 18 (SD 13.3; range 0, 46) Use of online tools
|
|
Patrick et al., 2011 United States |
Duration: 12 months Mode of delivery: Online |
N = 441, 43.9 years (SD 8.0) |
|
|
|
Login frequency: 23.4 weeks (SD 16.7) |
|
Wilson et al., 2019 United States |
Duration: 16 weeks Mode of delivery: in person and online |
N = 125 families, children's' ages: 11–16 |
|
|
|
Percent of content accessed: 4.28 of 8 sessions (SD 3.01) Login duration: 12.99 min (SD 11.63) PA content exposure: 25.4% Repeat exposure: 7.5% |
Behavior change content based on Michie et al. (2013) cluster analysis of behavioral change techniques.
3.2. Metrics used to determine intervention usage
Our review identified nine usage metrics that were reported in the selected studies. This included: total logins, login frequency, login duration, total time, use of online tools, forum visits, percent of content accessed, physical activity content exposure, and repeated content exposure. Total logins, login frequency, and use of online tools were the most popular metrics used to determine intervention usage. See Table 2 for a breakdown of metrics used in the selected studies.
3.3. Dose-response relationship between usage and study outcome
All the studies included in this review found that a significant increase in intervention usage was associated with improvements in study outcomes (see Table 3). Study outcomes included participant retention (Wilson et al., 2019), weight regain (Funk et al., 2010), satisfaction with fitness (Hurling et al., 2006), improvements in MVPA (Maher et al., 2015), reduction in weight, BMI, and waist circumference (Patrick et al., 2011). Table 3 summarizes the relationship between usage and study outcomes.
Table 3.
Dose response relationship.a
| Study outcomes | Strength of usage metric and outcome |
||||||||
|---|---|---|---|---|---|---|---|---|---|
| Total logins | Login frequency | Login duration | Total time | Use of online tools | Forum visits | Percent of content accessed | PA content exposure | Repeat exposure | |
| Weight regain | − (n = 1) | − (n = 1) | − (n = 1) | − (n = 1) | |||||
| Self-reported fitness | + (n = 1) | ||||||||
| MVPA | + (n = 1) | + (n = 1) | |||||||
| BMI | − (n = 1) | ||||||||
| Weight | − (n = 1) | ||||||||
| Waist circumference | − (n = 1) | ||||||||
| Retention | + (n = 1) | + (n = 1) | + (n = 1) | + (n = 1) | |||||
The rating indicator (+ = positive, − = negative) followed by number of studies that reported usage metrics for the physical activity outcomes.
3.3.1. Total login
Two studies reported on the total number of unique logins throughout the entire intervention (Funk et al., 2010; Maher et al., 2015). Funk et al. (2010) reported logins in an average of 107 times (range 52,143) on the website during the 30 months of the intervention. Maher et al. (2015) reported that participants logged in a total of 18 times (SD 13.3; range 0,46) during the 50 days of the intervention. The total number of logins was associated with less weight regain (Funk et al., 2010) and positively associated with improvements in MVPA (Maher et al., 2015).
3.3.2. Login frequency
Two studies reported on the rate at which participants logged onto the interventions (Patrick et al., 2011; Hurling et al., 2006). Hurling et al. (2006) reported a login frequency of 1.4 times per week over the 10-week intervention and found that login frequency was positively associated with self-reported fitness. Patrick et al. (2011) reported participants logged in a mean 23.4 weeks (SD 16) of the 12-month intervention and found it was negatively associated with a decrease in BMI, weight, and waist circumference.
3.3.3. Login duration
Login duration was reported in one study. Wilson et al. (2019) reported that the amount of time a participant stayed logged in to the intervention during each viewing (12.99 min; SD 11.63) over the 16-week intervention was significantly correlated with participant retention.
3.3.4. Total time on website
Only one study reported total intervention usage time. Funk et al. (2010) reported that participants spent an average of 433 min on the website (Range 236,792) during the 30 months of the intervention. Their results showed that greater usage (total time) was associated with less weight regain.
3.3.5. Use of online tools
Online tools were reported in two studies. Funk et al. (2010) reported that participants logged their current weight 104 times (range 51,130) and logged their exercise 124 (range 32, 376) times during the 30 months of the intervention. Maher et al. (2015) reported that participants sent 4.8 (SD 6.3; range 0,27) gifts to other participants and made 2.7 (SD 3.4; range 0,13) discussion posts during the 50-day intervention. We identified that the number of online tools accessed was associated with less weight regain (Funk et al., 2010), and positively associated with an increase in MVPA (Maher et al., 2015).
3.3.6. Forum visits
One study utilized forums for participants to interact. Funk et al. (2010) found that participants read on average 54 (range 14,152) forum messages and made one (range 0,4) forum post during the 30 months of the intervention. We identified that an increase in forum visits was associated with less weight regains.
3.3.7. Percent of content accessed
One study reported on the percent of content accessed. Wilson et al. (2019) found that on average 53.5% (SD 37.6%) of content was accessed over the 16-week intervention. The study reported that an increase in the percent of content accessed was significantly associated with program retention.
3.3.8. PA content exposure and repeat content exposure
The percent of content exposure is defined as the percentage of overall intervention modules viewed by the participants at once. Repeated content exposure is defined as the completion of a module multiple times. Only one study reported percent of content exposure and repeated content exposure. Wilson et al. (2019) found the average physical activity content exposure was 25.4% and repeat content exposure was 37.5% over the 16-week intervention. Both variables were found to be positively associated with increased participant retention.
4. Discussion
4.1. Summary of evidence
The purpose of this review was to examine the types of intervention usage metrics reported in online physical activity interventions for weight-loss and to describe the dose-response relationship between usage and intervention outcomes. We found total logins, login frequency, and use of online tools were reported most frequently. We found that increased intervention usage was associated with an improvement in satisfaction with fitness (Hurling et al., 2006), MVPA (Maher et al., 2015), and retention (Wilson et al., 2019), and prevented weight regain following an intervention (Patrick et al., 2011; Funk et al., 2010). Our review identified that there is a limited number of studies examining the dose-response relationship in online physical activity interventions for weight-loss and highlighted the importance to promote intervention engagement.
The results from this review suggest that there were several usage metrics reported among online physical activity interventions for weight-loss. The majority of studies in this review focused on usage metrics on the time an individual spends interacting with an intervention (e.g. login duration, and total time) rather than the quality of the interaction. There is a possibility to overestimate the time an individual spends on a webpage. Participants may log into the intervention and leave the computer or forget to logout between sessions. Thus, this would lead to a misrepresentation of the total time the participant actively engaged with the intervention (Donkin et al., 2013).Capturing usage on the quality of the intervention interaction may help distinguish areas of the intervention that were most successful in achieving the outcomes (Donkin et al., 2013). The usage metrics that may inform the quality of the intervention interaction may include the percent of intervention accessed and repeat exposure (e.g. total logins and login frequency). It is important to note that total login and login frequency are both markers measuring repeat intervention exposure, but they can contain different information. Total login measures the sum of all logins throughout an intervention and this usage metric is useful to evaluate the overall repeated exposure of the intervention. Meanwhile, the login frequency captures the rate of login within a specific timeframe. Login frequency may be particularly useful when comparing repeated intervention exposure between interventions. For example, two interventions may vary in overall intervention length (10 weeks vs 12 weeks) but login frequency expressed in weekly frequency for both interventions may enable researchers to compare repeated exposure between these interventions. Future online-based interventions reporting usage metrics may consider using a combination of frequency and quality of interaction metrics. Cluster analysis may also be a useful method to identify participants' usage patterns as it combines multiple metrics (Gough, 2001; Nolan et al., 2015).
Results from this systematic review suggest that there is a dose-response relationship between the usage of online physical activity interventions and improvements in weight, physical activity, and intervention retention outcomes. Our findings were similar to previous studies examining dose-response relationships for online-based interventions for e-therapies and depression (Donkin et al., 2011; Donkin et al., 2013). Due to the limited number of studies, we were not able to determine whether certain usage metrics were more appropriate at evaluating dose-response relationships. However, a systematic review of online-based cognitive behavior therapies reported that only certain usage metrics (e.g. number of log-ins, and proportion of modules completed) showed a dose-response relationship with intervention outcomes (Donkin et al., 2011). Specifically, the number of logins was associated with improvements in behavioral outcomes (e.g. smoking, fruit and vegetable consumption, physical activity), meanwhile, the proportion of modules completed was associated with improvements in psychological outcomes (e.g. Anxiety, depression, body dissatisfaction). These findings suggest that program engagement may be important for physical and psychological interventions in different ways.
This review found that intervention usage patterns varied among studies and thus an “optimal” intervention use may be dependent upon the intervention or participant characteristics (Ritterband et al., 2009). Patrick et al. (2011) reported that participants who completed 60% of the weekly goal setting sessions were associated with a decrease in BMI, weight, and waist circumference. Funk et al. (2010), however, reported a much greater engagement rate was required to achieve a statistically significant improvement in outcomes. They found that participants who logged in and reported their weight over 26 out of 28 study months (93%) of the intervention were associated with less weight regain (Funk et al., 2010). These two studies have very different values of program usage where a significant change in outcome achievement occurred. Our current understanding of dose-response often comes from drug trials where the dose is a “prescribed” measure, whereby participants either receive the full treatment or none (Eysenbach, 2005). A decrease in intervention engagement over time does not necessarily mean that participants did not sustain behavior change. Participants may have gained the necessary motivation and skills from the intervention before completing the intervention. Thus, this may lead participants to spend less time interacting with intervention content (Eysenbach, 2005; Christensen and Mackinnon, 2006; Fleming et al., 2018). The findings from this review suggest that dose-response may be better described as a curvilinear relationship where a saturation point is reached before completion of the entire intervention. Future studies are warranted.
This review also highlighted the need to design interactive and engaging online-based interventions. The inclusion of gamification features and incentives may help further boost intervention engagements. Gamification involves adopting game-like mechanics within an online-based health intervention. Previous studies have identified several popular gamification elements, including point scoring, competition, challenges, and collection of items (Floryan et al., 2019). Recent studies have suggested that integrating game mechanics with the core intervention content and making it fit with user requirements is critical for adopting gamification to promote intervention engagement (Floryan et al., 2019). There is emerging evidence to suggest that incentives (e.g. loyalty rewards) can also be an effective strategy to engage users and promote behavior change (Liu et al., 2014).
4.2. Limitations
Some limitations should be noted regarding the results of this review. The small number of studies selected limited our ability to generalize these findings. There was a lack of consistency between studies with regard to the methods used to evaluate intervention usage. Furthermore, the studies selected for this review were heterogeneous in intervention protocol, study duration, and outcome measures. Thus, a meta-analysis was not feasible due to the heterogeneity.
5. Conclusion
The objective of this review was to examine the types of intervention usage metrics reported in online physical activity interventions for weight-loss and to describe the dose-response relationship between usage and intervention outcomes. The usage metrics reported in online physical activity interventions for weight-loss included login frequency, login duration, and use of online tools. We found that increased intervention usage appeared to be associated with an improvement in participants' weight-loss, weight regain, physical activity behaviors, intervention retention. However, these findings should be interpreted with caution due to the limited number of studies. Future research should examine innovative ways to maintain intervention usage throughout the intervention.
CRediT authorship contribution statement
NS and SL were involved in the design and concept of the study. NS performed the study selection, data extraction, and analysis. NS wrote the draft of the manuscript. SL provided revisions of the manuscript.
Acknowledgements/funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
Declaration of competing interest
The authors declare that there is no conflict of interest.
References
- Alley S.J., Kolt G.S., Duncan M.J. The effectiveness of a web 2.0 physical activity intervention in older adults - a randomised controlled trial. Int. J. Behav. Nutr. Phys. Act. 2018;15(1):4–11. doi: 10.1186/s12966-017-0641-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Background: Development and Use of Study Quality Assessment Tools. NHLBI, NIH; 2020. https://www.nhlbi.nih.gov/node/80102 (Accessed July 22) [Google Scholar]
- Christensen H., Mackinnon A. The law of attrition revisited. J. Med. Internet Res. 2006;8(3):e20. doi: 10.2196/jmir.8.3.e20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Couper M.P., Alexander G.L., Zhang N. Engagement and retention: measuring breadth and depth of participant use of an online intervention. J. Med. Internet Res. 2010 doi: 10.2196/jmir.1430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donkin L., Christensen H., Naismith S.L., Neal B., Hickie I.B., Glozier N. A systematic review of the impact of adherence on the effectiveness of e-therapies. J. Med. Internet Res. 2011;13(3):e52. doi: 10.2196/jmir.1772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donkin L., Hickie I.B., Christensen H. Rethinking the dose-response relationship between usage and outcome in an online intervention for depression: randomized controlled trial. J. Med. Internet Res. 2013;15(10):e231. doi: 10.2196/jmir.2771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edney S., Ryan J.C., Olds T. User engagement and attrition in an app-based physical activity intervention: secondary analysis of a randomized controlled trial. J. Med. Internet Res. 2019 doi: 10.2196/14645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eysenbach G. The law of attrition. J. Med. Internet Res. 2005;7(1):e11. doi: 10.2196/jmir.7.1.e11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fleming T., Bavin L., Lucassen M., Stasiak K., Hopkins S., Merry S. Beyond the trial: systematic review of real-world uptake and engagement with digital self-help interventions for depression, low mood, or anxiety. J. Med. Internet Res. 2018 doi: 10.2196/jmir.9275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Floryan M.R., Ritterband L.M., Chow P.I. Principles of gamification for Internet interventions. Transl. Behav. Med. 2019 doi: 10.1093/tbm/ibz041. [DOI] [PubMed] [Google Scholar]
- Funk K.L., Stevens V.J., Appe L.J. Associations of internet website use with weight change in a long-term weight loss maintenance program. J. Med. Internet Res. 2010 doi: 10.2196/jmir.1504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geraghty A.W.A., Torres L.D., Leykin Y., Pérez-Stable E.J., Muñoz R.F. Understanding attrition from international internet health interventions: a step towards global eHealth. Health Promot. Int. 2013 doi: 10.1093/heapro/das029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gough L. Social assistance regimes: a cluster analysis. J. Eur. Soc. Policy. 2001 doi: 10.1177/095892870101100205. [DOI] [Google Scholar]
- Hales C.M., Carroll M.D., Fryar C.D., Ogden C.L. Prevalence of obesity and severe obesity among adults: United States, 2017–2018 key findings data from the national health and nutrition examination survey. 2020. https://www.cdc.gov/nchs/products/index.htm (Accessed March 1, 2020) [PubMed]
- Hurling R., Fairley B.W., Dias M.B. Internet-based exercise intervention systems: are more interactive designs better? Psychol. Health. 2006;21(6):757–772. doi: 10.1080/14768320600603257. [DOI] [Google Scholar]
- Liberati A., Altman D.G., Tetzlaff J. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J. Clin. Epidemiol. 2009 doi: 10.1016/j.jclinepi.2009.06.006. [DOI] [PubMed] [Google Scholar]
- Liu S., Hodgson C., Zbib A.M., Payne A.Y.M., Nolan R.P. The effectiveness of loyalty rewards to promote the use of an internet-based heart health program. J. Med. Internet Res. 2014 doi: 10.2196/jmir.3458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu S., Brooks D., Thomas S.G., Eysenbach G., Nolan R.P. Effectiveness of user- and expert-driven web-based hypertension programs: an RCT. Am. J. Prev. Med. 2018 doi: 10.1016/j.amepre.2018.01.009. [DOI] [PubMed] [Google Scholar]
- Liu S., Tanaka R., Barr S., Nolan R.P. Effects of self-guided e-counseling on health behaviors and blood pressure: results of a randomized trial. Patient Educ. Couns. 2019 doi: 10.1016/j.pec.2019.10.007. [DOI] [PubMed] [Google Scholar]
- Maher C., Ferguson M., Vandelanotte C. A web-based, social networking physical activity intervention for insufficiently active adults delivered via Facebook app: randomized controlled trial. J. Med. Internet Res. 2015;17(7):e174. doi: 10.2196/jmir.4086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marcus B.H., Lewis B.A., Williams D.M. A comparison of internet and print-based physical activity interventions. Arch. Intern. Med. 2007 doi: 10.1001/archinte.167.9.944. [DOI] [PubMed] [Google Scholar]
- Michie S., Richardson M., Johnston M. The behavior change technique taxonomy (v1) of 93 hierarchically clustered techniques: building an international consensus for the reporting of behavior change interventions. Ann. Behav. Med. 2013 doi: 10.1007/s12160-013-9486-6. [DOI] [PubMed] [Google Scholar]
- Nolan R.P., Ross H., D'Antono B. Prototypical trajectories of patient engagement with an e-counselling platform to promote self-care in heart failure. Can J Cardiol. 2015 doi: 10.1016/j.cjca.2015.07.571. [DOI] [Google Scholar]
- Nolan R.P., Feldman R., Dawes M. Randomized controlled trial of e-counseling for hypertension: REACH. Circ Cardiovasc Qual Outcomes. 2018 doi: 10.1161/CIRCOUTCOMES.117.004420. [DOI] [PubMed] [Google Scholar]
- Patrick K., Calfas K.J., Norman G.J. Outcomes of a 12-month web-based intervention for overweight and obese men. Ann. Behav. Med. 2011;42(3):391–401. doi: 10.1007/s12160-011-9296-7. [DOI] [PubMed] [Google Scholar]
- Ritterband L.M., Thorndike F.P., Cox D.J., Kovatchev B.P., Gonder-Frederick L.A. A behavior change model for internet interventions. Ann. Behav. Med. 2009 doi: 10.1007/s12160-009-9133-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomas B.H., Ciliska D., Dobbins M., Micucci S.A. Process for systematically reviewing the literature: providing the research evidence for public health nursing interventions. 2004;1 doi: 10.1111/j.1524-475X.2004.04006.x. https://sigmapubs.onlinelibrary.wiley.com/doi/pdf/10.1111/j.1524-475X.2004.04006.x (Accessed July 29, 2019) [DOI] [PubMed] [Google Scholar]
- Wangberg S.C., Bergmo T.S., Johnsen J.A.K. Patient Prefer Adherence. 2008. Adherence in Internet-based interventions. [PMC free article] [PubMed] [Google Scholar]
- White M.A., Martin P.D., Newton R.L. Mediators of weight loss in a family-based intervention presented over the internet. Obes. Res. 2004 doi: 10.1038/oby.2004.132. [DOI] [PubMed] [Google Scholar]
- Wilson D.K., Sweeney A.M., Law L.H., Kitzman-Ulrich H., Resnicow K. Web-based program exposure and retention in the families improving together for weight loss trial. Ann. Behav. Med. 2019 doi: 10.1093/abm/kay047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization Obesity and overweight. 2016. https://www.who.int/en/news-room/fact-sheets/detail/obesity-and-overweight (Accessed June 6, 2019)