FIG. 1.
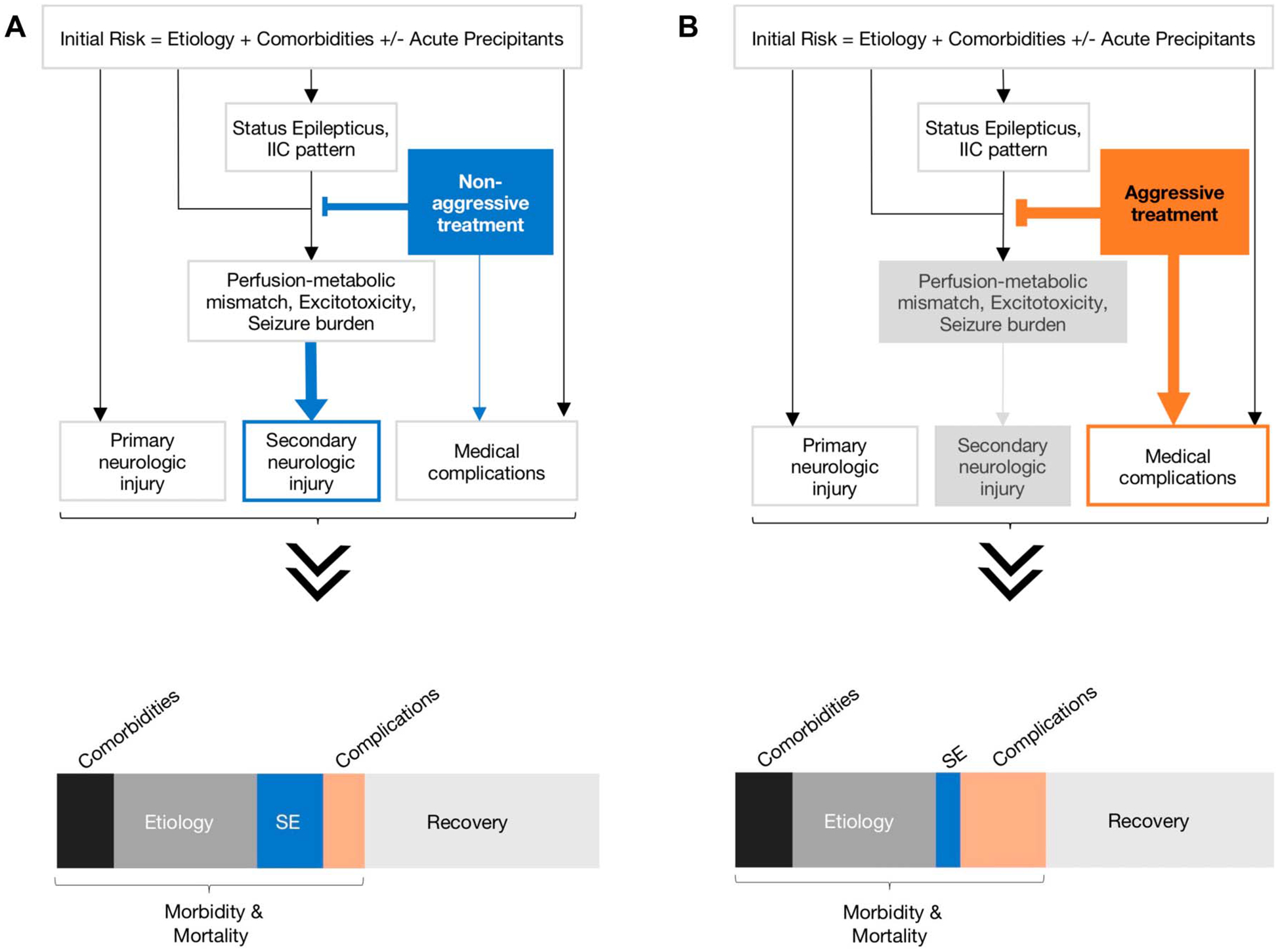
Simplified pathophysiological model for status epilepticus outcomes based on nonaggressive versus aggressive treatment strategies. This simple generic model demonstrates the relationships between an inciting event (seizure etiology and patient comorbidities) leading to status epilepticus (SE) or ictal–interictal continuum (IIC) patterns and functional outcomes and mortality. There may or may not be a new primary neurologic injury as a result of the inciting event or secondary injury from perfusion-metabolic mismatch or excitotoxicity from SE. The inciting event and its medical treatment (nonaggressive vs. aggressive) can lead to medical complications. These factors interact in a nonlinear way to produce an individual’s outcome and, across many patients, shape the distribution of functional outcomes (recovery vs. morbidity) and mortality rate. Here, we assume that the type of treatment strategy (nonaggressive vs. aggressive) does not impact the overall outcome distribution, but it does affect morbidity and mortality proportion from secondary injury and medical complications of treatment. A, Nonaggressive treatment: In this model, we assume delay in seizure control because of nonaggressive treatment, which would presumably lead to worse outcomes because of secondary injury from uncontrolled seizures, but lower rate of medical complications of treatment. B, Aggressive treatment: In this model, we assume faster seizure control with aggressive treatment, what would limit seizure burden and secondary brain injury. This approach has an increased likelihood for harm because of medical complications. The distribution of contributing factors for SE outcomes (recovery vs. morbidity and mortality) may change depending on which treatment strategy is used.
