Abstract
Background
Home-based newborn care has been found to reduce neonatal mortality in rural areas. Study evaluated effectiveness of home-based care delivered by specially recruited newborn care workers- Shishu Rakshak (SR) and existing workers- anganwadi workers (AWW) in reducing neonatal and infant mortality rates.
Methods
This three-arm, community-based, cluster randomised trial was conducted in five districts in India. Intervention package consisted of pregnancy surveillance, health education, care at birth, care of normal/low birthweight neonates, identification and treatment of sick neonates and young infants using oral and injectable antibiotics and community mobilisation. The package was similar in both intervention arms—SR and AWW; difference being healthcare provider. The control arm received routine health services from the existing health system. Primary outcomes were neonatal and young infant mortality rates at ‘endline’ period (2008–2009) assessed by an independent team from January to April 2010 in the study clusters.
Findings
A total of 6623, 6852 and 5898 births occurred in the SR, AWW and control arms, respectively, during the endline period; the proportion of facility births were 69.0%, 64.4% and 70.6% in the three arms. Baseline mortality rates were comparable in three arms. During the endline period, the risk of neonatal mortality was 25% lower in the SR arm (adjusted OR 0.75, 95% CI 0.57 to 0.99); the risks of early neonatal mortality, young infant mortality and infant mortality were also lower by 32%, 27%, and 33%, respectively. The risks of neonatal, early neonatal, young infant, infant mortality in the AWW arm were not different from that of the control arm.
Interpretation
Home-based care is effective in reducing neonatal and infant mortality rates, when delivered by a dedicated worker, even in settings with high rates of facility births.
Trial registration number
The study was registered with Clinical Trial Registry of India (CTRI/2011/12/002181).
Keywords: child health, health services research, public health, cluster randomised trial
Key questions.
What is already known?
Pooled analysis of trials from South Asia found a significant reduction in neonatal mortality rate (NMR) following home-based newborn care (pooled RR 0.75; 95% CI 0.61 to 0.92) suggesting greater beneficial effect with a higher baseline NMR (>50 per 1000 live births) based on the results of subgroup and meta-regression analyses.
What are the new findings?
We found a similar magnitude of reduction in NMR when home-based newborn care is delivered by dedicated worker even in settings with low NMR (low ‘endline’ NMR—of 33.5 per 1000 live births—in the control arm) and high facility birth.
What do the new findings imply?
Home-based newborn care is effective in reducing neonatal mortality including deaths within first week of life and infant mortality particularly when delivered by dedicated worker even in setting with high facility births.
Introduction
The global burden of neonatal deaths is estimated to be 2.6 million, of which 0.76 million—more than a quarter—occur in India.1 With a neonatal mortality rate (NMR) of 26 per 1000 live births and infant mortality rate of 39 per 1000 live births,2 deaths in the neonatal period alone contribute to two-thirds of infant deaths in India. Even among postneonatal infant deaths (1–12 months), a major proportion of deaths occur in the second month of life. Any further reduction in infant mortality is therefore intricately linked to a major reduction of neonatal and young infant (0–59 days) deaths.
Various attempts have been made to implement innovative approaches for newborn care at community/home level. The Cochrane review on community-based interventions found a significant reduction—by about 25%—in neonatal mortality with community mobilisation and antenatal and postnatal home visits by health workers.3 The Lancet Every Newborn Study Group estimated that immediate scaling up of various community-based and primary care interventions can avert almost a third of all neonatal deaths by 2017 and one-fifth by 2025.4
One of the key components of community-based interventions for neonatal health is the home-based newborn care (HBNC), that is, care provided at homes by health workers in the antenatal, intrapartum and postnatal periods. An earlier study by the Society for Education, Action and Research in Community Health (SEARCH) in Gadchiroli district of Maharashtra, India, demonstrated that HBNC by trained female village health workers significantly reduced the NMR by up to 62% in settings with high baseline NMRs.5 The effectiveness of this approach in diverse rural settings with varying NMRs needs to be assessed given the profound implications of this intervention. If effective, such an approach must be incorporated into the existing health systems.
In this background, we conducted a community-based cluster randomised effectiveness trial at multiple sites across India to evaluate the effect of home-based care for neonates and young infants delivered by community-based workers on neonatal and young infant mortality rates (YIMR). The primary research question was whether a package of interventions for young infants (0–59 days of age) delivered through home visits by (1) existing village-level community workers and (2) specially recruited village-level workers tasked to perform newborn/young infant care would reduce their mortality rates.
Methods
Study area and existing health system
This community-based cluster randomised trial was conducted in five districts in the north, east and western states of India: Barabanki (Uttar Pradesh), Cuttack (Odisha), Patna (Bihar), Rajsamand (Rajasthan) and Yavatmal (Maharashtra). The study was implemented by non-governmental organisations at two districts (Action Research and Training for Health, Udaipur (Rajsamand) and National Institute of Applied Human Research and Development, Cuttack) and by government institutions at the other three districts (King George Medical College, Lucknow (Barabanki), Patna Medical College (Patna) and Mahatma Gandhi Institute of Medical Sciences, Wardha (Yavatmal).
The public healthcare infrastructure at these districts comprised a hierarchical system of district hospital(s), community health centres (CHC), primary health centres (PHC) and subcentres (SC). Typically, the health services are provided by medical officers, nurses and auxiliary nurse midwives (ANM) at facility level, and by ANM and anganwadi workers (AWWs) at the community level. An ANM usually caters to a population of 5000–7000 and provides antenatal check-ups, counselling of pregnant women and childhood immunisation. The AWW serves approximately a population of 1000 and is responsible for supplementary nutrition to pregnant and lactating women and preschool children and non-formal education to preschool children.
Study design and ethical considerations
The study was designed as a three-arm cluster randomised controlled trial, with PHC being the unit of randomisation. The intervention package in the two intervention arms was delivered by either a specially recruited community-based worker—Shishu Rakshak (SR)—or by the already existing AWW. The control arm received routine health services from the public and private health system.
Selection of clusters
The study sites were selected in consultation with the state and district health authorities, the essential criteria for selection being a high NMR (>40 per 1000 live births) and high incidence of home deliveries (>70%). A baseline survey was undertaken in nine conveniently selected PHCs in each district to estimate NMRs and home deliveries in the year preceding survey (2002–2003). From these nine, six PHCs (in each district) that fulfilled the criteria were selected to participate in the study. Usually, one PHC served a population of about 30 000. In case a PHC catered to more than 30 000 individuals, only a limited number of SC enough to cover 30 000 population were included.
Randomisation, consent and ethics
The PHCs were paired to arrive at matched three sets (two PHCs in each) with comparable NMRs in each study district. These were then randomly allocated to the two intervention arms and control arm with the help of computer generated random numbers (generated by an independent statistician). Thus, two PHCs in each district constituted 10 clusters in five districts in each arm. Informed verbal consent was obtained from the village leaders, mukhiyas (chiefs) and heads of the panchayats prior to beginning of the study. At each site, a safety monitoring committee monitored the safety of the intervention. A central Data Safety Monitoring Board (DSMB) monitored the overall study progress and results.
Intervention
Preparatory phase
The preparatory phase of the study began in January 2003 with the baseline house-to-house survey by trained local field workers who collected information on pregnancy history in women of reproductive age group and the number of neonatal deaths in the last year. This was followed by selection of the SR in those sites that were randomised to SR arm. Selection was done in 3-day residential camps, the eligibility criteria being (1) resident of the village, (2) education of at least 5th standard and uptil 10th standard (3) has been a mother herself and (4) willing to attend delivery at night and undergo residential training. For the other intervention (AWW) arm, the AWWs already in place were deployed. These workers were employed by the state government (salary approximately US$50) and had varying level of training and experience.
The workers from both the categories were trained in the same manner by using competency-based training curriculum, modules and manual developed by SEARCH, Gadchiroli. Initially, the SEARCH team trained the master trainers-cum-field supervisors from all five study sites in three training workshops of 15–17 days each. The master trainers in turn conducted training of SRs and AWWs at respective study sites in seven workshops of 5 days duration each, interspersed by field practice of 1 month. The training involved classroom sessions followed by hands-on in the field, and was accomplished in a step-ladder fashion, that is, one set of skills at a time. The whole training package was covered in 17 modules. In addition to SRs and AWWs, the ANMs from the health system were also trained on supportive supervision for two days apart from their regular training. In both the intervention arms, 2-day training workshops were conducted for the traditional birth attendants (TBAs) (on safe delivery practices) and for medical officers of PHCs and private practitioners (orientation training).
Training of master trainers began in October 2003 and was completed in August 2004, while training of SR/AWW/ANM began in November 2003 and got completed in December 2004 (save for AWW arm of one centre, which got completed by April 2005). The workers were assessed after each training session and a final evaluation was done at the end of training. A joint team of Indian Council of Medical Research (ICMR) and SEARCH conducted the end-of-training assessment. Because many workers did not acquire the skills necessary for giving intramuscular (IM) injections after a single training session, additional training sessions were conducted by using dummies and having hands-on sessions in the health facilities. Regular reorientation training and on-job training for the SR/AWWs were undertaken during monthly meetings.
Intervention phase
In the next phase, the trained workers (SRs or AWWs) performed house-to-house surveys every 2 months to identify eligible women. Pregnant women thus identified were registered at around fifth month of pregnancy and were provided the package of interventions. Briefly, the package consisted of the following interventions—health education, care at birth, care of normal/low birthweight neonates, identification and treatment of sick neonates and young infants, and community mobilisation (table 1; further details provided in online supplementary web table 1). The package essentially remained the same in both the intervention arms (save for the provision of IM injection for sepsis in the SR arm; Table 1)—only the healthcare provider was different.
Table 1.
List of interventions in the three arms
| Intervention | Shishu Rakshak | Anganwadi worker | Control |
| Pregnancy surveillance every 2 months | + | + | – |
| Three antenatal home visits for health education | + | + | – |
| Presence at delivery | + | + | – |
| Care at birth | + | + | As per programme |
| Postnatal home visits, identification of high risk and sick neonates | + | + | – |
| Management of hypothermia, feeding, umbilical and skin infection, eye care | + | + | – |
| Cotrimoxazole and IM injections for probable sepsis | + | – | – |
| Training of MOs/PPs | + | + | – |
| Training of TBAs | + | + | – |
| Awareness of community leaders | + | + | – |
| Group health education and community mobilisation | + | + | – |
IM, intramuscular; MO, medical officer; PP, private practitioners; TBAs, traditional birth attendants.
bmjgh-2017-000680supp001.pdf (41.9KB, pdf)
Health education messages during antenatal period and on the second day after delivery comprised of care and nutrition during pregnancy, birth preparedness (antenatal care (ANC), tetanus toxoid immunisation, safe delivery), early initiation and exclusive breast feeding, prevention of infection, prevention and management of hypothermia and recognising danger signs during pregnancy and danger signs in the neonates and seeking immediate help from health worker. The village-level worker—SR/AWW as per the intervention arm—attended delivery along with the TBA and provided care at birth (if the women chose to deliver at home). She did suctioning with an oral mucus sucker and if required, bag and mask ventilation for newborns with weak/absent cry or slow breathing at birth. She weighed them within 6 hours of birth using Salter weighing scale (with sensitivity of 100 g) and counselled the mothers regarding thermal care and early initiation of breast feeding and duration of exclusive breast feeding. She also assessed for high-risk status to decide on the number of follow-up visits at home. For health education, a flipchart and a 1-hour long digital versatile disc (DVD)—‘Nanhisi Jan’ (tiny life)—produced by SEARCH were used in the intervention clusters. Information gathered from focus group discussions during preparatory phase was used as resource information for health education messages.
Home visits were made on days 1, 2, 3, 5, 7, 14, 21, 28, 35, 42, 49 and 56 for normal newborns, and on days 1, 2, 3, 4, 5, 6, 7, 9, 12, 15, 18, 21, 28, 35, 42, 48 and 56 for high-risk newborns (defined as birth weight <2000 g or preterm or breastfeeding problems on the first day of life). Gestation was determined using the last menstrual period method, confirmed with the help of local events calendar. During home visits, the workers assessed the newborns for any signs of illness, recorded temperature using a digital thermometer, provided treatment for minor illnesses and offered referral services for those with severe disease like suspected sepsis. Newborns with hypothermia (axillary temperature <35°C) were managed by keeping in a warm bag or by covering with blankets; those with hyperthermia (temperature >37.2°C) were managed with adequate breast feeding, oral paracetamol and optimal room temperature and ventilation. Sepsis was suspected in the presence two or more of the following conditions: weak or abnormal cry, poor suck or inability to suck, drowsy or unconsciousness, temperature >37.2°C or <35°C, multiple skin pustules or pus draining from umbilicus, persistent vomiting or abdominal distension and fast breathing (respiratory rate more than 60/min in a quiet infant). All infants with probable sepsis were referred to a health facility. If the family refused or was unable to go to a health facility but consented to home treatment, the worker managed the infant at home with oral cotrimoxazole and IM gentamicin. The project team at the sites ensured supplies of equipment and drugs for managing newborns at home in both the intervention arms. All the SRs and AWWs were provided a kit containing weighing scale, thermometer, bag and mask, syringes and medicines (box 1). They were also provided performance-linked remuneration up to Rs.350 (US$6) per month.
Box 1. Components of Shishu Rakshak kit during visits.
Weighing scale.
Thermometer.
Wrist watch.
Cotton balls for wiping thermometer.
Soap.
Booklet of forms.
Extra forms.
Warm bag.
Blanket.
Health education flip chart.
High-risk information sheets (3).
A square piece of clean cloth to spread and keep the items.
Medicines
Syr. Cotrimoxazole.
Inj. Gentamicin.
Spirit soaked cotton balls.
Gentian violet paint.
Syr. Paracetamol.
Syringes.
Chloramphenicol eye-drops.
Syr. Salbutamol.
Tea spoon/pallady for teaching feeding newborns with expressed breast milk.
In the control arm, the ANM/AWWs provided antenatal and newborn care services through antenatal contacts and three postnatal home visits as per the ongoing Reproductive and Child Health programme. All study clusters—irrespective of the random group allocation—were open to concomitant improvements and changes in the healthcare and developmental activities driven by the respective state governments. For example, as a part of the National Rural Health Mission (NRHM), facility strengthening took place, accredited social and health activists (ASHA) got deployed and Janani Suraksha Yojana (JSY) got scaled up in all the three arms during implementation of the trial.
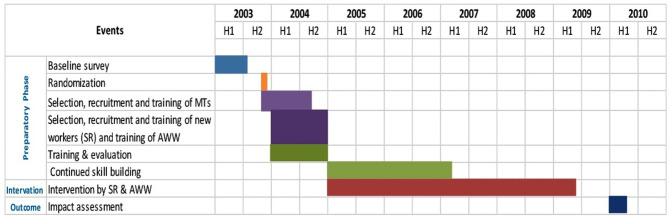
Implementation of the intervention began in January 2005 (figure 1). However, the full package of interventions including IM injections for probable sepsis could be implemented from only 2007 because of the delay in obtaining ethical clearance for this particular intervention and the longer time required to acquire the skills by the workers. In the AWW arm, injection component could not be imparted because permission was not granted for AWWs to administer IM injections. A district steering committee was constituted at each site that met every 6–12 months to address issues related to implementation. The health authorities at the district level were involved in the study from the planning stage. The District Health Officer was designated as coinvestigator in this study and ANMs, LHVs were envisaged to provide supportive supervision to SRs/AWWs.
Figure 1.
Study timeline. AWW, anganwadi workers; SR, Shishu Rakshak; MT, master trainer.
Data collection
During the intervention phase, the SRs and AWWs collected data and maintained records of past pregnancy, problems during current pregnancy and delivery details including duration of labour, place of delivery, personnel conducting delivery, type of delivery, birth outcomes for all pregnant women. They also recorded the need for resuscitation at birth, time of first visit to the baby, time of initiation of breastfeeding, birth weight and morbidities detected on follow-up visits for all the babies. They were monitored by a supervisor (1 for every 20–30 workers) who crosschecked the information collected by them on randomly identified cases and validated all the births and deaths by visiting the households and/or verifying with other sources. The supervisor also provided on-job training to the workers and refresher training during monthly meetings. He/she did not fill-up any separate forms.
In addition, the coverage data for other key indicators such as home visits for health education during antenatal period, home deliveries attended by SRs and AWWs, first examination of infant within 24 hours of birth (only for home deliveries), postnatal home visits and sepsis cases managed were recorded from the self-reported service delivery records of SR and AWW.
Outcomes and their measurement
Primary outcome measures were the endline neonatal and YIMR at the end of the intervention period (2008–2009). NMR and YIMR were defined as the number of deaths within 28 days and within 59 days of life, respectively per 1000 live births. The secondary outcomes were early-NMR (deaths within 6 days of life/1000 live births), infant mortality rate (IMR; deaths from 0 to 364 days/1000 live births), stillbirth rate (stillbirths per 1000 births) and perinatal mortality rate (stillbirths plus early neonatal deaths per 1000 births).
Evaluation of the intervention was done by means of an endline cross-sectional survey conducted from January 2010 to April 2010. The survey got delayed by about 9 months due to practical reasons (the intervention phase was over by March 2009; last follow-up home visit was done in May 2009). An independent team who had no role in implementation of the intervention conducted the survey using similar methods and tools as the baseline survey. The team was provided names of all the PHCs/villages and the data collection tools of the baseline survey. Extensive efforts were made to ensure complete enumeration of all households in the intervention and control arms.
The survey team collected information on births, deaths and other key demographic indicators for all the births in the clusters as well as for those births in which the mothers delivered outside the cluster areas but returned within 2 months of the date of delivery. For convenience of enrolled mothers, information was collected for the period from Holi festival in March 2008 to Holi in March 2009. Process outcome: In addition to the mortality indicators, coverage in the intervention arms was also assessed by recording the proportion of births attended by the SRs and AWWs for the period from 22 March 2008 to 21 March 2009 in the two intervention arms.
Quality control of data
Data were double entered in CSpro database that had built-in range and consistency checks. The surveillance supervisors–1 for every 5–6 field workers of the survey team–independently filled up the forms of 5% infants and then cross-checked with the forms submitted by the field workers. They also checked all details of randomly selected 5% households by through spot checks and reinterviews. In addition, the members of central coordinating team also independently validated the details of births and deaths in a randomly selected sample during their field visits. The central team also observed a few interviews conducted by the field workers.
Statistical analysis
Assuming a baseline NMR of 40/1000 live births, design effect of 1.5, 95% level of confidence (one sided), and 80% power, we had to enrol 1500 live births in each arm to detect 50% reduction in NMR in the two intervention arms. The estimated sample size was more than enough to detect the same quantum of reduction in the other primary outcome (young infant mortality with baseline rate of 50/1000 live births) also. With the prevailing birth rate of 25/1000 population, it was expected that two PHCs with an average population of 30 000 each had to be included for enrolling 1500 live births in a year. Therefore, two PHCs were included in each of the three arms. This sample size calculation was for each state. However, the mid-term survey—planned a priori to inform the Project Advisory Committee (PAC) and DSMB—showed a secular trend with lower NMR and YIMR in all the arms including the control arm (see online supplementary web table 2). In view of the low baseline NMR than expected, the PAC recommended to analyse the results from all five sites together to have a single effect size at the end of the study.
bmjgh-2017-000680supp002.pdf (40.6KB, pdf)
Analysis was by intention to treat at cluster and participant levels. We analysed the data from all the sites together with adjustment for clusters, as per the DSMB approved plan of analysis (see ‘online supplementary: Plan of analysis’). Means and proportions of background characteristics were compared using analysis of variance and X2 test. Mortality rates were adjusted for religion, caste, resident status (resident/visitor), and education at the individual level, and distance to district hospital (<25 km), access to PHC or CHC, presence of private clinics, provision of JSY and presence of ASHA at the cluster level. The adjusted ORs, along with 95% CIs, of mortality rates were estimated for each intervention arm—after adjusting for cluster design—by using ‘logistic’ model in Stata V.11.2 (StataCorp). For cluster adjustment, we considered each village as a ‘cluster’ because the outcomes were more likely to be correlated within the village than the PHCs (which were only 10 in each arm).
bmjgh-2017-000680supp003.pdf (189.9KB, pdf)
The study was registered with Clinical Trial Registry of India (CTRI/2011/12/002181).
Role of funding source
The ICMR, the central research organisation under the aegis of the Ministry of Health and family Welfare, Government of India, conducted the present study as a Task Force study. The organisation did not receive any external funding for this study.
Results
Figure 2 shows the trial profile. Out of the 45 clusters (ie, PHCs) assessed for eligibility, 30 were chosen based on NMR and home births and were randomly allocated to SR, AWW or control arms.
Figure 2.
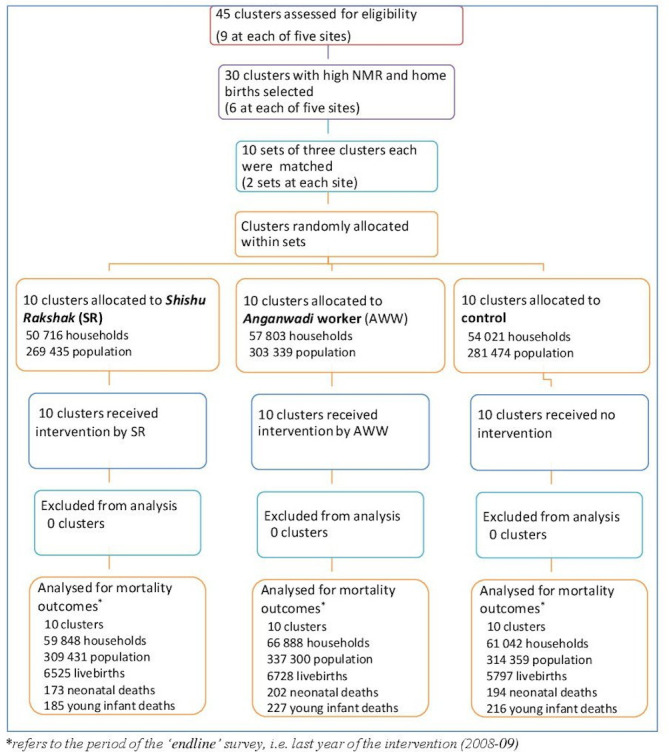
Study profile. NMR, neonatal mortality rate.
Demographic characteristics and baseline mortality rates
Table 2 shows the demographic characteristics of enrolled clusters at baseline period (2002–2003).
Table 2.
Demographic characteristics and baseline mortality rates (2002–2003)
| Characteristics | SR arm | AWW arm | Control arm |
| Population | 269 435 | 303 339 | 281 474 |
| Households | 50 716 | 57 803 | 54 021 |
| Births | 6349 | 6650 | 6365 |
| Live births | 6210 | 6519 | 6223 |
| Still births | 139 | 131 | 142 |
| Caste | |||
| SC/ST | 17 802 (35.1) | 20 404 (35.3) | 19 772 (36.6) |
| Others | 32 914 (64.9) | 37 339 (64.7) | 34 249 (63.4) |
| Maternal education | |||
| Illiterate | 3968 (62.5) | 3937 (59.2) | 3673 (57.7) |
| Literate | 2381 (37.5) | 2713 (40.8) | 2692 (42.3) |
| Place of delivery | |||
| Home | 4710 (74.2) | 4894 (73.6) | 4423 (69.5) |
| Facility | 1639 (25.8) | 1756 (26.4) | 1942 (30.5) |
| Delivery by skilled birth attendant | 2013 (31.1) | 2082 (31.1) | 2091 (32.7) |
| NMR per 1000 live births | 52.9 (47.4–58.6) | 53.7 (48.2–59.2) | 55.0 (49.3–60.7) |
| Young infant mortality rate per 1000 live births | 61.0 (55.0–67.0) | 61.1 (55.3–66.9) | 59.6 (53.7–65.5) |
Data presented as n (%) or mean (95% CI).
AWW, anganwadi workers; NMR, neonatal mortality rate; SC/ST, scheduled caste/scheduled tribe; SR, Shishu Rakshak.
The baseline survey covered 50 716, 57 803 and 54 021 households in SR, AWW and control arms, respectively. The level of maternal education and the proportion of women from socially disadvantaged groups were similar in the three arms. Only one-fourth of deliveries happened at a health facility, and less than one-third were attended by a skilled birth attendant in all the arms. The NMR ranged from 53 to 55 per 1000 live births while the YIMR varied from 60 to 61 per 1000 live births in the three arms (table 2).
Coverage of interventions
Table 3 shows the coverage of study interventions in the two intervention arms. The source of this information was the service delivery record of SRs and AWWs (available for 4788 and 3956 deliveries, respectively). When compared with AWW arm, more women received home visits during the antenatal period, a higher proportion of deliveries at home were attended by the worker, more newborns were examined within 24 hours after birth, and more infants were suspected to have sepsis in the SR arm. About one-third (39.8%) of infants with probable sepsis in the SR arm received oral cotrimoxazole and IM gentamicin; another one-fifth received oral cotrimoxazole alone. In the AWW arm, about half of the infants (53.2%) with probable sepsis received oral cotrimoxazole alone; no IM injections were administered in this arm. When compared with SR arm, the proportion of infants being referred to a health facility was higher in the AWW arm (table 3). No adverse events related to IM injection administration were documented in the SR arm. Out of the 259 SRs recruited, 82% (212) had acquired desired injection skills.
Table 3.
Coverage of study interventions in SR and AWW arms
| Intervention | SR (n=4788) | AWW (n=3956) |
| Home visits | 4546 (94.9) | 3427 (86.6) |
| Deliveries at home attended by the concerned health worker | 959/1448 (64.4) | 340/1267 (26.8) |
| First examination of infant within 24 hours after birth (in home deliveries only) | 1120/1378 (81.3) | 701/1272 (55.1) |
| Postnatal home visits for newborns | n=4600 | n=3805 |
| No of high-risk visits (median) | 13 | 11 |
| No of normal visits (median) | 11 | 9 |
| Probable sepsis | ||
| Total infants suspected | 462 (10.0) | 329 (8.6) |
| Received only oral cotrimoxazole | 90 (19.5) | 175 (53.2) |
| Received oral cotrimoxazole and IM gentamicin* | 184 (39.8) | Nil |
| Referred to a health facility | 188 (40.7) | 154 (46.8) |
Data presented as n (%).
*IM gentamicin was administered in only SR clusters.
AWW, anganwadi workers; IM, intramuscular; SR, Shishu Rakshak.
Endline survey
The endline survey (for 2008–2009 period) covered 59 848, 66 888 and 61 042 households in SR, AWW and control arms, respectively (table 4). Maternal age and religion were similar in the three arms but there was significant difference in the caste distribution—about 21% of women in the control arm belonged to general category (‘others’) in contrast to 14% of the women in SR and AWW arms. More villages in the control arm had a district hospital within 25 km radius, an ASHA provider, and a functioning JSY programme as compared with the villages in the two intervention arms. More villages in the AWW arm had access to a private health facility (table 4).
Table 4.
Demographic characteristics during ‘endline’ period (2008–2009)
| SR arm | AWW arm | Control arm | |
| Population | 309 431 | 337 300 | 314 359 |
| Households | 59 848 | 66 888 | 61 042 |
| Births | 6623 | 6852 | 5898 |
| Live births | 6525 | 6728 | 5797 |
| Still births | 98 | 124 | 101 |
| Religion | |||
| Hindu | 6207 (93.7) | 6351 (92.7) | 5329 (90.3) |
| Muslim | 346 (5.2) | 438 (6.4) | 508 (8.6) |
| Others | 70 (1.1) | 63 (0.9) | 61 (1.1) |
| Caste | |||
| Scheduled caste | 1417 (21.3) | 1443 (21.0) | 1285 (21.7) |
| Scheduled tribe | 755 (11.4) | 1036 (15.2) | 659 (11.2) |
| Other backward castes | 3522 (53.2) | 3402 (49.6) | 2740 (46.4) |
| Others | 929 (14.0) | 971 (14.2) | 1214 (20.7) |
| Maternal education | |||
| Illiterate | 1331 (20.0) | 1346 (19.7) | 1379 (23.4) |
| Primary to middle school | 1348 (20.4) | 1475 (21.5) | 1412 (24.0) |
| High school and above | 3844 (59.6) | 4031 (58.8) | 3107 (52.6) |
| Proportion of villages with | n=351 | n=430 | n=344 |
| Access to primary health centre* | 27 (7.8) | 50 (11.6) | 31 (8.8) |
| Access to community health centre* | 21 (6.1) | 37 (8.0) | 10 (2.8) |
| Distance to district hospital <25 km | 38 (11.0) | 103 (23.9) | 164 (46.7) |
| Private clinic/nursing home | 13 (2.8) | 23 (5.3) | 10 (2.8) |
| ASHA provider | 299 (86.9) | 346 (80.5) | 312 (88.9) |
| Functioning JSY programme | 307 (89.2) | 350 (81.4) | 326 (92.8) |
| Antenatal visit(s) by ANM | n=6341 | n=6560 | n=5688 |
| At least 1 visit | 5892 (92.9) | 5740 (87.5) | 5270 (92.6) |
| >3 visits | 2129 (33.6) | 2702 (41.2) | 2698 (47.4) |
| Tetanus immunisation | 6037/6448 (93.6) | 6019/6643 (90.6) | 5350/5717 (93.6) |
| Place of delivery | |||
| Home | 2057 (31.0) | 2440 (35.6) | 1737 (29.4) |
| Facility | 4566 (69.0) | 4412 (64.4) | 4161 (70.6) |
| Delivery attended by | n=5515 | n=5675 | n=5015 |
| Unskilled personnel | 807 (14.6) | 924 (16.3) | 719 (14.3) |
| Skilled birth attendant | 4708 (85.4) | 4751 (83.7) | 4296 (85.7) |
| Mother received payment under JSY (for deliveries at health facility) | 3208/4566 (70.3) | 3285/4412 (74.5) | 2633/4161 (63.3) |
Data are number (%).
*Access to health facility means that the village is connected by all-weather road to a health facility.
ANM, auxiliary nurse midwives; ASHA, accredited social health activist; AWW, anganwadi workers; JSY, Janani Suraksha Yojana; SR, Shishu Rakshak.
Key indicators during endline period (2008–2009)
Most women had at least one antenatal visit by ANM in all the three arms; the proportion of women who had three or more antenatal visits by ANMs was, however, low in the SR arm when compared with the other two arms (table 4). About two-thirds of deliveries occurred in health facilities, though the proportion of facility births was lower in the AWW arm. More than 90% of women received tetanus immunisation in all the arms. A higher proportion of mothers who delivered in health facilities in the SR and AWW arms than those in the control arm received payment under JSY programme (table 4).
Outcomes: mortality rates
Table 5 provides the mortality rates in the three arms. There were 173, 202 and 194 neonatal deaths, respectively, in the SR, AWW and control arms during the final year of intervention. The risk of neonatal mortality was 25% lower in the SR arm than the control arm (adjusted OR 0.75, 95% CI 0.57 to 0.99). There was also a significant reduction in the risks of early neonatal mortality, young infant mortality and infant mortality—by 32%, 27% and 33%, respectively—in infants in the SR arm when compared with those in the control arm (table 5). The stillbirth rate was not different between the SR and control arms, but the perinatal mortality rate was significantly lower in the former (adjusted OR 0.73, 95% CI 0.57 to 0.93).
Table 5.
Mortality rates of infants born in the final year of intervention*
| SR | AWW | Control | SR versus control; adjusted OR† (95% CI) | AWW versus control; adjusted OR† (95% CI) | |
| Neonatal mortality rate (per 1000 live births) |
26.5 | 30.0 | 33.5 | 0.75 (0.57 to 0.99) | 0.85 (0.65 to 1.09) |
| Early neonatal mortality rate (per 1000 live births) |
17.9 | 22.9 | 24.8 | 0.68 (0.52 to 0.90) | 0.87 (0.66 to 1.16) |
| Young infant mortality rate (per 1000 live births) |
28.3 | 33.7 | 37.3 | 0.73 (0.56 to 0.95) | 0.86 (0.66 to 1.10) |
| Infant mortality rate (per 1000 live births) |
37.7 | 46.1 | 52.4 | 0.67 (0.54 to 0.83) | 0.81 (0.65 to 1.02) |
| Stillbirth rate (per 1000 births) |
14.8 | 18.1 | 17.3 | 0.81 (0.56 to 1.16) | 1.06 (0.79 to 1.41) |
| Perinatal mortality rate (per 1000 births) |
32.5 | 40.6 | 41.5 | 0.73 (0.57 to 0.93) | 0.94 (0.75 to 1.19) |
*Between Holi festival in March 2008 and next Holi in March 2009.
†Adjusted for religion, caste, resident status and education at the individual level, and distance to district hospital (<25 km), access to PHC or CHC, presence of private clinics, provision of Janani Suraksha Yojana and ASHA in the village; cluster adjusted for villages.
ASHA, accredited social and health activists; AWW, anganwadi workers; CHC, community health centres; PHC, primary health centres; SR, Shishu Rakshak.
The risks of neonatal mortality, early neonatal mortality, young infant mortality and infant mortality in infants born in the AWW arm were, however, not different from those born in the control arm; similarly, there was no difference in the stillbirth rate or perinatal mortality rate between the AWW and control arms (table 5).
Discussion
The present study showed a significant reduction in the neonatal, young infant and infant mortality rates in the SR arm—but not in the AWW arm—when compared with the control arm (table 5). The coverage of intended interventions like home visits for health education during AN period, deliveries at home attended by SR/AWW and postnatal visits within 24 hours of birth was significantly higher in the SR arm than the AWW arm (table 3). The study, therefore, confirms the effectiveness of HBNC package, if delivered by a dedicated village level worker and a reasonably high coverage is achieved.
The findings of the present study are not entirely ‘new’; rather they reaffirm the results of the previous community-based cluster RCTs on HBNC from South Asia6–9 and Africa.10 An earlier systematic review that included five such trials from South Asia6–9 11 found a significant reduction in NMR following HBNC (pooled RR 0.75; 95% CI 0.61 to 0.92).12 It had suggested a greater beneficial effect with a higher baseline NMR (>50 per 1000 live births) based on the results of subgroup and meta-regression analyses.12 We found a similar magnitude of reduction in NMR in the SR arm—adjusted OR 0.75; 95% CI 0.57 to 0.99. Our results are particularly noteworthy because of the low ‘endline’ NMR—33.5 per 1000 live births—in the control arm. The updated meta-analysis including the trial from Africa10 and the present study revealed 22% reduction in NMR following home based care (seven studies; pooled effect size 0.78; 95% CI 0.67 to 0.90; see ‘online supplementary web figure 1’).
bmjgh-2017-000680supp004.pdf (103.2KB, pdf)
Of the two intervention arms, only one (SR) showed a significant reduction in the neonatal and YIMR while the other (AWW) did not. This apparent discrepancy in beneficial effects between the SR and AWW arms is unlikely due to underlying differences in baseline characteristics between the two arms (given the similar demographic characteristics like NMR and place of birth; table 2). The key components of intervention were also the same, except for IM injections for probable sepsis (table 1). The major difference between the two arms, apparently, was the presence of a new, dedicated health worker—SR—in the SR arm. It seems that her presence ensured much higher coverage of key interventions like home visits during AN period and first postnatal home visit within 24 hours after birth in the SR arm than in the AWW arm (table 3). About 40% of infants with probable sepsis in the SR arm did receive IM gentamicin along with oral cotrimoxazole whereas no IM injections were administered in the AWW arm. But provision of IM injections alone is unlikely to explain the difference in effect between the two arms given that only 40% of eligible infants received IM injections in the SR arm. Hence, the discrepancy observed in beneficial effects between the SR and AWW arms was most likely due to delivery of the interventions by a dedicated health worker and not by the ‘routine’ staff. Interestingly, the subgroup analysis in the updated meta-analysis based on the presence of dedicated/specially recruited health worker showed 36% and 12% reduction in NMR, respectively, in the studies with and without dedicated health worker (see online supplementary web figures 1 and 2). The magnitude of benefit observed in the AWW arm—15% reduction—is consistent with the pooled effect size of the studies that employed only existing health staff. Indeed, the present study has possibly addressed a major policy dilemma faced by most governments in low-income and middle-income countries—whether to deliver the home-based package of newborn interventions by a dedicated health worker or by the existing village level worker. Unlike the SR, the AWW had to take care of her routine tasks like child development and nutrition, in addition to delivering the study interventions. The modest and non-significant benefits observed in the AWW arm despite training, incentive, and supervision demonstrates that there are limits to expanding the multitasking role by a given class of providers beyond their primary mandate.
bmjgh-2017-000680supp005.pdf (137.5KB, pdf)
The other interesting and programme-relevant finding of the study relates to the effects of the intervention on early NMR and infant mortality rates. Infants in the SR arm had 32% lower mortality in the first week of life—the observed effect size for early NMR was more than that of NMR (32% vs 25%; table 5). The beneficial effects in early NMR were observed in facility births also (online supplementary web table 3), which underscores the need for postnatal home visits by the health workers in the first few days of life, irrespective of the place of birth. Infants in the SR arm had 27% lower mortality in 0–59 days (young infant mortality) and 33% reduction in 0–364 days (infant mortality; table 5). This could be due to the ‘lasting’ effect of the family and provider-counsellor contact, in the crucial days including antenatal and postnatal period, on healthy behaviours like exclusive breastfeeding and care-seeking. Newborns are likely to fall sick even if they are delivered at facility when they return home after discharge from the hospital. HBNC ensures continuam of care beginning from care during antenatal period, through labour and birth, followed by care at postnatal period. This is an additional convincing argument in favour of scaling up HBNC for further reduction in neonatal including early NMR.
bmjgh-2017-000680supp006.pdf (49.8KB, pdf)
Strengths and limitations
The major strengths of the study are the cluster randomised study design, having two intervention arms to address the pertinent question on the need to have a dedicated health worker to deliver the package of interventions, the package of interventions being similar to the original HBNC package in the Gadchiroli study,5 similar and independent measurement of outcomes in the intervention and control clusters, and large sample size.
The study has important limitations too. First, the outcomes were measured by a survey and not by ongoing surveillance of births and deaths in the clusters. Also, the survey was conducted almost a year after the completion of intervention phase. The risk of recall bias and bias in categorising the deaths—neonatal ersus postneonatal mortality—cannot be ruled out. But given the nature of the outcome (death) and the overall pattern in reduction of different mortality rates in the SR clusters, the risk of these biases is likely to be low; also, the recall bias is likely to be similar in three arms. Second, the trial included only 10 clusters per arm. A smaller unit of randomisation, such as villages, would have improved the efficiency of cluster randomisation. Third, the coverage of interventions in both the SR and AWW arms was not optimal—a small but considerable proportion of infants did not receive the whole package of interventions in both the arms; less than half of the infants with probable sepsis received IM injections in the SR arm. If the coverage of interventions were almost universal, the observed beneficial effects could have been more striking.
With the launch of NRHM, several efforts were made to improve maternal child survival that resulted in substantial increase in numbers of institutional delivery at the time of endline evaluation. The proportion of facility births in the present study was around 67%—more than double the rate at baseline. Therefore, we did post hoc subgroup analysis based on the place of birth, which revealed results similar to that of overall study cohort for facility births—the risks of neonatal, early neonatal, infant, young infant and perinatal mortality were found to be significantly lower in the SR arm but there was no difference in the mortality rates between the AWW and control arms. Among home births, no difference was found in the mortality rates between either the SR and control arms or the AWW and control arms (possibly because of the small numbers and subsequent low power; online supplementary web table 3).
Implications for policy-makers
The findings of the present study have three major implications for the policy-makers. First, the HBNC package, if delivered optimally, has the potential to reduce both neonatal (including early neonatal) and infant mortality rates. The effect on early neonatal mortality is particularly important because of the high proportion of deaths occurring in the first week of life and the general lack of interventions known to reduce the early NMR. Second, to achieve maximum benefits, presence of a dedicated health worker is a must. Third, the intervention is relevant even in settings with high rates of facility births.
Conclusions
This cluster randomised community-based trial conducted at five sites across India confirms that the HBNC package is feasible to deliver and is effective in reducing neonatal and YIMR, particularly when delivered by a dedicated worker devoted to only maternal/neonatal care. The intervention package was effective even in settings with high rates of institutional births.
Acknowledgments
We are grateful to Dr. MK Bhan (Department of Biotechnology (DBT) New Delhi -Chair, project advisory group), Dr. S Bhargava (New Delhi), Dr. R Kumar (PGIMER Chandigarh), Dr. AT Bang (SEARCH Gadchiroli) for ongoing review of the study and constructive suggestions. We also acknowledge contribution of DSMB members –Dr. VI Mathan (Chennai), Dr. S Ghosh (New Delhi) Ϯ, Dr. P Singh (EPOS Health India, Delhi). Coordinating unit: We acknowledge the technical assistance provided by KK Ganguly, S Chauhan, Arnab, Ajitha, Barnali, Meenakshi, Sonia, Mohan and Garima during implementation of the project and technical guidance received from Dr. M. Roy. We acknowledge the contribution of I Kambo (ICMR) and S Datey (ICMR), Dr. N Bhandari (Society for Applied Studies, New Delhi), Dr. R Bahl (WHO, Geneva), during project planning and implementation. We are grateful to SEARCH for technical contents of HBNC, designing and providing training to master trainers and supervisors. We acknowledge the training support (for master trainers) provided by Priya Paranjpe, Pradip Paranjpe, S Baitule, MD Deshmukh (SEARCH). We are grateful to the family members as well as Department of Health & Family Welfare, governments of Bihar, Odisha, Maharashtra, Rajasthan and Uttar Pradesh for their support and cooperation during implementation of the study.
Footnotes
Handling editor: Stephanie M Topp
Collaborators: ICMR-HBMYI Study Group: Investigators team:D Ganguly, S Kumar, R P Singh, SK Jha, U Prasad, U K Singh, M S Bharambe, P V Bahulekar, A Mohanty, H K Dash, L Kanungo, R K Dattatreya, J K George, K Sen, A Dadhich; A Srivastava, N Agarwal, S Shakir, S Singh; Endline survey team: R J Yadav, R K Gupta, T Adhikari, A Juneja, A Kumar, D Sahu, J Singh, R K Sharma.
Contributors: NCS, RR, SR VKP and ATB conceptualised and contributed significantly to the design of the study. Collaborating sites: Investigators implemented the study in the field at five sites. NCS and RR coordinated the study. AT Bang, Priya Paranjpe and Pradip Paranjpe, S Baitule trained master trainers, monitored training at sites. SR, VKP, R Kumar, AT Bang, NCS, RR, AS contributed to study implementation and monitoring. SK, NCS, AP, RMP, HSS, D Sahu, J Singh, MJS, RR, AS, VKP, SR helped in analysis and interpretation of data. RR wrote the first draft of the manuscript. RR and MJS did literature review. MJS and VKP analysed research in context. RR, VKP, MJS, SR finalised the draft manuscript. All other authors provided input, reviewed results, contributed to the final manuscript. Central Coordinating Unit—Indian Council of Medical Research (ICMR), Ansari Nagar, New Delhi: NCS, RR, AS, SK, M Roy. Investigators: Patna Medical College Hospital (PMCH), Patna, Bihar: S Pandey (site principal investigator), S Sinha, D Ganguly, S Kumar, R P SinghϮ, SK Jha, U Prasad, U K Singh: Mahatma Gandhi Institute of Medical Sciences (MGIMS), Sevagram, Wardha, Maharashtra: BS Garg (site principal investigator), S Gupta, M S Bharambe, P V Bahulekar: National Institute of Applied Human Research & Development (NIAHRD), Cuttack, Odisha: S Swain (Site Principal Investigator), A MohantyϮ, H K Dash, L Kanungo. Action Research and Training for Health, (ARTH), Udaipur, Rajasthan: SD Iyengar (Site Principal Investigator), R K Dattatreya, J K George, K Sen, A Dadhich. King George Medical University (KGMU), Lucknow, Uttar Pradesh: V Das (site principal investigator), G K MalikϮ, A Srivastava, N Agarwal, S Shakir, S Singh. Project Implementation Committee: S Ramji (Maulana Azad Medical College (MAMC), New Delhi, VKP (All India Institute of Medical Sciences (AIIMS), New Delhi), R Kumar (Post Graduate Institute of Medical Education and Research (PGIMER), Chandigarh), A T Bang (Society for Education, Action and Research in Community Health (SEARCH), Gadchiroli, Maharashtra), RR, AS, NCS, M Roy. Data Management Team: (ICMR)- S Kumar (coordinator), NCS, RR, AS. Endline evaluation team (National Institute of Medical Statistics (NIMS), New Delhi): - A Pandey (Coordinator), R J Yadav, R K Gupta, T Adhikari, A Juneja, A Kumar, D Sahu, J Singh; Regional Medical Research Center for Tribals (RMRCT), Jabalpur–R K Sharma. Data analysis and interpretation: A Pandey (NIMS), RMP (AIIMS), NCS (ICMR), SK (ICMR), MJS (AIIMS), RR (ICMR), AS (ICMR), VKP (AIIMS), SR (MAMC), HSS, Sitaram Bhartia Institute of Science and Research (SBISR) New Delhi. Systematic review for research in context: MJS, VKP. Project Investigator and team leader: NCS and RR. Writing committee: MJS, RR, SR and VKP.
Funding: This study was funded by Ministry of Health and family Welfare, Government of India and Indian Council of Medical Research (ICMR).
Competing interests: None declared
Patient consent for publication: Not Required
Ethics approval: The Central Ethics Committee of Indian Council of Medical Research (ICMR) as well as institutional ethics committees at each participating centre approved the project.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: The full data set is available from the corresponding author 1.
Contributor Information
On behalf of the ICMR -HBMYI Study Group:
A Dadhich, A Juneja, A Mohanty, A Kumar, A Srivastava, D Ganguly, D Sahu, H K Dash, J K George, J Singh, K Sen, L Kanungo, M S Bharambe, N Agarwal, P V Bahulekar, R J Yadav, R K Dattatreya, R K Gupta, R K Sharma, R P Singh, SK Jha, S Kumar, S Shakir, S Singh, T Adhikari, U K Singh, and U Prasad
References
- 1. Wang H, Bhutta ZA, Coates MM, et al. . Global, regional, National, and selected subnational levels of stillbirths, neonatal, infant, and under-5 mortality, 1980-2015: a systematic analysis for the global burden of disease study 2015. Lancet 2016;388:1725–74. 10.1016/S0140-6736(16)31575-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Registrar General of India Sample registration system (SRS) statistical report 2014. New Delhi, 2016. [Google Scholar]
- 3. Lassi ZS, Bhutta ZA. Community-based intervention packages for reducing maternal and neonatal morbidity and mortality and improving neonatal outcomes. Cochrane Database Syst Rev 2015:CD007754. 10.1002/14651858.CD007754.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Bhutta ZA, Das JK, Bahl R, et al. . Can available interventions end preventable deaths in mothers, newborn babies, and stillbirths, and at what cost? Lancet 2014;384:347–70. 10.1016/S0140-6736(14)60792-3 [DOI] [PubMed] [Google Scholar]
- 5. Bang AT, Bang RA, Baitule SB, et al. . Effect of home-based neonatal care and management of sepsis on neonatal mortality: field trial in rural India. Lancet 1999;354:1955–61. 10.1016/S0140-6736(99)03046-9 [DOI] [PubMed] [Google Scholar]
- 6. Kumar V, Mohanty S, Kumar A, et al. . Effect of community-based behaviour change management on neonatal mortality in Shivgarh, Uttar Pradesh, India: a cluster-randomised controlled trial. Lancet 2008;372:1151–62. 10.1016/S0140-6736(08)61483-X [DOI] [PubMed] [Google Scholar]
- 7. Baqui AH, El-Arifeen S, Darmstadt GL, et al. . Effect of community-based newborn-care intervention package implemented through two service-delivery strategies in Sylhet district, Bangladesh: a cluster-randomised controlled trial. Lancet 2008;371:1936–44. 10.1016/S0140-6736(08)60835-1 [DOI] [PubMed] [Google Scholar]
- 8. Darmstadt GL, Choi Y, Arifeen SE, et al. . Evaluation of a cluster-randomized controlled trial of a package of community-based maternal and newborn interventions in Mirzapur, Bangladesh. PLoS One 2010;5:e9696. 10.1371/journal.pone.0009696 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Bhutta ZA, Soofi S, Cousens S, et al. . Improvement of perinatal and newborn care in rural Pakistan through community-based strategies: a cluster-randomised effectiveness trial. Lancet 2011;377:403–12. 10.1016/S0140-6736(10)62274-X [DOI] [PubMed] [Google Scholar]
- 10. Kirkwood BR, Manu A, ten Asbroek AHA, et al. . Effect of the Newhints home-visits intervention on neonatal mortality rate and care practices in Ghana: a cluster randomised controlled trial. Lancet 2013;381:2184–92. 10.1016/S0140-6736(13)60095-1 [DOI] [PubMed] [Google Scholar]
- 11. Bhandari N, Mazumder S, Taneja S, et al. . Effect of implementation of integrated management of neonatal and childhood illness (IMNCI) programme on neonatal and infant mortality: cluster randomised controlled trial. BMJ 2012;344:e1634. 10.1136/bmj.e1634 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Gogia S, Sachdev HPS. Home-based neonatal care by community health workers for preventing mortality in neonates in low- and middle-income countries: a systematic review. J Perinatol 2016;36(Suppl 1):S55–73. 10.1038/jp.2016.33 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjgh-2017-000680supp001.pdf (41.9KB, pdf)
bmjgh-2017-000680supp002.pdf (40.6KB, pdf)
bmjgh-2017-000680supp003.pdf (189.9KB, pdf)
bmjgh-2017-000680supp004.pdf (103.2KB, pdf)
bmjgh-2017-000680supp005.pdf (137.5KB, pdf)
bmjgh-2017-000680supp006.pdf (49.8KB, pdf)