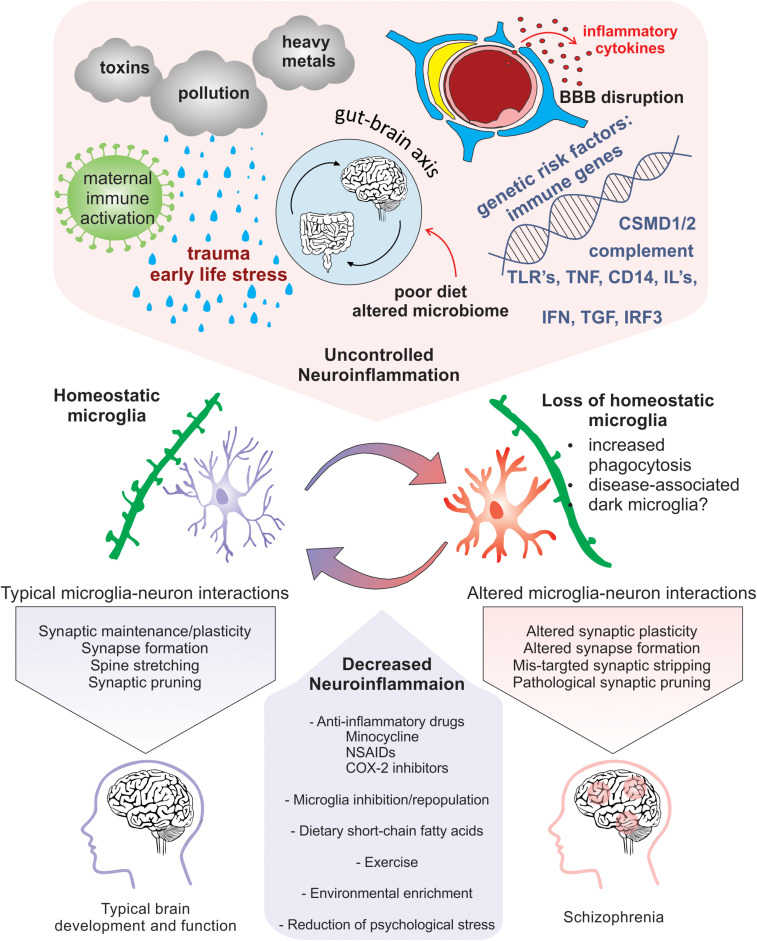
FIGURE 3.
Neuroinflammation-induced changes in microglia that are implicated in SCZ pathogenicity. Risk factors for SCZ that alter microglial function and enhance neuroinflammation include pollution, stress, nutrition induced gut-brain axis dysbiosis, viral infection, maternal immune activation, genetic predisposition, and cytokine secretion. Homeostatic microglia perform their immune sentinel role by interacting with neurons to guide circuit wiring during development. In an increased inflammatory milieu, loss of microglial homeostasis perturbs microglia-neuron interactions that may cause altered plasticity due to pathogenic synaptic formation, synaptic stripping, and pruning. Therapeutic approaches that promote homeostatic microglia through the reduction of neuroinflammation via anti-inflammatory drugs, microglial inhibition and repopulation, improved nutrition, environmental enrichment, and prevention of psychological stress could be potentially exploited to limit exacerbation of SCZ.