Figure 2.
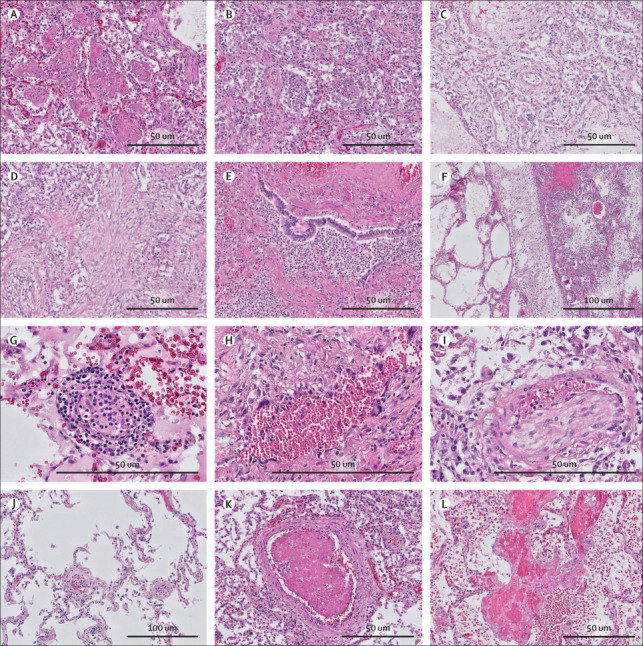
Lung histopathology in COVID-19
Different phases of diffuse alveolar damage were identified in COVID-19 (haematoxylin and eosin stain). (A) Exudative pattern with intra-alveolar fibrin exudation. (B) Exudative pattern with desquamation with early fibroblastic proliferation. (C) Proliferative diffuse alveolar damage with fibroblastic proliferation in the alveoli, partially incorporated in the alveolar septa. (D) Fibrosing phase of alveolar damage with collagen deposition (pink) in the areas with fibroblastic proliferation. (E) Exudative bronchopneumonia with neutrophil granulocyte infiltration of bronchi and surrounding alveolar parenchyma. (F) Patchy distribution of the acute damage and prominent lymphatic stasis in the septa. (G) Endotheliitis of small vessels (<100 μm) with infiltration of the endothelium and vessel wall by lymphocytes and plasma cells. (H) Giant cell transformation of the endothelium in a patient with longstanding COVID-19 (disease course 30 days). (I) Chronic thromboembolic vasculopathy with an organised thrombus in an arteriole. (J) Patchy thrombi in microvessels (<70 μm) and segregation of thrombocytes and neutrophil granulocytes in the vessels in the spared lung parenchyma. (K) New-formed thrombus in an arteriole. (L) Focal necrosis of the alveolar septa with blood and fibrin exudation in the parenchyma.
