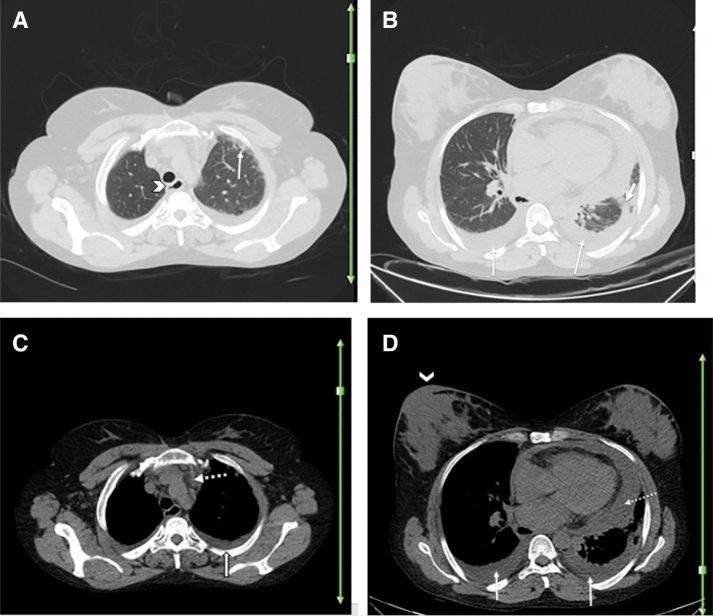
Fig. 5.
A 49-year-old woman with a history of well-controlled scleroderma and uncomplicated pregnancy and delivery 3 months ago, presented with fever, dry cough, and myalgia for 2 days. O2 saturation was 81%. Reverse transcription polymerase chain reaction was negative for SARS-CoV-2. Axial chest CT a–d shows bilateral pleural effusion (thin arrows; b–d) and pericardial effusion (dotted arrow; d) which are uncommon findings of COVID-19 in general population, but can be more common in patients with preexisting disease. Small focal patchy GGO in the left lower lobe (thick arrow; b) is noted, which can be related to COVID-19 or secondary to compressive atelectasis. Although the RT-PCR test was negative in this patient, due to high clinical suspicion, living in an epidemic region, suboptimal sensitivity of serologic test and recuperation after 2 weeks, COVID-19 was the clinical diagnosis for this patient. Subpleural interstitial reticulation in left upper lobe is suggestive of scleroderma-related lung involvement (thin arrow; a). A soft tissue opacity in left anterior mediastinum (dotted arrow; c) is noted, suggestive of thymus hyperplasia, which can be related to underlying scleroderma. Evidence of esophageal dilatation (arrowhead; a) may be suggestive of scleroderma related esophagus involvement and warrants further evaluation. Cutaneous thickening of the right breast (arrowhead; d) is noted, which can be due to infectious/inflammatory diseases of lactation phase versus SSc-related skin change or neoplastic in etiology and warrants correlation with physical exam findings