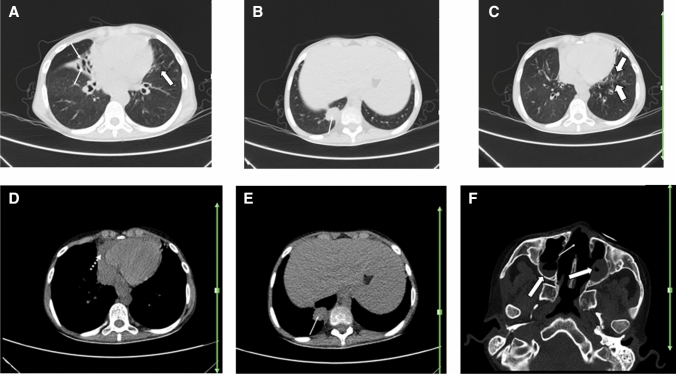
Fig. 7.
A 22-year-old man with a known history of granulomatosis with polyangiitis for over 1 year, presented with fever, dry cough, and shortness of breath. Reverse transcription polymerase chain reaction was positive for SARS-CoV-2. Axial chest CT shows ground glass opacities in lingula (thick arrows; a, c), which can be due to the patient’s known COVID-19 pneumonia versus pulmonary involvement by the underlying autoimmune disease. Diffuse central bronchiectasis (thin arrow; a), subpleural soft tissue density, non-calcified mass of 35 × 25 mm in the paravertebral basal segment of right lower lobe (arrows; b, e), pericardial effusion (dotted arrow; d), nasal septal osseous defect (thin arrow; f), and suggestive signs of sinusitis such as soft tissue opacity in left maxillary sinus, as well as fluid level in right maxillary sinus (thick arrows; f) are noted. These findings are suggestive of involvement of lower airways, pulmonary parenchyma, pericardial, and sino-nasal structures related to granulomatosis with polyangiitis. However, pericardial effusion can also be a rare finding in COVID-19