Abstract
Objective
To assess the diagnostic value of B-type natriuretic peptide (BNP) or N-terminal pro-B-type natriuretic peptide (NT-proBNP) for contrast-induced acute kidney injury (CI-AKI) in patients with acute coronary syndrome (ACS) undergoing coronary angiography.
Background
ACS remains a major cause of death worldwide. Patients with ACS undergoing coronary angiography are more likely to develop CI-AKI, which correlates highly with poor clinical outcomes. Early diagnosis of CI-AKI remains a challenge. Many recent studies have suggested that BNP or NT-proBNP may be a useful biomarker for the early diagnosis of CI-AKI.
Methods
We searched databases (PubMed, EMBASE, and Cochrane Library) to identify eligible studies. Two authors independently screened the studies and extracted data. We used the Quality Assessment of Diagnostic Accuracy Studies 2 (QUADAS-2) criteria to assess the methodological quality of the included studies and STATA to perform all statistical analyses.
Results
Nine studies including 2832 patients were identified. The pooled sensitivity of 0.73 (95% CI 0.65–0.79), specificity of 0.79 (95% CI 0.70–0.85), and area under the summary receiver operating characteristic curve of 0.81 (95% CI 0.77–0.84) suggested that BNP or NT-proBNP had a good diagnostic value for CI-AKI in patients with ACS undergoing coronary angiography.
Conclusions
Our findings suggest that BNP or NT-proBNP may be an effective predictive marker for CI-AKI. However, additional high-quality studies are required to find the optimal cutoff value and the diagnostic value of BNP or NT-proBNP in combination with other biomarkers.
1. Introduction
Acute coronary syndrome (ACS), including unstable angina (UA), non-ST elevation myocardial infarction (NSTEMI), and ST-elevation myocardial infarction (STEMI), generally results from atherosclerotic plaque rupture or superficial plaque erosion [1, 2]. Despite great progress in the treatment of ACS over the past few decades, ACS is still a major cause of death worldwide [3]. For patients with ACS, coronary angiography plays a key role. Early invasive treatment with cardiac catheterization and revascularization remains the preferred treatment for UA and NSTEMI, and timely percutaneous coronary intervention (PCI) for STEMI is recommended as a first-line treatment when prohibitive comorbidities are absent [4–6]. These treatments can reduce mortality and improve prognosis in patients with ACS.
Acute kidney injury (AKI) is a common and serious complication of inpatients that causes significant mortality and other severe complications [7, 8]. Patients with ACS, especially those undergoing coronary angiography or PCI, are more likely to develop AKI due to contrast agent exposure [9, 10]. The development of CI-AKI after coronary angiography is highly correlated with poor clinical outcomes, such as mortality [11–13], adverse cardiac events [14], and stent restenosis [15]. The ability to identify patients at high risk for developing CI-AKI identified early is important to allow the treating physician to take necessary precautions to prevent it.
Brain natriuretic peptides are released into the circulation in response to myocardial ischemia, pressure overload, or ventricular dilatation [16, 17]. Previous studies have found elevated concentrations of B-type natriuretic peptide (BNP) or N-terminal pro-B-type natriuretic peptide (NT-proBNP) in patients with ACS and have a prognostic value in patients with ACS [18, 19]. Moreover, some studies have found that levels of BNP or NT-proBNP are higher in patients with AKI [20–22], especially for those who are diagnosed with ACS and undergo coronary angiography or PCI [23–25].
To fully understand the correlation between elevated levels of brain natriuretic peptide and CI-AKI, we performed this meta-analysis to evaluate the diagnostic value of brain natriuretic peptide for CI-AKI in patients with ACS undergoing coronary angiography.
2. Methods
We conducted this meta-analysis following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA statement) guidelines [26]. There was no prospectively registered protocol; however, search terms, data extraction, inclusion and exclusion criteria, and data synthesis were applied according to a plan made by our team.
2.1. Selection of Studies
We reviewed PubMed, EMBASE, and the Cochrane Central Register of Controlled Trials Library database through April 2020. The search terms were as follows: (“B-type natriuretic peptide” or “BNP” or “N-terminal pro-B-type natriuretic peptide” or “NT-proBNP”) and (“acute kidney injury” or “AKI” or “contrast-induced acute kidney injury” or “CI-AKI” or “contrast-induced nephropathy” or “CIN”) and (“acute coronary syndrome” or “ACS” or “acute myocardial infarction” or “AMI” or “ST-elevation myocardial infarction” or “STEMI” or “Non–ST elevation myocardial infarction” or “NSTEMI” or “unstable angina”). We did not impose any language restrictions. To find additional citations, the reference lists of the included studies and recent reviews were manually searched when necessary.
Studies were selected if they met the following criteria: a diagnostic value of BNP or NT-proBNP for CI-AKI morbidity in adult patients (≥18 years old) with ACS undergoing coronary angiography or PCI was reported; a 2 × 2 table of results could be constructed; CI-AKI was clearly defined; and the study type was a prospective or retrospective study. The exclusion criteria were as follows: case report, review, editorial, conference abstract, comment, letter, animal study, involving pediatric patients, and insufficient information to extract a 2 × 2 table of results. Two authors (X. L and C. L) assessed the selected studies for the final analysis independently, and any discrepancies were resolved through consultation with the third author (F. Z).
2.2. Data Extraction and Quality Assessment
The following data were extracted by two authors (X. L and C. L) and checked by the third author (Z. M): the first author, year of publication, study design, sample size, average age, patient population, definition of CI-AKI, measurement method of brain natriuretic peptide, timing of brain natriuretic peptide measurement, cutoff points, area under the curve (AUC), true positives (TP), true negatives (TN), false positives (FP), false negatives (FN), sensitivity (SEN), and specificity (SPE).
We used the QUADAS-2 (Quality Assessment of Diagnostic Accuracy Studies-2) criteria to evaluate each of these studies in 4 domains: patient selection; index test; reference standard; and flow and test timing [27]. Any disagreements were resolved by discussion.
2.3. Statistical Analysis
The statistical analyses were conducted by STATA (version 14.0) using the MIDAS module [28]. A bivariate random-effects regression model was performed to calculate SEN, SPE, the positive likelihood ratio (PLR), the negative likelihood ratio (NLR), the diagnostic odds ratio (DOR), and the corresponding 95% credible interval (CI). A summary receiver operating characteristic (SROC) curve was drawn to assess the overall diagnostic accuracy [29]. We used the Deek funnel plots to detect publication bias, whereby publication bias may exist if the P value is less than 0.1. The I2 index was calculated to assess heterogeneity between studies, and I2 values above 50% were regarded as indicative of substantial heterogeneity. We generated a Fagan nomograph and likelihood ratio scattergram to evaluate clinical applications. Sensitivity and subgroup analyses were conducted to investigate potential sources of heterogeneity among the included studies.
3. Results
3.1. Selection and Characteristics of Studies
As a result of the literature search, 170 studies were identified, of which 55 duplicate publications were excluded. We excluded 101 studies for various reasons by evaluating the titles and abstracts.
The remaining 14 articles were further scrutinized by reading the full text. Four studies were excluded due to an inability to extract a 2 × 2 contingency table [30–33], and one retrospective study was excluded after discussion between two authors because it used peak NT-proBNP as the cutoff value [34]. In total, nine studies [23–25, 35–40] including 2832 patients fulfilled the inclusion criteria and were ultimately included in this meta-analysis (Figure 1).
Figure 1.
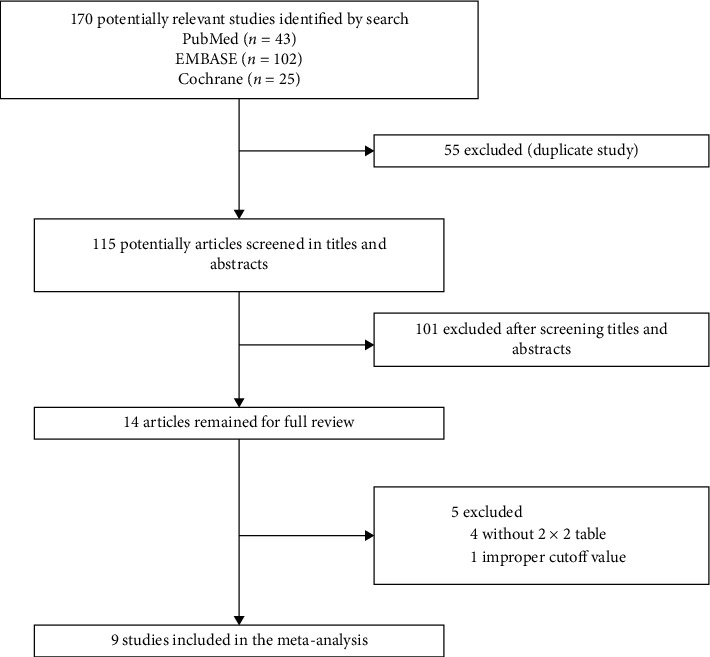
Flow diagram for the identification of eligible studies.
Table 1 summarizes the details of the nine included studies (prospective: 7; retrospective: 2). These studies were published between 2013 and 2020. Different SEN, SPE, and AUC values of BNP or NT-proBNP for the diagnosis of CI-AKI were reported. The AUC values in the studies ranged from 0.65 to 0.92, and the definition of CI-AKI varied. Five studies [23–25, 36, 37] measured NT-proBNP and four [35, 38–40] BNP. The decision cutoff value used in the studies varied widely between 42.4 and 676 pg/ml for BNP and between 512 and 2320 pg/ml for NT-proBNP (Table 2). Five studies included patients only with STEMI [24, 35, 37, 38, 40]. One study [37] was published in Russian, and the others were published in English.
Table 1.
Characteristics of included studies.
| Marker | Study | Study type | Definition of CI-AKI | Population | No. of patients | Male/female | Mean age |
|---|---|---|---|---|---|---|---|
| BNP | Akgul et al. 2013 [40] | Prospective | An absolute increase in SCr of ≥0.3 mg/dl or ≥50% from the baseline | STEMI patients undergoing PCI | 424 | 340/84 | 55.3 ± 12.0 |
| Moltrasio et al. 2014 [39] | Prospective | An absolute increase in SCr of ≥0.3 mg/dl | ACS patients undergoing PCI | 639 | 484/155 | 70.6 ± 12.5 | |
| Tung et al. 2015 [38] | Prospective | An absolute increase in SCr of ≥0.3 mg/dl or ≥50% from the baseline | STEMI patients undergoing PCI | 189 | 163/26 | 62.6 ± 13.9 | |
| Parenica et al. 2020 [35] | Retrospective | An absolute increase in SCr of ≥0.3 mg/dl or ≥50% from the baseline | STEMI patients undergoing PCI | 427 | 328/99 | 73 (45–83)∗ 62 (45–78)∗ | |
|
| |||||||
| NT-proBNP | Kurtul et al. 2014 [25] | Prospective | An increase in SCr of ≥0.5 mg/dL or ≥25% above baseline within 72 hours after contrast administration | ACS patients undergoing PCI | 436 | 280/156 | 62.27 ± 13.01 |
| Liu et al. 2016 [24] | Prospective | An increase in SCr of >0.5 mg/dL above baseline within 48 to 72 hours after contrast administration | STEMI patients undergoing PCI | 283 | NA | 62.9 ± 12.3 | |
| Agarwal et al. 2018 [23] | Prospective | An increase in SCr of ≥0.5 mg/dL or ≥25% above baseline within 48 hours after index angiography | ACS patients undergoing PCI | 150 | 96/54 | 63.03 ± 9.07 | |
| Kopytsya et al. 2018 [37] | Retrospective | An absolute increase in SCr of ≥0.3 mg/dl from the baseline within 48 hours | STEMI patients undergoing SCAG | 68 | NA | NA | |
| Alan et al. 2019 [36] | Prospective | An absolute increase in SCr of ≥0.3 mg/dl at 48 h of injection or >50% above baseline within 72 hours after contrast administration | ACS patients undergoing coronary angiography | 216 | 170/46 | 63.9 ± 12.3 | |
BNP, B-type natriuretic peptide; NT-proBNP, N-terminal pro-B-type natriuretic peptide; CI-AKI, contrast-induced acute kidney injury; SCr, serum creatinine; ACS, acute coronary syndrome; STEMI, ST-elevation myocardial infarction; PCI, percutaneous coronary intervention; SCAG, selective coronary angiography; NA, not available; ∗median (5th–95th percentile ranges).
Table 2.
BNP and NT-proBNP measurements.
| Marker | Study | Assay | Optimal timing | Cutoff (pg/ml) | AUC | SEN/SPE, % | TP/FP/TN/FN |
|---|---|---|---|---|---|---|---|
| BNP | Akgul et al. 2013 [40] | Biosite triage meter | On admission | 42.4 | 0.65 | 60/61 | 35/143/223/23 |
| Moltrasio et al. 2014 [39] | Beckman coulter, triage | On admission | 184 | 0.7 | 79/74 | 67/144/410/18 | |
| Tung et al. 2015 [38] | Biosite diagnostics, triage | On admission | 676 | 0.86 | 75/89 | 27/17/136/9 | |
| Parenica et al. 2020 [35] | Enzyme immunoassay, (abbott laboratories) | 12 h after admission | 623 | 0.75 | 57.9/88.2 | 22/46/343/16 | |
|
| |||||||
| NT-proBNP | Kurtul et al. 2014 [25] | Elecsys 2010 analyzer, (roche diagnostics) | Before angiography | 2149 | 0.83 | 79.4/74.3 | 50/96/277/13 |
| Liu et al. 2016 [24] | Electrochemiluminescence immunoassay, (roche diagnostics) | On admission | 1800 | 0.76 | 69/70 | 18/80/178/8 | |
| Agarwal 2018 [23] | NA | On admission | 2320 | 0.92 | 90.9/81.5 | 20/24/104/2 | |
| Kopytsya et al. 2018 [37] | Enzyme-like immunoassay | At the 1st day of STEMI. | 1345 | 0.75 | 61.5/94.9 | 14/2/43/9 | |
| Alan et al. 2019 [36] | NA | NA | 512 | 0.79 | 81/66 | 17/66/129/4 | |
BNP, B-type natriuretic peptide; NT-proBNP, N-terminal pro-B-type natriuretic peptide; STEMI, ST-elevation myocardial infarction; AUC, area under curve; SEN, sensitivity; SPE, specificity; TP, true positives; TN, true negatives; FP, false positives; FN, false negatives and NA, not available.
3.2. Study Quality and Publication Bias
Supplementary material S1 shows the risk of bias in the nine included studies. The results revealed that one study had a high risk of bias in the flow and timing domain [37]. Because that study initially included 103 patients, only 68 patients were assessed. A Deek funnel plot is shown in Figure 2. No significant publication bias was detected (P=0.27).
Figure 2.
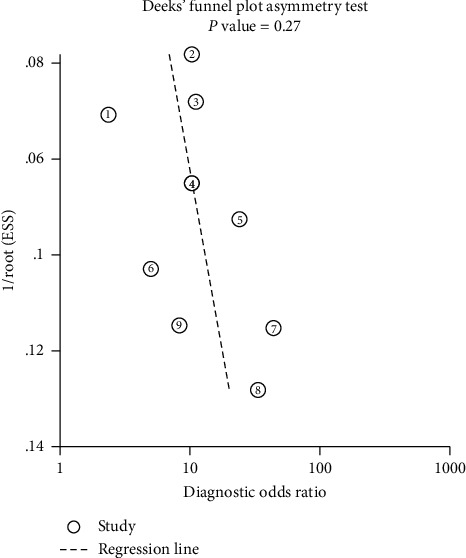
Deek funnel plot asymmetry test for publication bias, with P < 0.1 indicating publication bias. There was no significant publication bias (P=0.27).
3.3. Diagnostic Value of Brain Natriuretic Peptide for CI-AKI Prediction
The pooled SEN and SPE values were 0.73 (95% CI 0.65–0.79) and 0.79 (95% CI 0.70–0.85), respectively (Figure 3). DOR was 10 (95% CI 6–17); PLR and NLR were 3.5 (95% CI 2.4–4.9) and 0.35 (95% CI 0.27–0.44), respectively (supplementary material S2). The SROC curve is depicted in Figure 4. The AUC of brain natriuretic peptide for the diagnosis of CI-AKI was 0.81 (95% CI 0.77–0.84), indicating a high diagnostic value. Based on the Fagan nomogram (Figure 5), if the pretest probability was set to 50%, the use of BNP or NT-proBNP for the detection of CI-AKI increased the posttest probability to 78% when the brain natriuretic peptide results were positive; the posttest probability decreased to 26% when the brain natriuretic peptide results were negative. The above results suggest that BNP or NT-proBNP is a useful biomarker for the diagnosis of CI-AKI in patients with ACS undergoing coronary angiography.
Figure 3.
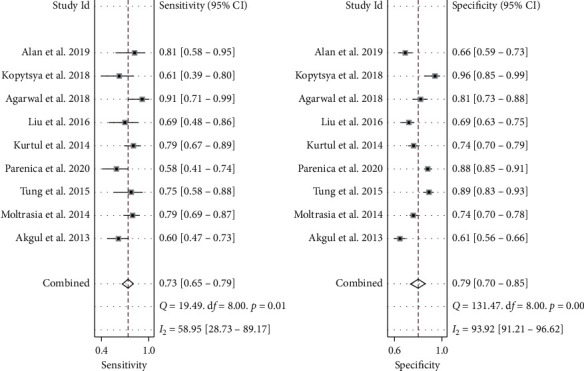
Forest plot of the sensitivity and specificity of brain natriuretic peptide for the diagnosis of contrast-induced acute kidney injury in patients with acute coronary syndrome undergoing coronary angiography. The pooled SEN and SPE values were 0.73 (95% CI 0.65–0.79) and 0.79 (95% CI 0.70–0.85), respectively. SEN, sensitivity and SPE, specificity.
Figure 4.
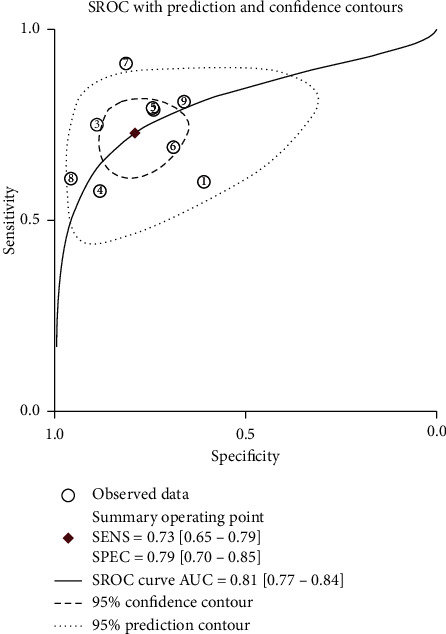
Summary receiver operating characteristic curve for the included studies. The AUC of brain natriuretic peptide for the diagnosis of contrast-induced acute kidney injury was 0.81 (95% CI 0.77–0.84), indicating a high diagnostic value. SROC, summary receiver operating characteristic; AUC, area under curve; SEN, sensitivity and SPE, specificity.
Figure 5.
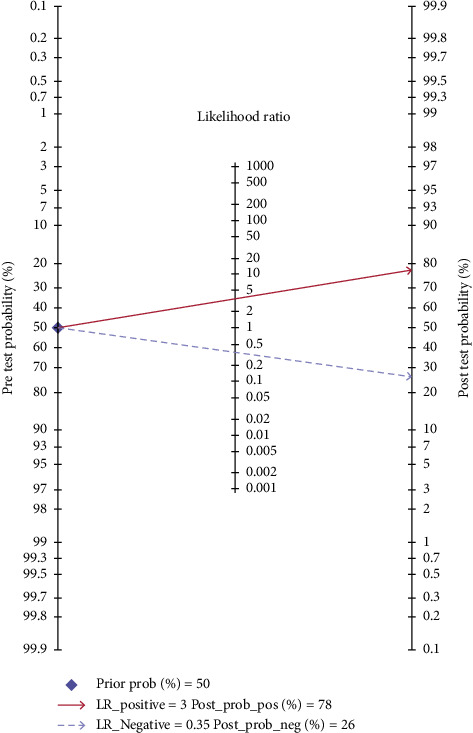
Fagan nomogram of brain natriuretic peptide for the diagnosis of contrast-induced acute kidney injury in patients with acute coronary syndrome undergoing coronary angiography. The pretest probability was set to 50%. The use of brain natriuretic peptide for the detection of contrast-induced acute kidney injury increased the posttest probability to 78% when the brain natriuretic peptide results were positive; the posttest probability decreased to 26% when the brain natriuretic peptide results were negative.
A total of 4 studies included patients diagnosed with ACS but not subdivided into UA, STEMI, or NSTEMI and were termed the “ACS” subgroup [23, 25, 36, 39]. Five others focusing on patients with STEMI used the term the “STEMI” subgroup [24, 35, 37, 38, 40]. Interestingly, brain natriuretic peptide showed a great diagnostic value in the “ACS” subgroup, with an estimated AUC of 0.85 (95% CI 0.81–0.88). Pooled SEN and SPE were 0.81 (95% CI 0.74–0.86, I2 = 0) and 0.74 (95% CI 0.69–0.78, I2 = 69.06%), respectively (Table 3).
Table 3.
Results of sensitivity analysis and subgroup analysis.
| Categories | Number of studies | Sensitivity (95% CI)/I2 | Specificity (95% CI)/I2 | AUC (95% CI) | DOR (95% CI) | PLR/NLR |
|---|---|---|---|---|---|---|
| All studies | 9 [23–25, 35–40] | 0.73 (0.65, 0.79)/58.95 | 0.79 (0.70, 0.85)/93.92 | 0.81 (0.77, 0.84) | 10 (6, 17) | 3.5/0.35 |
|
| ||||||
| Biomarker | ||||||
| BNP | 4 [35, 38–40] | 0.69 (0.59, 0.78)/72.06 | 0.80 (0.67, 0.89)/97.22 | 0.78 (0.75, 0.82) | 9 (4, 20) | 3.4/0.39 |
| NT-proBNP | 5 [23–25, 36, 37] | 0.77 (0.68, 0.83)/43.57 | 0.78 (0.66, 0.87)/84.33 | 0.82 (0.79, 0.85) | 12 (7, 21) | 3.5/0.30 |
|
| ||||||
| Patient's condition | ||||||
| STEMI | 5 [24, 35, 37, 38, 40] | 0.64 (0.57, 0.71)/9.1 | 0.83 (0.69, 0.92)/97.08 | 0.66 (0.62, 0.70) | 9 (4, 21) | 3.8/0.43 |
| ACS | 4 [23, 25, 36, 39] | 0.81 (0.74, 0.86)/0 | 0.74 (0.69, 0.78)/69.06 | 0.85 (0.81, 0.88) | 12 (7, 20) | 3.1/0.26 |
| Prospective study | 7 [23–25, 36, 38–40] | 0.76 (0.69, 0.82)/52.08 | 0.74 (0.67, 0.80)/90.41 | 0.82 (0.78, 0.85) | 9 (5, 17) | 2.9/0.32 |
| Undergoing PCI | 7 [23–25, 35, 38–40] | 0.73 (0.65, 0.80)/65.65 | 0.78 (0.70, 0.84)/94.60 | 0.82 (0.78, 0.85) | 10 (5, 17) | 3.3/0.34 |
BNP, B-type natriuretic peptide; NT-proBNP, N-terminal pro-B-type natriuretic peptide; ACS, acute coronary syndrome; STEMI, ST-elevation myocardial infarction; PCI, percutaneous coronary intervention; AUC, area under curve; PLR, positive likelihood ratio; NLR, negative likelihood ratio; DOR, diagnostic odds ratio and CI, credible interval.
3.4. Threshold Effect and Heterogeneity Analysis
The overall I2 value for the bivariate model was 90% (95% CI 81–100). The proportion of heterogeneity likely caused by the threshold effect was not significant (P=0.08). For the pooled SEN and SPE, the I2 values were 58.95% and 93.92%, respectively. Subgroup analysis based on the patient's condition (“STEMI” subgroup or “ACS” subgroup) revealed that heterogeneity in SEN may be caused by the patient's condition. The pooled I2 values for SEN in the “STEMI” subgroup and “ACS” subgroup were 9.1% and 0, respectively, though significant heterogeneity in SPE was observed. The results failed to show that different biomarkers or study types were the sources of the potential heterogeneity in SEN and SPE (Table 3).
4. Discussion
This is the first meta-analysis to evaluate the value of brain natriuretic peptide for CI-AKI in patients with ACS undergoing coronary angiography. Overall, the results suggested that BNP or NT-proBNP is a useful biomarker for the diagnosis of CI-AKI (AUC = 0.81, SEN = 0.73, and SPE = 0.79). The finding applies to both BNP (AUC = 0.78, SEN = 0.69, and SPE = 0.80) and NT-proBNP (AUC = 0.82, SEN = 0.77, and SPE = 0.78).
CI-AKI is a frequent complication in patients who receive iodinated contrast agent [41], and it is a common cause of hospital-acquired AKI and accounts for approximately 11% of hospital-acquired renal failure [42]. Previous studies have indicated that CI-AKI is associated with adverse clinical outcomes, including prolonged hospitalization, an increased risk of mortality, stent restenosis, and cardiovascular and cerebrovascular events in patients with ACS undergoing coronary angiography [43, 44]. At present, the diagnosis of CI-AKI is based on the increased serum creatinine concentration after a contrast agent injection. However, changes in serum creatinine lack sensitivity because in healthy people, nearly 50% of the glomerular filtration rate (GFR) must be lost before changes in serum creatinine can be detected [7, 45]. Moreover, there are no consistent thresholds of serum creatinine levels for the diagnosis of CI-AKI [41]. Thus, finding new biomarkers is of great significance for the early prediction of CI-AKI.
CI-AKI in ACS is a multifactorial phenomenon. First, the contrast agent is completely excreted by the kidney, and the concentration of the contrast agent increases as it passes through the renal tubules, possibly reaching a level toxic to tubular cells [41]. Toxins can have direct cytotoxic effects on endothelial cells or renal tubular epithelial cells, impair renal hemodynamics, and lead to the precipitation of metabolites or crystals, among others [7]. In addition, the impaired cardiac output and increased venous congestion lead to systemic and renal hemodynamic changes, which result in a decrease in GFR. This may be a key mechanism in the pathogenesis of AKI. Moreover, patients with ACS are characterized by progressive activation of several neurohormonal systems, involving an imbalance of endogenous vasodilating and vasoconstrictive factors and exerting profound effects on kidney perfusion and function [46]. Although the mechanism underlying the relationship between brain natriuretic peptide and CI-AKI has not been explained completely, the following reasons might be involved it to some extent. First, renal hemodynamic impairment in the context of ACS may decrease the clearance of brain natriuretic peptide [47]. Second, Vila et al. found that in healthy people with normal heart function, plasma brain natriuretic peptides were elevated in a model of systemic inflammation [48], and brain natriuretic peptide is accepted as an acute-phase reactant [49]. Therefore, brain natriuretic peptide may be an indicator of increased inflammation and immune response in ACS, which plays an important role in the occurrence and development of CI-AKI [50, 51]. Furthermore, AKI primarily presents as a sharp decrease in GFR and water and sodium retention, which accelerate the overall progression of cardiovascular disease and heart failure, followed by an increase in BNP or NT-proBNP [52]. Nonetheless, more research are needed to identify the potential mechanism between brain natriuretic peptides and CI-AKI.
BNP or NT-proBNP elevation in AKI patients was found in clinical practice, and recent data suggest that baseline BNP or NT-proBNP may help to identify ACS patients at risk for CI-AKI after coronary angiography. The results from our meta-analysis confirm the role of BNP or NT-proBNP in predicting CI-AKI. Furthermore, we built a Fagan nomogram and a likelihood ratio scattergram to evaluate the clinical application value.
There was considerable heterogeneity among the included studies. Although we conducted sensitivity and subgroup analyses, the heterogeneity was not significantly decreased. This may be caused by different cutoff values, different definitions of CI-AKI, different conditions of patients, or different study designs among the included studies. Some studies measured NT-proBNP, whereas others measured BNP, and the number of participants in the different studies varied greatly, which may also lead to heterogeneity. More high-quality studies are required to shed light on the role of brain natriuretic peptide in the diagnosis of CI-AKI for ACS patients undergoing coronary angiography.
Measuring brain natriuretic peptide is inexpensive, repeatable, and easy to achieve. For patients with ACS, monitoring brain natriuretic peptide is important and essential. Combining brain natriuretic peptide, creatinine, urine output, and other novel biomarkers, such as neutrophil gelatinase-associated lipocalin (NGAL) and cystatin C, which have been identified as potential biomarkers of CI-AKI [53, 54], can improve early diagnostic precision for CI-AKI. Moreover, early detection, intervention, and treatment contribute to a favorable prognosis in CI-AKI.
There are several limitations in our meta-analysis. First, the definition of CI-AKI was not completely consistent among the included studies. Second, in terms of sample size, brain natriuretic peptide assays, cutoff values, and study type differed across the included studies, which may have led to heterogeneity. Finally, substantial heterogeneity existed, and additional subgroup analyses could not be performed to reduce and interpret the heterogeneity because a limited number of studies were included in the meta-analysis.
5. Conclusions
This study is the first meta-analysis to evaluate the diagnostic value of brain natriuretic peptide for CI-AKI in patients with ACS undergoing coronary angiography, and the results suggest that BNP or NT-proBNP can serve as an effective predictive marker for CI-AKI. However, additional high-quality studies are required to find the optimal cutoff value and the diagnostic value of BNP or NT-proBNP in combination with other biomarkers.
Acknowledgments
This work was supported by grants from the Special Scientific Research Project of Military Health Care (17BJZ30).
List of abbreviations
- ACS:
Acute coronary syndrome
- AKI:
Acute kidney injury
- AUC:
Area under curve
- BNP:
B-type natriuretic peptide
- CI-AKI:
Contrast-induced acute kidney injury
- CI:
Credible interval
- DOR:
Diagnostic odds ratio
- FN:
False negatives
- FP:
False positives
- NT-proBNP:
N-terminal pro-B-type natriuretic peptide
- NLR:
Negative likelihood ratio
- NSTEMI:
Non-ST elevation myocardial infarction
- PLR:
Positive likelihood ratio
- PCI:
Percutaneous coronary intervention
- PRISMA:
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- QUADAS-2:
Quality Assessment of Diagnostic Accuracy Studies-2
- SEN:
Sensitivity
- STEMI:
ST-elevation myocardial infarction
- SPE:
Specificity
- SROC:
Summary receiver operating characteristic
- TP:
True positives
- TN:
True negatives
- UA:
Unstable angina.
Data Availability
The data used to support the findings of this study are included within the article and its supplementary material files.
Conflicts of Interest
The authors of this manuscript have no relevant conflicts of interest.
Authors' Contributions
XML and CL contributed equally to this work. XML and CL conceived the study, participated in the design, collected the data, performed statistical analyses, and drafted the manuscript. ZM performed statistical analyses and helped to draft the manuscript. RJS and SQ collected the data and revised the manuscript critically for important intellectual content. FHZ collected the data, performed statistical analyses, and helped to revise the manuscript critically for important intellectual content. All authors read and approved the final manuscript.
Supplementary Materials
Supplementary material S1: summary of the methodological quality of the studies according to the QUADAS-2 (Quality Assessment of Diagnostic Accuracy Studies-2) criteria. Supplementary material S2: likelihood ratio scattergram.
References
- 1.Libby P. Mechanisms of acute coronary syndromes and their implications for therapy. New England Journal of Medicine. 2013;368(21):2004–2013. doi: 10.1056/nejmra1216063. [DOI] [PubMed] [Google Scholar]
- 2.Widimsky P., Crea F., Binder R. K., Lüscher T. F. The year in cardiology 2018: acute coronary syndromes. European Heart Journal. 2019;40(3):271–282. doi: 10.1093/eurheartj/ehy904. [DOI] [PubMed] [Google Scholar]
- 3.Eisen A., Giugliano R. P., Braunwald E. Updates on acute coronary syndrome. JAMA Cardiology. 2016;1(6):718–730. doi: 10.1001/jamacardio.2016.2049. [DOI] [PubMed] [Google Scholar]
- 4.Ibanez B., James S., Agewall S., et al. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation. Kardiologia Polska. 2018;76(2):229–313. doi: 10.5603/kp.2018.0041. [DOI] [PubMed] [Google Scholar]
- 5.Hindricks D. L. Percutaneous coronary intervention in 2018. JAMA. 2018;319(20):2127–2128. doi: 10.1001/jama.2018.5281. [DOI] [PubMed] [Google Scholar]
- 6.Roffi M., Patrono C., Collet J.-P., et al. 2015 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation. European Heart Journal. 2015;37(3):267–315. doi: 10.1093/eurheartj/ehv320. [DOI] [PubMed] [Google Scholar]
- 7.Ronco C., Bellomo R., Kellum J. A. Acute kidney injury. The Lancet. 2019;394(10212):1949–1964. doi: 10.1016/s0140-6736(19)32563-2. [DOI] [PubMed] [Google Scholar]
- 8.Al-Jaghbeer M., Dealmeida D., Bilderback A., Ambrosino R., Kellum J. A. Clinical decision support for In-hospital AKI. Journal of the American Society of Nephrology. 2018;29(2):654–660. doi: 10.1681/asn.2017070765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mehran R., Aymong E. D., Nikolsky E., et al. A simple risk score for prediction of contrast-induced nephropathy after percutaneous coronary intervention. Journal of the American College of Cardiology. 2004;44(7):1393–1399. doi: 10.1016/s0735-1097(04)01445-7. [DOI] [PubMed] [Google Scholar]
- 10.Marenzi G., Lauri G., Assanelli E., et al. Contrast-induced nephropathy in patients undergoing primary angioplasty for acute myocardial infarction. Journal of the American College of Cardiology. 2004;44(9):1780–1785. doi: 10.1016/j.jacc.2004.07.043. [DOI] [PubMed] [Google Scholar]
- 11.Kanic V., Kompara G., Suran D., Ekart R., Bevc S., Hojs R. Impact of KDIGO-defined acute kidney injury on mortality after percutaneous coronary intervention for acute myocardial infarction. Cardiorenal Medicine. 2018;8(4):332–339. doi: 10.1159/000492287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Goldberg A., Hammerman H., Petcherski S., et al. Inhospital and 1-year mortality of patients who develop worsening renal function following acute ST-elevation myocardial infarction. American Heart Journal. 2005;150(2):330–337. doi: 10.1016/j.ahj.2004.09.055. [DOI] [PubMed] [Google Scholar]
- 13.Rihal C. S., Textor S. C., Grill D. E., et al. Incidence and prognostic importance of acute renal failure after percutaneous coronary intervention. Circulation. 2002;105(19):2259–2264. doi: 10.1161/01.cir.0000016043.87291.33. [DOI] [PubMed] [Google Scholar]
- 14.Garratt K., Yasuoka Y., Adachi H., et al. Impact of contrast-induced acute kidney injury on outcomes in patients with ST-segment elevation myocardial infarction undergoing primary percutaneous coronary intervention. Cardiovascular Revascularization Medicine. 2013;14(5):253–257. doi: 10.1016/j.carrev.2013.07.009. [DOI] [PubMed] [Google Scholar]
- 15.Güngör B., Karataş M. B., İpek G., et al. Association of contrast-induced nephropathy with bare metal stent restenosis in STEMI patients treated with primary PCI. Renal Failure. 2016;38(8):1167–1173. doi: 10.1080/0886022x.2016.1209024. [DOI] [PubMed] [Google Scholar]
- 16.Öztürk J. P., Christoffersen C., Perko M., et al. Increased cardiac BNP expression associated with myocardial ischemia. The FASEB Journal. 2003;17(9):1105–1107. doi: 10.1096/fj.02-0796fje. [DOI] [PubMed] [Google Scholar]
- 17.Epstein F. H., Levin E. R., Gardner D. G., Samson W. K. Natriuretic peptides. The New England Journal of Medicine. 1998;339(5):321–328. doi: 10.1056/NEJM199807303390507. [DOI] [PubMed] [Google Scholar]
- 18.Jaberg L., Toggweiler S., Puck M., et al. Prognostic value of N-terminal pro-B-type natriuretic peptide in patients with acute coronary syndromes undergoing left main percutaneous coronary intervention. Circulation Journal. 2011;75(11):2648–2653. doi: 10.1253/circj.cj-11-0095. [DOI] [PubMed] [Google Scholar]
- 19.Lemos J. A. d., Morrow D. A., Bentley J. H., et al. The prognostic value of B-type natriuretic peptide in patients with acute coronary syndromes. New England Journal of Medicine. 2001;345(14):1014–1021. doi: 10.1056/nejmoa011053. [DOI] [PubMed] [Google Scholar]
- 20.Chae M. S., Park H., Choi H. J, et al. Role of serum levels of intraoperative brain natriuretic peptide for predicting acute kidney injury in living donor liver transplantation. PLoS One. 2018;13(12) doi: 10.1371/journal.pone.0209164.e0209164 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cardinale D., Cosentino N., Moltrasio M., et al. Acute kidney injury after lung cancer surgery. Lung Cancer. 2018;123:155–159. doi: 10.1016/j.lungcan.2018.07.009. [DOI] [PubMed] [Google Scholar]
- 22.Wang K., Li H. L., Chen L. L., et al. Association of N-terminal pro-brain natriuretic peptide with contrast-induced acute kidney injury and long-term mortality in patients with heart failure and mid-range ejection fraction: an observation study. Medicine (Baltimore) 2017;96(10) doi: 10.1097/md.0000000000006259.e6259 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Agarwal S., Kareem H., Devasia T., et al. Baseline NT-proBNP level as a risk predictor of contrast induced-acute kidney injury in acute coronary syndrome patients undergoing primary angioplasty. Journal of Clinical and Diagnostic Research. 2018;12(3):OC11–OC14. doi: 10.7860/jcdr/2018/32152.11338. [DOI] [Google Scholar]
- 24.Liu Y.-h., Jiang L., Chen J.-y., Tan N., Liu Y., He P. c. Does N-terminal pro-brain natriuretic peptide add prognostic value to the Mehran risk score for contrast-induced nephropathy and long-term outcomes after primary percutaneous coronary intervention? International Urology and Nephrology. 2016;48(10):1675–1682. doi: 10.1007/s11255-016-1348-2. [DOI] [PubMed] [Google Scholar]
- 25.Kurtul A., Duran M., Yarlioglues M., et al. Association between N-terminal pro-brain natriuretic peptide levels and contrast-induced nephropathy in patients undergoing percutaneous coronary intervention for acute coronary syndrome. Clinical Cardiology. 2014;37(8):485–492. doi: 10.1002/clc.22291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Moher D., Liberati A., Tetzlaff J., Altman D. G., The PRISMA Group Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. International Journal of Surgery. 2010;8(5):336–341. doi: 10.1016/j.ijsu.2010.02.007. [DOI] [PubMed] [Google Scholar]
- 27.Whiting P. F., Rutjes A. W., Westwood M. E., et al. QUADAS-2: a revised tool for the quality assessment of diagnostic accuracy studies. Annals of Internal Medicine. 2011;155(8):529–536. doi: 10.7326/0003-4819-155-8-201110180-00009. [DOI] [PubMed] [Google Scholar]
- 28.Dwamena B. Newton, MA, USA: Department of Economics, Boston College; 2007. MIDAS: stata module for meta-analytical integration of diagnostic test accuracy studies. Statistical Software Components, S456880. [Google Scholar]
- 29.Arends L. R., Hamza T. H., van Houwelingen J. C., Heijenbrok-Kal M. H., Hunink M. G. M., Stijnen T. Bivariate random effects meta-analysis of ROC curves. Medical Decision Making. 2008;28(5):621–638. doi: 10.1177/0272989x08319957. [DOI] [PubMed] [Google Scholar]
- 30.Zhou X., Sun Z., Zhuang Y., et al. Development and validation of nomogram to predict acute kidney injury in patients with acute myocardial infarction treated invasively. Scientific Reports. 2018;8(1):p. 9769. doi: 10.1038/s41598-018-28088-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Goussot S., Mousson C., Guenancia C., et al. N-terminal fragment of pro B-type natriuretic peptide as a marker of contrast-induced nephropathy after primary percutaneous coronary intervention for ST-segment elevation myocardial infarction. The American Journal of Cardiology. 2015;116(6):865–871. doi: 10.1016/j.amjcard.2015.06.007. [DOI] [PubMed] [Google Scholar]
- 32.Yildiz E., Köse M., Yürüyen G., et al. Relationship between brain natriuretic peptide, microalbuminuria, and contrast-induced nephropathy in patients with acute coronary syndrome. Anadolu Kardiyoloji Dergisi/The Anatolian Journal of Cardiology. 2014;14(6):505–510. doi: 10.5152/akd.2014.4931. [DOI] [PubMed] [Google Scholar]
- 33.Jarai R., Dangas G., Huber K., et al. B-type natriuretic peptide and risk of contrast-induced acute kidney injury in acute ST-segment-elevation myocardial infarction. Circulation: Cardiovascular Interventions. 2012;5(6):813–820. doi: 10.1161/circinterventions.112.972356. [DOI] [PubMed] [Google Scholar]
- 34.Genereux A., Masnik K., Mihevc M. Predictors of acute kidney injury (AKI) in high-risk ST-elevation myocardial infarction (STEMI) patients: a single-center retrospective observational study. Bosnian Journal of Basic Medical Sciences. 2019;19(1):101–108. doi: 10.17305/bjbms.2018.3797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Parenica J., Kala P., Mebazaa A., et al. Activation of the nitric oxide pathway and acute myocardial infarction complicated by acute kidney injury. Cardiorenal Medicine. 2020;10(2):85–96. doi: 10.1159/000503718. [DOI] [PubMed] [Google Scholar]
- 36.Alan G., Guenancia C., Arnould L., et al. Retinal vascular density as A novel biomarker of acute renal injury after acute coronary syndrome. Scientific Reports. 2019;9(1):p. 8060. doi: 10.1038/s41598-019-44647-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kopytsya M., Hilova Y., Vyshnevska I., Petyunina O. Biomarker ST2 as a new predictor of acute kidney injury in patients with acute ST segment elevation myocardial infarction. Georgian Medical News. 2018;282:61–65. [PubMed] [Google Scholar]
- 38.Tung Y. C., Chang C. H., Chen Y. C., Chu P. H. Combined biomarker analysis for risk of acute kidney injury in patients with ST-segment elevation myocardial infarction. PLoS One. 2015;10(4) doi: 10.1371/journal.pone.0125282.e0125282 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Moltrasio M., Cabiati A., Milazzo V., et al. B-type natriuretic peptide and risk of acute kidney injury in patients hospitalized with acute coronary syndromes∗. Critical Care Medicine. 2014;42(3):619–624. doi: 10.1097/ccm.0000000000000025. [DOI] [PubMed] [Google Scholar]
- 40.Akgul O., Uyarel H., Pusuroglu H., et al. High BNP level as risk factor for acute kidney injury and predictor of all-cause mortality in STEMI patients. Herz. 2013;39(4):507–514. doi: 10.1007/s00059-013-3853-8. [DOI] [PubMed] [Google Scholar]
- 41.Akturk M., Seeliger E., Patzak A., Persson P. B. Understanding and preventing contrast-induced acute kidney injury. Nature Reviews Nephrology. 2017;13(3):169–180. doi: 10.1038/nrneph.2016.196. [DOI] [PubMed] [Google Scholar]
- 42.McCullough P. A., Adam A., Becker C. R., et al. Epidemiology and prognostic implications of contrast-induced nephropathy. The American Journal of Cardiology. 2006;98(6):5–13. doi: 10.1016/j.amjcard.2006.01.019. [DOI] [PubMed] [Google Scholar]
- 43.Yang Y., George K. C., Luo R., et al. Contrast-induced acute kidney injury and adverse clinical outcomes risk in acute coronary syndrome patients undergoing percutaneous coronary intervention: a meta-analysis. BMC Nephrology. 2018;19(1):p. 374. doi: 10.1186/s12882-018-1161-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.James M. T., Samuel S. M., Manning M. A., et al. Contrast-induced acute kidney injury and risk of adverse clinical outcomes after coronary angiography. Circulation: Cardiovascular Interventions. 2013;6(1):37–43. doi: 10.1161/circinterventions.112.974493. [DOI] [PubMed] [Google Scholar]
- 45.Slocum J. L., Heung M., Pennathur S. Marking renal injury: can we move beyond serum creatinine? Translational Research. 2012;159(4):277–289. doi: 10.1016/j.trsl.2012.01.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Marenzi G., Cosentino N., Bartorelli A. L. Acute kidney injury in patients with acute coronary syndromes. Heart. 2015;101(22):1778–1785. doi: 10.1136/heartjnl-2015-307773. [DOI] [PubMed] [Google Scholar]
- 47.Vickery S., Price C. P., John R. I., et al. B-type natriuretic peptide (BNP) and amino-terminal proBNP in patients with CKD: relationship to renal function and left ventricular hypertrophy. American Journal of Kidney Diseases. 2005;46(4):610–620. doi: 10.1053/j.ajkd.2005.06.017. [DOI] [PubMed] [Google Scholar]
- 48.Vila G., Resl M., Stelzeneder D., et al. Plasma NT-proBNP increases in response to LPS administration in healthy men. Journal of Applied Physiology. 2008;105(6):1741–1745. doi: 10.1152/japplphysiol.90442.2008. [DOI] [PubMed] [Google Scholar]
- 49.Madak N., Nazli Y., Mergen H., et al. Acute phase reactants in patients with coronary slow flow phenomenon. Anadolu Kardiyoloji Dergisi/The Anatolian Journal of Cardiology. 2010;10(5):416–420. doi: 10.5152/akd.2010.139. [DOI] [PubMed] [Google Scholar]
- 50.Ortega-Hernández J., Springall R., Sánchez-Muñoz F., Arana-Martinez J. C., González-Pacheco H., Bojalil R. Acute coronary syndrome and acute kidney injury: role of inflammation in worsening renal function. BMC Cardiovascular Disorders. 2017;17(1):p. 202. doi: 10.1186/s12872-017-0640-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Kurtul A., Murat S. N., Yarlioglues M., et al. Procalcitonin as an early predictor of contrast-induced acute kidney injury in patients with acute coronary syndromes who underwent percutaneous coronary intervention. Angiology. 2015;66(10):957–963. doi: 10.1177/0003319715572218. [DOI] [PubMed] [Google Scholar]
- 52.Schefold J. C., Filippatos G., Hasenfuss G., Anker S. D., von Haehling S. Heart failure and kidney dysfunction: epidemiology, mechanisms and management. Nature Reviews Nephrology. 2016;12(10):610–623. doi: 10.1038/nrneph.2016.113. [DOI] [PubMed] [Google Scholar]
- 53.Kafkas N., Liakos C., Zoubouloglou F., Dagadaki O., Dragasis S., Makris K. Neutrophil gelatinase-associated lipocalin as an early marker of contrast-induced nephropathy after elective invasive cardiac procedures. Clinical Cardiology. 2016;39(8):464–470. doi: 10.1002/clc.22551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Briguori C., Visconti G., Rivera N. V., et al. Cystatin C and contrast-induced acute kidney injury. Circulation. 2010;121(19):2117–2122. doi: 10.1161/circulationaha.109.919639. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary material S1: summary of the methodological quality of the studies according to the QUADAS-2 (Quality Assessment of Diagnostic Accuracy Studies-2) criteria. Supplementary material S2: likelihood ratio scattergram.
Data Availability Statement
The data used to support the findings of this study are included within the article and its supplementary material files.


