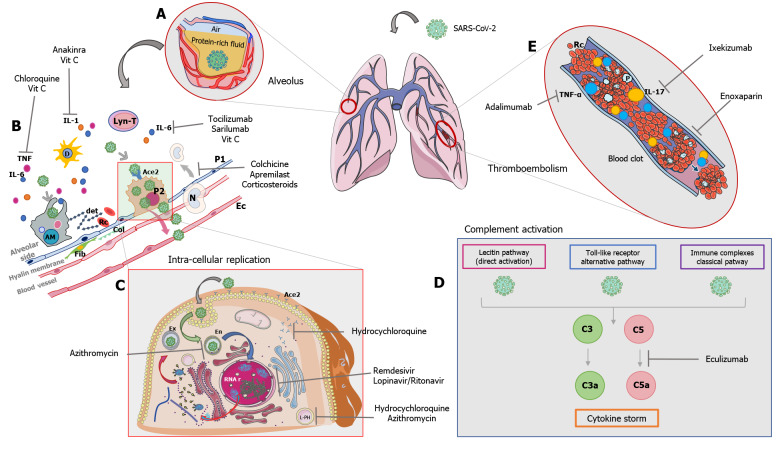
Figure 1.
Severe acute respiratory syndrome coronavirus 2 infection, consequences and rationale of treatment. A: The virus in the alveolus induces the production of a protein rich fluid interfering with ventilation gas exchanges; B: Description of what happens in the alveolus after the infection and drugs involved in this phase. The virus binds the angiotensin-converting enzyme 2 (ACE2) receptor and replicates in the Type 2 pneumocyte (P2), leading to apoptosis (accumulation of cellular dendrites), activation of alveolar macrophages, dendritic cells, lymphocytes T, and neutrophils. There is an augmentation of cytokines levels, especially interleukin 6 (IL-6), IL-1, and tumor necrosis factor (TNF). The inflammatory process leads to damage of the alveolar barrier and to the formation of the hyaline membrane between the alveolar side and the blood vessels. In this phase, chloroquine reduces the levels of TNF; vitamin C reduces the levels of TNF, IL-1, and IL-6; anakinra inhibits IL-1 binding to its receptor; tocilizumab and sarilumab inhibit IL-6 binding to its receptor; and colchicine, apremilast, and corticosteroids reduce the migration of lymphoid cells into the alveolus; C: Synthesis of the intra-cellular replication of the virus. Hydroxychloroquine reduces the exposition of ACE2 receptors on the surface of P2, and as azithromycin reduces the pH in lysosomes and endosomes. Remdesivir and lopinavir/ritonavir interfere with viral replication; D: The virus is capable of activating the complement system that can be inhibited by eculizumab. E: Enoxaparin may be effective against the typical thromboembolism induced by the virus. Furthermore, in the plasmatic torrent, the high levels of TNF-alpha and IL-17 can be reduced by selective binders such as adalimumab and ixekizumab, respectively. Original picture by Di Franco S and Alfieri A (2020).