Abstract
Introduction
We aimed to investigate postoperative stability after orthognathic surgery in patients with skeletal class III malocclusion with severe open bite by comparison between bilateral sagittal splitting osteotomy (BSSRO) and BSSRO with Le Fort 1 osteotomy.
Materials and methods
Seventeen patients with skeletal class III malocclusion with severe open bite who were needed more than 6 degree counterclockwise rotation of distal segment by only BSSRO in preoperative cephalometric prediction. The subjects were divided into group A, where 9 patients were treated by BSSRO, and group B, where 8 patients were treated by BSSRO with Le Fort 1 osteotomy. Patient’s characteristics of age, gender, preoperative over jet (OJ) and over bite (OB) were not found to be significantly different between the two groups. Counterclockwise rotation of distal segment in preoperative cephalometric prediction by only BSSRO was not found to be significantly different between group A of 7.6 (6–10.6) degree and group B of 9 (6–13) degree. The amount of rotation was reduced to 5.4 (3–10) degree by bimaxillary surgery using BSSRO and Le Fort 1 osteotomy in group B. OJ and OB were measured as occlusal stability factor. Distance between ANS-to-PNS plane and the edge of upper incisor (NF–U1Ed), and distance between Menton and edge of lower incisor (Me–L1Ed) were measured as skeletal stability factor using cephalometric analysis. These lengths were measured at pre-surgery (T0), 2 weeks after surgery (T1) and 1 year after surgery (T2), and these differences between the two groups were statistically analyzed.
Results
OJ and OB kept a good relation at any experimental periods. The change of Me–L1Ed was significantly larger in group A (1.21 mm at T0–T1, 1.02 mm at T0–T2) than in group B (0.14 mm at T0–T1, 0.16 mm at T0–T2). The change of NF–U1Ed was not significantly different between group A (1.07 mm at T0–T1, 0.57 mm at T0–T2) and group B (0.51 mm at T0–T1, − 0.05 mm at T0–T2).
Conclusion
In case with more than 6 degree counterclockwise rotation of distal segment, skeletal stability was better after bimaxillary surgery than only BSSRO; however, OJ and OB kept a good relation.
Keywords: Skeletal stability, Sagittal splitting ramus osteotomy, Le Fort 1 osteotomy, Skeletal class III with severe open bite
Introduction
Stability of skeletal class III with anterior open bite correction is a challenging topic in surgical orthodontics because postoperative relapse is occurred at a high probability if the rotation of distal segment is counterclockwise . Several treatment protocols have been proposed to correct anterior open bite malocclusions [1–3] that can distinctly influence long-term stability [4, 5]. Conventional orthodontic treatment is marked by significant open bite relapse [6, 7]. Surgical orthodontic treatment has long-term stability and has been established as a standard method [8], while its treatment by orthodontics alone leads to significant postoperative relapse [9]. If the amount of distal segment counterclockwise rotation is large at preoperative cephalometric prediction, not only mandibular osteotomy but also maxillary osteotomy at the same time is performed to reduce counterclockwise rotation of distal segment. In general, bimaxillary surgery was performed by Le Fort I osteotomy and bilateral sagittal splitting ramus osteotomy (BSSRO) in almost all the cases. However, there are few reports about skeletal stability using comparison between bimaxillary osteotomy and mandibular osteotomy in skeletal class III malocclusion with severe anterior open bite. In these reasons, we investigated skeletal stability after orthognathic surgery of skeletal class III malocclusion with severe anterior open bite between bimaxillary osteotomy and mandibular osteotomy.
Patients and Methods
Seventeen patients with skeletal class III with anterior open bite who had orthognathic surgery at the Hokkaido University Hospital, Sapporo, Japan, were included in this study. In all cases, the amount of distal segment counterclockwise rotation is over 6 degree at preoperative cephalometric prediction. Lip or cleft palate patient was not included. The subjects were divided into two groups. Nine patients performed single mandibular surgery by BSSRO (group A) and 8 patients performed bimaxillary surgery by Le Fort 1 osteotomy and BSSRO (group B). In both groups, age, gender, preoperative over jet (OJ) and over bite (OB) were not found to be significantly different. Preoperative amount of mandibular counterclockwise rotation of distal segment at cephalometric prediction was 7.6 (5.4–10.6) degree in group A and 9.0 (6.0–10.6) degree in group B. The final amount of mandibular counterclockwise rotation was reduced to 5.3 (3.0–9.0) by bimaxillary surgery (Table 1). Titanium mini plates were used for osteosynthesis in both groups. Maxillomandibular fixation was not performed after surgery. We measured OJ, OB, distance between ANS-to-PNS plane and the edge of upper incisor (NF–U1Ed) and distance between Me and edge of lower incisor (Me–L1Ed) using cephalometric analysis (Fig. 1). These were measured at before surgery (T0), 2 weeks after surgery (T1) and 1 year after surgery (T2). These differences between the both groups were investigated by statistical analysis for comparing skeletal stability after surgery. Values of P < 0.05 were considered to be significant.
Table 1.
Patient’s characteristics in skeletal class III malocclusion with severe open bite
| A | B | P value | |
|---|---|---|---|
| Case: (number) | 9 | 8 | |
| Gender: (male/female) | 3/6 | 3/5 | |
| Age: mean (range) | 23 (19–32) | 24 (19–32) | 0.6524 |
| Over jet | − 3.2 (− 6.0 to − 1.0) | − 2.7 (− 4.8 to 0) | 0.5563 |
| Over bite | − 2.5 (− 3.4 to − 1.5) | − 2.9 (− 5.7 to − 0.6) | 0.4954 |
| Counterclockwise rotation (°) | 7.6 (5.4–10.6) | 9.0 (6.0–13.0) | 0.3042 |
| Cephalometric prediction by BSSRO after surgery | 7.6 (5.4–10.6) | 5.3 (3.0–9.0) | 0.0351* |
Mean (range)
*P < 0.05 Mann–Whitney test
A: Bilateral sagittal splitting ramus osteotomy (BSSRO)
B: Le Fort 1 osteotomy + BSSRO
Fig. 1.
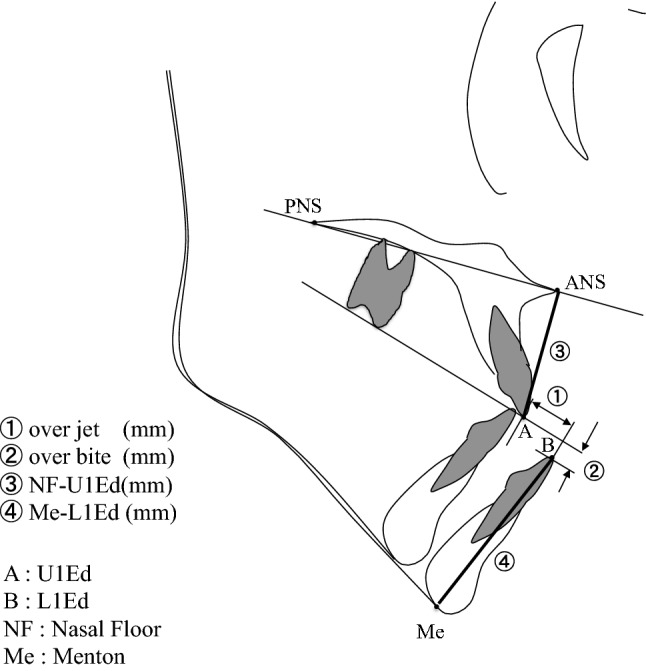
Measurement points and distance on lateral cephalograms
This study complied with the principles stated in the Declaration of Helsinki Ethical Principles for Medical Research Involving Human Subjects, adopted by the 18th World Medical Assembly, Helsinki, Finland, June 1964, and as amended most recently by the 64th World Medical Assembly, Fortaleza, Brazil, October 2013. The work has been approved by Hokkaido University Research Ethical Committee (Ref. No. 010-0285, approved on 22 February 2011).
All patients are informed about research purpose and agree to use their clinical data for this study and gave written informed consent prior to any study-related activities.
Results
OJ was − 2.7 (− 4.8 to 0.0) mm at T0, 2.4 (1.0–3.0) mm at T1, 2.7 (0.5–4.0) mm at T2 in group A and − 3.2 (− 6.0 to − 1.0) mm at T0, 2.7 (0.7–3.8) mm at T1, 2.8 (1.8–4.0) mm at T2 in group B (Fig. 2, Table 2). OB was − 2.9 (− 5.7 to − 0.6) mm at T0, 1.4 (1.0–2.0) mm at T2, 1.6 (0–2.5) mm at T2 in group A and − 2.5 (− 3.4 to − 1.5) mm at T0, 2.7 (1.5–3.7) mm at T1, 2.2 (1.0–3.3) mm at T2 in group B (Fig. 3, Table 2). OJ and OB kept a good relation during experimental periods.
Fig. 2.
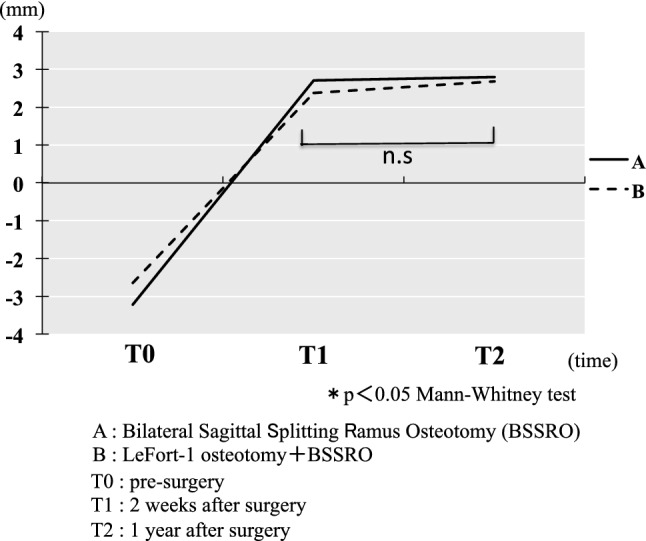
Changes of over jet
Table 2.
Comparison of the variable changes between BSSRO and LF-1 + BSSRO
| Variable | A | B | P value | ||
|---|---|---|---|---|---|
| Mean | SD | Mean | SD | ||
| Over jet | |||||
| T0–T1 | 5.93 | 1.75 | 5.03 | 1.91 | 0.3213 |
| T1–T2 | 0.09 | 0.99 | 0.31 | 0.88 | 0.7231 |
| T0–T2 | 6.02 | 1.94 | 5.34 | 1.80 | 0.6224 |
| Over bite | |||||
| T0–T1 | 5.16 | 0.63 | 4.28 | 1.65 | 0.2076 |
| T1–T2 | − 0.48 | 0.64 | 0.25 | 0.80 | 0.0621 |
| T0–T2 | 4.68 | 1.09 | 4.53 | 1.90 | 0.6216 |
| NF–U1Ed | |||||
| T0–T1 | 1.07 | 1.10 | 0.51 | 0.18 | 0.1171 |
| T1–T2 | − 0.50 | 0.86 | − 0.56 | 0.88 | 0.8697 |
| T0–T2 | 0.57 | 0.93 | − 0.05 | 0.77 | 0.2454 |
| Me–L1Ed | |||||
| T0–T1 | 1.21 | 0.63 | 0.14 | 0.69 | 0.0160 |
| T1–T2 | − 0.19 | 0.53 | 0.03 | 0.52 | 0.7387 |
| T0–T2 | 1.02 | 0.85 | 0.16 | 0.80 | 0.0191 |
*P < 0.05 Mann–Whitney test
T0: pre-surgery
T1: 2 weeks after surgery
T2: 1 year after surgery
A: Bilateral sagittal splitting ramus osteotomy (BSSRO)
B: Le Fort 1 osteotomy (LF-1) BSSRO
Fig. 3.

Changes of over bite
The change of NF–U1Ed was 0.5 (0.3–0.9) mm in group A and 1.1 (− 0.9 to 2.5) mm in group B between T0 and T1, − 0.6 (− 2.4 to 0.1) mm in group A and − 0.5 (− 1.9 to 1.1) mm in group B between T1 and T2 and − 0.1 (− 1.5 to 1.0) mm in group A and 0.6 (− 0.7 to 2.2) mm in group B between T0 and T2. The change of Me–L1Ed was 0.1 (− 0.7 to 0.9) mm in group A and 1.2 (0.5–2.1) mm in group B between T0 and T1, 0 (− 1.1 to 0.8) mm in group A and − 0.2 (− 1.3 to 0.5) mm in group B between T1 and T2 and 0.2 (− 1.1 to 0.8) mm in group A and 1.0 (− 0.8 to 2.0) mm in group B between T0 and T2. The changes in group B were larger than in group A between T1 and T2 and between T1 and T3 (Table 2).
Discussion
In skeletal class III with anterior open bite cases, bimaxillary or one-jaw surgery (Le Fort I osteotomy or mandibular surgery alone) is performed according to the amount of movement and mandibular counterclockwise rotation. Bimaxillary surgery achieves the better esthetic and functional results rather than one-jaw surgery [10–13], while mandibular osteotomy alone can also be used to treat skeletal open bite in which the maxillary position is esthetically acceptable preoperatively [14]. Procedures such as bilateral sagittal splitting osteotomies and counterclockwise rotation of the mandible with rigid internal fixation were found to be at least as stable as maxillary impaction and bimaxillary surgery [15]. Despite improvement in surgical techniques and rigid internal plate fixation, postoperative stability appeared better with bimaxillary surgery with maxillary posterior impaction when compared to isolated mandibular surgery [16–18]. However, counterclockwise rotation of the distal segment should inevitably be performed during mandibular prognathism with anterior open bite correction when mandibular setback with posterior maxillary impaction results in a severely retruded chin or mandible.
Generally, it has been reported that postoperative maxillary position is well maintained after maxillary advancement for skeletal class III patients. Following bimaxillary surgery with maxillary downward movement and advancement of less than 6 mm, horizontal stability was well maintained and improvement of vertical stability was also observed [19]. In mandibular osteotomies, most short-term relapse appears to be occurred during the first 3–6 weeks [14]. The result of our study showed that during the first 2 weeks, the distance between Menton and edge of lower incisor was significantly longer by one-jaw surgery rather than bimaxillary surgery; however, there were no significant differences between ANS and edge of upper incisor; over jet and over bite kept a good relationship. This result indicated that mandibular counterclockwise rotation was occurred in one-jaw surgery with over 6 degree mandibular counterclockwise rotation. The postoperative long-term stability of the mandible is influenced by many factors. One of the most important factors is the amount of mandibular setback and the clockwise rotation of proximal segment leading to elongation of the pterygomasseteric sling. The stretched muscle returns to its original length after surgery, and this force results in postoperative counterclockwise rotation of the mandible, which causes forward and upward mandibular movement, and the more the mandible moves backward during surgery, the greater the posterior pushes on the gonial angle [20]. Mobarak et al. also reported a weak but significant relationship between horizontal relapse at the pogonion and surgical clockwise ramus inclination change in their study of 80 consecutive single-jaw mandibular setbacks [21]. It has been demonstrated that greater over bite stability is achieved with maxillary surgical repositioning only or with bimaxillary surgery, whereas mandibular surgery only produces less stable results [22, 23]. Maxillary incisor proclination during the long-term posttreatment period showed a significant and strong inverse correlation with open bite relapse. This postsurgical labial tipping of the maxillary incisors has been frequently reported as a significant open bite relapse factor [23, 24]. Incisor proclination can be associated with inadequate tongue pressure or thrust because the tongue did not adapt [25]. Furthermore, pre-surgical dental decompensation of excessive labial incisor tipping could have relapsed to some extent [26]. The increase in maxillary incisor dentoalveolar height was correlated to over bite increase as a result of natural dental compensation. Long-term vertical dental changes tend to counteract skeletal changes, decreasing the open bite relapse, but it is not always present or sufficient to prevent a negative over bite [22]. In conclusion, bimaxillary surgery is better than only BSSRO for skeletal stability by reducing mandibular counterclockwise rotation after surgery in class III patients with severe anterior open bite.
Author contributions
KO and NI designed most of the experiments and wrote the main manuscript text and prepared all figures and tables. KM and HY are the primary persons responsible for carrying out all experimental procedures. TM analyzed the data. SK and KT are the persons who made the final approval of the article.
Funding
None to declare.
Compliance with ethical standards
Conflict of interest
The authors declare that they have no conflicts of interest.
Ethical approval
Approval was given by Hokkaido University Hospital Ethics Committee (Ref. No 010-0285).
Patient consent
All patients are informed about research purpose and agree to use their clinical data for this study.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Epker BN, Fish L. Surgical-orthodontic correction of open-bite deformity. Am J Orthod. 1977;71:278–299. doi: 10.1016/0002-9416(77)90188-9. [DOI] [PubMed] [Google Scholar]
- 2.Beane RA., Jr Nonsurgical management of the anterior open bite: a review of the options. Semin Orthod. 1999;5:275–283. doi: 10.1016/S1073-8746(99)80021-8. [DOI] [PubMed] [Google Scholar]
- 3.Janson G, Crepaldi MV, de Freitas KM, de Freitas MR, Janson W. Evaluation of anterior open-bite treatment with occlusal adjustment. Am J Orthod Dentofacial Orthop. 2008;134:10–11. doi: 10.1016/j.ajodo.2008.06.005. [DOI] [PubMed] [Google Scholar]
- 4.Janson G, Valarelli FP, Henriques JF, de Freitas MR, Cançado RH. Stability of anterior open bite nonextraction treatment in the permanent dentition. Am J Orthod Dentofacial Orthop. 2003;124:265–276. doi: 10.1016/S0889-5406(03)00449-9. [DOI] [PubMed] [Google Scholar]
- 5.de Freitas MR, Beltrão RT, Janson G, Henriques JF, Cançado RH. Long-term stability of anterior open bite extraction treatment in the permanent dentition. Am J Orthod Dentofacial Orthop. 2004;125:78–87. doi: 10.1016/j.ajodo.2003.01.006. [DOI] [PubMed] [Google Scholar]
- 6.Lopez-Gavito G, Wallen TR, Little RM, Joondeph DR. Anterior open-bite malocclusion: a longitudinal 10-year postretention evaluation of orthodontically treated patients. Am J Orthod. 1985;87:175–186. doi: 10.1016/0002-9416(85)90038-7. [DOI] [PubMed] [Google Scholar]
- 7.Remmers D, Van’t Hullenaar RW, Bronkhorst EM, Berge SJ, Katsaros C. Treatment results and long-term stability of anterior open bite malocclusion. Orthod Craniofac Res. 2008;11:32–42. doi: 10.1111/j.1601-6343.2008.00411.x. [DOI] [PubMed] [Google Scholar]
- 8.Iannetti G, Fedda MT, Marianetti TM, Terenzi V, Cassoni A. Long-term skeletal stability after surgical correction in class III open-bite patients: a retrospective study on 40 patients treated with mono- or bimaxillary surgery. J Craniofac Surg. 2007;18:350–354. doi: 10.1097/01.scs.0000248658.38158.d2. [DOI] [PubMed] [Google Scholar]
- 9.Maia FA, Janson G, Barros SE, Maia NG, Chiqueto K, Nakamura AY. Long-term stability of surgical-orthodontic open-bite correction. Am J Orthod Dentofac Orthop. 2010;138(3):254.e1–254.e10. doi: 10.1016/j.ajodo.2010.03.021. [DOI] [PubMed] [Google Scholar]
- 10.Espeland L, Dowling PA, Mobarak KA. Three-year stability of open-bite correction by 1-piece maxillary osteotomy. Am J Orthod Dentofac Orthop. 2008;134:60–66. doi: 10.1016/j.ajodo.2006.05.049. [DOI] [PubMed] [Google Scholar]
- 11.Politi M, Costa F, Cian R, Polini F, Robiony M. Stability of skeletal class III malocclusion after combined maxillary and mandibular procedures: rigid internal fixation versus wire osteosynthesis of the mandible. J Oral Maxillofac Surg. 2004;62:169–181. doi: 10.1016/j.joms.2003.04.010. [DOI] [PubMed] [Google Scholar]
- 12.Abeltins A, Jakobsone G, Urtane I, Bigestans A. The stability of bilateral sagittal ramus osteotomy and vertical ramus osteotomy after bimaxillary correction of class III malocclusion. J Craniomaxillofac Surg. 2011;39:583–587. doi: 10.1016/j.jcms.2011.01.002. [DOI] [PubMed] [Google Scholar]
- 13.De Lir ALS, De Moura WL, Ruellas ACO, Souza MMG, Nojima LI. Long-term skeletal and profile stability after surgical-orthodontic treatment of class II and class III malocclusion. J Craniomaxillofac Surg. 2013;41:296–302. doi: 10.1016/j.jcms.2012.10.001. [DOI] [PubMed] [Google Scholar]
- 14.Stansbury CD, Evans CA, Miloro M, BeGole EA, Morris DE. Stability of open bite correction with sagittal split osteotomy and closing rotation of the mandible. J Oral Maxillofac Surg. 2010;68:149–159. doi: 10.1016/j.joms.2009.07.105. [DOI] [PubMed] [Google Scholar]
- 15.Oliveira JP, Bloomquist DS. The stability of the use of bilateral sagittal split osteotomy in the closure of anterior open bite. Int J Adult Orthod Orthognath Surg. 1997;12:101. [PubMed] [Google Scholar]
- 16.Costa F, Robiony M, Politi M. Stability of sagittal split ramus osteotomy used to correct class III malocclusion: review of the literature. Int J Adult Orthod Orthognath Surg. 2001;16:121–129. [PubMed] [Google Scholar]
- 17.Gallego-Romero D, Llamas-Carrera JM, Torres-Lagares D, Paredes V, Espinar E, Guevara E, et al. Long-term stability of surgical-orthodontic correction of class III malocclusions with long-face syndrome. Med Oral Patol Oral Cir Bucal. 2012;17:E435–E441. doi: 10.4317/medoral.17647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Proffit WR, Phillips C, Turvey TA. Stability after mandibular setback: mandibular- only versus 2-jaw surgery. J Oral Maxillofac Surg. 2012;70:e408–e414. doi: 10.1016/j.joms.2012.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mucedero M, Coviello A, Baccetti T, Franchi L, Cozza P. Stability factors after double- jaw surgery in class III malocclusion. A systematic review. Angle Orthod. 2008;78:1141–1152. doi: 10.2319/101807-498.1. [DOI] [PubMed] [Google Scholar]
- 20.Franco JE, Van Sickels JE, Thrash WJ. Factors contributing to relapse in rigidly fixed mandibular setbacks. J Oral Maxillofac Surg. 1989;47:451. doi: 10.1016/0278-2391(89)90276-0. [DOI] [PubMed] [Google Scholar]
- 21.Mobarak KA, Krogstad O, Esperland L, Lyberg T. Long-term stability of mandibular setback surgery: a follow-up of 80 bilateral sagittal split osteotomy patients. Int J Adult Orthod Orthognath Surg. 2000;15:83–95. [PubMed] [Google Scholar]
- 22.Ding Y, Xu TM, Lohrmann B, Gellrich NC, Schwestka-Polly R. Stability following combined orthodontic-surgical treatment for skeletal anterior open bite—a cephalometric 15-year follow-up study. J Orofac Orthop. 2007;68:245–256. doi: 10.1007/s00056-007-0632-2. [DOI] [PubMed] [Google Scholar]
- 23.Fischer K, von Konow L, Brattstrom V. Open bite: stability after bimaxillary surgery—2-year treatment outcomes in 58 patients. Eur J Orthod. 2000;22:711–718. doi: 10.1093/ejo/22.6.711. [DOI] [PubMed] [Google Scholar]
- 24.Hoppenreijs TJ, Freihofer HP, Stoelinga PJ, Tuinzing DB, van’t Hof MA, van der Linden FP, et al. Skeletal and dento-alveolar stability of Le Fort I intrusion osteotomies and bimaxillary osteotomies in anterior open bite deformities. A retrospective three-centre study. Int J Oral Maxillofac Surg. 1997;26:161–175. doi: 10.1016/S0901-5027(97)80813-2. [DOI] [PubMed] [Google Scholar]
- 25.Shapiro PA. Stability of open bite treatment. Am J Orthod Dentofac Orthop. 2002;121:566–568. doi: 10.1067/mod.2002.124175. [DOI] [PubMed] [Google Scholar]
- 26.Emshoff R, Scheiderbauer A, Gerhard S, Norer B. Stability after rigid fixation of simultaneous maxillary impaction and mandibular advancement osteotomies. Int J Oral Maxillofac Surg. 2003;32:137–142. doi: 10.1054/ijom.2002.0315. [DOI] [PubMed] [Google Scholar]


