Abstract
Many cases of human exposures to high-dose radiation have been documented, including individuals exposed during the detonation of atomic bombs in Hiroshima and Nagasaki, nuclear power plant disasters (e.g., Chernobyl), as well as industrial and medical accidents. For many of these exposures, injuries to the skin have been present and have played a significant role in the progression of the injuries and survivability from the radiation exposure. There are also instances of radiation-induced skin complications in routine clinical radiotherapy and radiation diagnostic imaging procedures. In response to the threat of a radiological or nuclear mass casualty incident, the U.S. Department of Health and Human Services tasked the National Institute of Allergy and Infectious Diseases (NIAID) with identifying and funding early- to mid-stage medical countermeasure (MCM) development to treat radiation-induced injuries, including those to the skin. To appropriately assess the severity of radiation-induced skin injuries and determine efficacy of different approaches to mitigate/treat them, it is necessary to develop animal models that appropriately simulate what is seen in humans who have been exposed. In addition, it is important to understand the techniques that are used in other clinical indications (e.g., thermal burns, diabetic ulcers, etc.) to accurately assess the extent of skin injury and progression of healing. For these reasons, the NIAID partnered with two other U.S. Government funding and regulatory agencies, the Biomedical Advanced Research and Development Authority (BARDA) and the Food and Drug Administration (FDA), to identify state-of-the-art methods in assessment of skin injuries, explore animal models to better understand radiation-induced cutaneous damage and investigate treatment approaches. A two-day workshop was convened in May 2019 highlighting talks from 28 subject matter experts across five scientific sessions. This report provides an overview of information that was presented and the subsequent guided discussions.
INTRODUCTION
In the wake of the terrorist attacks on September 11, 2001, the U.S. Government re-focused attention on the potential threat from a radiological or nuclear incident on U.S. soil. In response to growing concerns about the ability of the Government to mount a medical response to such a disaster, several agencies were tasked with the mission to support research to develop medical countermeasures (MCMs) to diagnose (biodosimetry) and treat radiation injuries in the wake of a mass casualty, public health emergency. One of these organizations was the National Institute of Allergy and Infectious Diseases (NIAID), National Institutes of Health (NIH), within the Department of Health and Human Services (HHS). Since 2004, the NIAID has supported countermeasure development across the entire spectrum of radiation research: development of animal models, basic research to identify and target biological pathways involved in the radiation damage response, and advanced development of approaches needed to obtain approval2 for marketing by the U.S. Food and Drug Administration (FDA). The Biomedical Advanced Research and Development Authority (BARDA), also a part of HHS, supports late-stage activities needed for product approval and is responsible for procurement of products to be placed in the U.S. Strategic National Stockpile (SNS). In parallel, the FDA provides guidance to drug developers seeking approval of products for a radiation countermeasures indication, for which efficacy studies in humans cannot be feasibly or ethically obtained. Referred to as the “Animal Rule” (1), the FDA created a pathway that has been used to obtain approval for three MCMs to treat hematopoietic complications resulting from radiation exposure: filgrastim (Neupogen®, FDA approved March 2015);3 pegfilgrastim (Neulasta®, FDA approved November 2015);4 and sargramostim (Leukine®, FDA approved March 2018).5
Although there are now products approved to address radiation-induced hematopoietic complications, there are still other injuries for which no treatment options specific to radiation exposure are approved. These injuries include damage to the gastrointestinal (GI) tract, lungs, kidneys, cardiovascular systems and skin. There are products in development for all of these radiation sub-syndromes; however, the skin represents the organ system that historically has been most affected in human cases of radiation exposure. For this reason, the Radiation and Nuclear Countermeasures Program (RNCP), within the NIAID, NIH convened a workshop with other agencies within HHS to address cutaneous radiation injuries, partnering with the FDA’s Center for Drug Evaluation and Research (CDER) and Center for Devices and Radiological Health (CDRH), BARDA and the NIH National Institute of General Medical Sciences (NIGMS). Held in Rockville, MD on May 6 and 7, 2019, the target audience for the workshop included U.S. Government planning and funding entities, healthcare providers, hospital-based emergency management professionals, agencies involved with emergency preparedness, and industry and academic researchers engaged in assessing biomarkers for radiation-induced skin injuries and developing MCM treatment approaches. The workshop highlighted talks from 28 subject matter experts (Table 1) across five scientific sessions.
TABLE 1.
Workshop Speakers and Areas of Expertisea
| Name | Affiliation | Areas of expertise |
|---|---|---|
| Christopher Abularrage, MD | Johns Hopkins Medicine, Baltimore, MD | Ulcer and wound care, peripheral vascular injury |
| Peter Antinozzi, PhD | Argentum Medical, Geneva, IL | Wound care and dressings, product development |
| David J. Barillo, MD | Disaster Response/Critical Care Consultants, Mount Pleasant, SC | Mass casualty response/management, burn and wound care |
| J. Daniel Bourland, PhD | Wake Forest University, Winston-Salem, NC | Medical physics, oncology imaging, radiation oncology |
| Luke Burnett, PhD | KeraNetics, Winston-Salem, NC | Product development model development |
| Darrell Carney, PhD | Chrysalis, Galveston, TX | Radiation mitigators, product development |
| Deborah Citrin, MD | National Cancer Institute, Bethesda, MD | Radiation oncology, radiation injury |
| Nicholas Dainiak, MD | Yale University School of Medicine, New Haven, CT | Medical management of radiation injury |
| Andrea DiCarlo, PhD | RNCP, NIAID, NIH, Rockville, MD | Radiobiology, product development, MCM testing |
| Alexis Gabard, MS, MBA | Technical Project Solutions, Winston-Salem, NC | Product development, model development |
| Jorg Gerlach, MD, PhD | McGowan Institute for Regenerative Medicine, Pittsburgh, PA | Cellular therapies, devices for burn and radiation injury |
| Gautam Ghatnekar, PhD | FirstString Research, Mount Pleasant, SC | MCM development, wound therapies, product development |
| Ronald Honchel, PhD | CDER, FDA, White Oak, MD | Pharmacology, toxicology, Animal Rule, MCMs |
| Narayan Iyer, PhD | BARDA, HHS, Washington, DC | Radiation MCM development, thermal burn and CRI |
| Juliann Kiang, PhD | AFRRI, DoD,b Bethesda, MD | Animal models, MCM testing, RCI |
| Adebayo Laniyonu, PhD | CDER, FDA, White Oak, MD | Pharmacology, toxicology, Animal Rule, MCMs |
| Lixin Liu, PhD | CDRH,c FDA, White Oak, MD | Animal models, MCM development |
| William McBride, PhD, DSc | University of California, Los Angeles, Los Angeles, CA | Radiobiology, immunology, radiation mitigation |
| Maria Moroni, PhD | AFRRI, DoD, Bethesda, MD | Porcine models, MCMs for cutaneous radiation injuries |
| Neil Ogden, MS | CDRH, FDA, White Oak, MD | Device evaluation, imaging, MCM development |
| Kathleen Rodgers, PhD | University of Arizona, Tucson, AZ | Small molecule discovery, product development |
| Julie Ryan Wolf, PhD, MPH | University of Rochester Medical School, Rochester, NY | Pathology, dermatology, radiation-induced skin injury |
| Alla Shapiro, MD, PhD | CDER, FDA, White Oak, MD | Radiation, MCM development |
| Stanley Stern, PhD | CDER, FDA, White Oak, MD | Health physics, Animal Rule, MCM development |
| Radia Tamarat, PhD | Institut de Radioprotection et de Sûreté Nucléaire (IRSN), Fontenay-aux-Roses, France | Radiation biology, surgery, radiation burn wound care |
| Nushin Todd, MD, PhD | CDER, FDA, White Oak, MD | Medical affairs, Animal Rule, MCM development |
| Sue Jane Wang, PhD | CDER, FDA, White Oak, MD | Animal Rule, MCM development |
| Waylon Weber, PhD | Lovelace Biomedical Research Institute, Albuquerque, NM | Animal models, MCMs testing, product development |
All speakers had the opportunity to review this meeting report prior to journal submission.
Armed Forces Radiobiology Research Institute, Department of Defense.
Center for Devices for Radiological Health.
The purpose of the meeting was to: 1. discuss what is known about the clinical manifestations of cutaneous radiation injuries (CRI) in humans; 2. review current diagnostic and medical management of skin injuries (from radiation and other causes or complications, e.g., burns, diabetic ulcers and other wounds) in the clinic; 3. consider in vitro and in vivo human and animal models for radiation-induced skin injuries, including natural history, end points and medical management; 4. examine available radiation exposure devices and methods to induce injuries that simulate CRI in preclinical studies; 5. review MCMs currently under development to treat CRI; and 6. discuss whether current rodent and large animal models satisfy the requirements of the FDA Animal Rule, including relevance to injuries that could result from a radiation mass casualty incident. The agenda included presentations in many areas of preclinical development and clinical use of treatments. Participants and clinical experts provided context for methods to assess severity of skin injuries and progression of healing through a series of talks and guided discussions at the conclusion of each session. Other investigators with experience in preclinical modeling of these injuries, and in determining efficacy of MCMs to treat radiation-induced skin complications, presented and were part of the discussion. Together, the gathered medical, scientific and regulatory communities contributed to a greater understanding of CRI, available models and their use to advance MCM research. An overview of these presentations and discussions is provided below.
BACKGROUND
Radiation can be especially damaging, due to its impact on multiple tissues. These effects, when combined, can lead to severe morbidities and even death from multi-organ dysfunction and failure. Although CRI alone is not often life threatening, it can lead to complications including those that affect quality of life, such as chronic pain, fibrosis and disfigurement, which can translate into a lifetime need for medical interventions. In addition, when skin injuries are coupled with total-body irradiation [TBI; radiation combined injury (RCI)], skin injuries (in the form of thermal or radiation injuries and/or wounds) can reduce chances of survival. For example, after the Chernobyl accident, of the 115 patients presenting with acute radiation syndrome, most patients had injuries to more than one organ system, and 56 (48.6%) also had thermal burns (2). Early assessment of the severity and extent of CRI is often difficult, since clinical signs and symptoms develop over days to weeks after exposure to ionizing radiation. Erythema is the earliest sign of CRI and may be followed by skin ulceration. Delayed effects of injury to the soft tissue may manifest months or years after radiation exposure. Thus, for medical, and particularly surgical decision-making, clinical assessment of CRI must include consideration of co-morbidities (e.g., diabetes, hypertension, smoking, etc.), and estimates of radiation dose and dose rates, in addition to evaluation of surface area and depth of injury (skin only, versus muscle involvement), interaction with concomitant injuries, and systemic effects of radiation (3). In the context of CRI, dosimetry broadly refers to physical and biological modeling, measurement, computational simulation, quantitative estimation, and characterization of the radiation dose and resulting skin injury. Radiation dose and dose rate are used as prognostic indicators (4) to help guide early intervention. In industrial accidents where exposure parameters were known, biodosimetry along with dosimetric maps and models have informed the surgical boundaries for early excision of non-viable skin and soft tissues to minimize extension of injury to viable tissue (5). The effects of radiation dose can vary due to differences in intrinsic radiosensitivity of different cell types. Radiosensitive organs are characterized by highly proliferative and adequately oxygenated tissue. Within the skin, the melanocytes, hair follicle stem cells and the basal keratinocyte layer are most radiosensitive and are affected by deep dermal injury (6).
The challenge in developing models and methods specific to CRI is the need to consider exposure scenarios anticipated during a radiation public health emergency, and end points to be measured must be based on existing best practice of medicine. Animal studies of CRI have employed various radiation sources (e.g., X rays, beta rays and gamma rays, and neutrons) (7–13). Use of any of these modalities to simulate CRI in animals is generally considered reasonable, because the mechanisms of cell injury, necrosis and other downstream effects are similar between them and are consistent with the radiobiology of CRI. Dosimetric models of CRI are largely informed by experiences with radiotherapy patients and by animal studies conducted under controlled irradiation conditions. However, a scenario of concern is that of a ground detonation of an improvised nuclear device yielding, for example, a 10-kiloton TNT-equivalent blast (16). The medical exigencies ensuing from such a blast would include multiple, systemic insults and physiological responses such as ruptured eardrums and damaged lungs, blunt injuries from flying debris, and thermal burns (14, 15). A primary cause of CRI could be beta-particle emissions of radioactive fallout in prolonged contact with unprotected skin (16). Within 20 miles of the blast, dose rates from beta particle “ground shine” are estimated at approximately 1 mGy/h, while gamma-ray dose rates are estimated at 0.1 mGy/h (14, 16, 17). Gamma rays with an average energy of approximately 0.6 MeV would penetrate more than 30 cm in soft tissue (18), whereas beta particles with an average energy of approximately 0.4 MeV would penetrate approximately 0.1–0.2 cm of skin (16, 19). For skin doses ranging greater than 2 Gy, reactions range from transient erythema, epilation, moist desquamation, edema and acute ulceration, to dermal atrophy, induration and necrosis over timeframes of less than two weeks to 52 weeks, with severe injury requiring surgical intervention (20). Severe CRI can extend into the subcutaneous fat and muscle; its pathophysiology has been reviewed in detail elsewhere (20–22). A more in-depth discussion of these factors, as well as other considerations for creating, assessing and treating radiation-induced skin injuries is provided below.
MEETING PROGRAM OVERVIEW6
The two-day meeting was structured with the following scientific sessions.
Session 1: Skin Injuries from Radiation and Other Clinical Conditions. Here, clinical manifestations and assessment of cutaneous radiation and other injuries, and standard of care considerations were addressed.
Session 2: Radiation Sources and Animal Models of Cutaneous Radiation Injury
Session 3: Assessment Methods to Determine Extent of Skin Injuries
Session 4: Regulatory Considerations for Development of Products for CRI
Session 5: Medical Countermeasures to Treat CRI.
All sessions included a discussion, during which participants were provided with prompts to address issues of concern (Table 2). Common elements of these discussions are captured in the Discussion section below.
TABLE 2.
Topics Addressed During the Discussion Sessions
| Session | Topic |
|---|---|
| Session 1 | |
| Common pathophysiologic mechanisms that can be modeled from the clinical setting to the animal | |
| Standard methods to evaluate extent and depth of skin injury to define severity and progression | |
| Standards of care to be applied to the animal model | |
| Session 2 | |
| Strengths and weaknesses of each available model and how wound assessment is best conducted in each | |
| Impact of euthanasia and other IACUC criteria on animal models | |
| Gaps in appropriate modeling of drug efficacy with different mechanisms of action | |
| Species most suitable for small and large animal pivotal efficacy studies | |
| Usefulness of rodent models and their ability to reflect findings that extrapolate well to humans | |
| Session 3 | |
| Commonly used methods for assessing CRI and their mapping to end points | |
| Standardization of wound placements if multiple per animal and their systemic interaction | |
| Appropriate end points for use in animal models | |
| Session 4 | |
| Considerations for animal models of CRI (animal care, euthanasia criteria) | |
| Methods for verifying depth or grade of injury | |
| Study design and data quality issues (reproducibility, single versus multiple labs) | |
| Statistical issues surrounding multiple wounds in the same animal | |
| Clinical outcomes for burn wounds and chronic cutaneous ulcers: incidence of complete wound closure, time to complete closure, facilitation of surgical closure, quality of closure | |
| Appropriateness of end points for a CRI product using the Animal Rule | |
| Consideration of additional end points for a successful CRI product, e.g., meaningful reduction compared to the untreated group in the development of full- or partial-thickness injury | |
| Appropriateness of survival end point, e.g., in combined injuries | |
| Appropriate methods for assessing these end points for CRI | |
| Utility of repurposing approaches for other related conditions in CRI studies | |
| Session 5 | |
| Impact of selection of a model for MCM testing on findings of efficacy | |
| Impact of infection and sepsis derived from radiation-induced chronic cutaneous wounds on animal models | |
| Key elements to successfully developing new therapies for CRI | |
Session 1: Skin Injuries from Radiation and Other Clinical Conditions
In the first session of day 1, the intent was to set the stage on the current understanding of radiation injuries to the skin. This involved a historical look at human exposures resulting from radiation incidents, such as those observed in atomic bomb survivors, as well as victims of nuclear energy accidents, nuclear testing, and industrial or medical overexposures. In addition, subject matter experts from different dermatologic and vascular disciplines shared best medical practices in their fields of thermal burn and diabetic foot ulcers, to highlight established assessment and care protocols in those areas.
Historical experience from large-scale human exposures to radiation
Beginning with an exploration of the 1945 bombings in Japan, an overview of three major incidents involving cutaneous radiation exposures was presented. These included the U.S. bombings of Hiroshima and Nagasaki, Marshall Islands nuclear testing, and the Chernobyl Nuclear Power Plant accident. The goal of this overview was to learn about the types of skin injuries that resulted from these radiation exposures and understand the outcome of medical treatments used for the injuries. As a physician first responder during the Chernobyl accident, the speaker focused on her experience treating patients after the incident (A. Shapiro).
Perhaps the most significant human radiological incident was the large-scale exposure and resulting devastation from the dropping of the atomic bombs on Japan in August of 1945. Although the majority of all deaths occurred immediately after the explosion, reports estimate that over 50% of the deaths were due to thermal burns, as the resulting fireball temperature reached one million degrees Celsius (23). In addition, ~65% of the casualties had combined radiation injuries (i.e., radiation exposure combined with another trauma such as burns or other wounds) (24, 25). Patients with burns at Hiroshima were all less than ~1.4 miles from the hypocenter of the explosion at the time of the bombing, and in Nagasaki, patients with burns were observed out to the remarkable distance of ~2.6 miles. Several types of burns were noted in the survivors, including those resulting from direct exposure to fire, and also flash-burns, which presented with different pathologies than the fire burns. Flash burns showed immediate erythema, and skin that was covered by clothing appeared to be protected dependent on the color of the fabric.7 At the time, burn treatments were very crude, and included topical applications of cooking oil, potato or cucumber slices, and tomato juice.8
Less than ten years later, there was another atomic incident that resulted in unanticipated human exposures, with both systemic radiation damage and also skin injuries. The Marshall Islands in the Pacific were an important test site for the U.S. military. Although there were 67 nuclear tests carried out there by the U.S. between 1946 and 1958,9 problems developed with the March 1, 1954 detonation. This particular testing led to fallout for the atolls of the Marshall Islands, and in particular, crewmembers on a Japanese fishing boat were exposed to fallout and sustained severe radiation skin injuries.10 Although the detonation that day initially went as planned, testing of a larger and more potent bomb design led to an unexpected reaction, which meant the explosion was much larger than predicted. In addition, the prevailing winds were stronger than meteorologists had forecasted and went in unanticipated directions. These factors resulted in widespread fallout contamination to islands hundreds of miles downwind from the test site, and consequently high radiation exposures to the Marshall Islanders (26). These exposures of nearby populations (~250 persons) to radioactive fallout resulted in nausea, vomiting, and skin beta burns associated with large external doses (up to 1.9 Gy).11
Although inadvertent radiation exposures continued to be documented in the intervening years between 1954 and 1986, most of these were limited in terms of number of individuals affected, and tended to occur in Russian and U.S. research and industrial settings.12 However, on April 26, 1986, as a treating physician in Kiev, Ukraine, Dr. Alla Shapiro had first-hand experience in managing the care of employees and first responders after the fire and explosion that occurred at the Chernobyl Nuclear Power Station. There were fatalities and injuries at the site, and changing winds allowed for dissemination of dangerous radionuclides across many parts of world. Triage care provided to casualties within the first 36 h included antiemetics, symptomatic treatments, sedatives and potassium iodide (27). Twenty-two patients died 14–34 days after exposure and in twenty of those fatalities, beta burns were the main cause of death. An additional five patients succumbed from 48–99 days postirradiation, which is after the bone marrow recovery stage. Although 13 patients received bone marrow transplants, 11 of them died. Concomitant skin burns were thought to be a contributing factor as to why the transplants were seemingly ineffective. Both early and late skin lesions were noted in patients, which included erythema, edema, blisters and ulcers (early) as well as pigment alterations, atrophy, keratosis, non-healing ulcers and fibrosis (A. Shapiro). In addition, basal cell carcinomas were noted in some patients years after the initial radiation exposure.13
There were some interesting skin pathologies noted in those with radiation skin injuries. For example, the face and wrists were found to be the first areas affected, followed by the neck and feet, and then torso. Presence of wrinkling in those areas is thought to be the cause of the early reaction after the burn was produced. Also, burn severity was found to be worse for those individuals who worked the night shift at the plant. Because the accident occurred at 1:23 am, night shift employees, without access to locker room keys, could not obtain clean and dry uniforms, and therefore spent significant time in uniforms drenched in radioactive water (A. Shapiro). The most severe skin lesions were observed in patients who also had severe radiation-induced myelosuppression and GI syndrome.
Early skin injuries led to chronic skin syndromes in several patients (A. Shapiro). Skin ulcers were found to be progressive and often complicated with infections. Late manifestations included keratosis and fibrosis as well as hyperpigmentation and telangiectases (even after 15 years had passed). Although significantly more advanced than the crude remedies that were used in Japan in 1945, there were still many aspects of the treatment of the Chernobyl accident victims that were experimental. Systemic treatments to address the radiation and thermal burns included hemoperfusion, plasmapheresis, continuous heparinization, and administration of fresh frozen plasma. Local treatment of skin injuries consisted primarily of combutec-2 (a polymer formulation based on soluble collagen with antibacterial elements to promote skin regeneration) (28, 29). Lioxazol, an approved spray that was composed of a combination of hydrocortisone and topical antibiotic, was also applied. Pain management was challenging and not effective due to a scarcity of local anesthetics, and in some cases, there was a need for early-stage surgical interventions (2, 27, 30, 31). Although not used at the time of the Chernobyl incident, Indralin, an α1-adrenomimetic radioprotector (32–34) is also now approved in Russia for the treatment of radiation victims, and alongside Lioxazol, is part of a standard, anti-radiation first aid kit on hand at the site (30). There were many lessons learned in Chernobyl about the nature and progression of CRI. What was unexpected was the diversity of clinical manifestations of skin lesions and unrecognized course of clinical stages of radiation injury to skin. Because of the significant severity of injuries that were noted, there was a pronounced influence of skin burns on the general state of a patient. Finally, more surgical operations than anticipated were required at an early stage of the injury. The take-home message is that a nuclear accident anywhere has the potential to be a nuclear accident everywhere, as evidenced by the Chernobyl experience, which also revealed that safety culture at radiation/nuclear facilities requires constant assessment to prevent equipment malfunction and human errors. It is also important to note that the presentation and manifestation of radiation skin burns differ from thermal burns, and that novel, multidisciplinary therapeutic approaches for treating victims of radiation accidents open new prospects in the field of medical care for future radiation casualties.
Radiation cutaneous injuries resulting from industrial accidents
The Institute for Radiological Protection and Nuclear Safety (IRSN), under the joint authority of the Ministries of Defense, the Environment, Industry, Research, and Health in France is the nation’s public service resource for nuclear and radiation scientific and technical activities. The IRSN, together with the Hôpital d’Instruction des Armées Percy (Percy Hospital) in Paris have a broad and unique experience working together to address CRI in humans. Radiation accidents present certain distinctive characteristics, which explains why healthcare management is so complex, and harmonization of the methods of diagnosis and treatment is needed (R. Tamarat). In 2001, a manual was published by expert scientists evaluating worldwide victims of radiation accidents (35). Several of the case studies highlighted in that publication, as well as a few cases that have occurred since that time, were presented to demonstrate the severity of cutaneous injuries that might be observed after a radiological or nuclear incident. In general, radiation burns are not thermal burns, and therefore, standard clinical burn treatments may not be appropriate to radiation-induced lesions (R. Tamarat). For example, radiation burns are a dynamic process: they evolve over time in successive inflammatory waves, making prognosis difficult because the development of lesions is often delayed. Further, wound healing takes a long time, and closed wounds are often fragile and unpredictable. Perhaps the most challenging difference is that the pain resulting from a radiation skin wound is often resistant to opiates, which can lead to psychological crises for the patients.
The first case study presented involved a radiation exposure at the Yanango Hydroelectric Power Plant in Peru on February 20, 1999 (36). During a gammagraphy assessment of a pipe being repaired, a source pigtail became detached from the equipment. The welder placed the iridium (Ir)-192 source in his pocket and began to experience pain at the end of the day. Preliminary dose estimates showed high localized doses to the welder and low doses to his family and other persons. Persistent complications ensued, along with moderate to severe lumbar pain and necrosis by day 72. Unfortunately, that patient continues to suffer skin complications and chronic pain, even 20 years later (R. Tamarat). In the second radiation exposure case, which occurred after an incident in Lilo, Georgia in 1997, soldiers found a sealed radiation source in the forest, which was then placed into a jacket pocket (37). As a result, one patient was hospitalized in France on the 25th day after exposure. After four excision procedures, five skin autografts and one omentum flap, the wound finally closed; however, due to the chronic and latent nature of radiation wounds to the skin, the patient returned to France 22 years later, and was treated again (38).
The third radiation accident that was documented occurred at a building site for a cellulose manufacturing plant in Nueva Aldea, Chile on December 4, 2005 (39). In that incident, involving arc welding quality control, an Ir-192 source was found outside its storage container. A worker held the source in his hand then transferred it to his pocket, with the total time of exposure estimated at 40 min (1,900 Gy skin surface exposure) (40). The patient was transferred to the burn treatment department of Percy Hospital, and a new dosimetry-guided surgical approach was used to examine the pathology of the lesion after removal (41). Although the victim continued to experience superficial erosions on occasion, years after the exposure, the skin was essentially fully-healed in the exposed area. Significant in the Chile case was that a new treatment approach was tested involving mesenchymal stem cells (MSCs) derived from autologous bone marrow expanded ex vivo, that were then re-injected into the site of the irradiated wound (42). These highly proliferative stem cells have the capacity to acquire the morphology and function of damaged resident cells, as well as the capacity for growth factor production, immunotolerance and multipotentiality (they can become bone cartilage, muscle, stroma, tendon or adipocytes). Using a cell therapy unit for clinical-grade MSC production approved by the French regulatory agency (CTSA, Percy Hospital), cells are harvested and cultured for ten days, and are then selected for MSC differentiation and amplified for injection. These cells have been used along with other treatment modalities such as wound dressings or skin autografts (R. Tamarat). Improved progression of healing was observed in patients given these cells, as evidenced by their successful use in the treatment of a hand injury, which resulted in complete functional recovery and a dramatic decrease in pain for the patient (5).
In the fourth human radiation accident case considered, another Ir-192 source for arc welding quality control was found outside a storage container in Francisco de Orellana, Ecuador on April 12, 2009. Three spots appeared on the leg of the victim after exposure, and he was hospitalized in France later that month. Dosimetry-guided surgery and phantom reconstructions were also used to treat this patient; however, additional lesions continued to appear, and the initial injury was not improving. For this reason, at day 38 after exposure, physicians pursued more excisions, skin grafts and ultimately MSC injections into the wound site, which were repeated on day 51. Additional skin transplants on day 65 finally led to healing of the CRI.
In the final case report presented, involving an Ir-192 source accident in Dakar, Senegal in 2006, a patient was sent to Percy Hospital for assessment (including dose reconstruction) and treatment 29 days after radiation exposure (43). His hematopoietic acute radiation syndrome was successfully treated with cytokines, which led to recovery of his bone marrow (44); however, he had also suffered radiation burns that led to moist desquamation on his left arm (45). By day 63 postirradiation, the wound had extended from his shoulder to elbow, and was associated with intense pain. Treatments were initiated using a standard surgical approach that included use of a dermal substitute and skin autograft. The spontaneous evolution of the wound was marked by whole dry necrosis involving the underlying muscles. The patient was also treated with the autologous MSC therapy that had been successful with the patient from Chile detailed above (5) as well as conservative surgery. Dose reconstruction estimated 70 Gy at the surface of the skin. Multiple treatment attempts also included a skin flap that eventually became ischemic and necrotic. Finally, after multiple MSC therapies and skin grafting, the lesion finally healed, and the pain disappeared.
Although the above case histories represent small-scale exposures, they are informative in that they provide insight into the predictable complexity of a mass casualty incident. In addition, follow-up with some of the patients suggests that radiation necrosis can re-appear even years after the initial exposure, reinforcing the need for long-term monitoring. For this reason, it is critically important to prepare, conduct and evaluate exercises to test preparedness for response to nuclear and radiological emergency, and be prepared to spend many years engaged in medical follow-up.
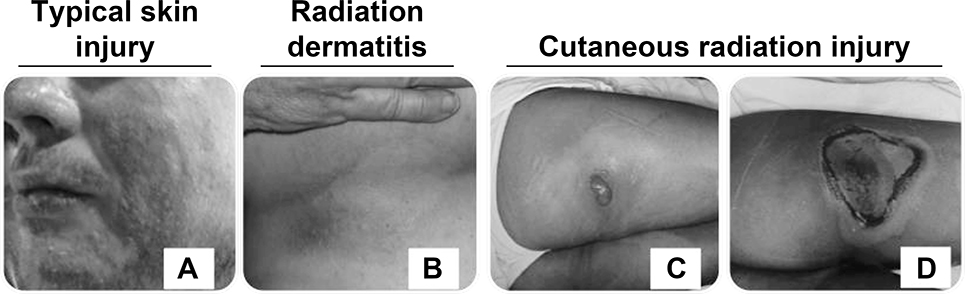
Radiotherapy and fluoroscopy-induced cutaneous injuries
Skin injuries from radiotherapy continue to be a problem despite technological advances in these kinds of cancer treatments, and there are currently no effective treatments to prevent or reduce radiotherapy-associated skin reactions (J. Ryan Wolf). Acute skin reactions (radiation dermatitis) are a commonly observed toxicity from radiation therapy (46); however, there is larger variation in late effects such as fibrosis, with incidence ranging from 6–85% (47). Treatment- (dose, body location, fractionation) and patient-(age, gender, obesity) related factors contribute to severe radiation-induced skin injuries. Skin reactions from radiotherapy are most common in patients receiving radiation to the neck, face, upper chest or back, or extremities. The clinical rating scale most commonly used for radiation dermatitis is the NIH Common Terminology Criteria for Adverse Events (CTCAE), which has five grades of severity, ranging from light erythema (grade 1) up to ulceration/skin necrosis (grade 4) and death (grade 5). Approximately 20–25% of radiotherapy patients experience grade 3 or 4 skin reactions. A major need in this field is a more objective and quantitative way to measure severity of radiation dermatitis rather than multiple, subjective clinical rating scales (46). Radiation skin injury presents in various stages depending on the dose to the skin and length of time exposed, with hair loss, erythema or hyperpigmentation, dry and moist desquamation, weeping, and ulceration possible (48). After fractionated radiation doses >45 Gy, late or chronic radiation skin effects such as continued ulceration, atrophy, fibrosis, and telangiectasia may be noted even years after exposure. Radiation-induced skin fibrosis results from overproduction of connective tissue and can also be caused from infections, implants, autoimmune disease and tumors (49). In 2001, Schmuth et al. (50) showed that trans-epidermal water loss, a functional measure for epidermal integrity, increases as the severity of radiation dermatitis increases. These increases are temporary, and the skin barrier is often able to recover. Radiation burns are not thermal burns in that they have a dose-dependent clinical pattern in skin breakdown, and inflammatory waves can occur for weeks to years after exposure. Radiation recall is another skin complication seen in radiotherapy. It is an uncommon and unpredictable inflammatory reaction that is confined to a previously irradiated area that is triggered by a systemic medication, such as chemotherapy or antibiotics (51).
Radiation skin injury can also occur from fluoroscopy procedures that use X rays. In fluoroscopy, such as that used during cardiac catheterization procedures, an X-ray beam contributes its high dose at and within a few centimeters of the skin surface, with a normal initial presentation of a rash within a week of a procedure, which can then progress and persist. Within a year, patients have presented with nonhealing ulcers diagnosed as fluoroscopy-induced chronic radiation dermatitis. Standard care is often in the form of topical steroids and surgical debridement, with or without skin graft. Fortunately, these kinds of adverse fluoroscopy reactions are now uncommon, due to limitations on the length of time for fluoroscopy procedures or repeated procedures in the same area (52, 53).
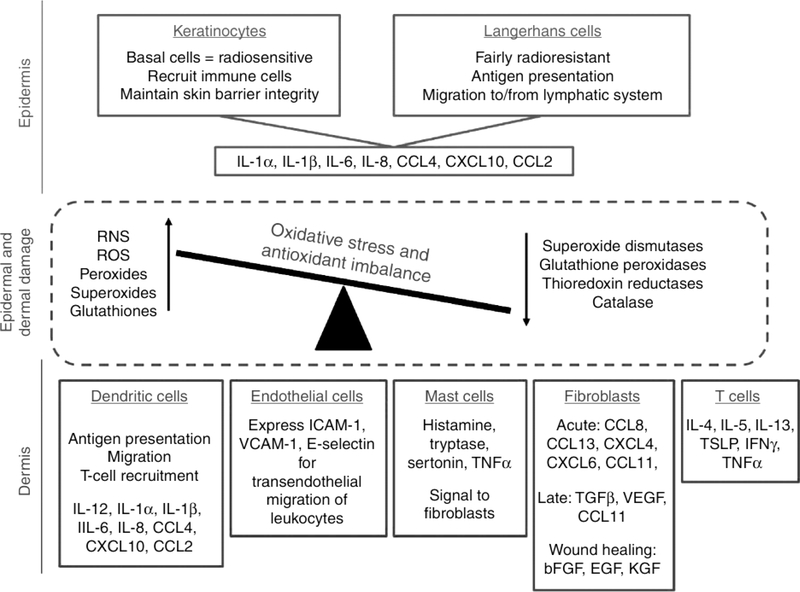
In terms of mechanism, radiation skin injury is a complicated process involving an imbalance of antioxidant status and redox control of wound healing, as well as chronic inflammation (Fig. 2). Radiation skin fibrosis is a result of chronic inflammation from tissue injury in which there is an immune imbalance that causes release of profibrotic cytokines (54, 55). Overall, an effective therapeutic would be one that targets more than one aspect of the immune system (48, 56, 57).
FIG. 2.
Tissue mediators of radiation skin effects. Shown is a schematic identifying the key cells and mediators involved in radiation skin injury. (Reprinted with permission, J Invest Dermatol 2012; 132/3, part 2:985–93; Ryan JL. “Ionizing Radiation: The Good, the Bad, and the Ugly”)
Until recently, standard medical management for radiation therapy-associated dermatitis has consisted of washing the area and applying water-based moisturizing creams. In a recent clinical trial, 16 different topical, standard-of-care treatments were utilized at six different cancer sites (J. Ryan Wolf). The most commonly used topicals were Aquaphor®, Silvadene®, and topical steroids, based on the results of a study addressing high-grade dermatitis in patients who received radiation therapy after a mastectomy (58). To date, there is little consensus on topical agents that could provide alleviation of symptoms, although a few approaches have been studied, including pentoxifylline and alpha-tocopherol in combination (59, 60); silver nylon dressings (61); hyaluronic acid (61); Silvadene (62); epidermal growth factor (EGF) (63); and statins (64). Another novel treatment for skin fibrosis is visible red light, which decreases collagen production and fibroblast proliferation (65), and is cleared by the FDA for acne and herpes infections. Further development of therapeutics addressing the skin microbiome could be beneficial, since microbiota and immune cells both respond to skin damage, and harnessing both could lead to accelerated and scarless healing (66). Given the similarities in injuries that occur in human cancer patients and some low-level CRI reactions, radiotherapy-induced dermatitis in the clinic could potentially provide insight into developing models for CRI. In addition, more studies on the skin microbiome, wound healing of other clinical complications (e.g., diabetic ulcers) and chronic skin diseases such as psoriasis may help identify effective therapeutics.
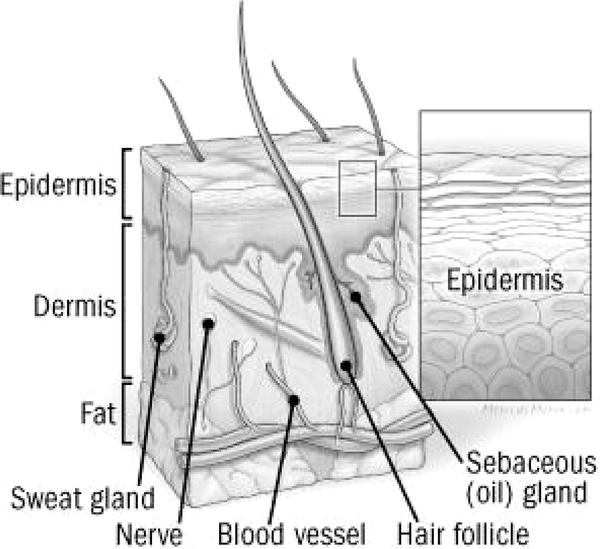
Clinical experience in thermal burn
Autologous keratinocyte spray-grafting represents an innovative investigational approach for potential use in the treatment of radiation skin burns in humans (J. Gerlach). Skin anatomy is made up of the epidermis, dermis, with underlying fat, and lower levels of muscle and bone (Fig. 1). Radiation burns are most problematic in the lower layers because cells in the upper layers are either dead or viable but not dividing. Because the basal layer (stratum basale) contains stem and progenitor cells, it represents the greatest interest for radiation burns (67). Standard therapeutic options to address skin wounds include full-thickness skin grafting, split skin or mesh-split skin (allows for stretching of the graft), micro-grafting skin cubes (1 mm), and more recently, single-cell spray-grafting. Culturing keratinocytes in sheets and then applying to the wound is also an approach, but these grafts do not always take, and the closure can be thin and vulnerable (68). In addition, keratinocytes have a high division rate, but during culture, stemness of the cells can be lost, resulting in transplantation of primarily more mature keratinocytes. In contrast, epidermal stem/progenitor cells from the regenerative basal keratinocyte layer can be isolated and sprayed onto the wound where they can then increase in size, divide, and differentiate within the site of injury. To achieve this, cells for spray-grafting are isolated by enzymatic digestion and then sprayed onto the wound bed (69). Current investigational work has focused on the development of the stem cell spray devices. Although this approach might work well for first- and second-degree burns, third-degree injuries require mesh grafting.
FIG. 1.
Cross-section representation of the skin.19 The three major layers of the skin are shown, along with underlying structures.
It is important to note that the source of the cells is defined by different patterns of surface markers. Ideally, cells should be isolated from the dermis as an autologous source (J. Gerlach). These cells behave in vitro in the same way as MSCs from other sources, in that they differentiate into adipocytes, chondrocytes and osteocytes. Case studies have been published describing the experience with spray grafting in over 71 patients (70, 71), and the treatment has been evaluated in a number of different burn etiologies, including flame, scald, grease, chemical and electrical, among others. Experimental results were successful independent of the cause of the injury, suggesting that spray grafting might be extrapolated for use in the treatment of radiation burns. Another approach for potential skin wound treatments is the use of active wound dressings (with inflow and outflow fluids) to enable tissue engineering in the wound. These technologies could be brought to bear in healing of mild first- and second-degree radiation burns. These novel dressings regulate the chemical environment of the wound (e.g., pH, electrolytes, nutrition), remove debris, and allow for the provision of regenerative factors and local antibiotics (72). In summary, there are a number of innovative investigational technologies that are being developed to address thermal burns that could have applicability in the treatment of radiation-induced skin injuries.
Clinical experience in chronic wounds
There exists overlap between studies of chronic wounds resulting from disease states, such as diabetes, because radiation burns often involve the vasculature, as do diabetic foot ulcers. There are a number of underlying factors in the development and progression of diabetic foot complications, which involve neuropathy and local trauma, and can lead to skin ulceration in ~25% of cases. These ulcers often become chronic wounds that do not heal normally because of poor blood flow, structural imbalance, infection, edema and poor glycemic control. In some instances, the failure of these wounds to heal is a risk for limb loss. In diabetic wounds, vascular disease of both the macro- and microvasculature is predominant. Involvement of major blood vessels bringing blood to the site of injury is classified by angiosomes (specific areas of the skin supplied by a single vessel; direct perfusion). Radiation is known to cause macrovascular diseases through activation of cytokines and recruitment of inflammatory cells and can also lead to stenosis in the larger blood vessels. Clinically, it is important to define wound healing, which is commonly referred to as complete epithelialization and restoration of sustained functional and anatomical continuity for six weeks after healing (73, 74). Chronic wounds have multiple risk factors that can be affected by radiation exposure, including poor perfusion to specific arteries and impaired microcirculatory reactivity to stimuli, which can make it difficult to predict which wounds will heal. Other factors include narrowing of larger arteries and structural deformity due to scarring and edema.
There are several classification systems commonly used for assessing wounds resulting from diabetic complications, with the wound, ischemia, and foot infection (WIfI) model being preferred by clinicians as an accurate predictor of wound healing. In this scoring system, all three individual components of the skin complication are individually graded on a scale of 0–3 to generate a composite score and clinical staging (75). Wounds are graded based on ulcer, gangrene and clinical description; ischemia is graded 0–3 based on perfusion and ankle and toe pressures, and infection is graded 0–3 (none to systemic inflammatory response). This system has been used by other researchers to accurately predict the probability of wound healing (76–79). In summary, there is a wealth of knowledge that can be accessed from both the human radiation experience of accidental and clinical exposures, as well as from existing practice of medicine for other types of skin injuries, such as thermal burns, and chronic, non-healing wounds. Learning more about how wounds are assessed and treated in these other situations can help guide the selection of the best approaches to address CRI.
Session 2: Radiation Sources and Animal Models of Cutaneous Radiation Injury
When embarking on studies to look at mechanisms of radiation-induced skin injuries, biomarkers for severity of damage as well as testing of MCMs, it is critical to select animal models that both match the proposed action of the approach to be tested and represent anticipated human responses. As discussed above, data from human exposures has its limitations, in terms of dose of radiation received and inter-individual variabilities in response. Animal models, however, represent a means of studying radiation-induced skin damage that can be closely monitored, and damage is more uniform than that seen in humans due to the fact that the radiation exposure is closely controlled. In this session, different species of animal and human skin models, both in vivo and in vitro, are considered, as well as different means of creating radiation-induced injuries.
Cutaneous radiation injuries created using different radiation sources
Before embarking on a new study to investigate cutaneous radiation injuries, it is important to first consider how the radiation-induced skin damage will be generated. There are many ways to induce radiation skin injury. For example, sunburns are a simple case study that can manifest injuries ranging from first degree (erythema) to second degree (blistering) and third degree (necrosis). Although ozone blocks some of the ultraviolet light that reaches Earth, and application of sunscreen can block even more, radiation from a weak energy source (like the sun) can still create burns of concern. There are other, more powerful radiation emissions from sources such as Co-60 and Cs-137, which are gamma-emitters but also emit beta radiation at different energies. Similarly, radiation exposure devices can have different energies. For example, Grenz irradiators (20 kV), orthovoltage radiotherapy units (200–300 kV), and linear accelerators (LINACs) (6–20 MV) cover a large range of X-ray energies. Whereas low-erenergy photons have long wavelengths and lower penetration, higher energies have shorter wavelength and higher penetration. All of these details must be considered when designing a model for radiation-induced skin injury.
Researchers at Lovelace Biomedical Research Institute have used a Grenz machine to deliver a dose of 150 Gy of X rays to produce injuries in Göttingen minipigs (W. Weber). Animals were photographed at day 60 postirradiation, and although very little effect of the exposure was seen early on, profound necrosis was noted at later time points for some dose levels. This is because the Grenz device provides a more superficial, surface dose, depositing most of the dose in the outer layers of the skin. In contrast, when a 250 kVp X-ray machine was used, which possesses a ten-fold higher energy, less damage was noted on the surface, but injuries were seen deeper within the skin layers. In fact, pigs exposed to X rays from the 250 kVp irradiator died because of underlying, systemic radiation effects. Similarly, irradiation with a 6 MV LINAC resulted in the need to euthanize animals due to hematopoietic complications within the first nine days, although there were no dermal wounds (W. Weber).
Particles can also be used to create radiation skin wounds, which might better approximate radiation injuries resulting from fallout. Unlike photons, they have a physical mass, and are grouped into alpha (helium nuclei, α) or beta (electron, β) particles. An alpha particle is not likely to result in a full-thickness wound because the particles do not penetrate beyond the top layer, which protects the underlying tissue. However, this kind of particle can be very damaging if it is internalized (e.g., through inhalation, ingestion or wound contamination). Beta particles deposit their energy in the first several layers of tissue, resulting in more external damage compared to photons; however, there is also deeper tissue damage resulting in complex wounds. The presence of particles creates more damage at lower doses compared to photons. The linear energy transfer (LET), or the amount of energy deposited per unit distance, explains why the severity of skin injuries is not always proportional to dose.
In summary, it is important to understand the source that will be used for the radiation exposure. Pure gamma rays will require a large dose to create a dermal wound, while alpha particles as an external beam directed at the surface are less likely to result in a significant dermal wound (for intact skin, alphas do not penetrate the outer dead layer, and thus, do not reach living tissue). Beta particles, which would be the biggest concern in a fallout exposure, have penetration at all dermal levels. Lower doses can result in dermal injuries similar to high gamma doses. In terms of isotopes with multiple routes of decay (beta and gamma), exposure will result in wounds from either of these radiation emissions; however, the beta injuries will be more pronounced due to dermal interactions. The radiation exposure should be relevant to the desired skin injury model (e.g., full- or partial-thickness or combined injury).
Radiation combined injuries
Radiation combined injury (RCI) has been previously defined as an injury that involves both radiation exposure and other trauma. (80, 81). RCI can result from a radiological dispersal device (RDD) or a nuclear detonation event. Both the Hiroshima and Nagasaki atomic bombings resulted in many combined injuries, comprising upwards of 39–42% of the injuries noted in victims (82). In animal models of burns or wounds combined with TBI, combined injuries reduce survival (83). This was demonstrated in a mouse model of skin wound or burn, combined with photons alone, or a combination of gamma rays and neutrons, in which animals were irradiated and then wounded 1 h later. Survival was assessed at day 30 postirradiation; photon radiation was found to delay the wound-healing rate and skin thickness, a finding that was worse when neutrons were involved (84–86). Rodent models may be reasonable for early studies to screen MCMs for RCI. For example, wound areas in the rat correlate well with blood vessel regeneration (87), and the use of mouse models of radiation skin injury to determine MCM efficacy by survival and wound healing have been demonstrated (84, 88).
Wounding enhances radiation injury-induced biomarker signals from hours to days after exposure (86). For example, wounds increase iNOS protein levels in the skin and also the level of some circulating cytokines, primarily pro-inflammatory interleukins and chemokines, and in animals exposed to combined wound and radiation, systemic bacterial infection increased (85). Combined injuries were also found to alter blood cell counts in a manner different from radiation or wounding alone. Levels of other serum biomarkers such as c-reactive protein (a marker of chronic inflammation), C3, prostaglandin E2 and Ig, although variable based on the nature of the injury (wounding, burning or combinations), may represent good biomarkers for these injuries (89). A number of drugs have been screened at the Armed Forces Radiobiology Research Institute (AFRRI) for their ability to improve wound healing and survival in an established mouse model for combined radiation injury (J. Kiang). Only a few drug approaches were shown to be successful in accelerating wound healing in the RCI mouse model; these include ciprofloxacin, ghrelin, and bone marrow-derived mesenchymal stem cells (J. Kiang). In summary, wound-induced alterations in levels of circulation blood cells, platelets, cytokines, c-reactive protein, complement C3, IgM, and prostaglandin E2 cause homeostatic imbalances. Clinically, evidence of elevated levels of these factors in blood, taken together with skin biopsy, could be a reliable measure of wound healing prognosis, and agents that target these pathways could be therapeutic for addressing wound healing postirradiation.
Guinea pig model of cutaneous radiation injury
Several companies have approached the FDA for consideration of both their drugs and animal models for approval to treat CRI. US Biotest (San Luis Obispo, CA) has received U.S. Government funding to develop a guinea pig model for CRI, to test their MCM candidate, DSC127 (also called USB001) (90). It was important to identify appropriate, large animal models to simulate human CRI and the impact of drug treatments, since rodents are known to have skin properties that differ from humans and can lead to dissimilar permeation of drugs across the skin (91). There are a number of reasons that the guinea pig model is a preferred choice for radiation-induced skin injury studies. This rodent species has a skin architecture and thickness that is similar to humans (92), in that its hair growth cycle has follicles that grow independently in time (93), they are tight-skinned, and therefore have contracture similar to humans (94), and their metabolism and bacterial responses are also similar to humans (95). The company has used the Dunkin-Hartley guinea pig, an albino strain derived from the short-haired English guinea pig, as their animal model to assess MCMs for radiation skin injuries under the Animal Rule (K. Rodgers).
The device in use for US Biotest radiation exposures is a 50 kVp X-ray machine (90), which is optimized to administer low-penetrating radiation (50% of the radiation energy deposits at 3 mm) (K. Rodgers). Lead shielding is used to restrict radiation to a specific area of the skin. Prior to irradiation, fur is removed by shaving and then the skin is depilated using Nair™. During the study described, it became clear that it is of the utmost importance to be mindful of how the wounds will be cared for in any animal model of skin injuries. For example, guinea pigs are known to scratch their wounds if they are unbandaged, and therefore, hygiene must be carefully considered. Great effort was devoted to designing the bandages used for the wounds. Given the nature of these experiments, animal care concerns need to be incorporated into the study design, along with humane end points for euthanasia (if applicable).
Among the available visual scoring scales (Table 3), U.S. Biotest scientists selected the Kumar scale to assess the extent of injury in the guinea pigs, ranging from a score of 1.0 (no effect) to 5.0 (full-thickness, open wound), with scoring increments of 0.5. This scoring system has been used historically in animal models of skin wounds (96). In addition to the Kumar scale, the Radiation Therapy Oncology Group (RTOG®) Clinical Assessment System for Cutaneous Radiation Injury (97) was also utilized to assess severity of damage in the guinea pigs, to more closely align with scoring used clinically. Unlike the Kumar scale, the RTOG system has a six-point-range scoring scale (0–5); however, it has a more compressed scale with only integer scoring and includes death as a score of 5. US Biotest researchers established a natural history of their CRI model by exposing animals to localized radiation doses ranging from 23–79 Gy. They found they could achieve severe radiation-induced skin ulcerations in the model and observed improvements in healing when wounds were treated with their product, USB001, when initiated either at start of erythema or at loss of dermal integrity (90). They also established an in-house histology scoring system, which incorporates aspects of epithelial integrity, blood vessel presence, depth of collagen damage, inflammation and quality of adipose tissue. Using these end points, the group established the ability to treat irradiated skin with USB001 to reduce inflammation in the upper dermis (90). The company has developed a severe CRI guinea pig model and has shown efficacy of their drug by visual and histologic assessment, and reduced expression of inflammatory cytokines. Researchers concluded that this full-thickness ulceration model provided a replicable injury for which clinical and histological assessment of severe CRI was possible.
TABLE 3.
Different Skin Injury Scoring Scales Discussed at the Meeting
| Scale name | Preclinical or clinical | Features | Ref. |
|---|---|---|---|
| Common Terminology Criteria for Adverse Events (CTCAE) | Clinical | Scoring ranges from grade 1 (light erythema) to 5 (death) | (47) |
| Wake Forest University (JD Bourland) | Clinical | Scoring ranges from grade I–IV; correlates in-person and pictorial scoring; measured features are erythema 0–6, and moist desquamation 0–3. | (107) |
| Erythema and moist desquamation | Clinical | Scoring ranges from 0–4 based primarily on redness, swelling and peeling of the skin | (99) |
| Acute Phase Skin Scoring (Dion) | Preclinical | Scoring ranges from 1.0 to 5.0 (0.5 increments) based on erythema, desquamation (dry and moist), necrosis and loss of dermis | (148) |
| Kumar | Preclinical | Scoring ranges from 1.0 (no effect) to 5.0 (full-thickness, open wound), with scoring increments of 0.5 | (96) |
| METREPOL | Clinical | Scoring ranges C1–C4; based on erythema, sensation, swelling, blistering, desquamation, ulcer, hair loss, and onycholysis. Does not incorporate pain assessment | (127) |
| Radiation Therapy Oncology Group (RTOG) | Clinical | 6-point range scale; 0 = no injury to 5 = death. Scoring on atrophy, pigmentation, telangiectasia, hair loss, ulceration | (97) |
| University of Texas San Antonio Diabetic Wound Classification System | Clinical | Wounds graded by depth (0–III). Divides based on vascular complications or infections and dept of necrosis. Four stages within each grade (non-ischemic clean, non-ischemic infected, ischemic, infected ischemic | (170) |
| Visual Analog Scale (VAS) | Clinical | Scale based on erythema, dry and moist desquamation and ulceration | (100) |
| Wound Ischemia and foot Infection (WIfI) | Clinical | Scores from 0–3 in each assessment area in patients with diabetic foot ulcers; Vascular assessments are wounds (ulcer, gangrene) ischemia (perfusion), and infection (none to systemic) | (75) |
Porcine (minipig) skin radiation injuries
In animal model development conducted at AFRRI, large animal species have been studied as potential models for human skin injuries caused by radiation (M. Moroni). Specifically, CRI in the Göttingen minipig strain was modeled on a documented human radiation accident involving skin injuries, which occurred in Maryland in 1991 (98). In this accident, while conducting maintenance on an accelerator, a technician received radiation exposure to his hands, feet and head from the beam. This exposure led to severe damage to the hands, resulting in amputation of affected fingers. In designing the minipig model, researchers attempted to recreate injuries that paralleled those observed clinically, through delivery of 50 Gy to the back of the animals, resulting in non-healing, partial- to full-thickness CRI. The use of 4 MeV electrons generated by a LINAC, in conjunction with a 1 cm bolus material, limited the damage to the epidermal and dermal layers. Six sites per animal were irradiated, and animals were monitored for 90 days, with clinical observations and wound scoring, blood samples and histopathology conducted. The lesions that formed in the minipig were compared to the lesions suffered by the Maryland accident victim and were found to correlate closely in terms of severity and timeline. During model development, lessons learned included the need to produce a level of injury from which recovery was possible, to understand the nature of the lesions, including predictability from experiment to experiment. There were several sources of variability identified, which included the cells affected in the pig skin and the immunological status of the animal,14 as well as radiation quality and radiation scatter from nearby bones underlying the skin. To move beyond a clinical description of the injury toward a more quantifiable outcome, a combination of imaging, histology and other novel methods (e.g., planimetry, color image analysis, ultrasound, thermography, MRI, etc.) were employed. Kumar scoring and other methods, such as an adapted Visual Analog Scale (VAS, based on erythema, dry and moist desquamation and ulceration) were also considered (96, 99, 100). Common pathologies in the Göttingen minipig included erythema, edema, inflammation, vascular damage, tissue necrosis, alopecia, fibrosis, thinning of the epithelial layer, and loss of hair follicles.
In working with this model, it became clear that extra care was needed when obtaining skin biopsies and that more non-invasive methods would be preferred. Furthermore, progress of wound healing needs to be determined across various depths of skin to ensure stable healing. In discovering appropriate biomarkers to use as a determinant of healing, some cytokines, including TGF-b1, appeared to be upregulated after injury, which is known to lead to delayed healing (101). In summary, the Göttingen minipig appears to be suitable to study CRI, since the lesions generated by radiation exposure are similar to those seen in humans. Development of this model has established end points that may be applicable to assessing the severity of skin injury and studying the efficacy of MCMs to mitigate CRS.
Porcine (Yorkshire) skin radiation injuries
White pigs are relatively well-characterized in terms of the similarity of their skin to humans and are easily trained for handling (102). They are frequently used for study of drug efficacy for many dermatologic indications including vitiligo, necrosis, burns, wounds and melanoma (103). Several strains of these animals have been used in radiation skin research dating back to the 1980s (104, 105). More recently, the Yorkshire pig has been studied for its ability to demonstrate significant improvements in skin healing with MCM administration after exposure to a beta radiation source (J/D. Bourland). Researchers at Wake Forest University using this animal model have developed a unique beta irradiation device that is composed of an array of Sr-90 sources (106). Radiation emissions from this novel device, tested using ionizing chambers and film dosimetry methods, show good uniformity, with a dose rate of ~2.64 Gy/min. Dose profiles were found to have acceptable homogeneity, flatness and symmetry.
In this model, animals are irradiated in ten circular areas (five per side, 10 cm2) and then treated at day +35 postirradiation with an MCM (107). Radiation doses evaluated have ranged from 16 to 42 Gy. Evaluations are done until day +70, at which time strip biopsies are collected, images are scored, and histology is conducted. CRI symptoms progress reliably from epidermal degradation to moist desquamation with exposure to doses in excess of 24 Gy. The progression of CRI is most pronounced at the highest radiation doses, with scabbing noted between +35 and +46 days postirradiation (107). A unique, on-screen image-scoring technique is conducted using both an erythema and moist desquamation scale, with a consensus score then derived. This method, conducted in a single laboratory, reduces bias, allows for more independent scorers to be utilized, and shows good correlation when compared to in-person scoring. Other scoring modalities have also contributed to the overall assessment of the wound, including histopathology and planimetry. The Wake Forest University research group is currently working toward development of Good Laboratory Practice (GLP) capabilities to continue to carry out this work, in the hopes of making the model the basis for advanced development of an MCM for CRI.
Alternative skin models
Although a number of appropriate animal models for the study of CRI have been published, they are still just models of the human situation. Therefore, there is still knowledge to be gained by using alternative human skin models (e.g., in vitro constructs), to more fully understand radiation responses in human skin. More than 50 different kinds of cells make up the complex structure of human skin, in addition to other components such as vascular, neuronal and immune (108). Advances in tissue engineering have provided additional models for the study of the human skin radiation response (D. Citrin). Several models that were considered included human and animal cell lines, organoids, full-thickness skin, tissue chips, 2-D and 3-D models and dermal equivalents. As with in vivo models, the goal of these alternatives is to more closely simulate human skin, minimize animal use, and allow for less expensive screening of potential MCMs. Epidermal models, such as one in which a bed of cells is scratched to simulate injury, are able to discern decreased wound healing capacity (109), and other 2-D cell models assess wound healing by measuring contraction of a gel in which the cells are grown (110).
There exist several commercially-available, 3-D tissue products, which usually have both a dermal and epidermal layer, along with an air/liquid interface. These include EpiDermFT™, Phenion® FT Model, StrataTest®, Hyalagraft 3D, Apligraf and Tissue Tech Autograft. In addition, one study on how matrices can be used to heal wounds used a biopsy punch of human skin, which was injured and then used to test different dermal substitutes (111). One of the problems with these in vitro models is that they often lack supporting cells (e.g., dendritic, Langerhans, endothelial, mast, and T cells as well as the skin microbiome) that play a critical role as mediators of radiation-induced tissue injury and repair (Fig. 1). Although many alternative in vitro platforms allow for evaluation of histologic outcomes like collagen accumulation and fibroblast proliferation (112), it is difficult to reproduce other skin responses commonly observed in patients, such as vascular leakage, hemorrhage and infiltration of immune elements (113). To address these potential confounders, tissue engineering using human constructs has led to the development of 3-D printed models, in which the various structural elements can be layered (114). Using induced pluripotent stem (iPS) cells to create both animal and human skin organoids also provides models that more closely resemble human skin and its niche elements; however, these models lack the influence of the immune system. Although these alternative approaches do have limitations, they are nonetheless useful in understanding aspects of CRI, especially those dealing with structural damage.
There currently exist many in vitro, in vivo and ex vivo surrogate models that are available to conduct preclinical studies on different aspects of CRI. Some of these models are more appropriate for determining a mechanism of action of the radiation-induced injury, whereas other models may be better used to pursue studies for MCM efficacy that could provide necessary data for drug approval.
Session 3: Assessment Methods to Determine Extent of Skin Injuries
Moving beyond scoring paradigms to determine the depth and severity of CRI, talks in this session focused on other novel means of assessing skin wounds, with presentations and discussions focusing on imaging modalities, clinical grading and histopathological assays, as well as functional outcomes, such as mechanical means of determining strength of healing.
Overview of wound imaging methods
In bringing a skin imaging device to the market, it is important to establish a consistent regulatory strategy. This necessitates an understanding of how the device will be used (e.g., systemic versus topical; invasive versus non-contact) and if it will mimic an existing clinical or pathological assessment or a new measurement (N. Ogden). In addition, one must determine in what setting (e.g., in the field or in the lab) use is anticipated, since the regulatory pathways can vary based on these factors. There have been a number of technologies for general skin imaging that have been reviewed by the FDA, including optical approaches, Raman, OCT, laser doppler, laser spectral, hyperspectral, near infrared, spatial frequency domain, fluorescence and photoacoustic. Although there are numerous steps associated with clearance of a device for CRI, demonstration of “levels of evidence”, typically stand-alone clinical data showing performance, is at the center of any effort.
Data requirements that need to be addressed for a device to be reviewed by the FDA include device labeling, performance specifications, an understanding of any tissue effects (e.g., increased temperature or blood flow), clinical validation of detection and valid scientific evidence. The latter requirement has been defined in 21 CFR 860.7, which states “Valid scientific evidence is evidence from well-controlled investigations, partially controlled studies, studies and objective trials without matched controls, well-documented case histories conducted by qualified experts, and reports of significant human experience with a marketed device, from which it can fairly and responsibly be concluded by qualified experts that there is reasonable assurance of the safety and effectiveness of a device under its conditions of use.” 15 There are a number of devices that have been cleared for wound imaging to date,16 including:
Old Tech Verge Videometer provides 3-D volume measurements for wounds.
moorLDl Laser Doppler Imager is used for blood flow studies in a range of clinical research applications.
Visitrak™ System (Smith and Nephew) uses a template to calculate wound area and can also determine wound depth.
Silhouette® (ARANZ Medical) is used for wound measurement and documentation.
Aimago Easy LDI is used for blood flow measurements in the microcirculation.
SpectralMD™ DeepView™ Wound Imaging System (Spectral MD) is used for studies of blood flow in the microcirculation.
WoundVision Wound Measuring and Monitoring System is a combination digital and infrared camera that provides a measure of wound and body surface data.
Optical imaging technology for wounds represents an emerging field in many medical applications, particularly coupled with dermatology diagnostics (115); however, no devices have yet been cleared for imaging of CRI or radiation dermatitis.
Radiation effects on skin wound tensile strength
Scientific studies to determine the effects of radiation on the skin began in the early 1940s, when Strandquist determined that the effect of radiation on the skin depends on the dose and time of exposure and that fractionation was an important component (4). These findings were further supported by work using pig skin that demonstrated the effect of number of fractions of radiation on skin-related radiotherapy complications (116). Later, others generated plots to derive injuries resulting from alpha and beta in pig skin (117), and Withers (118), who developed the first in situ clonogenic assay, showed that skin will remain intact (no evolution to moist desquamation) if postirradiation clonogen survival in the skin is approximately 10–6 per cm2. In full-thickness wound healing, the dermis is considered to be a slow-proliferating, late-responding tissue (119). Complex tissue responses that occur in CRI are the reason that the dermal tissue is so different from typical acute responses (W. McBride).
A murine model has been developed in which a full-thickness incision is made in the skin and then allowed to heal. Skin from the healed wound is then removed and cut into thin strips. When placed in a device called a tensiometer that applies pressure to and stretches the strip, it is possible to determine the applied force needed to break the wounded skin open again, referred to as the wound tensile strength (WTS). This technique is reproducible (120–123) and can measure the strength of healing of the wound in the presence or absence of radiation and MCM treatments. Using this approach, it has been shown that for animals irradiated prior to wounding, WTS (at day-14 after wounding) was 40% lower. In a partial-shielded model (hemi-body irradiation in which only the bottom half of the animal is irradiated), wound healing was found to be impaired. Furthermore, the resulting radiation injury varied depending on whether the radiation exposure was localized to a part of the skin or to the entire body. At lower doses, TBI decreased WTS. Even if more than three months elapsed between irradiation and incision, skin did not recover its tensile strength, despite appearing visually normal. For this reason, clinicians are often hesitant to perform surgery on preirradiated sites (124).
In the progression of wound healing over a five-week period, there are several phases of repair, with inflammation occurring from one to two weeks, tissue formation from two to three weeks, followed by remodeling from three to four weeks. RNA-Seq analysis suggests a complex wound signature with different cell types, and genes expressed (high within the first week, but declining by the end of the second week). There are also processes that occur during healing (e.g., lymphocyte activation, phagocytosis and chemotaxis, vasculature development). Bone marrow-derived mesenchymal stromal cells (MSCs, which are multipotent progenitor cells that can differentiate into fibroblasts, osteoblasts, chondrocytes, adipocytes, myocytes, stromal cells, and may transdifferentiate into vascular/perivascular cells at sites of injury) can home in on damaged tissues. MSCs placed directly into the wound site are under study as a means of correcting radiation-reduced WTS. Use of this cellular treatment approach improves healing of wounds caused after TBI, but for optimal effects, a structure to deliver sufficient cells to the wound site is needed. Research suggests that culturing the MSCs on fibrin microbeads (FMBs) delivered to the wound promotes in situ cell proliferation and survival and has also been shown to benefit hair follicle re-growth (123). These FMBs are biodegradable and can last two to four weeks in vivo. These MSC-FMB constructs are being evaluated to correct wound healing deficits caused by TBI and skin-only irradiation, but they are better at compensating the former, which compromises the bone-marrow derived cellular infiltration. Whereas FMBs are applicable for use in smaller wounds, the technology can be adapted to larger wounds using collagen sheets, which can be fabricated to allow MSCs to be delivered to a larger surface area (123). In addition to MSC use for radiation-induced skin wounds, research has focused on a B-Raf enzyme inhibitor, vemurafenib (marketed as Zelboraf® for treatment of late-stage melanoma). The agent causes hyperproliferative responses in the skin, and when added to a radiation wound, might increase healing (as measured by a gain in WTS) via a MAP kinase pathway (125).
Diagnosis and medical management of cutaneous injury after accidental exposure to ionizing radiation
In addition to other scoring systems in use to assess skin injuries, METREPOL (MEdical TREatment ProtocOLs for Radiation Accident Victims) grading, which includes scoring for other radiation injuries as well as skin, can be helpful to determine the course of treatment for injured patients during a mass casualty incident (126–128). Signs and symptoms for skin injuries are rated from 1 to 4, based on a number of diverse criteria. Classification of skin injuries by colleagues in the METREPOL project provided the first objective system to compare cutaneous injuries observed among different radiological incidents; it is used today with minor modification by clinicians worldwide (N. Dainiak). As a follow-on to the establishment of this scoring system, in 2009, the World Health Organization (WHO) convened a panel of 37 experts (from 13 countries) to rank the evidence for medical countermeasures for management of acute radiation syndrome (ARS) in a hypothetical scenario involving the hospitalization of 100 to 200 victims. The goal of this panel was to achieve consensus on optimal management of ARS affecting nonhematopoietic organ systems based on evidence in the published literature (129). The WHO Consultancy discussed approaches for clinical management of radiation injuries, including specific suggestions for treatment of CRI based on an evidence-based review, and made treatment recommendations for radiation-induced skin wounds:
Topical class II–III steroids, antibiotics and antihistamines;
Silver sulfadiazine cream with non-adherent dressings;
Surgical excision of necrotic tissue and skin grafts/flaps/amputation.
Interestingly, systemic steroids were not recommended, unless there is another medical reason for their use, and the panel noted that some products with limited data (e.g., pentoxifylline, α-tocopherol, transforming growth factor-b, fibroblast growth factor, interferon-γ and estradiol) could be viable treatment options. As for the use of cellular therapies such as MSCs, the group found controlled clinical trials were needed to assess their efficacy. One anecdotal report supporting their possible use involved the treatment of an industrial skin wound with adipose-derived MSC. That patient, after receiving hyperbaric oxygen treatments, still experienced wound recurrence and pain, which was resolved (healed lesion and pain decreased) at four months postirradiation after MSC therapy (130).
Several human exposures were presented for consideration, which involved internal contamination with radionuclides. The first was the poisoning of Alexander Litvinenko, in which he was determined to have ingested 1,800 Bq of 210Po radiation per gram of skin tissue (131). The second was a nuclear worker who experienced skin contamination with 238Pu from an industrial procedure. In that case study, contaminated tissue was excised to remove the isotope (132). These human exposures highlight the fact that skin complications arising from radiation are not limited to high-dose, external X-ray or gamma exposures. In summary, assessment of what lies beneath the skin surface is required to inform medical decision-making in humans; this evaluation may include radiological surveys, ultrasound imaging and thermography. Radiation injury to the skin and surrounding tissues may be localized, but a systemic effect may be observed.
Histopathology assessments of cutaneous radiation injury
The skin is not considered to be especially radiosensitive; however, as it is the largest organ, it can be more affected than other areas of the body (D. Barillo). In addition, localized radiation therapy has to transit the skin layers to be deposited in the deep organs, thus there are inadvertent skin injuries in human patients undergoing cancer treatments. Unlike thermal burns, radiation injury creates a chronic wound that has a large effect on the vasculature, creating ischemia in the tissues and making the damage difficult to address. There have been documented human exposures to radiation fallout that have resulted in beta burns to the skin. For example, beta burns of the feet and neck were noted in one patient one month after fallout exposure from the Castle Bravo 15 megaton thermonuclear test (133, 134). In addition, there were beta burns noted in victims of the Chernobyl Nuclear Power Plant accident (31).
Generally, histopathology is considered the gold standard for characterizing CRI. In irradiated minipigs, quantifiable measures of CRI include the presence of subepidermal edema, ulceration, collagen thickness, hypodermal changes, presence of vascular damage, and number of hair follicles and sebaceous glands. In pig skin, only a very small proportion of basal cells are stem cells. By giving a sufficient radiation dose to produce moist desquamation in the minipig, at day 21 postirradiation, the number of visible layers in the epidermis is reduced and the dermal ridges that lead to stronger skin are lost. Damage consisting of epidermal hyperplasia and dermis cell infiltration can be revealed with immunostaining (118), and biomarkers such as TGF-b1 have been proposed as indicators of inflammatory response and delayed wound healing (119). In a Göttingen minipig model of gamma-radiation-induced skin injury, erythema presents in waves. Onset of the first wave tends to occur within 24 h of exposure and lasts several days; the second wave begins between 10 and 14 days postirradiation. This is typically the only presentation for exposures in the range of 2–5 Gy. At higher radiation doses, erythema can be followed by dry (12–20 Gy) and/or moist desquamation (acute dose exceeding 25 Gy or cumulative dose over 40 Gy) at later time points. Ulcerations are also possible in exposures higher than 30 Gy, with necrosis a possibility at doses above 35 Gy. To assess wound severity, there are a number of different modalities that can be considered:
Clinical assessment, including photography and documentation of wound size;
Planimetry, which relies on digital color photography followed by computer analysis to determine the progression of injury or of healing;
Thermography, which is useful as both a research tool and for pre-operative planning;
Ultrasound, which is widely available and allows assessment of deeper tissue injury;
Histopathology, which is the gold standard, although accessing tissue for staining can be challenging.
The above methods have different situations in which they are most useful. For example, planimetry is objective, quantitative, and can measure the wound area, but assesses only the skin surface. It is useful both in research and in the clinic to document re-epithelialization and wound closure. However, assessment of deeper tissue and microvascular damage may require techniques such as ultrasound, thermography, and light-based imaging. A combination of ultrasound and thermography to image skin lesions has been used to evaluate subcutaneous changes in irradiated animals and human patients (135). Optical imaging devices have been used to quantify the 3-D volume of wounds and blood flow in the microcirculation (115). Areas of continued research include the use of magnetic resonance spectroscopy and fusion imaging to evaluate skin function (e.g., metabolic changes) rather than structure. Finally, point-of-care ultrasound devices are now widely available, and some versions are now very compact (portable, battery-operated, and hand-held, built on smartphone and iPad formats). Because of the low risk associated with many of these approaches, these devices, which facilitate serial examination, should be further investigated for evaluation of CRI.
Session 4: Regulatory Considerations for Development of Products for CRI
The fourth session of the meeting comprised presentations from FDA staff. To provide consistent information that the FDA considers important to the development of CRI product advancement, the talks are presented here as an integrated narrative. Included in this session were talks on: 1. dosimetry considerations for skin irradiation; 2. study designs and statistical considerations, difficult experimentation for cutaneous radiation injury drug development; 3. non-clinical considerations for drug development under the Animal Rule; and 4. regulation of wound dressing devices and considerations for development of medical devices used for cutaneous radiation injury.
Development of drug products for CRI should include studies of the natural history of disease, radiation dose-response curve, and pharmacokinetics of therapeutic product in animals. The safety of MCM products designed to counter radiological threats is evaluated in healthy volunteers; however, where human efficacy studies of MCMs are unethical or not feasible, the “Animal Rule” allows the FDA to grant approval of new drugs or biologics based on efficacy studies in animals, provided that such studies are well controlled and establish the MCM product as reasonably likely to provide clinical benefit in humans (136). Generally, the efficacy of the drug product should be demonstrated in more than one animal species; however, it is not necessarily rodent and non-rodent, as the rule is silent on which species is selected. Understanding the natural history of CRI in the animal model is also essential to establishing clinically meaningful end points and the timing of end point measurement. Landmark timepoints include the manifestations of maximal injury, optimal wound healing in response to standard care and investigational treatment, and post-healing timepoints to show durability of treatment effect. Natural history studies should establish a reproducible injury model with well characterized documentation of the depth and area of the wound based on histological verification. Consideration should be given to supportive care, including adequate pain management, wound debridement when clinically indicated, and criteria for euthanasia.
For clinical studies of therapies for non-healing chronic wounds, the FDA recommends as the primary end point complete wound closure, defined as skin re-epithelization without drainage or dressing requirements confirmed at two consecutive study visits two weeks apart, and durable wound closure (based on follow-up evaluation at least three months after complete wound closure). Complete wound closure of a chronic, nonhealing wound is one of the most objective and clinically meaningful wound healing end points (137). The duration of efficacy studies should be long enough to establish the durability of treatment effect.
Desired clinical outcomes in CRI include improvement in survival, reduction in the depth and area of irradiated skin that undergoes necrosis, improvement in healing or ability to achieve durable skin coverage of the wound, and improvement in the quality and durability of the skin repair. Additional outcomes include facilitation of skin closure using surgical wound closure and grafting, reduced time to wound healing or surgical closure, decreased infection at the wound site, quality of healing (e.g., decreased scarring that may improve function, improved cosmesis), and improved wound care (e.g., decreased need for pain management). Examples of efficacy end points in animal models of CRI include the assessment of wound area and depth or the proportion of wounds meeting a minimal level of improvement (e.g., at least x% of the defined area improved); evidence of durability of treatment effect is also necessary.
While complete re-epithelization and durable wound closure is desired, wound healing demonstrated with a meaningful reduction in full-thickness CRI17 may be considered for product development under the Animal Rule. The demonstration of a defined reduction in wound size may also be considered clinically meaningful, if it can facilitate additional interventions for wound closure. Partial-thickness CRI generally requires the demonstration of complete wound closure/healing. The incidence and time to full closure should be assessed in the animal model in the presence of standard wound care (surgical and nonsurgical). Descriptive end points that do not adequately characterize the depth and area of skin injury (e.g., moist desquamation) are not recommended. Efficacy determination may also include improvements in tissue histology of irradiated sites. Histologic characterization of the wound(s) in the animal model is recommended at pre-specified time intervals determined in natural history studies.
Efficacy of treatments for CRI may be assessed using either a two-arm parallel design (treatment animals and matched control animals, each with multiple injury sites) or a paired design in which a single animal has treated and control sites in bilaterally symmetrical locations. While the latter is generally more efficient, efficacy gains may be offset by two major drawbacks: blinding to the treatment allocation of skin sites in a single animal is challenging, and contamination of an animal’s control sites with the treatment product is a risk for topical studies (138). Wound scoring and histopathological evaluation by personnel blinded to treatment are important to minimize bias in an adequate and well-controlled study for Animal Rule licensure. Statistical approaches to account for correlation among skin sites within an animal should be considered. The length of trials and the number of test animals required may be reduced via a two-stage adaptive design approach that uses the same end point for establishing dose response as well as for demonstrating efficacy with the selected dose. Design efficiency depends on how much learning can be gained in stage one, which may also include an improved investigation of the natural history of CRI, in addition to assessing dose-response relationship.
As of 2019, no wound dressing device for CRI has yet been cleared or approved for marketing by the FDA. Wound dressings cleared for radiation dermatitis may be an appropriate predicate device for the 510(k) review of a dressing indicated for the same signs and symptoms in patients with CRI, provided that there are similarities in the primary action of the device (i.e., to provide a moist wound healing environment) and in the health status of indicated patients. Dressing devices intended for severe CRI and comorbidities associated with CRI may not be appropriate for 510(k) review, and additionally, depending on the claims and mechanism of action, other regulatory paths may be appropriate. Wound healing studies in animals are recommended for 510(k) submission when a device is cytotoxic, which may have the potential to impair the natural wound healing process, or when the sponsor elects to evaluate local tissue response in lieu of an implantation study as part of the biocompatibility assessment. Note that the Animal Rule does not apply to devices, as it may be acceptable not to have clinical data for some marketed devices. As an animal model is being developed, it is important to have a conversation with the FDA and demonstrate what the study will look like in terms of model and end points. In closing, regulatory guidance from the FDA should be sought as early as possible, so that resources are not wasted in developing models that would not be acceptable to the agency for the Animal Rule, or another pathway to approval for marketing. Regulators are hoping to understand from scientists the current thinking in their area of research, and what should be incorporated into the regulatory process to make the path to drug approval more predictable and standardized.
Session 5: Medical Countermeasures to Treat CRI
The final session of the conference focused on medical countermeasures to address CRI. For the purposes of the meeting, MCMs for CRI included both physical barrier (e.g., wound dressings) and drug treatment approaches. Also included was additional information on appropriate animal models and metrics to assess MCM efficacy.
Overview of NIAID/BARDA portfolios and possible repurposing of approaches
The RNCP, NIAID has supported several funding mechanisms focused on skin research (A. DiCarlo). These mechanisms include RC1 challenge grants on radiation-induced skin injuries funded through the American Recovery and Reinvestment Act, combined injury R21/R33 grants, Small Business Innovation Research (SBIR) grants (R43/R44), an interagency agreement (IAA) with the Armed Forces Radiobiology Research Institute (AFFRI), and both pilot and full projects funded through the Centers for Medical Countermeasures against Radiation Consortium (CMCRC). The RNCP has categorized types of skin damage as either radiation-only injuries localized to the skin by gamma, beta and X-ray sources, or RCI. RCI is further categorized as irradiated wounds (incision or punch) or irradiated thermal burns. Such thermal burns are created in several ways, including contact with scalding water or a heated metal bar contact, flash exposure, or ignited ethanol. The RNCP has identified the following animal models that have been utilized since 2009 in studies in their funded portfolio: mice, guinea pigs, minipigs, domestic pigs and human ex vivo skin. Study model selection is based on availability of animals and equipment with oversight by IACUC. End points for studies commonly used are survival, time to full closure, percentage healing, histopathology, limb shortening, barrier function, wound tensile strength, and biomarkers of injury with impact of MCM intervention. Current approaches under study by the NIAID include many small molecules, antibodies, cellular therapies, antioxidants and growth factors regulated by the Center for Biologics Evaluation and Research (CBER), FDA and CDER, FDA as appropriate (Table 4). In addition, BARDA has supported the advanced development of approaches that are generally under CDRH regulatory purview, such as Silverlon® wound dressing (Argentum Medical LLC, Geneva, IL), and KeraStat® Cream (KeraNetics Inc., Winston-Salem, NC), both detailed below.
TABLE 4.
Skin MCM Studies Supported by the NIAID
| MCM | Site (mechanism) | Model |
|---|---|---|
| Granexin gel (aCT1 peptide)a | AFRRI (IAA) | Minipig (CRI) |
| TP508 (thrombin peptide)a | University of Texas Medical Branch, Galveston (SBIR) | Mouse TBIb + wound |
| Nor Leu 3-A(1–7) (angiotensin analog)a,b | US Biotest (grant) | Guinea Pig and mouse RCIb (thermal) |
| Antibiotics (cipro, gentamicin)a | Multiple (IAA) | IR alone / RCI (burn or wound) |
| Mesenchymal stromal cells (MSCs)a | UCLA (grant) | Mouse |
| Curcumin (nutraceutical)a | University of Rochester (grant) | Mouse |
| Celecoxib (non-steroidal anti-inflammatory drug) (NSAID) | University of Rochester (grant) | Mouse RCI (wound) |
| Timolol (beta blocker) | University of California, Davis (grant) | Ex vivo human culture – RCI (burn) |
| Esculentoside-A (Chinese herbal) | University of Rochester (grant) | Mouse IR alone |
| Granulocyte-colony stimulating factor (G-CSF) | AFRRI (IAA) | RCI (wound) |
| Ghrelin (hormone) | AFRRI (IAA) | RCI (burn) |
| CpG-ODN (TLR9 receptor agonist) | Brigham and Women’s Hospital (grant) | Mouse IR & RCI (burn) |
| Ex-RAD (chlorobenzylsulfone derivative) | AFRRI (IAA) | Mouse IR & RCI (wound) |
| Insulin-like growth factor-1 (IGF-1) | Duke University (grant) | Mouse RCI (wound) |
| Bone marrow cells | Duke University (grant) | Mouse RCI (wound) |
| ARA-290 (non-erythropoietic peptide from erythropoietin) | AFRRI (IAA) | Mouse RCI (wound) |
| ALXN-4100 (TPO mimetic) | AFRRI (IAA) | Mouse RCI (wound) |
| 17-DMAG (Hsp90 inhibitor) | AFRRI (IAA) | Mouse RCI (wound) |
| Euk-189 (SOD/Catalase mimetic) | University of Rochester/MCW (grant) | Rat IR alone |
| Euk-207 (SOD/Catalase mimetic) | University of Rochester/MCW (grant | Rat IR alone |
| Meloxicam (NSAID) | AFRRI (IAA) | Mouse RCI (wound) |
| Recombinant IL-12 | University of Rochester (grant) | Mouse IR alone |
| Bone marrow derived MSCs | AFRRI (IAA) | Mouse RCI (burn) |
| Hemjoba (cannabinoid derivative) | AFRRI (IAA) | RCI (wound) |
| Kineret (interleukin-1 receptor antagonist) | University of Massachusetts (grant) | Mouse IR alone |
| JP4-039 (mitochondrial-targeted gramicidin S (GS)-nitroxide) | University of Pittsburgh (grant) | Mouse IR only |
| Alpha-chemokine | AFRRI (IAA) | Mouse RCI (burn) |
Presented at the meeting.
Also funded by BARDA.
Abbrevations: AFRRI = Armed Forces Radiobiology Research Institute; CRI = cutaneous radiation injury; IAA = inter-agency agreement; IR = ionizing radiation; MCW = Medical College of Wisconsin; MSC = mesenchymal stromal cell; NSAID = non-steroidal anti-inflammatory drug; ODN = oligodeoxynucleotide; RCI = radiation combined injury; SBIR = Small Business Innovative Research; TBI = total body irradiation.
Cellular therapy approaches to treat cutaneous radiation injuries
IRSN’s expertise in regenerative medicine has focused on stem cell therapy and its impact on radiation-induced lesions involving skin, muscle and bone that lasts decades (R. Tamarat). It has been well established that tissue regeneration involves several major processes: 1 mobilization of bone marrow cells that pre-differentiate into inflammatory cells; 2. circulation of angiogenic cells to be recruited to the site of lesions for revascularization; and 3. participation of resident stem cells in the damaged tissue. As described in several studies, stem cells used for treatment originate from different sources such as the bone marrow (i.e., MSCs), blood (i.e., cord blood, somatic stem cells) and other organ-specific tissues such as the heart, brain and adipose tissue. Mechanisms of action driving cell homing and tissue regeneration span from endothelial cell to smooth muscle cell differentiation and paracrine effects, to intrinsic mechanisms and host-tissue effects. Together, the interaction of the pathways regulating these activities allow for the remodeling and regeneration of tissues. Percy Military Hospital has performed stem cell therapy in human patients, with technical support from IRSN scientists who developed experimental animal protocols (139). They have documented complete healing of radiological burns with functional recovery and rapid loss of pain during patient follow-up. To optimize the strategy based on stem cell therapy, researchers from IRSN showed that adipose-derived stem cells (ADSCs) participate in dermal wound healing by promoting re-epithelialization and angiogenesis (140). This work showed that adipose lineage cells could represent an alternative cell source for therapy in the context of wound healing. The study method involved delivery of a full-thickness wound made by punch application on the back of mice, and subsequent 20 Gy irradiation. To assess the ability of ADSCs to fuse with epithelial cells, ADSCs from female mice were transplanted into male recipients. Follow-up assessments included morphometric observations to determine wound closure, laser Doppler to measure cutaneous blood flow, a cutometer to determine viscoelasticity and immunohistochemistry. Stem cells were found to enhance vascular density, improve blood perfusion to the skin and have a positive effect on angiogenesis in the affected tissues. Furthermore, skin viscoelasticity was higher in animals treated with ADSCs, and wound closure was accelerated (140). Another study demonstrated the beneficial effect of bone marrow mononuclear cells on radiation-induced skin lesions, by preventing vascular dysfunction, permeability and unfavorable remodeling in the acute and late phases after radiation exposure (141).
The IRSN group later sought to determine the effect of stem cell therapy by combining MSC cells with ADSC cells and endothelial progenitors cells to stimulate tissue regeneration after irradiation. MSCs with the ability to secrete paracrine factors were delivered for immunomodulation, which demonstrated a dose-dependent effect of the cells. More importantly, the neovascularization process was investigated by different approaches, including microangiography, cutaneous blood flow assessment with laser Doppler for perfusion imaging, and capillary density analysis in frozen sections of gastrocnemius muscles. Finally, based on a strategy of improved treatment in a mass casualty scenario, another therapeutic approach that has been explored by IRSN teams over the past ten years is to treat CRI with extracellular vesicles (EVs). Known to be involved in the regulation of biological processes (142, 143), EVs play an important role in intercellular communication. Recently published studies show a role for EVs in radiation injuries to multiple organ systems (144, 145), including the skin (146), suggesting their use as a therapeutic. In summary, bench-to-bedside advancements in cellular therapies to treat radiation skin injuries are ongoing, with outcomes observed in patients informing research. This paradigm of a partnership between clinicians and investigators represents an effective means of accelerating the advancement of these valuable therapies.
Repurposing burn dressings to address radiation skin injuries
Argentum Medical, LLC is funded by BARDA to advance development of their Silverlon burn contact dressing for a radiation indication (P. Antinozzi). Silverlon consists of a single layer of knitted nylon fiber substrate coated with metallic silver and is currently cleared for the management of a wide variety of wounds including partial-thickness wounds and 1st and 2nd degree burns.18 The goal of the company is to obtain clearance for Silverlon dressings for both radiation therapy-induced dermatitis as well as CRI. To do this, the company has devised a two-stage regulatory strategy. Stage one seeks clearance for indications in lower-severity radiation injuries leading up through dry desquamation with clinical data in radiotherapy patients. Stage two seeks a submission for higher-severity indications leading up through moist desquamation and necrosis. Preclinical studies utilizing a Yorkshire swine model and beta-irradiation devices with highly reproducible single radiation doses per site are planned in stage two. Assessments will include visual observations weekly and end of study, and histopathology at necropsy. Three independent scorers will perform visual assessments at the time of bandage change, based on Erythema and Moist Desquamation scales (discussed above). For computational scoring, an image analysis pipeline is used to process study images. On-image color patches are used for image scaling with respect to color and lighting quality measures. Every image is assigned a computational score and a longitudinal analysis is established for each wound site. In a similar fashion, histopathology-scoring bias is also being addressed with further development of such computational strategies. This scoring platform is scalable and can be distributed for remote scoring of both clinical and preclinical studies. It is the company’s hope that this assessment method, which avoids bias and incorporates computer learning, will be acceptable to the FDA in terms of determining degree of injury, and amelioration of damage by application of the dressings.
Approaches targeting skin structural components
Kera-Netics presented on MCM approaches under development that target skin structural components to retain barrier function. Skin injuries presented were characterized as typical, radiation dermatitis or CRI (Fig. 3). Typical skin injuries (Fig. 3A) such as abrasions and thermal/chemical burns are immediately evident and have a known course of healing. Radiation dermatitis (Fig. 3B) has an unpredictable course of healing with evidence of injury that progresses over time. Much like radiation dermatitis, CRI (Fig. 3C) also exhibits evidence of injury that progresses over time (A. Gabard). The visible effects to the skin are dependent on the magnitude and penetration depth of the radiation dose with lesions appearing hours to days after exposure. Profiling injuries resulting from diagnostic radiation procedures can further characterize the nature of radiotherapy-induced skin reactions. For example, a patient with a radiation-induced skin injury resulting from a fluoroscopy procedure displayed prolonged erythema at 6–8 weeks postirradiation imaging (20). The injury during this timeframe had a distinctive mauve central area suggestive of ischemia. At 16–21 weeks later, the skin injury was depigmented with a central area of necrosis. Onset of deep necrosis with atrophic borders developed 18–21 months after exposure. In another case, a radiation oncology patient developed radiation dermatitis four weeks into the course of radiotherapy (147). The skin injury displayed erythema associated with cutaneous necrosis, pain and fever, and the patient developed a wound-based Staphylococcus aureus infection. At five weeks postirradiation, an escharotomy of the dead tissue was performed and by 7–8 weeks, the patient’s infection was resolved, and re-epithelialization was observed at the site of injury. A patient with cutaneous radiation injuries was profiled as well.19 This patient developed a skin wound that advanced from mild erythema to confluent moist desquamation by 26 days after irradiation. The wound progressed to the point of necrosis, fibrosis and telangiectasia at two years postirradiation (see similar wound in Fig. 3C and D).
FIG. 3.
Reactions observed from radiation exposure of the skin.19 Panel A: Typical mild skin injury in a radiation therapy patient. Panel B: Radiation dermatitis in a patient after a skin reaction to radiation therapy. Panels C and D: Acute ulceration in a patient who inadvertently placed an Ir-192 source in his back pocket, at 3 and 10 days, respectively, after exposure (36).
It is important to standardize terminology used by the medical and scientific communities to describe radiation skin injuries. Scoring that aligns with terminology needs to be established to allow for measurement of individual symptoms of injury across the full spectrum of skin pigments (L. Burnett). Current systems for grading skin damage vary on how they score injuries. For example, the scales differ somewhat in their grading of symptoms such as edema, blistering, desquamation and ulceration/necrosis (Table 3). These inconsistencies could best be addressed by stakeholders in the field, including clinicians, researchers, FDA product reviewers, and other government agencies. In addition to the vital human data available, animal models are tools that can be used to assess dose-dependent injury over time and across multiple skin pigments. Data from well-established animal models can be translated to better understand similar injuries in humans. One such animal model, the Yorkshire swine [presented in Session 2 (107)], was administered radiation at multiple doses using beta, orthovoltage X-ray or linear accelerator. As described above, observations and histological data show radiation dose-dependent evolution of skin pathology over time, including the diminishing, then absent, basal cell population by day 70 (107). The severity of skin reactions was assessed using a modified methodology and acute skin injury scale (148). In addition, given the fact that skin comes in many different shades, CRI studies using the red Duroc pig, a dark-skinned animal, are also important to properly assess injuries in darker skin shades (149).
Since ionizing radiation causes disruption of skin barrier function leading to trans-epidermal water loss, it was suggested that preservation of the epidermal permeability barrier function with topical treatment could reduce the negative effects of radiation dermatitis (50). Interacting molecular partners that maintain skin barrier are potential targets for development of treatments; therefore, alpha-catenin and its many molecular partners were investigated (150). Alpha-catenin sits at the junction of intercellular adhesion, coordinating activity between cells. Electron microscopy of the intercellular components of the skin shows the major cellular junctions and desmosomes (150), which are known to be adversely affected by ionizing radiation (107). For this reason, KeraStat Cream (containing purified, human-derived keratin) has been tested for its ability to manage both porcine and human skin injuries, in the hopes that the application of human-derived keratin, the main skin protein, will create an environment supportive of healing. In a large white pig model, wounds dressed with the cream showed improvement by four weeks postirradiation, and in a human skin wound, skin dressed with the cream showed less injury (as assessed by RTOG scoring) by four weeks, compared to skin treated with standard of care (L. Burnett).
Focusing on future directions, drug development for radiation-induced skin injury should include a “multi-omic” approach with biomarker pathway analysis. This is necessary to correlate animal model data with human skin biopsies after radiation oncology procedures. For example, in the large swine model of irradiated skin, metabolomic analysis revealed dose- and time-dependent changes in several metabolites not previously shown to be associated with CRI. These changes occurred in pathways reflecting protein degradation, oxidative stress, eicosanoid production, collagen matrix remodeling, mitochondrial stress, cell membrane composition and vascular disruption (107).
Alpha connexin carboxyl-terminal (ACT1) peptide to mitigate the progression of CRI
FirstString Research (Mount Pleasant, SC) is focused on developing and bringing therapies to market based on inflammation and injury-focused medical conditions. FirstString has developed a first-in-class new chemical entity called Granexin® gel that has demonstrated activity in multiple non-clinical and clinical studies (G. Ghatnekar). Granexin has been studied to enhance tissue regeneration (151), promote faster healing (152), reduce inflammation, and attenuate scarring (153, 154) in several clinical and non-clinical models of injury. FirstString has advanced Granexin into late-stage clinical trials for cutaneous radiation injury, cutaneous scarring and thermal burns (153, 155, 156). Preclinical development is also ongoing in ophthalmology indications (157). Cell-cell communication is a key aspect of injury response with cells communicating with each other to effectively bring about fast and efficient healing. The connexin 43 protein is a key component of cellular junctions that are essential for mediating cell-cell communication and inflammatory responses as well as maintaining tissue integrity. The aCT1 peptide, the active pharmaceutical ingredient in Granexin, tempers damaging inflammatory responses and helps preserve and restore the coordinated cellular activity that is compromised after injury, thus preventing the spread of the damage and acting to reboot the healing and regenerative process.
As described previously, pigs represent the gold standard to evaluate cutaneous disorders; however, not all pigs are created equal. A comparison study performed using Göttingen, Sinclair and Yorkshire pigs showed consistent development of CRI symptoms by day 35 postirradiation only in the Yorkshire strain. For this reason, the natural history of CRI in the Yorkshire pig was studied further for the determination of clinically meaningful end points, quantitative methodology for assessment of radiation injury, concept of operations, and an indication statement. Animals were exposed at eight separate circular sites on the back to a single fraction of 60 Gy with 6-MeV electrons from a LINAC. For 120 days, clinical parameters and skin healing were assessed using four scoring scales to analyze the progression of CRI phenotypes. The study used the Kumar, Erythema and Desquamation, RTOG, and an adapted VAS system (Table 3). All four metrics revealed consistent progression of CRI across all irradiated sites that followed a similar time course as that seen for CRI progression in humans (98). By day 50, the majority of sites showed clinically meaningful levels of injury, and at day 90, all irradiated sites showed clinically significant dermal necrosis and ulceration. In response to 60 Gy doses of acute ionizing radiation, Yorkshire pigs showed a controlled, reproducible full-thickness cutaneous radiation injury. A proof-of-concept pig study was performed using Granexin as the test article. Treatment of radiation sites with Granexin mitigated CRI progression and reduced injury severity over time compared to vehicle control treatment (G. Ghatnekar). The gel was applied once daily upon observation of erythema (Kumar score >1.0). In conclusion, FirstString’s novel connexin-based peptide has shown promise in modulating injury response. Their Granexin compound has successfully demonstrated activity in both Göttingen and Yorkshire pig models of CRI. These studies have laid a solid foundation to advance Granexin gel into a pivotal GLP efficacy study in the Yorkshire pig model of CRI.
Using regenerative medicine to mitigate effects of radiation combined injury
Chrysalis BioTherapeutics (Galveston, TX) has developed novel thrombin peptide regenerative drugs to address skin injuries. The company’s lead product, thrombin peptide 508 (TP508), is a clinical-stage, investigational peptide drug with demonstrated safety and activity in human clinical trials for topical and local delivery to diabetic foot ulcers and bone fractures (D. Carney). The company has been funded by the NIAID to develop TP508 as a radiation MCM, which is also under development for clinical use to protect normal tissues from damage caused by radiation therapy. Normal wound healing is a complex network of processes involving the interaction of multiple cell types such as keratinocytes, fibroblasts and endothelial cells. However, radiation-impaired wound healing is disrupted, leading to inflammation and ongoing cellular regeneration (158, 159). This type of wound healing represents a major problem for radiation therapy patients and for survivors of nuclear exposure. Chrysalis has shown that a single topical application of TP508 accelerates normal revascularization and healing of injured tissue in rats after full-thickness excisional wounding. Histological sections from wounds treated with TP508 showed more advanced healing with larger functioning blood vessels, fewer inflammatory cells and more mature granulation of tissue by day 7 (160). In clinical studies, TP508 has been shown to be effective for treating diabetic foot ulcers; TP508 shortens time to closure and doubles the number of completely healed ulcers on the foot and heel by day 60 (161). TP508 has been found to be especially active in the treatment of complex ischemic heel ulcers that are known to be the most difficult ulcers to treat effectively. Heel ulcers are more ischemic and prone to infection, leading to the highest percentage of amputation. It is believed that diabetic ulcers may be representative of ulcers resulting from radiation exposure. In one study, TP508-treated ulcers closed more completely compared to saline controls, and treatment more than doubled the rate of healing (161). TP508 stimulates cell signaling and endothelial cell nitric oxide (NO) production to activate progenitor stem cells, stimulate regeneration and revascularization, and mitigate effects of radiation. Its mode of action includes restoration of endothelial function and vascular epidermal growth factor, NO-dependent signaling, reducing ischemia and decreasing inflammation (162, 163), stimulation of progenitor stem cell proliferation (164), and increasing survival and maintenance of GI crypt integrity (165, 166). An RCI animal model was also developed by Chrysalis, in which mice received either 3 or 8 Gy of gamma radiation, followed by full-dermal excisional wounds 24 h later. Radiation exposure decreased the rate of wound closure. By day 16, nonirradiated control wounds were closed ~97% (3% open) while only 75% of irradiated wounds were closed (25% open). In contrast, TP508 treatment resulted in closure of 91% of wounds when the drug was administered 24 h after wounding. In other studies, intravenous injection of TP508 at 24 h postirradiation also restored normal healing and minimized RCI-induced increases in lethality.
Chrysalis held a pre-investigational new drug (Pre-IND) meeting, which led to the FDA’s recommendation that survival be the primary end point for the proposed animal efficacy studies and that end points related to major morbidities (e.g., wound healing) could be supportive. It was also suggested that TP508 efficacy in the setting of acute radiation syndrome be clearly shown before pursuing a combined radiation injury indication (e.g., radiation injury plus traumatic wound or burn). To date, TP508 has demonstrated a survival benefit in rodent models of hematopoietic and gastrointestinal radiation injuries and is undergoing testing in survival models in large animals (minipig/nonhuman primate) for both acute and delayed radiation sub-syndromes.
MEETING DISCUSSION
To direct comments to the areas of greatest interest to both the funding and regulatory agencies, questions were developed by the meeting planners for each session, to more readily gain expert responses from the presenters and other participants. Although conversations were held at the end of each session, content from all the discussions has been grouped together, and is further divided by topic area below.
Animal Models
Because the FDA Animal Rule is so important in the development of MCM approaches to address CRI, the development of animal models to simulate human injuries is central to moving approaches toward approval for marketing. Because human exposures could result from industrial or radiotherapy accidents, multiple animal models could be employed to generate data that could be extrapolated to clinical patients. Issues with clinical assessments of CRI are that they are often subjective, not reproducible, do not define well the depth of the skin area involved, and do not discriminate well between the types of injuries to the skin (CRI versus chronic diabetic ulcer versus thermal burn). Animal modeling may help bridge clinical scales with histopathology to make clinical assessments more quantitative and objective. To this end, there are a number of factors that must be considered when selecting the appropriate model:
- Anatomical and physiological similarity between humans and the animal species under consideration:
- The anatomy and physiology of large pig models seem to most closely resemble that of humans, with similar skin thickness, hair and sweat glands.
- The cost of a large pig and the inability to house these animals can be limiting.
- For preliminary studies, guinea pig or minipig models may be appropriate as a rodent species for testing.
- Human and animal heterogeneity in terms of skin tissue distribution and impact on radiation dose distribution:
- In humans, subcutaneous skin thickness and body fat vary as a function of age, sex and ethnicity. Fat tissue thickness can lead to wound variability, especially in the case of beta radiation, and the presence of MSCs in the adipose tissue could alter the response. Therefore, care must be used in selecting a model that minimizes these variables.
- In pig and mouse models, there can be different healing rates based on what part of the skin is irradiated. For example, in the pig, thicker dorsal skin heals differently than the thinner ventral skin. Mice also have similar skin location differences, in that radiation-induced damage can be very different in that of leg skin compared with that of ear skin.
- Proximity of the radiation exposure to bone can play a role in the extent of damage.
- Effect of skin melanization in view of possible differential radiation responses due to higher levels of melanin, as well as challenges involved in scoring erythema in pigmented skin:
- Concerning the use of a pig such as the Duroc, which is more heavily melanized, differential sensitivity to high-energy radiation may be observed due to the presence of melanin (167).
- Humane and ethical challenges encountered in these studies:
- Partial-thickness burns in animals raise concerns due to humane considerations surrounding pain.
- Full-thickness wounds are better tolerated, because the nerves are killed, and the animal is no longer sensing the pain.
- Use of a fentanyl patch should be considered.
- Because pain in animal models can be difficult to evaluate, a test or tool is needed to be better quantify the pain, especially in rodents (168).
- Euthanasia criteria must also be carefully designed and closely monitored.
- Radiation type selected for the study:
- The main issue is the penetration depth of the radiation that is being used.
- Different structures within the skin may receive different radiation doses, for example, if exposed to beta (which goes up to ~5 mm), or X rays/gamma, which penetrate farther and can therefore cause damage to deeper structures like the vasculature.
- Statistical considerations:
- Planning for the use of appropriate statistical approaches is important when embarking on any animal study. It is critical to power studies properly, and it is necessary to justify these experiments.
- Pilot studies may be a precursor to designing a fully-powered study.
- Consideration of the number of areas per animal that will be wounded:
- It is possible that radiation exposure can affect the animal’s response to an adjacent wound (via a bystander effect involving biological signaling), as there is likely a systemic component to the lesion that depends on the area of the wound as well as the dose of radiation administered.
- It is advisable to irradiate small areas that are as far away from each other as possible, while remaining in the same general area of the animal (e.g., in the pig, the back).
- For mouse studies, their small size limits the number of wounds per animal. Furthermore, since the body surface area of a wound can have a dramatic effect on the outcome in studies that use TBI combined with a skin injury, it is important to confine that exposure to ~15% (J. Kiang).
Standards of Wound Care that Could be Applied to an Animal Model
Once an appropriate animal model has been selected, it is important to determine how that model will be treated, to mimic expected human care as accurately as possible. In humans, there is a high level of variability in how the patient will be treated; however, in an animal model, the care provided needs to be standardized to achieve comparable outcomes across studies. Nonetheless, there are standard clinical practices involved in the care of wounds that could be translated into animal models:
- Maintain a clean wound bed and be diligent in looking for signs of infection, while understanding that the native cutaneous microbiome can play a role in the progression of healing.
- Remove necrotic tissues (debridement); this is a common standard of care in the clinic that is not often used in animal models (although there has been limited use in pigs) due to challenges with assessing animal pain.
- Consider antimicrobial therapy; however, given the low incidence of infections in caged rodent models, it is assumed that they are robust in their ability to fight off infection.
Keep the wound area moist with a dressing.
Assessment Methods to Evaluate Extent of Skin Injury
After decisions have been made concerning selection of an animal model and its treatment during the study, a determination of how the wound and any healing will be evaluated must also be considered. One of the most common methods to assess these end points are scoring scales (Table 3); however, no current consensus exists in research or clinical communities:
- Many researchers use the Kumar scale, although there are some challenges with the method, because CRI lesions are not homogeneous; for example:
- It is possible to have erythema and desquamation with an overlying blister.
- There have been cases where an irradiated animal with skin that appeared normal was scored as a “0” using this scale; however, after histological assessment, that skin was found to be severely damaged in the lower layers.
- There could be lesions that exhibit primarily desquamation, but with a small area of necrosis. That wound would receive a higher score that may not be representative of the whole lesion.
- Recommendation is to combine some form of visual scoring with histopathology.
- Similarly, using photography to assess skin injuries can be challenging:
- Amount of light in the room is critical when assessing erythema.
- Positioning of the animal, and the animal’s position within the room must be exactly replicated using the same camera for all images.
- Every detail must be carefully documented, to compare between photographs taken over time and between subjects.
For these reasons, a system that quantifies damage and eliminates subjectivity is needed. To address this shortfall, computer programs have been developed to enable unbiased scoring; however, a computer-learning algorithm is only as good as its training. Although there may still be systematic bias in computerized systems, these approaches could still improve on individual or group scoring.
Other methodologies that may be useful in determining the extent of injury and progression of healing, which have already been used for CRI, include the following.
Ultrasound allows for a full-thickness view of the skin, but depending on the nature of the radiation exposure, there may be other damaged tissues beneath the skin layer that will not be detected.
Infra-red imaging cameras have also been used to get a better look at deeper radiation dose injuries.
Optical coherent tomography is under development; however, this methodology may not be as reliable as a histology sample.
Fluorescein dye with a spy camera can be useful.
Laser Dopple is available, but not necessarily amenable to a mass casualty assessment.
Photography-based apps may be useful to determine if tissue is healthy or damaged in an open wound.
Thermography is a useful tool to assess local injury, which can present as elevated skin temperature (135).
CT scans and MRI (better for soft tissue than CT) have been used. MRI is good for bone and general structures, but there are no known studies of MR images of CRI or radiation dermatitis.
Assessment of the vasculature to look at long-term viability of the closure, which can be accomplished via dye injection and imaging to assess vascularization, is the gold standard for assessing vascularization clinically (i.e., routinely done pre-operatively for reconstructive surgery), but has not been used for CRI.
Other end points that are used clinically include epithelial integrity, extent of blood vessel involvement or proliferation in the dermis, depth of collagen necrosis, extent of inflammation, infection rates, adipose integrity, and pain.
Clinical Presentations
Although radiation skin injuries are not commonly encountered from a public health emergency perspective, it may be possible to leverage injuries encountered in existing clinical populations to learn more about possible assessment and treatment approaches:
Relatively few overexposures result from fluoroscopy procedures (standards limit the length of time and repeated procedures in the same area, so they are not as common).
Skin reactions from fractionated radiation therapy exposures are seen in patients irradiated for breast, lung, or head and neck cancers.
Patients undergoing combined chemotherapy and radiation protocols often have more severe skin reactions; the exposures are often fractionated, making it difficult to compare to victims of a prompt radiation exposure.
Irradiated patients may have skin injuries that are unmasked after a second radiation exposure. Patients with TBI conditioning for bone marrow transplant are more prone to developing graft versus host disease (GvHD).
After radiotherapy, it is possible to see vascular effects in patients 20–30 years later. The healed wound looks fine, but the patient develops toxicity decades later due to vascular atrophy.
Because radiation burns can result from normal tissue radiotherapy complications or some diagnostic procedures, it is informative to also study thermal burns to better understand how medical professionals assess these kinds of wounds. From a regulatory perspective, it may be appropriate to conduct therapeutic studies for radiation dermatitis in humans, but CRI studies in animals, given that it is difficult to identify clinical damage consistent with CRI outside of rare, accidental exposures.
Clinicians would appreciate products that allow for more rapid and accurate diagnosis and better assessment, especially of layers beneath the skin and other aspects of cutaneous injury that are not easily visible. Surgeons need as much objective information about the depth, breadth and severity of injury including evaluation of blood supply to understand the injury and plan resection. Histopathology, which is the gold standard for animals, cannot be easily done for human injury, and needs to be linked to human skin lesions observed with imaging modalities such as ultrasonography, thermography or MRI, or molecular signatures such as biomarkers or chromosomal abnormalities, to accurately map out the extent of a lesion. Some suggested end points used in other skin injuries such as 100% re-epithelialization, defined as complete epithelialization observed at two visits two weeks apart, may be too ambitious in the context of CRI, though this could represent an appropriate regulatory and clinical end point. It is important that durable skin stays closed, and that sufficient blood supply is available to the wound to support tissue remodeling in the years after injury. While a functional, desirable outcome for diabetic foot ulcer care may be 100% wound closure, radiation injuries are more complex, making it difficult to achieve similar outcomes. The following end points could be alternatives:
decrease in skin necrosis,
facilitation of surgical closure,
accelerating time to autograft,
cosmesis,
reduction in pain,
other parameters that affect patient quality of life.
Wound closure should still be assessed as a safety end point to ensure the treatment being studied does not interfere with or delay the wound-healing process. In the clinic, there are a few functional outcomes that can be assessed to determine if skin will remain durable or a wound will remain closed/healed, such as blood flow assessment via laser doppler. In the burn field, physicians utilize different scoring scales to assess for fibrotic outcomes such as scarring and to look for vascularization, which often utilizes the Vancouver Scar Scale (169). This assessment method uses the color and pliability of a scar to provide some indications concerning the expected duration of healing. In chronic diabetic foot ulcers, edema of the extremity must be managed for wound healing to be long-term. The inter-center FDA guidance document on burns and chronic cutaneous ulcers is an excellent resource for other potential end points (138).
It is clear that a team approach is needed to appropriately address CRI, including well-established relationships between trauma clinicians, radiation oncologists, radiation physicists, dermatologists and others. For example, in the case of radiation dermatitis, dermatologists will often be sought for treatment, but may not know that patient’s history well enough to understand the cause of the rash. Often, the presence of a grid pattern of a delineated field edge from the collimator may be the only indication of a radiation burn. It is critical to have all care providers working together to best diagnose and treat patients with suspected skin radiation injuries.
Medical Countermeasures
Medical countermeasures (MCMs) under study to address CRI have ranged from small molecules and growth factors to cellular therapies. In developing these various approaches, it is important to note that it is not reasonable to expect that a single product will be able to address the heterogeneity of the lesions observed after radiation exposure of the skin. When to initiate treatment with a MCM for CRI depends on the agent’s mechanism of action. For example:
Antioxidants might be best initiated prior to irradiation.
Anti-inflammatories could yield greatest efficacy when administered postirradiation.
For some approaches, equal efficacy has been observed whether the drug is started at erythema or moist desquamation; however, if treatment was initiated only at time of moist desquamation, with an equal outcome, an argument could be made to wait until that time in a scarce-resources setting.
Some topicals could work better if given at the time of moist desquamation because the skin would be more open to accept the drug.
Bone marrow stromal cells as mitigators of radiation fibrosis provided improvement when administration was delayed until macrophages accumulated at the site, up to 6 weeks postirradiation. It is notable that cellular approaches such as MSCs could also address intractable pain known to accompany CRI.
An understanding of the mechanism of action of the drug and the end point it will modify allow researchers to determine the appropriate time point for intervention in the process.
SUMMARY AND CONCLUSIONS
As demonstrated through the presentations and discussions held during this meeting, CRI represents damage that must be considered when discussing injuries anticipated from a radiation mass casualty incident. Development of animal models to address this damage has lagged behind those for other radiation syndromes; however, there are several approaches currently under study that utilize both small and large animals generally believed to approximate a human response to radiation exposure. Standardization of methods to assess the severity of the injury and its amelioration by treatment is also needed. It is, nonetheless, promising that several repurposed MCMs (e.g., skin wound dressings for thermal burn), or drugs for which clinical data are being gathered for another indication (e.g., diabetic foot ulcers), are undergoing testing. This approach could accelerate the clearance/approval/licensure of these MCMs. It is, therefore, important for funding agencies to continue to support basic-through-advanced development of all of these aspects of CRI.
ACKNOWLEDGMENTS
We thank the meeting speakers (Table 1) and conference attendees for providing their expertise and insight during both the presentations and discussion sessions. We would also like to acknowledge the conference moderators (Session 1: Scott Somers, NIGMS and Betsy Ballard, FDA; Session 2: Andrea DiCarlo, NIAID and Adebayo Laniyonu, FDA; Session 3: Nushin Todd, FDA and Narayan Iyer, BARDA; Session 4: Sue Jane Wang, FDA and Cynthia Chang, FDA; and Session 5: Carmen Rios, NIAID and Aaron Bandremer, BARDA). We recognize the efforts of other FDA members of the planning committee (Heather Agler, Frank Lutterodt, Lisa Skarupa, Cynthia Welsh, Kunyi Wu, and Zishan Zhao), and the strong guidance and support of Libero Marzella (FDA). Finally, we thank DAIT, NIAID colleagues (David Cassatt, Merriline Satyamitra, Lanyn Taliaferro and Thomas Winters) for their critical review of the manuscript prior to submission.
Footnotes
As per FDA nomenclature, drugs are approved, biological products are licensed, and devices are cleared.
Where pre-publication data are discussed, the first initial and the last name of the presenter who provided the information is shown in parentheses.
Any reference in this publication to any person, organization, product or service does not constitute or imply endorsement, recommendation or favoring by the U.S. Government.
Full-thickness cutaneous radiation injury is defined by the presence of an ulcer, as observed in the irradiated skin, along with the histological measures of loss of epidermis, reduced number of blood vessels, increased dermal inflammation, loss of adipose integrity and collagen necrosis in the dermis.
REFERENCES
- 1.Food and Drug Administration (FDA), Center for Drug Evaluation and Research (CDER), Center for Biologics Evaluation and Research (CBER) Product Development Under the Animal Rule. Guidance for Industry; 2015. [Google Scholar]
- 2.Barabanova A Acute radiation syndrome with cutaneous syndrome In: Ricks R, Berger ME, Ohara FM Jr., editor. Medical basis for radiation accident preparedness: The clinical care of victims. New York: Parthenon Publishing Group; 2002. [Google Scholar]
- 3.Hirsch E, Oliveira A, Browne D, et al. Consensus statement on the cutaneous radiation syndrome. In: MacVittie TJ, Weiss JF, Browne D, editors. Advances in the treatment of radiation injuries. Proceedings of the Second Consensus Development Conference on the Management of Radiation Injuries, Bethesda, MD, April 12–14, 1993 New York: Pergamon Elsevier; 1996. [Google Scholar]
- 4.Strandquist M A study of the cumulative effects of fractionated X-ray treatment based on the experience gained at Radiumhem-met with the treatment of 280 cases of carcinoma of skin and lip. Acta Radiol 1944; 55:300. [Google Scholar]
- 5.Lataillade J, Doucet C, Bey E, Carsin H, Huet C, Clairand I, et al. New approach to radiation burn treatment by dosimetry-guided surgery combined with autologous mesenchymal stem cell therapy. Regen Med 2007; 2:785–94. [DOI] [PubMed] [Google Scholar]
- 6.Rachidi W, Harfourche G, Lemaitre G, Amiot F, Vaigot P, Martin MT. Sensing radiosensitivity of human epidermal stem cells. Radiother Oncol 2007; 83:267–76. [DOI] [PubMed] [Google Scholar]
- 7.Agay D, Scherthan H, Forcheron F, Grenier N, Herodin F, Meineke V, et al. Multipotent mesenchymal stem cell grafting to treat cutaneous radiation syndrome: development of a new minipig model. Exp Hematol 2010; 38:945–56. [DOI] [PubMed] [Google Scholar]
- 8.Archambeau J, Mathieu G, Brenneis H, Thompson K, Fairchild R. The response of the skin of swine to increasing single exposures of 250-KVP X-rays. Radiat Res 1968; 36:299–326. [PubMed] [Google Scholar]
- 9.Forcheron F, Agay D, Scherthan H, Riccobono D, Herodin F, Meineke V, et al. Autologous adipocyte derived stem cells favour healing in a minipig model of cutaneous radiation syndrome. PLoS One 2012; 7:e31694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hadad I, Johnstone BH, Brabham JG, Blanton MW, Rogers PI, Fellers C, et al. Development of a porcine delayed wound-healing model and its use in testing a novel cell-based therapy. Int J Radiat Oncol Biol Phys 2010; 78:888–96. [DOI] [PubMed] [Google Scholar]
- 11.Hopewell J The skin: its structure and response to ionizing radiation. Int J Radiat Biol 1990; 57:751–73. [DOI] [PubMed] [Google Scholar]
- 12.Riccobono D, Agay D, Scherthan H, Forcheron F, Vivier M, Ballester B, et al. Application of adipocyte-derived stem cells in treatment of cutaneous radiation syndrome. Health Phys 2012; 103:120–6. [DOI] [PubMed] [Google Scholar]
- 13.Sieber V, Wells J, Rezvani M, Hopewell J. Radiation induced damage to the cells of pig hairs: a biological indicator of radiation dose and dose distribution in skin. Radiat Prot Dosimetry 1986; 16:301–6. [Google Scholar]
- 14.National Security Staff, Interagency Policy Coordination Subcommittee for Preparedness and Response to Radiological and Nuclear Threats. Planning guidance for response to a nuclear detonation. 2nd ed. Homeland Security Council Interagency Policy Coordination Subcommittee for Preparedness and Response to Radiological and Nuclear Threats; 2010. [Google Scholar]
- 15.Tsipis K Understanding nuclear weapons. London: Wildwood House; 1985. [Google Scholar]
- 16.Barss NM, Weitz RL. Reconstruction of external dose from beta radiation sources of nuclear weapon origin. Health Phys 2006; 91:379–89. [DOI] [PubMed] [Google Scholar]
- 17.Adams TG, Yeddanapudi N, Clay M, Asher J, Appler J, Casagrande R. Modeling cutaneous radiation injury from fallout. Disaster Med Public Health Prep 2019; 13:463–9. [DOI] [PubMed] [Google Scholar]
- 18.Hubbell J, Seltzer S. Tables of X-ray mass attenuation coefficients and mass energy-absorption coefficients 1 keV to 20 MeV for elements Z=1 to 92 and 48 additional substances of dosimetric interest. Gaithersburg, MD: National Institute of Standards and Technology; 1995. [Google Scholar]
- 19.Berger MJ, Coursey J, Zucker M, Chang J. ESTAR, PSTAR, and ASTAR: Computer programs for calculating stopping-power and range tables for electrons, protons, and helium ions, v1.2.3. Gaithersburg, MD: National Institute of Standards and Technology; 2005. [Google Scholar]
- 20.Balter S, Hopewell JW, Miller DL, Wagner LK, Zelefsky MJ. Fluoroscopically guided interventional procedures: a review of radiation effects on patients’ skin and hair. Radiology 2010; 254:326–41. [DOI] [PubMed] [Google Scholar]
- 21.Bolderston A, Lloyd NS, Wong RK, Holden L, Robb-Blender-man L. Supportive Care Guidelines Group of Cancer Care Ontario Program in Evidence-Based Care. The prevention and management of acute skin reactions related to radiation therapy: a systematic review and practice guideline. Support Care Cancer 2006; 14:802. [DOI] [PubMed] [Google Scholar]
- 22.Jacobson LK, Johnson MB, Dedhia RD, Niknam-Bienia S, Wong AK. Impaired wound healing after radiation therapy: A systematic review of pathogenesis and treatment. JPRAS Open 2017; 13:92–105. [Google Scholar]
- 23.Iijima S Pathology of atomic bomb casualties. Acta Pathol Jpn 1982; 32:S237–70. [PubMed] [Google Scholar]
- 24.Report of the United Nations Scientific Committee on the Effects of Atomic Radiation to the General Assembly. Annex G: Early effects in man of high doses of radiation. New York: United Nations; 1988. p. 545–65. [Google Scholar]
- 25.Kishi HS. Effects of the “special bomb”: recollections of a neurosurgeon in Hiroshima, August 8–15, 1945. Neurosurgery 2000; 47:441–46. [DOI] [PubMed] [Google Scholar]
- 26.Abella M, Molina MR, Nikolic-Hughes I, Hughes EW, Ruder-man MA. Background gamma radiation and soil activity measurements in the northern Marshall Islands. Proc Natl Acad Sci U S A 2019; 116:15425–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Guskova AK, Baranov AE, Barabanova AV, Gruzdev GP, K. PE, Nadezhina NM. Acute radiation effects in exposed persons at the Chernobyl Atomic Power Station accident. Med Radiol 1986; 477:3–18. [Google Scholar]
- 28.Potentials of polyhydroxyalkanoates for repair of skin defects In: Volova TG, Vinnik YS, Shishatskaya EI, Markelova NM, Zaikov GE, editors. Natural-based polymers for biomedical applications. 1st ed. Palm Bay, FL: Apple Academic Press; 2017. [Google Scholar]
- 29.Selezneva LG, Barabanova AV, Adamian AA, Drobysh SV, Kochergina LD, Chechetkin PI, et al. The use of kombutek 2 in treating patients with radiation damages to the skin. Med Radiol (Mosk) 1990; 35:33–4. (Article in Russian) [PubMed] [Google Scholar]
- 30.Baranov AE, Gus’kova AK, Protasova TG. [Experience in treating the victims of the accident at the Chernobyl Atomic Electric Power Station and the immediate disease outcomes. Med Radiol (Mosk). 1991; 36:29–32. (Article in Russian) [PubMed] [Google Scholar]
- 31.Barabanova AV. Significance of beta-radiation skin burns in Chernobyl patients for the theory and practice of radiopathology. Vojnosanit Pregl 2006; 63:477–80. [DOI] [PubMed] [Google Scholar]
- 32.Vasin MM, Ushakov IB, Kovtun VY. Radioprotector indralin at early and late manifestations of local radiation injuries. Vopr Onkol 2016; 62:406–12. [PubMed] [Google Scholar]
- 33.Vasin MV, Antipov VV, Chernov GA, Abramov MM, Gavriliuk DN, L’Vova TS, et al. The role of the vasoconstrictor effect in realizing the radioprotective properties of indralin in experiments on dogs. Radiats Biol Radioecol 1997; 37:46–55. (Article in Russian) [PubMed] [Google Scholar]
- 34.Vasin MV, Chernov GA, Antipov VV. Width of radiation protective effects of indralin in comparative studies using different animal species. Radiats Biol Radioecol. 1997;37(6):896–904. (Article in Russian) [PubMed] [Google Scholar]
- 35.Gusev IA, Guskova AK, Mettler FA. Medical management of radiation accidents. 2nd ed. Boca Raton, FL: CRC Press; 2001. [Google Scholar]
- 36.Barriga LE, Zaharia M, Pinillos L, Moscol A, Heredia A, Sarria G, et al. Long–term follow-up of radiation accident patients in Peru: review of two cases. Radiat Prot Dosimetry 2012; 151:652–5. [DOI] [PubMed] [Google Scholar]
- 37.International Atomic Energy Agency. The radiological accident in Lilo. Vienna, Austria: IAEA; 2000. [Google Scholar]
- 38.Jikia D Long-term follow-up of the patients injured in the Lilo radiological accident. Health Phys 2010; 98:872–5. [DOI] [PubMed] [Google Scholar]
- 39.International Atomic Energy Agency. The radiological accident in Nueva Aldea. Vienna, Austria: IAEA; 2009. [Google Scholar]
- 40.Lima CM, Lima AR, Degenhardt AL, Valverde NJ, Silva FC. Reconstructive dosimetry for cutaneous radiation syndrome. Braz J Med Biol Res 2015; 48:895–901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Jose de Lima Valverde N, Ferreira da Silva J, Tantalean OB. An update on three radiation accidents in South America. Health Phys 2010; 98:868–71. [DOI] [PubMed] [Google Scholar]
- 42.Tamarat R, Lataillade JJ, Bey E, Gourmelon P, Benderitter M. Stem cell therapy: from bench to bedside. Radiat Prot Dosimetry 2012; 151:633–9. [DOI] [PubMed] [Google Scholar]
- 43.Clairand I, Huet C, Trompier F, Bottollier-Depois JF. Physical dosimetric reconstruction of a radiological accident due to gammagraphy equipment that occurred in Dakar and Abidjan in summer 2006. Radiat Meas 2008; 43:698–703. [Google Scholar]
- 44.Bertho JM, Roy L, Souidi M, Benderitter M, Bey E, Racine R, et al. Initial evaluation and follow-up of acute radiation syndrome in two patients from the Dakar accident. Biomarkers 2009; 14:94–102. [DOI] [PubMed] [Google Scholar]
- 45.Gourmelon P, Benderitter M, Bertho JM, Huet C, Gorin NC, De Revel P. European consensus on the medical management of acute radiation syndrome and analysis of the radiation accidents in Belgium and Senegal. Health Phys 2010; 98:825–32. [DOI] [PubMed] [Google Scholar]
- 46.Zenda S, Ota Y, Tachibana H, Ogawa H, Ishii S, Hashiguchi C, et al. A prospective picture collection study for a grading atlas of radiation dermatitis for clinical trials in head-and-neck cancer patients. J Radiat Res 2016; 57:301–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Leventhal J, Young MR. Radiation dermatitis: recognition, prevention, and management. Oncology 2017; 31:885–7, 94–9. [PubMed] [Google Scholar]
- 48.Ryan JL. Ionizing radiation: the good, the bad, and the ugly. J Invest Dermatol 2012; 132:985–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Hegedus F, Mathew LM, Schwartz RA. Radiation dermatitis: an overview. Int J Dermatol 2017; 56:909–14. [DOI] [PubMed] [Google Scholar]
- 50.Schmuth M, Sztankay A, Weinlich G, Linder DM, Wimmer MA, Fritsch PO, et al. Permeability barrier function of skin exposed to ionizing radiation. Arch Dermatol 2001; 137:1019–23. [PubMed] [Google Scholar]
- 51.Lamoureux C, Gerard E, Ouhabrache N, Toukal F, Pham-Ledard A, Beylot-Barry M. A case of potential radiation recall dermatitis induced by chemotherapy, following low-dose total-skin electron beam therapy. Eur J Dermatol 2019; 29:671–2. [DOI] [PubMed] [Google Scholar]
- 52.Reichman EF. Fluoroscopy-induced radiation dermatitis. J Emerg Med 2014; 47:e117–9. [DOI] [PubMed] [Google Scholar]
- 53.Lyons AB, Harvey VM, Gusev J. Fluoroscopy-induced chronic radiation dermatitis (FICRD) after endovascular abdominal aortic aneurysm endoleak repair. JAAD Case Rep 2015; 1:403–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Wick G, Grundtman C, Mayerl C, Wimpissinger TF, Feichtinger J, Zelger B, et al. The immunology of fibrosis. Annu Rev Immunol 2013; 31:107–35. [DOI] [PubMed] [Google Scholar]
- 55.Straub JM, New J, Hamilton CD, Lominska C, Shnayder Y, Thomas SM. Radiation-induced fibrosis: mechanisms and implications for therapy. J Cancer Res Clin Oncol 2015; 141:1985–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Gremy O, Benderitter M, Linard C. Acute and persisting Th2-like immune response after fractionated colorectal gamma-irradiation. World J Gastroenterol 2008; 14:7075–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Liao W, Hei TK, Cheng SK. Radiation-induced dermatitis is mediated by IL17-expressing gammadelta T cells. Radiat Res 2017; 187:454–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Ho AY, Olm-Shipman M, Zhang Z, Siu CT, Wilgucki M, Phung A, et al. A randomized trial of mometasone furoate 0.1% to reduce high-grade acute radiation dermatitis in breast cancer patients receiving postmastectomy radiation. Int J Radiat Oncol Biol Phys 2018; 101:325–33. [DOI] [PubMed] [Google Scholar]
- 59.Delanian S, Porcher R, Balla-Mekias S, Lefaix JL. Randomized, placebo-controlled trial of combined pentoxifylline and tocopherol for regression of superficial radiation-induced fibrosis. J Clin Oncol 2003; 21:2545–50. [DOI] [PubMed] [Google Scholar]
- 60.Delanian S, Lefaix JL. Current management for late normal tissue injury: radiation-induced fibrosis and necrosis. Semin Radiat Oncol 2007; 17:99–107. [DOI] [PubMed] [Google Scholar]
- 61.Fernandez-Castro M, Martin-Gil B, Pena-Garcia I, Lopez-Vallecillo M, Garcia-Puig ME. Effectiveness of semi-permeable dressings to treat radiation-induced skin reactions. A systematic review. Eur J Cancer Care (Engl) 2017; 26. [DOI] [PubMed] [Google Scholar]
- 62.Hemati S, Asnaashari O, Sarvizadeh M, Motlagh BN, Akbari M, Tajvidi M, et al. Topical silver sulfadiazine for the prevention of acute dermatitis during irradiation for breast cancer. Support Care Cancer 2012; 20:1613–8. [DOI] [PubMed] [Google Scholar]
- 63.Lee J, Lee SW, Hong JP, Shon MW, Ryu SH, Ahn SD. Foam dressing with epidermal growth factor for severe radiation dermatitis in head and neck cancer patients. Int Wound J 2016; 13:390–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Ghasemi A, Ghashghai Z, Akbari J, Yazdani-Charati J, Salehifar E, Hosseinimehr SJ. Topical atorvastatin 1% for prevention of skin toxicity in patients receiving radiation therapy for breast cancer: a randomized, double-blind, placebo-controlled trial. Eur J Clin Pharmacol 2019; 75:171–8. [DOI] [PubMed] [Google Scholar]
- 65.Mamalis A, Siegel D, Jagdeo J. Visible red light emitting diode photobiomodulation for skin fibrosis: key molecular pathways. Curr Dermatol Rep 2016; 5:121–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Canesso MC, Vieira AT, Castro TB, Schirmer BG, Cisalpino D, Martins FS, et al. Skin wound healing is accelerated and scarless in the absence of commensal microbiota. J Immunol 2014; 193:5171–80. [DOI] [PubMed] [Google Scholar]
- 67.Esteban-Vives R, Young M, Over P, Schmelzer E, Corcos A, Ziembicki J, et al. In vitro keratinocyte expansion for cell transplantation therapy is associated with differentiation and loss of basal layer derived progenitor population. Differentiation 2015; 89:137–45. [DOI] [PubMed] [Google Scholar]
- 68.Harris PA, Leigh IM, Navsaria HA. Pre-confluent keratinocyte grafting: the future for cultured skin replacements? Burns 1998; 24:591–3. [DOI] [PubMed] [Google Scholar]
- 69.Gerlach JC, Johnen C, Ottomann C, Brautigam K, Plettig J, Belfekroun C, et al. Method for autologous single skin cell isolation for regenerative cell spray transplantation with non-cultured cells. Int J Artif Organs 2011; 34:271–9. [DOI] [PubMed] [Google Scholar]
- 70.Gerlach JC, Johnen C, McCoy E, Brautigam K, Plettig J, Corcos A. Autologous skin cell spray-transplantation for a deep dermal burn patient in an ambulant treatment room setting. Burns 2011; 37:e19–23. [DOI] [PubMed] [Google Scholar]
- 71.Esteban-Vives R, Corcos A, Choi MS, Young MT, Over P, Ziembicki J, et al. Cell-spray auto-grafting technology for deep partial-thickness burns: Problems and solutions during clinical implementation. Burns 2018; 44:549–59. [DOI] [PubMed] [Google Scholar]
- 72.Esteban-Vives R, Young MT, Ziembicki J, Corcos A, Gerlach JC. Effects of wound dressings on cultured primary keratinocytes. Burns 2016; 42:81–90. [DOI] [PubMed] [Google Scholar]
- 73.Margolis DJ, Berlin JA, Strom BL. Interobserver agreement, sensitivity, and specificity of a “healed” chronic wound. Wound Repair Regen 1996; 4:335–8. [DOI] [PubMed] [Google Scholar]
- 74.Lazarus GS, Cooper DM, Knighton DR, Percoraro RE, Rodeheaver G, Robson MC. Definitions and guidelines for assessment of wounds and evaluation of healing. Wound Repair Regen 1994; 2:165–70. [DOI] [PubMed] [Google Scholar]
- 75.Mills JL Sr., Conte MS, Armstrong DG, Pomposelli FB, Schanzer A, Sidawy AN, et al. The Society for Vascular Surgery lower extremity threatened limb classification system: risk stratification based on wound, ischemia, and foot infection (WIfI). J Vasc Surg 2014; 59:220–34 e1–2. [DOI] [PubMed] [Google Scholar]
- 76.Weaver ML, Hicks CW, Canner JK, Sherman RL, Hines KF, Mathioudakis N, et al. The Society for Vascular Surgery Wound, Ischemia, and foot Infection (WIfI) classification system predicts wound healing better than direct angiosome perfusion in diabetic foot wounds. J Vasc Surg 2018; 68:1473–81. [DOI] [PubMed] [Google Scholar]
- 77.Hicks CW, Canner JK, Mathioudakis N, Sherman R, Malas MB, Black JH 3rd, et al. The Society for Vascular Surgery Wound, Ischemia, and foot Infection (WIfI) classification independently predicts wound healing in diabetic foot ulcers. J Vasc Surg 2018; 68:1096–103. [DOI] [PubMed] [Google Scholar]
- 78.Hicks CW, Canner JK, Karagozlu H, Mathioudakis N, Sherman RL, Black JH 3rd, et al. The Society for Vascular Surgery Wound, Ischemia, and foot Infection (WIfI) classification system correlates with cost of care for diabetic foot ulcers treated in a multidisciplinary setting. J Vasc Surg 2018; 67:1455–62. [DOI] [PubMed] [Google Scholar]
- 79.Mathioudakis N, Hicks CW, Canner JK, Sherman RL, Hines KF, Lum YW, et al. The Society for Vascular Surgery Wound, Ischemia, and foot Infection (WIfI) classification system predicts wound healing but not major amputation in patients with diabetic foot ulcers treated in a multidisciplinary setting. J Vasc Surg 2017; 65:1698–705 e1. [DOI] [PubMed] [Google Scholar]
- 80.Messerschmidt O, Birkenmayer E, Bomer H, Koslowski L. Radiation sickness combined with burn. Vienna, Austria: International Atomic Energy Agency; 1970. [Google Scholar]
- 81.Wintz H Injuries from roentgen rays in deep therapy. AJR Am J Roentgenol 1923; 10:140–7. [Google Scholar]
- 82.United Nations Scientific Committee of the Effects of Atomic Radiation (UNSCEAR). Sources and effects of ionizing radiation; 2006 Report to the General Assembly with Annexes. New York: United Nations; 2006. [Google Scholar]
- 83.Ledney GD, Elliott TB. Combined injury: Factors with potential to impact radiation dose assessments. Health Phys 2010; 98:145–52. [DOI] [PubMed] [Google Scholar]
- 84.Kiang JG, Garrison BR, Burns TM, Zhai M, Dews IC, Ney PH, et al. Wound trauma alters ionizing radiation dose assessment. Cell Biosci 2012; 2:20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Kiang JG, Jiao W, Cary LH, Mog SR, Elliott TB, Pellmar TC, et al. Wound trauma increases radiation-induced mortality by activation of iNOS pathway and elevation of cytokine concentrations and bacterial infection. Radiat Res 2010; 173:319–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Kiang JG, Olabisi AO. Radiation: a poly-traumatic hit leading to multi-organ injury. Cell Biosci 2019; 9:25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Doctrow SR, Lopez A, Schock AM, Duncan NE, Jourdan MM, Olasz EB, et al. A synthetic superoxide dismutase/catalase mimetic EUK-207 mitigates radiation dermatitis and promotes wound healing in irradiated rat skin. J Invest Dermatol 2013; 133:1088–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Kiang JG, Fukumoto R. Ciprofloxacin increases survival after ionizing irradiation combined injury: gamma-H2AX formation, cytokine/chemokine, and red blood cells. Health Phys 2014; 106:720–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Kiang JG, Ledney GD. Skin injuries reduce survival and modulate corticosterone, C-reactive protein, complement component 3, IgM, and prostagladin E2 after whole-body-reactor-produced mixed field irradiation. Oxid Med Cell Longev 2013; 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Rodgers KE, Tan A, Kim L, Espinoza T, Meeks C, Johnston W, et al. Development of a guinea pig cutaneous radiation injury model using low penetrating X-rays. Int J Radiat Biol 2016; 92:434–43. [DOI] [PubMed] [Google Scholar]
- 91.Todo H Transdermal permeation of drugs in various animal species. Pharmaceutics 2017; 9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Nicolai JP, Goris RJ. A guinea-pig model in burn research. Eur Surg Res 1980; 12:22–9. [DOI] [PubMed] [Google Scholar]
- 93.Zawacki BE, Jones RJ. Standard depth burns in the rat: the importance of the hair growth cycle. Br J Plast Surg 1967; 20:347–54. [DOI] [PubMed] [Google Scholar]
- 94.Gross J, Farinelli W, Sadow P, Anderson R, Bruns R. On the mechanism of skin wound “contraction”: A granulation tissue “knockout” with a normal phenotype. Proc Natl Acad Sci U S A 1995; 92:5982–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Bjornson AB, Bjornson HS, Knippenberg RW, Cardone JS. Temporal relationships among immunologic alterations in a guinea pig model of thermal injury. J Infect Dis 1986; 153:1098–107. [DOI] [PubMed] [Google Scholar]
- 96.Kumar S, Kolozsvary A, Kohl R, Lu M, Brown S, Kim JH. Radiation-induced skin injury in the animal model of scleroderma: implications for post-radiotherapy fibrosis. Radiat Oncol 2008; 3:40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Hoeller U, Tribius S, Kuhlmey A, Grader K, Fehlauer F, Alberti W. Increasing the rate of late toxicity by changing the score? A comparison of RTOG/EORTC and LENT/SOMA scores. Int J Radiat Oncol Biol Phys 2003; 55:1013–8. [DOI] [PubMed] [Google Scholar]
- 98.Schauer DA, Coursey BM, Dick CE, McLaughlin WL, Puhl JM, Desrosiers MF, et al. A radiation accident at an industrial accelerator facility. Health Phys 1993; 65:131–40. [DOI] [PubMed] [Google Scholar]
- 99.Babaee N, Mansourian A, Momen-Heravi F, Moghadamnia A, Momen-Beitollahi J. The efficacy of a paste containing Myrtus communis (Myrtle) in the management of recurrent aphthous stomatitis: a randomized controlled trial. Clin Oral Investig 2010; 14:65–70. [DOI] [PubMed] [Google Scholar]
- 100.Szepietowski JC, Sikora M, Kusztal M, Salomon J, Magott M, Szepietowski T. Uremic pruritus: a clinical study of maintenance hemodialysis patients. J Dermatol 2002; 29:621–7. [DOI] [PubMed] [Google Scholar]
- 101.Anscher MS. Targeting the TGF-beta1 pathway to prevent normal tissue injury after cancer therapy. Oncologist 2010; 15:350–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Meyer W, Schwarz R, Neurand K. The skin of domestic mammals as a model for the human skin, with special reference to the domestic pig. Curr Probl Dermatol 1978; 7:39–52. [DOI] [PubMed] [Google Scholar]
- 103.Herron AJ. Pigs as dermatologic models of human skin disease 60th Annual Meeting of the American College of Veterinary Pathologists; Monterey, CA: International Veterinary Information Service; 2009. [Google Scholar]
- 104.Peel DM, Hopewell JW, Wells J, Charles MW. Nonstochastic effects of different energy beta emitters on pig skin. Radiat Res 1984; 99:372–82. [PubMed] [Google Scholar]
- 105.Peel DM, Hopewell JW, Wells J, Charles MW. Late non-stochastic changes in pig skin after beta irradiation. Radiat Res 1985; 101:491–6. [PubMed] [Google Scholar]
- 106.Dorand JE, Burnett LR, Tytell M, Bourland JD. A Sr-90 irradiation device for the study of cutaneous radiation injury. Med Phys 2014; 41:493. [Google Scholar]
- 107.Burnett LR, Gabard AR, Robinson M, Bourland JD, Dorand JE, Dozier S, et al. Biomolecular analysis of beta dose-dependent cutaneous radiation injury in a porcine model. Radiat Res 2019; 192:145–58. [DOI] [PubMed] [Google Scholar]
- 108.Fuchs E Skin stem cells: rising to the surface. J Cell Biol 2008;180:273–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Jourdan MM, Lopez A, Olasz EB, Duncan NE, Demara M, Kittipongdaja W, et al. Laminin 332 deposition is diminished in irradiated skin in an animal model of combined radiation and wound skin injury. Radiat Res 2011; 176:636–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Horton JA, Li F, Chung EJ, Hudak K, White A, Krausz K, et al. Quercetin inhibits radiation-induced skin fibrosis. Radiat Res 2013; 180:205–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.van Kilsdonk JW, van den Bogaard EH, Jansen PA, Bos C, Bergers M, Schalkwijk J. An in vitro wound healing model for evaluation of dermal substitutes. Wound Repair Regen 2013; 21:890–6. [DOI] [PubMed] [Google Scholar]
- 112.Horton JA, Chung EJ, Hudak KE, Sowers A, Thetford A, White AO, et al. Inhibition of radiation-induced skin fibrosis with imatinib. Int J Radiat Biol 2013; 89:162–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Bernier J, Russi EG, Homey B, Merlano MC, Mesia R, Peyrade F, et al. Management of radiation dermatitis in patients receiving cetuximab and radiotherapy for locally advanced squamous cell carcinoma of the head and neck: proposals for a revised grading system and consensus management guidelines. Ann Oncol 2011; 22:2191–200. [DOI] [PubMed] [Google Scholar]
- 114.Abaci HE, Coffman A, Doucet Y, Chen J, Jackow J, Wang E, et al. Tissue engineering of human hair follicles using a biomimetic developmental approach. Nat Commun 2018; 9:5301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Jayachandran M, Rodriguez S, Solis E, Lei J, Godavarty A. Critical review of noninvasive optical technologies for wound imaging. Adv Wound Care 2016; 5:349–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Fowler JF, Bewley DK, Morgan RL, Silvester JA, Alper T, Hornsey S. Dose-effect relationships for radiation damage to organized tissues. Nature 1963; 199:253–5. [DOI] [PubMed] [Google Scholar]
- 117.Douglas BG, Fowler JF. The effect of multiple small doses of X rays on skin reactions in the mouse and a basic interpretation. Radiat Res 1976; 66:401–26. [PubMed] [Google Scholar]
- 118.Withers HR. The dose-response relationship for epithelial cells of skin. Radiology 1966; 86:1110–1. [DOI] [PubMed] [Google Scholar]
- 119.Gurtner GC, Werner S, Barrandon Y, Longaker MT. Wound repair and regeneration. Nature 2008; 453:314–21. [DOI] [PubMed] [Google Scholar]
- 120.Vegesna V, McBride WH, Taylor JM, Withers HR. Effect of low-dose radiation on mouse dermal tissue using wound strength as an endpoint. Int J Radiat Biol 1997; 72:645–52. [DOI] [PubMed] [Google Scholar]
- 121.Vegesna V, McBride WH, Taylor JM, Withers HR. The effect of interleukin-1 beta or transforming growth factor-beta on radiation-impaired murine skin wound healing. J Surg Res 1995; 59:699–704. [DOI] [PubMed] [Google Scholar]
- 122.Vegesna V, Withers HR, Holly FE, McBride WH. The effect of local and systemic irradiation on impairment of wound healing in mice. Radiat Res 1993; 135:431–3. [PubMed] [Google Scholar]
- 123.Xie MW, Gorodetsky R, Micewicz ED, Mackenzie NC, Gaber-man E, Levdansky L, et al. Marrow-derived stromal cell delivery on fibrin microbeads can correct radiation-induced wound-healing deficits. J Invest Dermatol 2013; 133:553–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Vegesna V, McBride WH, Withers HR. Postoperative irradiation impairs or enhances wound strength depending on time of administration. Radiat Res 1995; 143:224–8. [PubMed] [Google Scholar]
- 125.Escuin-Ordinas H, Li S, Xie MW, Sun L, Hugo W, Huang RR, et al. Cutaneous wound healing through paradoxical MAPK activation by BRAF inhibitors. Nat Commun 2016; 7:12348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Fliedner TM. Medical management of radiation accidents-manual on the acute radiation syndrome. London: British Institute of Radiology; 2009. [Google Scholar]
- 127.Fliedner TM, Powles R, Sirohi B, Niederwieser D. European Group for Blood Marrow Transplantation Nuclear Accident Committee. Radiologic and nuclear events: the METREPOL severity of effect grading system. Blood 2008; 111:5757–8. [DOI] [PubMed] [Google Scholar]
- 128.Waselenko JK, MacVittie TJ, Blakely WF, Pesik N, Wiley AL, Dickerson WE, et al. Medical management of the acute radiation syndrome: recommendations of the Strategic National Stockpile Radiation Working Group. Ann Intern Med 2004; 140:1037–51. [DOI] [PubMed] [Google Scholar]
- 129.Dainiak N, Gent RN, Carr Z, Schneider R, Bader J, Buglova E, et al. Literature review and global consensus on management of acute radiation syndrome affecting nonhematopoietic organ systems. Disaster Med Public Health Prep 2011; 5:183–201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Iddins CJ, Cohen SR, Goans RE, Wanat R, Jenkins M, Christensen DM, et al. Case report: Industrial X-ray injury treated with non-cultured autologous adipose-derived stromal vascular fraction (SVF). Health Phys 2016; 111:112–6. [DOI] [PubMed] [Google Scholar]
- 131.Nathwani AC, Down JF, Goldstone J, Yassin J, Dargan PI, Virchis A, et al. Polonium-210 poisoning: a first-hand account. Lancet 2016; 388:1075–80. [DOI] [PubMed] [Google Scholar]
- 132.Sugarman SL, Findley WM, Toohey RE, Dainiak N. Rapid response, dose assessment, and clinical management of a plutonium-contaminated puncture wound. Health Phys 2018; 115:57–64. [DOI] [PubMed] [Google Scholar]
- 133.Glasstone S, Dolan PJ, United States Department of Defense, United States Department of Energy, United States. Defense Atomic Support Agency The effects of nuclear weapons. 3d ed. Washington, DC: U.S. Dept. of Defense; 1977. [Google Scholar]
- 134.National Research Council (US), Committee on Fire Research, Office of Civil Defense. Mass burns: Proceedings of a workshop, 13–14 March 1968 In: Walter CW, Phillips AW, editors. Washington, DC: National Academy of Sciences; 1969. p. 248. [Google Scholar]
- 135.Goans R, Iddins C, Christensen D. Ultrasound and thermography for diagnosis of extent and magnitude of acute local radiation injury (LRI). Proceedings of the 5th International REAC/TS Symposium: The Medical Basis for Radiation Accident Preparedness and the Biodosimetry Workshop Oak Ridge, TN: REAC/TS; 2013. [Google Scholar]
- 136.New drug and biological drug products; evidence needed to demonstrate effectiveness of new drugs when human efficacy studies are not ethical or feasible. Final rule. Fed Regist 2002; 67:37988–98. [PubMed] [Google Scholar]
- 137.U.S. Department of Health and Human Services, Food and Drug Administration, Center for Drug Evaluation and Research (CDER), Center for Biologics Evaluation and Research (CBER), Center for Devices and Radiological Health (CDRH). Guidance for industry. Chronic cutaneous ulcer and burn wounds–developing products for treatment. Rockville, MD: Food and Drug Administration; 2006. [Google Scholar]
- 138.Willard-Mack C, Ramani T, Auletta C. Dermatotoxicology: Safety evaluation of topical products in minipigs: Study designs and practical considerations. Toxicol Pathol 2016; 44:382–90. [DOI] [PubMed] [Google Scholar]
- 139.DiCarlo AL, Tamarat R, Rios CI, Benderitter M, Czarniecki CW, Allio TC, et al. Cellular therapies for treatment of radiation injury: Report from a NIH/NIAID and IRSN workshop. Radiat Res 2017; 188:e54–e75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Ebrahimian TG, Pouzoulet F, Squiban C, Buard V, Andre M, Cousin B, et al. Cell therapy based on adipose tissue-derived stromal cells promotes physiological and pathological wound healing. Arterioscler Thromb Vasc Biol 2009; 29:503–10. [DOI] [PubMed] [Google Scholar]
- 141.Holler V, Buard V, Roque T, Squiban C, Benderitter M, Flamant S, et al. Early and late protective effect of bone marrow mononuclear cell transplantation on radiation-induced vascular dysfunction and skin lesions. Cell Transplant 2019; 28:116–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Anderson HC, Mulhall D, Garimella R. Role of extracellular membrane vesicles in the pathogenesis of various diseases, including cancer, renal diseases, atherosclerosis, and arthritis. Lab Invest 2010; 90:1549–57. [DOI] [PubMed] [Google Scholar]
- 143.Thery C, Gho YS, Quesenberry P. Journal of extracellular vesicles: the seven year itch! J Extracell Vesicles 2019; 8:1654729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Wen S, Dooner M, Papa E, Del Tatto M, Pereira M, Borgovan T, et al. Biodistribution of mesenchymal stem cell-derived extracellular vesicles in a radiation injury bone marrow murine model. Int J Mol Sci 2019; 20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Szatmari T, Hargitai R, Safrany G, Lumniczky K. Extracellular vesicles in modifying the effects of ionizing radiation. Int J Mol Sci 2019; 20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Flamant S, Tamarat R. Extracellular vesicles and vascular injury: New insights for radiation exposure. Radiat Res 2016; 186:203–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Martella S, Rietjens M, Lohsiriwat V, Lazzari R, Vavassori A, Jereczek B, et al. Acute radiation dermatitis in breast cancer: topical therapy with vitamin E acetate in lipophilic gel base. Ecancermedicalscience 2010; 4:190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Dion MW, Hussey DH, Osborne JW. The effect of pentoxifylline on early and late radiation injury following fractionated irradiation in C3H mice. Int J Radiat Oncol Biol Phys 1989; 17:101–7. [DOI] [PubMed] [Google Scholar]
- 149.Zhu KQ, Engrav LH, Gibran NS, Cole JK, Matsumura H, Piepkorn M, et al. The female, red Duroc pig as an animal model of hypertrophic scarring and the potential role of the cones of skin. Burns 2003; 29:649–64. [DOI] [PubMed] [Google Scholar]
- 150.Kobielak A, Fuchs E. Alpha-catenin: at the junction of intercellular adhesion and actin dynamics. Nat Rev Mol Cell Biol 2004; 5:614–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Ghatnekar GS, O’Quinn MP, Jourdan LJ, Gurjarpadhye AA, Draughn RL, Gourdie RG. Connexin43 carboxyl-terminal peptides reduce scar progenitor and promote regenerative healing following skin wounding. Regen Med 2009; 4:205–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Montgomery J, Ghatnekar GS, Grek CL, Moyer KE, Gourdie RG. Connexin 43-based therapeutics for dermal wound healing. Int J Mol Sci 2018; 19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Rhett JM, Ghatnekar GS, Palatinus JA, O’Quinn M, Yost MJ, Gourdie RG. Novel therapies for scar reduction and regenerative healing of skin wounds. Trends Biotechnol 2008; 26:173–80. [DOI] [PubMed] [Google Scholar]
- 154.Grek CL, Montgomery J, Sharma M, Ravi A, Rajkumar JS, Moyer KE, et al. A multicenter randomized controlled trial evaluating a Cx43-mimetic peptide in cutaneous scarring. J Invest Dermatol 2017; 137:620–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Grek CL, Prasad GM, Viswanathan V, Armstrong DG, Gourdie RG, Ghatnekar GS. Topical administration of a connexin43-based peptide augments healing of chronic neuropathic diabetic foot ulcers: A multicenter, randomized trial. Wound Repair Regen 2015; 23:203–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Ghatnekar GS, Grek CL, Armstrong DG, Desai SC, Gourdie RG. The effect of a connexin43-based peptide on the healing of chronic venous leg ulcers: a multicenter, randomized trial. J Invest Dermatol 2015; 135:289–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Moore K, Bryant ZJ, Ghatnekar G, Singh UP, Gourdie RG, Potts JD. A synthetic connexin 43 mimetic peptide augments corneal wound healing. Exp Eye Res 2013; 115:178–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Hunt TK. The physiology of wound healing. Ann Emerg Med 1988; 17:1265–73. [DOI] [PubMed] [Google Scholar]
- 159.Haubner F, Ohmann E, Pohl F, Strutz J, Gassner HG. Wound healing after radiation therapy: Review of the literature. Radiat Oncol 2012; 7:162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Stiernberg J, Norfleet AM, Redin WR, Warner WS, Fritz RR, Carney DH. Acceleration of full-thickness wound healing in normal rats by the synthetic thrombin peptide, TP508. Wound Repair Regen 2000; 8:204–15. [DOI] [PubMed] [Google Scholar]
- 161.Fife C, Mader JT, Stone J, Brill L, Satterfield K, Norfleet A, et al. Thrombin peptide Chrysalin stimulates healing of diabetic foot ulcers in a placebo-controlled phase I/II study. Wound Repair Regen 2007; 15:23–34. [DOI] [PubMed] [Google Scholar]
- 162.Olszewska-Pazdrak B, Hart-Vantassell A, Carney DH. Thrombin peptide TP508 stimulates rapid nitric oxide production in human endothelial cells. J Vasc Res 2010; 47:203–13. [DOI] [PubMed] [Google Scholar]
- 163.Olszewska-Pazdrak B, Carney DH. Systemic administration of thrombin peptide TP508 enhances VEGF-stimulated angiogenesis and attenuates effects of chronic hypoxia. J Vasc Res 2013; 50:186–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Freyberg S, Song YH, Muehlberg F, Alt E. Thrombin peptide (TP508) promotes adipose tissue-derived stem cell proliferation via PI3 kinase/Akt pathway. J Vasc Res 2009; 46:98–102. [DOI] [PubMed] [Google Scholar]
- 165.Olszewska-Pazdrak B, McVicar SD, Rayavara K, Moya SM, Kantara C, Gammarano C, et al. Nuclear countermeasure activity of TP508 linked to restoration of endothelial function and acceleration of DNA repair. Radiat Res 2016; 186:162–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Kantara C, Moya SM, Houchen CW, Umar S, Ullrich RL, Singh P, et al. Novel regenerative peptide TP508 mitigates radiation-induced gastrointestinal damage by activating stem cells and preserving crypt integrity. Lab Invest 2015; 95:1222–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Ryan JL, Bole C, Hickok JT, Figueroa-Moseley C, Colman L, Khanna RC, et al. Post-treatment skin reactions reported by cancer patients differ by race, not by treatment or expectations. Br J Cancer 2007; 97:14–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Foley PL, Kendall LV, Turner PV. Clinical management of pain in rodents. Comp Med 2019; 69:468–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Baryza MJ, Baryza GA. The Vancouver Scar Scale: an administration tool and its interrater reliability. J Burn Care Rehabil 1995; 16:535–8. [DOI] [PubMed] [Google Scholar]
- 170.Laver LA, Armstrong DG, Harkless LB. Classification of diabetic foot wounds. J Foot Ankle Surg 1996; 35:528031. [DOI] [PubMed] [Google Scholar]