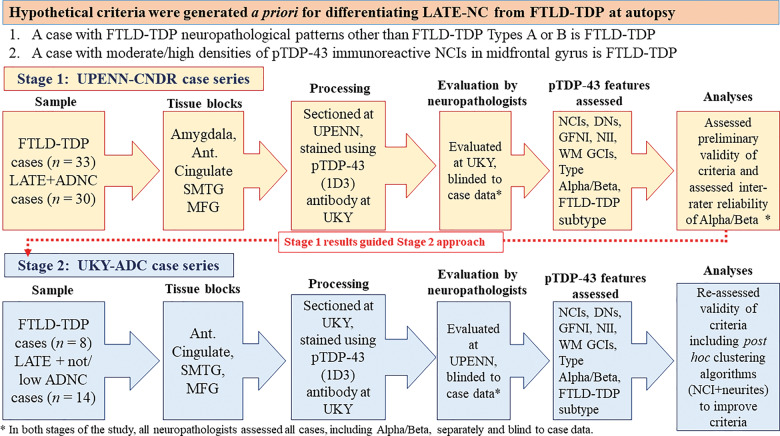
Figure 1.
Overall study design. Before grading the cases, hypothetical criteria were developed for differentiating LATE-NC from FTLD-TDP. These criteria were based on two assumptions: (i) a pattern of TDP-43 immunohistochemical staining interpreted to represent FTLD-TDP types C, D, or E was indicative of FTLD-TDP, not compatible with LATE-NC; and (ii) if the density of TDP-43 immunoreactive neuronal cytoplasmic inclusions (NCIs) was moderate or high in frontal cortex, it also was indicative of FTLD-TDP rather than LATE-NC. Next, we followed a two-stage study design. The first cases series, from University of Pennsylvania (UPENN), consisted of n = 33 cases with FTLD-TDP, and n = 30 cases with relatively severe LATE-NC, the large majority with co-morbid ADNC. Paraffin sections from amygdala, anterior cingulate, superior and middle temporal gyrus, and middle frontal gyrus were selected for the study. The sections were stained for phospho-TDP-43 at University of Kentucky (UKY) and TDP-43 pathology was evaluated by two UKY neuropathologists, applying the ad hoc criteria for differential diagnosis of LATE-NC or FTLD-TDP. Next, a separate cohort from UKY was selected, comprising n = 8 cases with FTLD-TDP and n = 14 cases with relatively severe LATE-NC, lacking co-morbid ADNC. These sections were immunostained for phospho-TDP-43 at UKY and TDP-43 pathology was evaluated by two UPENN neuropathologists, applying the same ad hoc criteria for differential diagnosis of LATE-NC or FTLD-TDP except also including ropy dystrophic neurites in the analyses. Ant Cingulate = anterior cingulate; DN = various types of TDP-43 immunoreactive dystrophic neurites; GFNI = granulofilamentous neuronal inclusions; NII = neuronal intranuclear inclusions; MFG = middle frontal gyrus; SMTG = superior and middle temporal gyri; WM GCI = white matter glial cytoplasmic inclusions.