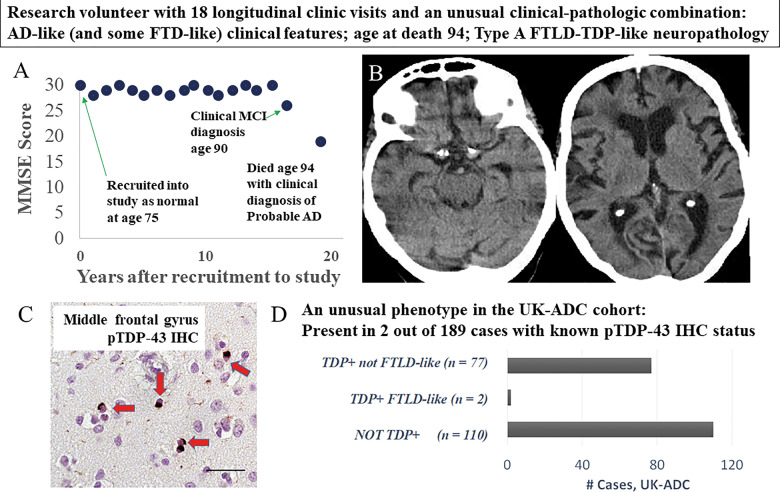
Figure 4.
Detailed information on a presumed LATE-NC research subject with an unusual clinical-pathological combination of clinical features. Clinical-pathological features included Alzheimer’s disease- and FTD-associated signs and symptoms, and neuropathology that was similar to FTLD-TDP type A. Changes in global cognitive status over the course of 20 years on study, operationalized by longitudinal MMSE scores at 18 successive clinic visits, are presented in A. Mild cognitive impairment (MCI) was diagnosed at age 90 and a final probable Alzheimer’s disease (AD) diagnosis was made at age 94, within a year of death. Although the overall clinical picture was compatible with Alzheimer’s disease, FTD-like symptoms were noted (including disinhibition and disorders in appetite and language), particularly in the final 5 years of life (Supplementary Table 11). A CT scan at age 90 when MCI was diagnosed (B) revealed frontal and temporal atrophy. In terms of genetic findings, this subject’s APOE allele status was ε2/ε3, homozygous for the TMEM106B risk allele (rs1990622 status TT), homozygous for the ABCC9 risk allele (rs704180 status AA), and homozygous for the non-risk GRN allele (rs5848 status CC). At autopsy, neuropathology (C) revealed a moderate number of neuronal cytoplasmic inclusions (red arrows) and dystrophic neurites across multiple cortical areas including the middle frontal gyrus. Scale bar = 50 µm. There was also hippocampal sclerosis pathology, but virtually no brain amyloid-β (not shown). Notably, whereas a quarter of cases from this community-based cohort had LATE-NC but lacked severe ADNC, only 2/79 of the UK-ADC cases with TDP-43 pathology had moderately severe frontal cortex TDP-43 proteinopathy (D).