Main Text
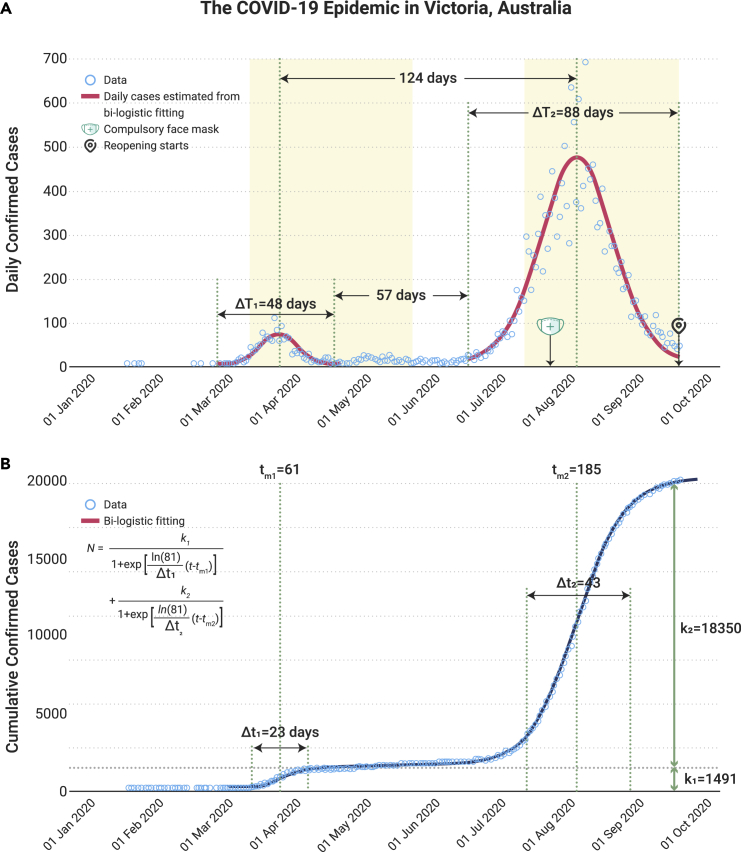
By 24 September 2020, the SARS-COV-2 epidemic had led to a total of 26,983 infections and 861 deaths in Australia, resulting in a significant disease burden on its health care system and disruption to its economy. The State of Victoria is the most severely affected Australian state and accounts for 74.5% of all infections and 89.7% deaths in Australia. Controlling the epidemic in Victoria is critical to the impact of the national epidemic. In response to the first outbreak of the epidemic, Victoria declared a state of emergency on 16 March and implemented stage 2 restrictions from 25 March to 25 May (first lockdown) with restrictions on major events, traveling, and social contacts (Figure 1A). In contrast, much stricter stage 3 and subsequent stage 4 (second lockdown) restrictions were implemented in metropolitan Melbourne and regional Victoria between the 9 July and 13 September in response to a substantially larger second outbreak since late June. The restriction measures have been effective, and the epidemic has seen a major decline from 500 to 700 cases/day in early August to 30–50 cases/day in early September. In preparation for reopening the economy, the Victorian government declared a COVID-19 roadmap for reopening on 9 September.1 In brief, the reopening plan for metro Melbourne requires the city to maintain a consistently declining trend of the epidemic, with the ease of restrictions in proportion to the number of the daily confirmed cases. The restrictions are less stringent for regional Victoria. The plan envisions complete elimination of the virus for 28 days state-wide before Victoria is allowed to return to a “COVID normal” scenario.
Figure 1.
The Number of Cumulative Confirmed Cases Was Calibrated to a Bi-logistic Function, Which Was Used to Model Biologic Patterns with Two Growth Phases
The details of the bi-logistic function have been documented previously by Meyer et al.2 The fitting of the bi-logistic function with six parameters was conducted on https://logletlab.com/. The parameters K1 (1,491) and K2 (18,350) represent the asymptotic values that bound the function and therefore specify the level at which the epidemic saturates; tm1 (29 March) and tm2 (31 July) represent the midpoint of the growth of the two epidemics and hence the peak of the two outbreaks; Δt1 (23 days) and Δt2 (43 days) are the time intervals required for the epidemics to grow from 10% to 90% of the saturation level, as defined by the bi-logarithmic function; in contrast, we defined the duration of the epidemics ΔT1 (48 days) and ΔT2 (88 days) as the length of time required for the epidemic to grow from 1% to 99% of the saturation level. The first lockdown period was between 16 March and 25 May 2020 (the State of Emergency was declared on 16 March and Stage 2 restrictions were in place between 25 March and 25 May). The second lockdown period was between 9 July and 13 September (9 July to 20 August, stage 3 for all Victoria; 21 August to 13 September, stage 4 for metro Melbourne and stage 3 for regional Victoria). Compulsory use of face masks in public spaces was implemented on 23 July. The first step of the COVID-19 Roadmap for reopening was initiated on 14 September with most of the stage 4 restrictions remaining.
We identified several key characteristics of the COVID-19 epidemic in Victoria, based on a simple bi-logistic model of growth2 on the cumulative number of confirmed COVID-19 cases in the state (Figure 1B). First, the second outbreak (estimated to saturate at 19,842 cases; Figure 1B) is significantly greater than the first outbreak (saturate at 1,491 cases), and accounts for >90% of all reported COVID-19 cases in Victoria. Second, the duration of the second outbreak (17 June to 13 September, 88 days) was almost double that of the first outbreak (5 March to 22 April, 48 days). Third, the peak of the 2 outbreaks is approximately 4 months (124 days) apart, whereas the duration between the end of the first outbreak and the beginning of the second outbreak is 57 days. The large separation between the 2 outbreaks indicates that they are independent of each other. The 57-day duration between the 2 outbreaks is a period of low-level transmission, with the number of new confirmed case averaging at 8 (0–21) cases per day. Fourth, the first lockdown was initiated on 16 March with 17 confirmed cases, whereas the second lockdown was initiated on 9 July with a much greater number of confirmed cases (143) on that day.
Achieving complete elimination of COVID-19 in Victoria, as recommended in the Roadmap, may face challenges if the pattern for the later part of the second outbreak follows what happened with the first. Our analysis demonstrates a period of nearly 2 months with low transmission following the first outbreak in Victoria. This persistent low-level transmission may represent a scenario where limited community transmission was contained by a combination of interventions including rapid screening, contact tracing, and isolation of infected individuals and those in close contact. This balance was later broken when transmission entered a population, and workplaces and large families gatherings led to a large surge in positive cases that overwhelmed the combination of interventions. As the number of cases continues to decline, the epidemic trend in Victoria may experience a similar period of low transmission during the reopening. According to the Roadmap, the threshold of daily confirmed cases needs to be less than five new cases state-wide to enable the curfew to be lifted, stay home requirements and intrastate travel by 26 October (from step 2 to step 3 of the Roadmap). To achieve this lower threshold in the specified time period, the government will need to suppress the epidemic more quickly than in the previous low-transmission period.
Complete elimination in Victoria would also necessarily require other Australian states to adopt the same target. Unless all Australian states are completely free of the virus or the country's state and national borders remained closed, occasional “seeding” due to imported cases from affected areas will be inevitable. Both China and New Zealand appeared to have largely “eliminated” the virus for an extensive period, yet sporadic outbreaks occurred.3,4 However, with early, localized, and strong measures, these outbreaks were quickly controlled. In Victoria, living with the virus at a very low endemic level as some other Australian states may be an alternative until an effective vaccine becomes available to the majority of its population.5 However, if this approach is taken, then certain measures must continue to mitigate the risk of outbreaks in addition to the combination of interventions discussed above.
We recommend 2 measures that are potentially important for the COVID-19 reopening in Victoria. First, an early epidemic alarm mechanism based on the number of daily confirmed cases should be established. The fact that the first lockdown was implemented when the daily confirmed cases were as low as 17 cases (on 16 March) compared with 143 cases (on 9 July) at the beginning of the second lockdown is likely to be why the epidemic was ten times smaller in the first outbreak. Consistent with this, a recent study indicated that in the early stage of the epidemic, a threshold of 30 confirmed cases might represent a threshold for epidemic conversion, where the epidemic switches from a slow-growing phase to a fast-growing phase.6 Second, persistent face mask usage inside and where social distancing is not possible should remain a key public intervention strategy until a vaccine is available. In Victoria, compulsory face mask use in public space was not in place until 23 July, when the community transmission was already close to its peak with 300–500 cases confirmed daily. This was despite the fact that more than 63 countries and regions had already adopted this policy by then7 and the World Health Organization recommended their use based on accumulating evidence on the protective effectiveness of face masks against COVID-19 transmission.8 Further evidence has shown that at least 70% face mask use is necessary to prevent a further outbreak if social interaction is to return to the pre-epidemic level.9,10 Until an effective vaccine becomes available, maintaining a high level of face mask use in addition to some ongoing social distancing restrictions such as COVID-safe workplaces and limiting the size of family gatherings should be an effective and economically friendly strategy to minimize the risk of further major outbreaks.
Acknowledgments
L.Z. is supported by the National Natural Science Foundation of China (grant number: 81950410639); Outstanding Young Scholars Support Program (grant number: 3111500001); Xi’an Jiaotong University Basic Research and Profession Grant (grant number: xtr022019003, xzy032020032); Epidemiology modeling and risk assessment (grant number: 20200344); and Xi'an Jiaotong University Young Scholar Support Grant (grant number: YX6J004).
Contributor Information
Lei Zhang, Email: lei.zhang1@monash.edu.
Guihua Zhuang, Email: zhuanggh@mail.xjtu.edu.cn.
References
- 1.State Government of Victoria Coronavirus (COVID-19) roadmap to reopening. 2020. https://www.vic.gov.au/coronavirus-covid-19-restrictions-roadmaps
- 2.Meyer P. Bi-logistic growth. Technol. Forecast. Social Change. 1994;47:89–102. [Google Scholar]
- 3.Blakely T., Thompson J., Carvalho N., et al. The probability of the 6-week lockdown in Victoria (commencing 9th July 2020) achieving elimination of community transmission of SARS-CoV-2. Med. J. Aust. 2020 doi: 10.5694/mja2.51157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.National Health Commission of the People’s Republic of China China’s risk of COVID-19 cluster infections caused by sporadic cases cannot be ignored: official. 2020. https://www.chinanews.com/gn/2020/05-13/9183211.shtml
- 5.Thanh Le T., Andreadakis Z., Kumar A., et al. The COVID-19 vaccine development landscape. Nat. Rev. Drug Discov. 2020;19:305–306. doi: 10.1038/d41573-020-00073-5. [DOI] [PubMed] [Google Scholar]
- 6.Zhang L., Tao Y., Wang J., et al. Early characteristics of the COVID-19 outbreak predict the subsequent epidemic scope. Int. J. Infect Dis. 2020;97:219–224. doi: 10.1016/j.ijid.2020.05.122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zhang L., Tao Y., Shen M., et al. Can self-imposed prevention measures mitigate the COVID-19 epidemic? PLoS Med. 2020;17:e1003240. doi: 10.1371/journal.pmed.1003240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chu D.K., Akl E.A., Duda S., et al. Physical distancing, face masks, and eye protection to prevent person-to-person transmission of SARS-CoV-2 and COVID-19: a systematic review and meta-analysis. Lancet. 2020;395:1973–1987. doi: 10.1016/S0140-6736(20)31142-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zhang L., Shen M., Ma X., et al. What is required to prevent a second major outbreak of SARS-CoV-2 upon lifting the quarantine of Wuhan city, China. Innovation. 2020;1:100006. doi: 10.1016/j.xinn.2020.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Shen M., Peng Z., Xiao Y., et al. Modelling the epidemic trend of the 2019 novel coronavirus outbreak in China. The Innovation. In press. 2020 doi: 10.1016/j.xinn.2020.100048. [DOI] [PMC free article] [PubMed] [Google Scholar]