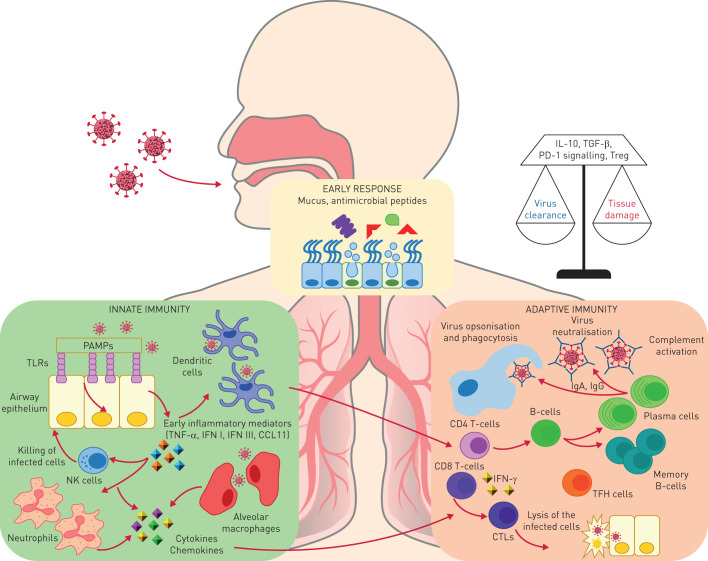
FIGURE 1.
The lungs and gut are exposed to environmental substances and pathogens. The early protection response to respiratory viruses includes mucus, surfactants and antiviral peptides that can prevent initial attachment and viral entry. Respiratory viruses enter via the respiratory epithelium. Epithelial cells have a key role in initiating the immune response by recognising viral components (pathogen-associated molecular patterns (PAMPs)) via Toll-like receptors (TLRs) and intracellular receptors. These cellular sensors trigger a signalling cascade resulting in the upregulation of type I and III interferon (IFN) and the inflammatory response. This leads to differentiation of dendritic cells that mediate the induction of the adaptive immunity and promote the recruitment of innate immunity cells, in particular neutrophils and natural killer (NK) cells. NK cells have the ability to kill virus-infected cells via perforin–granzyme-dependent mechanisms or by the Fas–Fas ligand pathway. Moreover, alveolar macrophages, recruited monocytes and macrophages as well as dendritic cells pick pathogen components and contribute to the immune response. All of these cells produce cytokines and chemokines that are important for the establishment of the adaptive responses and of the antiviral state. The adaptive response to respiratory viruses is mediated by both T- and B-cell compartments. T-cells contribute to the generation of the B-cell response. B-cells produce antibodies that may neutralise the respiratory viruses directly by binding to viral surface proteins that are essential for entry of the virus into host cells or through the ligation of Fc receptors to trigger the complement cascade and antibody-dependent cell-mediated cytotoxicity. Antibodies are in the form of IgA, mainly in the upper respiratory tract, or IgG, in the lower respiratory tract. Viral clearance is also mediated by CD8+-specific T-cells with cytolytic activity. The protective antiviral T-cell response is mainly mediated by IFN-γ production and is therefore biased toward a T-helper cell (Th) 1 response, whereas other T-cell subsets such as Th2 cells and Th17 cells play a minor role and they may be responsible for lung tissue damage. Moreover, regulatory mechanisms adopted by T-cells such as interleukin (IL)-10 secretion, or upregulation of inhibitory receptors such as programmed cell death protein 1 (PD-1) or expansion of the T-regulatory (Treg) cell subsets, work to balance tissue damage and viral clearance. TNF: tumour necrosis factor; CTL: cytotoxic T-lymphocyte; TFH: T-follicular helper; TGF: transforming growth factor.