Abstract
Purpose
To provide the first report of effective use of bilateral XEN Gel Stent implantation using an ab externo open-conjunctival approach designed to improve bleb function and meet the uniquely low intraocular pressure requirements of a Japanese patient with normal-tension glaucoma refractory to topical medical therapy.
Observations
A 54-year-old phakic Japanese woman with severe normal-tension glaucoma on maximally tolerated medical therapy of four topical agents presented with above-goal intraocular pressures and new medication intolerances. She underwent bilateral ab externo open-conjunctival XEN Gel Stent implantation with tenectomy and sub-Tenon's injection of 40μg of mitomycin-C, which resulted in reduction of intraocular pressures by 41.2 and 28.6% to 10 and 10 mmHg in the right and left eyes, respectively at the most recent visit. Postoperatively, a diffuse filtering bleb with good morphology developed in both eyes. The procedure has so far allowed for complete cessation of all four topical medications for up to eight months following surgery without any serious complications.
Conclusions
This case illustrates the potential of Xen Gel Stent implantation through an ab externo, open-conjunctival approach to be an effective, simple alternative to trabeculectomy to meet the unique low-pressure requirements of normal-tension glaucoma patients with practical and safety benefits of a micro-invasive approach.
Keywords: Low-tension glaucoma, Normal-tension glaucoma, XEN Gel Stent, Micro-invasive glaucoma surgery, Glaucoma, Stents, Glaucoma drainage implants
1. Introduction
Normal-tension glaucoma (NTG) is a unique and particularly challenging subgroup of primary open-angle glaucoma (POAG), in which the optic nerve degenerates despite intraocular pressures (IOPs) that remain within the statistically normal range below 21 mmHg.1 NTG represents a significant disease burden and comprises 30–92.3% of POAG patients, depending on race,2 with the highest proportion reported in Japanese patients.3 While the precise etiology of NTG is unknown, IOP appears to contribute to NTG pathogenesis, since IOP reduction slows disease progression.4 Thus, as with other forms of POAG, IOP-lowering therapies are mainstays of treatment.4 Many NTG patients are adequately treated with topical medication and laser therapy, however, there is a large subset that do not tolerate medication or progress despite these interventions, for which surgery may be necessary.2 Surgical management of NTG patients is especially challenging, since very low IOPs are required to achieve therapeutic reduction from baseline levels within the normal range.5 Consequently, surgeons face a narrow therapeutic window between these low target pressures and potentially dangerous hypotonus pressures.6
Trabeculectomy has traditionally been the first-line surgical option for NTG patients, since it is capable of meeting low IOP goals in NTG patients,5, 6, 7, 8, 9, 10, 11, 12 even when single-digit postsurgical IOPs are required.13 However, as a relatively invasive procedure, trabeculectomy has historically suffered from high complication rates, including long-term hypotony especially in NTG patients, ranging from 28 to 30%,6,12 which can lead to cataract formation,14 hypotonous maculopathy,6,13 and choroidal detachment.10,13 With recent improvements in trabeculectomy techniques15 and leveraging the experience of a dedicated NTG clinic, one group reported greatly reduced complication rates in NTG patients.16 However, these results are likely a best-case scenario, and it is not clear how widely applicable they are, since they require considerable surgical experience and skill to achieve pressures in the narrow therapeutic window through individualized fine-tuning of many complex surgical parameters, as well as diligent and intensive postoperative management, which may not be suitable for all patients and practices.15,16
To address the need for simpler, safer, and more reliable surgical options, micro-invasive glaucoma surgeries (MIGS) have been developed.17 MIGS provide numerous benefits including minimal tissue disruption and instrumentation, fast surgical times and postoperative recoveries, and improved safety profiles.18 While MIGS exploit a variety of mechanisms,19 devices such as the XEN Gel Stent mimic traditional trabeculectomies, creating an alternative, transscleral drainage pathway to a subconjunctival bleb.18 However, in contrast to trabeculectomies in which pressure is regulated by scleral flap suture tension,16 which can be unreliable, XEN Gel Stents (Allergran Inc., Irvine, CA) have a 45μm-diameter lumen designed using the Hagen-Poiseuille equation to limit outflow and theoretically prevent hypotony, providing a minimum IOP of 6–8 mmHg.20 Though a number of studies have investigated XEN Gel Stent implantation in mixed OAG patients and found it capable of effective IOP and medication reduction of 29–46% and 42–90%, respectively,18 it is currently unknown if XEN Gel Stent implantation can achieve the very low IOPs required for effective treatment of NTG patients. While the XEN Gel Stent has the theoretical potential to achieve IOPs ≤10 mmHg, in practice, post-implantation IOPs are typically in the 12–15 mmHg range in OAG patients using an ab interno approach.18,21, 22, 23, 24 It has been suggested that this discrepancy is due to additional outflow resistance of a suboptimal conjunctival bleb created following ab interno implantation.25,26 In contrast, an ab externo approach offers the opportunity to dissect Tenon's from the episclera and optimize stent positioning,27 which may allow for better bleb morphologies that can achieve lower IOPs closer to the theoretic limit. While no clinical studies have directly compared ab externo and ab interno implantation of XEN Gel Stents,28 anecdotally, clinicians have noted lower IOPs and better bleb morphologies with an ab externo approach.27 Thus for NTG, modifications to the XEN Gel Stent implantation procedure including an ab externo approach may produce better-functioning blebs with IOPs closer to the theoretical minimum that could effectively treat NTG.
To determine if ab externo open-conjunctival XEN Gel Stent implantation can achieve low IOPs required by NTG patients, we report the 8-month follow-up of an NTG patient, who received bilateral ab externo open-conjunctival XEN Gel Stent implantation without serious complications. This case illustrates the exciting potential for this approach to offer a safer, simpler, micro-invasive alternative to trabeculectomy to effectively achieve the uniquely low IOP requirements of NTG.
2. Case report
A 54-year-old Japanese woman was referred to the Massachusetts Eye and Ear Infirmary for evaluation and treatment of NTG in November of 2010. She had been previously diagnosed with NTG in December of 2009 at the age of 43 with initial IOPs of 16 mmHg in both eyes (OU) and was started on travaprost qhs OU. On presentation, the patient had a best corrected visual acuity (BCVA) of 20/20 in the right eye (OD) and 20/25 in the left eye (OS) and was myopic with a power of about -6D OU. Her IOPs measured 11 mmHg OD and 9 mmHg OS. Pachymetry showed thin corneas, averaging 499 μm OD and 505 μm OS. Dilated fundus exam revealed cup-to-disc ratios (CDR) of 0.9 OU with peripapillary atrophy and inferior notching in both eyes, which was confirmed by optical coherence tomography (OCT) with retinal nerve fiber layer (rNFL) measurement. No disc hemorrhages were observed. Functional testing with Humphrey Visual Fields (HVF) 24-2 showed a superior altitudinal defect in the right eye and a superior > inferior arcuate defect in the left eye.
She had several NTG risk factors including female sex, thin corneas, myopia, and Japanese ancestry.2 She had no family history of glaucoma. Her vascular and perfusion risk factors included borderline hypertension, treated with atenolol 12.5mg qAM, and impaired glucose tolerance. She denied any history of diabetes mellitus, migraines, Raynaud's phenomenon or obstructive sleep apnea.
Over the next 10 years, her NTG progressed slowly, requiring increasingly aggressive medical and laser therapies. Her IOPs remained slightly above target pressures despite increasing topical medical therapy that ultimately included latanoprostene bunod qhs OU, dorzolamide/timolol tid OU, and netarsudil qhs OU. She was also trialed on brimonidine at dosages of 0.15% and 0.1% and frequencies of bid and tid OU and methazolamide 25mg PO bid, which she did not tolerate due to side effects. Furthermore, she received 360-degree selective laser trabeculoplasty OS in 2011 and 2013, which had little effect on her IOP, as well as separate superior and inferior argon laser trabeculoplasty OD in 2013, which mildly lowered her pressures in that eye. Her IOPs over this period ranged from 12 to 18 mmHg OD and 10–20 mmHg OS on medication.
In 2019, she was stable with IOPs of 12 mmHg OU for roughly eight months on maximally tolerated medical therapy of latanoprostene bunod qhs OU, dorzolamide/timolol bid OU, and netarsudil OU, before her IOPs increased to 17 mmHg and 14 mmHg OD and OS respectively. Additionally, she began developing intolerances to dorzolamide/timolol and netarsudil with redness and tearing following application. Humphery visual field testing at this time showed mean deviations of −14.12 OD with a superior altitudinal defect and −12.17 OS with a superior arcuate defect and inferior nasal step (Fig. 1). Given her above-goal IOPs and new medication intolerances, the risks and benefits of various surgical interventions were weighed. The patient and surgeon agreed to proceed with XEN Gel Stent implantation, starting with the right eye with a plan to perform an identical procedure subsequently in the left eye, pending a good result.
Fig. 1.
Preoperative Humphery visual field testing. A mean deviation of −14.12 OD with a superior altitudinal defect (left) and −12.17 OS with a superior arcuate defect and inferior nasal step (right) were found.
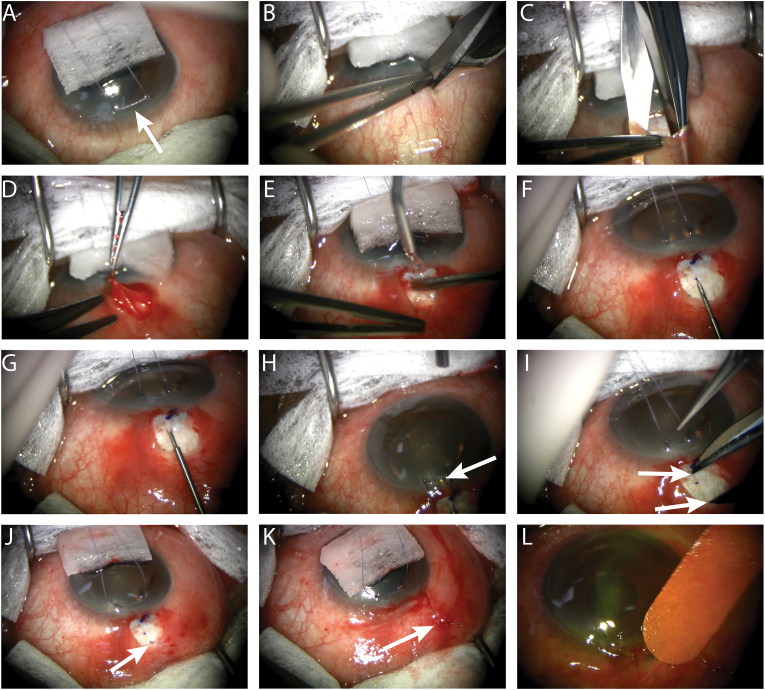
In December of 2019, a XEN Gel Stent was implanted OD ab externo (Fig. 2). The case was done under monitored anesthesia care with retrobulbar block (lidocaine 1% bupivacaine 0.375%), analgesia (50 mcg remifentanil), sedation (2mg midazolam), and topical anesthesia (0.5% proparacaine). First, a superior corneal traction suture was placed. The conjunctiva was opened with a small peritomy and the subconjunctival space was blunt dissected posteriorly. Tenon's was excised from the limbus posteriorly, creating a small perilimbal tenectomy. The sub-Tenon's space was blunt dissected posteriorly, and light cautery was performed on the exposed sclera. The XEN injector was placed bevel up in the sclera, 1.5 mm from the limbus and advanced through the sclera to the limbus. Countertraction was applied with the corneal traction suture to angle the stent at 30° and it was then advanced into the anterior chamber. The XEN gel Stent was then deployed, and the injector retracted slowly. The positioning of the XEN Gel Stent was then adjusted so that 2–3 mm of the stent was positioned correctly in the subconjunctival space. One single interrupted 8-0 Vicryl suture was used to lay the stent flat against the sclera and tied loosely to avoid occluding the stent before the conjunctival incision was sutured with an 8-0 Vicryl mattress suture. Since Tenon's was excised and not closed, a space between the sclera and conjunctiva was created for subsequent bleb formation. Approximately 0.1 mL of mitomycin-C (MMC) 0.4mg/mL was injected in the sub-Tenon's space and a Seidel test was performed to check for leaks. Since the Tenon's was partially excised and not closed, the subconjunctival and sub-Tenon's spaces are continuous so sub-Tenon's injection of MMC filled both of these spaces. No ophthalmic viscosurgical devices were used. Her glaucoma medications were stopped in the right, operative eye.
Fig. 2.
Serial photographs of the ab externo surgical approach for XENGelStent implantation. (A) A corneal traction suture is placed. (B) The conjunctiva is incised from the limbus posteriorly. (C) The subconjunctival space is blunt dissected posteriorly. (D) Tenon's is excised creating a small perilimbal tenectomy and sub-Tenon's posterior blunt dissection is performed (as in C). (E) Light cautery is applied to the exposed sclera. (F) The XEN Gel Stent injector is inserted 1.5 mm posterior to the limbus. (G) The injector is then advanced through the sclera to the limbus. (H) The XEN Gel Stent injector is angled at 30° with countertraction applied using the corneal suture and advanced into the anterior chamber. (I) The XEN Gel Stent injector is retracted, and the stent position is adjusted so that 2–3 mm of the stent is in the subconjunctival space. (J) The XEN Gel Stent is positioned beneath the conjunctiva and sutured flat against the sclera with a single interrupted 8-0 Vicryl suture. (K) The conjunctiva is then closed with an 8-0 Vicryl mattress suture. The Tenon's is not closed creating a space between the sclera and conjunctiva and allowing communication of the sub-Tenon's and subconjunctival spaces. (L) A Seidel test is performed to check for leaks and 0.1 mL of mitomycin-C 0.4 mg/ml is injected subconjunctivally. *Note: these images are of a representative XEN Gel Stent implantation from a different patient than described in this case.
On postoperative day (POD) 1, the IOP measured 3 mmHg OD and a Seidel test revealed a slow superotemporal leak. A bandage contact lens was placed for 1 week and she was started on moxifloxacin qid OD for 10 days, atropine qid OD for 4 weeks, and prednisolone acetate 1% qid OD, which was slowly tapered over 10 weeks. By postoperative week (POW) 2, her leak and hypotony resolved and her IOP was 9 mmHg OD without any IOP-lowering medications.
Given a good result at postoperative month (POM) 4 with single-digit IOPs and no need for medication in the right eye, XEN Gel Stent implantation was performed in the left eye in April of 2020 using the same technique. On POD1, her IOP measured 5 mmHg OS, increasing to 7 mmHg OS by POW1, with no evidence of wound leakage. She received a similar postoperative medication regime of moxifloxacin qid OS for one week, atropine bid OS for four weeks, and prednisolone acetate 1% q2h OS, which was slowly tapered over 10 weeks.
In the six months following surgery in the right eye, her IOPs ranged from 9 to 11 mmHg OD, while for the two and a half months following surgery in her left eye, her IOPs ranged from 7 to 9 mmHg OS. At her most recent visit (POM8.5 OD and POM4 OS), her BCVA was 20/25 OD and 20/30–1 OS. Her IOPs measured 10 mmHg OD and 10 mmHg OS off medications. The dilated fundus exam showed stable temporal thinning with peripapillary atrophy OU, and the OCT rNFL thickness was stable at 72 μm OD and 59 μm OS compared with preoperative measurements. OCT of the retina showed no evidence of maculopathy or cystoid macular edema. A diffuse, slightly elevated, avascular, posterior filtering bleb with good morphology appeared stable in the left eye one month after surgery (Fig. 3). The right eye bleb had a similar appearance to the left.
Fig. 3.
Diffuse filtering bleb following ab externo open-conjunctival Xen Gel Stent implantation in a patient with normal-tension glaucoma. Ocular-surface photo of left eye taken through a slit-lamp microscope 1 month after XEN Gel Stent implantation in a patient with normal-tension glaucoma. The XEN Gel Stent is visible within a diffuse fluid-filled subconjunctival filtering bleb (black arrow).
3. Discussion
Here we provide the first description of bilateral ab externo open-conjunctival XEN Gel Stent implantation designed to improve bleb function to meet the uniquely low IOP requirements of a Japanese NTG patient. Surgery has for now allowed the cessation of all glaucoma medications and stabilization of pressures beneath the goal IOP of 12 mmHg. Preoperatively, her maximum recorded IOPs were 18 mmHg OD and 20 mmHg OS, which were initially controlled with topical medications, but measured 17 mmHg OD and 14 mmHg OS immediately prior to surgery. At the most recent follow-up visit 8.5 months after surgery OD and 4 months after surgery OS, IOP was reduced to 10 mmHg (7 mmHg, 41.2% reduction) OD and 10 mmHg (6 mmHg, 28.6% reduction) OS and her medication burden of four IOP lowering medications OU was eliminated. This case demonstrates the ability of XEN Gel Stent implantation using an ab externo open-conjunctival approach to improve bleb function and reach the very low IOPs required to treat NTG through a simpler, potentially safer, micro-invasive surgery.
The surgical approach described here featured modifications to the original XEN Gel Stent implantation technique to improve bleb filtration capacity and achieve lower IOPs for this NTG patient. Bleb morphology is likely the main contributor to overall outflow resistance and thus determines the IOP one can achieve with XEN Gel Stents.25, 26, 27 Bleb efficacy is inversely related to the wound-healing response, which is more robust in Asian patients, including the Japanese patient in this case.29 While XEN Gel Stents were originally studied using an ab interno approach,21,23,24 in this case we chose an ab externo, open-conjunctival approach, which has gained popularity recently due to several key advantages.27 Most importantly for NTG patients, this approach allows for consistent sub-Tenon's stent placement, which has been shown to result in greater IOP reduction.30 The mechanism for greater IOP reduction of sub-Tenon's placement is unknown, though perhaps the scleral vasculature is more effective at draining fluid or the healing response in the sub-Tenon's space is more conducive for developing diffuse posterior blebs that facilitate better drainage. Additionally, Tenon's can be separated from the episclera creating a pocket of space to shape bleb morphology and ensure the stent is free and mobile.27,31 Thus, the ab externo open-conjunctival approach may offer improved bleb function and better IOP reduction capability, which is especially important for NTG patients with low IOP requirements. Additionally, the ab externo open-conjunctival approach does not require corneal incisions or instrumentation in the anterior chamber except for the Xen Gel Stent injector itself, making it theoretically safer in phakic eyes and offering the surgeon more flexibility in adjusting the stent's precise depth in the anterior chamber.27
Other techniques to reduce the wound-healing response and optimize bleb formation in this patient included scleral cautery following dissection of Tenon's to reduce intraoperative bleeding and limit the release of proinflammatory factors.31 Additionally, the antiproliferative agent, mitomycin C (MMC), was injected beneath Tenon's, which reduces scarring and fibrosis, primary causes of bleb failure32 and improves outcomes for both trabeculectomy and XEN Gel Stent implantation.31 Since a small portion of Tenon's was removed at the location of the stent, with blunt posterior dissection of both the subconjunctival and sub-Tenon's spaces, MMC injection can reach the inner conjunctival surface, both sides of the remaining Tenon's and the outer scleral surface, inhibiting fibroblast proliferation and scarring from all of these potential sources. Finally, a partial tenectomy was performed, which has been shown to reduce the frequency of encapsulated blebs following trabeculectomy in pediatric patients33 and may reduce the risk of early stent obstruction.27 These modifications likely promoted the formation of excellent diffuse, posterior, and avascular bleb morphologies.
While XEN Gel Stents are designed to reduce the rates of dangerous complications from chronic hypotony that are seen with trabeculectomies, inserting a foreign body introduces additional risks including conjunctival erosion, stent migration, and stent-iris touch, which are fortunately rare events.23,24,34 To help prevent stent migration and conjunctival erosion, especially after partial tenectomy, here the stent was sutured flush with sclera using 8-0 Vicryl for temporary protection during the vulnerable healing phase when bleb morphology is established. Others prefer Nylon for permanent fixation,27 though this introduces greater risks of XEN Gel Stent occlusion if the suture is tied tightly as well as an additional long-term foreign body. While XEN Gel Stents have higher rates of postoperative bleb needling compared with trabeculectomy,24 this has been greatly reduced with an ab externo open-conjunctival approach and subconjunctival mitomycin C injection.27 As was the case in this patient, transient numeric hypotony on the day following surgery is relatively common with XEN Gel Stent implantation, likely due to peri-tubular filtration.35 However, importantly, unlike dangerous chronic hypotony, this early hypotony is largely benign, typically resolving quickly with short-term topical atropine and steroid therapy and does not require additional surgical intervention.36 Unlike an ab interno approach, opening the conjunctiva also adds the risk of wound leak, which occurred following surgery in this patient's right eye, though it resolved quickly following application of a bandage contact lens. Overall, the benefits of this simple micro-invasive technique likely outweigh these minor and rare complications in the majority of cases.
XEN Gel Stents were introduced relatively recently, and implantation techniques have undergone rapid evolution as surgeons gain more experience using these devices. As a result, despite widespread adoption, no studies have been performed examining whether new techniques such as ab externo open-conjunctival implantation can improve bleb function and achieve IOPs closer to the theoretical minimum, especially in the challenging and vulnerable NTG patient population. A number of studies have examined ab interno XEN Gel Stent implantation in mixed POAG populations and found mean IOP reductions ranging from 28 to 42.1% with postoperative IOPs ranging from 12 to 15 mmHg.18,21, 22, 23, 24,37, 38, 39, 40, 41 Direct comparison of ab interno XEN Gel Stent implantation with trabeculectomy in POAG patients found no difference in the rates of surgical success or reduction in IOP lowering medications.24,39,42,43 While one study found that trabeculectomy resulted in lower postoperative IOPs,39 others found no difference.42,43 Patients receiving XEN Gel Stents benefited from fewer postoperative visits and a faster postoperative course.24 In terms of safety, one study found no differences,24 while another found an improved safety profile with XEN Gel Stent implantation.43 Overall, ab interno XEN Gel Stent implantation appears to compare favorably to trabeculectomy for many POAG patients with practical and safety benefits, though it is unknown whether this is also true for the more challenging IOP requirements of NTG patients. The low IOPs obtained in the NTG patient reported here serve as justification for future studies examining the role of XEN Gel Stent implantation with current surgical techniques to optimize bleb filtration in this patient population. It will be interesting to see if XEN Gel Stent implantation can provide an effective alternative to trabeculectomy to reliably meet the challenging low pressure needs of NTG patients with lower rates of potentially dangerous complications like long-term hypotony.
4. Conclusion
Here we report a case of a 54-year-old Japanese woman who received bilateral ab externo open-conjunctival XEN Gel Stent implantation for treatment of NTG refractory to topical medical therapy. This simple micro-invasive approach, optimized to improve bleb function, reduced IOPs by 41.2 and 28.6% to 10 and 10 mmHg in the right and left eye respectively and eliminated need for topical therapy, which consisted of 4 agents preoperatively. This outcome illustrates a potential role for ab externo open-conjunctival XEN Gel Stent implantation in NTG patients to achieve IOP reductions that can meet their uniquely low-pressure requirements, while limiting the rates of dangerous long-term hypotony that can occur following trabeculectomy.
Patient consent
The patient consented to publication of the case in writing.
Funding
The research was generously funded by Mr. Stephen Traynor, Mr. and Mrs. Chad and Anne Gifford, and Mr. Joseph Leitch. J.M.H acknowledges support from the National Institute of General Medical Sciences (T32GM007753).
Authorship
All authors attest that they meet the current ICMJE criteria for authorship. D.S.V. was the attending physician on the case. J.M.H. researched the case, and both authors contributed to the writing and revising processes.
Declaration of competing interest
The following authors have no financial disclosures: J.M.H., D.S·V.
Acknowledgements
None.
Contributor Information
James M. Harris, Email: james_harris@hms.harvard.edu.
David Solá-Del Valle, Email: David_Sola-DelValle@meei.harvard.edu.
References
- 1.Lee B.L., Bathija R., Weinreb R.N. The definition of normal-tension glaucoma. J Glaucoma. 1998;7(6):366–371. [PubMed] [Google Scholar]
- 2.Lee J.W.Y., Chan P.P., Zhang X., Chen L.J., Jonas J.B. Latest developments in normal-pressure glaucoma: diagnosis, epidemiology, genetics, etiology, causes and mechanisms to management. Asia Pac J Ophthalmol (Phila) 2019;8(6):457–468. doi: 10.1097/01.APO.0000605096.48529.9c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Iwase A., Suzuki Y., Araie M. The prevalence of primary open-angle glaucoma in Japanese: the Tajimi Study. Ophthalmology. 2004;111(9):1641–1648. doi: 10.1016/j.ophtha.2004.03.029. [DOI] [PubMed] [Google Scholar]
- 4.Collaborative Normal-Tension Glaucoma Study Group Comparison of glaucomatous progression between untreated patients with normal-tension glaucoma and patients with therapeutically reduced intraocular pressures. Am J Ophthalmol. 1998;126(4):487–497. doi: 10.1016/s0002-9394(98)00223-2. [DOI] [PubMed] [Google Scholar]
- 5.Naito T., Fujiwara M., Miki T. Effect of trabeculectomy on visual field progression in Japanese progressive normal-tension glaucoma with intraocular pressure < 15 mmHg. PLoS One. 2017;12(8) doi: 10.1371/journal.pone.0184096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Membrey W.L., Poinoosawmy D.P., Bunce C., Hitchings R.A. Glaucoma surgery with or without adjunctive antiproliferatives in normal tension glaucoma: 1 intraocular pressure control and complications. Br J Ophthalmol. 2000;84(6):586–590. doi: 10.1136/bjo.84.6.586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hitchings R.A., Wu J., Poinoosawmy D., McNaught A. Surgery for normal tension glaucoma. Br J Ophthalmol. 1995;79(5):402–406. doi: 10.1136/bjo.79.5.402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Aoyama A., Ishida K., Sawada A., Yamamoto T. Target intraocular pressure for stability of visual field loss progression in normal-tension glaucoma. Jpn J Ophthalmol. 2010;54(2):117–123. doi: 10.1007/s10384-009-0779-z. [DOI] [PubMed] [Google Scholar]
- 9.Schulzer M. Intraocular pressure reduction in normal-tension glaucoma patients. The normal tension glaucoma study group. Ophthalmology. 1992;99(9):1468–1470. doi: 10.1016/s0161-6420(92)31782-8. [DOI] [PubMed] [Google Scholar]
- 10.Jongsareejit B., Tomidokoro A., Mimura T., Tomita G., Shirato S., Araie M. Efficacy and complications after trabeculectomy with mitomycin C in normal-tension glaucoma. Jpn J Ophthalmol. 2005;49(3):223–227. doi: 10.1007/s10384-004-0181-9. [DOI] [PubMed] [Google Scholar]
- 11.Oie S., Ishida K., Yamamoto T. Impact of intraocular pressure reduction on visual field progression in normal-tension glaucoma followed up over 15 years. Jpn J Ophthalmol. 2017;61(4):314–323. doi: 10.1007/s10384-017-0519-8. [DOI] [PubMed] [Google Scholar]
- 12.Iverson S.M., Schultz S.K., Shi W., Feuer W.J., Greenfield D.S. Effectiveness of single-digit IOP targets on decreasing global and localized visual field progression after filtration surgery in eyes with progressive normal-tension glaucoma. J Glaucoma. 2016;25(5):408–414. doi: 10.1097/IJG.0000000000000240. [DOI] [PubMed] [Google Scholar]
- 13.Schultz S.K., Iverson S.M., Shi W., Greenfield D.S. Safety and efficacy of achieving single-digit intraocular pressure targets with filtration surgery in eyes with progressive normal-tension glaucoma. J Glaucoma. 2016;25(2):217–222. doi: 10.1097/IJG.0000000000000145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Vesti E. Development of cataract after trabeculectomy. Acta Ophthalmol. 1993;71(6):777–781. doi: 10.1111/j.1755-3768.1993.tb08599.x. [DOI] [PubMed] [Google Scholar]
- 15.Khaw P.T., Chiang M., Shah P., Sii F., Lockwood A., Khalili A. Vol. 50. Karger Publishers; 2012. Enhanced Trabeculectomy--the Moorfields safer surgery system; pp. 1–28. (Glaucoma Surgery). [DOI] [PubMed] [Google Scholar]
- 16.Jayaram H., Strouthidis N.G., Kamal D.S. Trabeculectomy for normal tension glaucoma: outcomes using the Moorfields Safer Surgery technique. Br J Ophthalmol. 2016;100(3):332–338. doi: 10.1136/bjophthalmol-2015-306872. [DOI] [PubMed] [Google Scholar]
- 17.Sheybani A., Scott R., Samuelson T.W. Open-angle glaucoma: burden of illness, current therapies, and the management of nocturnal IOP variation. Ophthalmol Ther. 2020;9(1):1–14. doi: 10.1007/s40123-019-00222-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.De Gregorio A., Pedrotti E., Stevan G., Bertoncello A., Morselli S. XEN glaucoma treatment system in the management of refractory glaucomas: a short review on trial data and potential role in clinical practice. Clin Ophthalmol. 2018;12:773. doi: 10.2147/OPTH.S146919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ahmed I.I.K. MIGS and the FDA: what's in a Name? Ophthalmology. 2015;122(9):1737–1739. doi: 10.1016/j.ophtha.2015.06.022. [DOI] [PubMed] [Google Scholar]
- 20.Sheybani A., Reitsamer H., Ahmed I.I.K. Fluid dynamics of a novel micro-fistula implant for the surgical treatment of glaucoma. Invest Ophthalmol Vis Sci. 2015;56(8):4789–4795. doi: 10.1167/iovs.15-16625. [DOI] [PubMed] [Google Scholar]
- 21.Sheybani A., Dick H.B., Ahmed I.I.K. Early clinical results of a novel ab interno gel stent for the surgical treatment of open-angle glaucoma. J Glaucoma. 2016;25(7):e691–e696. doi: 10.1097/IJG.0000000000000352. [DOI] [PubMed] [Google Scholar]
- 22.Buffault J., Graber M., Bensmail D. Efficacy and safety at 6 months of the XEN implant for the management of open angle glaucoma. Sci Rep. 2020;10(1) doi: 10.1038/s41598-020-61319-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Grover D.S., Flynn W.J., Bashford K.P. Performance and safety of a new ab interno gelatin stent in refractory glaucoma at 12 months. Am J Ophthalmol. 2017;183:25–36. doi: 10.1016/j.ajo.2017.07.023. [DOI] [PubMed] [Google Scholar]
- 24.Schlenker M.B., Gulamhusein H., Conrad-Hengerer I. Efficacy, safety, and risk factors for failure of standalone ab interno gelatin microstent implantation versus standalone trabeculectomy. Ophthalmology. 2017;124(11):1579–1588. doi: 10.1016/j.ophtha.2017.05.004. [DOI] [PubMed] [Google Scholar]
- 25.Lee R.M.H., Bouremel Y., Eames I., Brocchini S., Khaw P.T. The implications of an ab interno versus ab externo surgical approach on outflow resistance of a subconjunctival drainage device for intraocular pressure control. Transl Vis Sci Technol. 2019;8(3):58. doi: 10.1167/tvst.8.3.58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lenzhofer M., Strohmaier C., Hohensinn M. Longitudinal bleb morphology in anterior segment OCT after minimally invasive transscleral ab interno Glaucoma Gel Microstent implantation. Acta Ophthalmol. 2019;97(2):e231–e237. doi: 10.1111/aos.13902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Panarelli J.F., Yan D.B., Francis B., Craven E.R. XEN gel stent open conjunctiva technique: a practical approach paper. Adv Ther. 2020;37(5):2538–2549. doi: 10.1007/s12325-020-01278-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sheybani A., Grover D.S., Fellman R.L. Critical response to ab interno versus ab externo surgical approach on outflow resistance of a subconjunctival drainage device. Transl Vis Sci Technol. 2020;9(3) doi: 10.1167/tvst.9.3.14. 14-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Toh Z.H., Lee C.S.Y., Chew A.C.Y., Perera S. Time heals all wounds: obstacles in glaucoma surgery from an asian perspective. Proceedings of Singapore Healthcare. 2015;24(2):103–112. [Google Scholar]
- 30.Lenzhofer M., Strohmaier C., Sperl P. Effect of the outer stent position on efficacy after minimally invasive transscleral glaucoma gel stent implantation. Acta Ophthalmol. 2019;97(8):e1105–e1111. doi: 10.1111/aos.14167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Vera V., Sheybani A., Lindfield D., Stalmans I., Ahmed I.I.K. Recommendations for the management of elevated intraocular pressure due to bleb fibrosis after XEN gel stent implantation. Clin Ophthalmol. 2019;13:685–694. doi: 10.2147/OPTH.S195457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Skuta G.L., Parrish R.K., 2nd Wound healing in glaucoma filtering surgery. Surv Ophthalmol. 1987;32(3):149–170. doi: 10.1016/0039-6257(87)90091-9. [DOI] [PubMed] [Google Scholar]
- 33.Awadein A., El Sayed Y.M. Excision of Tenon capsule in pediatric trabeculectomy: a controlled study. J Glaucoma. 2016;25(1):39–44. doi: 10.1097/IJG.0000000000000220. [DOI] [PubMed] [Google Scholar]
- 34.Gillmann K., Bravetti G.E., Mermoud A., Mansouri K. Anterior chamber XEN gel stent movements: the impact on corneal endothelial cell density. J Glaucoma. 2019;28(6):e93–e95. doi: 10.1097/IJG.0000000000001200. [DOI] [PubMed] [Google Scholar]
- 35.Fea A.M., Durr G.M., Marolo P., Malinverni L., Economou M.A., Ahmed I. XEN® gel stent: a comprehensive review on its use as a treatment option for refractory glaucoma. Clin Ophthalmol. 2020;14:1805–1832. doi: 10.2147/OPTH.S178348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Karimi A., Lindfield D. Is a Day 1 postoperative review following ab interno Xen gel stent surgery for glaucoma needed? Clin Ophthalmol. 2018;12:2331–2335. doi: 10.2147/OPTH.S181530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hong K., Lind J., Sheybani A. Safety and efficacy outcomes of the Xen45 Gel Stent use for refractory glaucoma: a surgery series from surgeon trainees at a tertiary teaching hospital. Eye Vis (Lond). 2020;7:5. doi: 10.1186/s40662-019-0171-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Myers J.S., Zheng C.X., Moster S.J., Lin M. Short term outcomes of transconjunctival ab externo XEN 45 Gel Stent implantation. Invest Ophthalmol Vis Sci. 2019;60(9) 3735-3735. [Google Scholar]
- 39.Wagner F.M., Schuster A.K., Emmerich J., Chronopoulos P., Hoffmann E.M. Efficacy and safety of XEN(R)-Implantation vs. trabeculectomy: data of a “real-world” setting. PLoS One. 2020;15(4) doi: 10.1371/journal.pone.0231614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Reitsamer H., Sng C., Vera V. Two-year results of a multicenter study of the ab interno gelatin implant in medically uncontrolled primary open-angle glaucoma. Graefes Arch Clin Exp Ophthalmol. 2019;257(5):983–996. doi: 10.1007/s00417-019-04251-z. [DOI] [PubMed] [Google Scholar]
- 41.Galal A., Bilgic A., Eltanamly R., Osman A. XEN glaucoma implant with mitomycin C 1-year follow-up: result and complications. J Ophthalmol. 2017;2017:5457246. doi: 10.1155/2017/5457246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Teus M.A., Paz Moreno-Arrones J., Castaño B., Castejon M.A., Bolivar G. Optical coherence tomography analysis of filtering blebs after long-term, functioning trabeculectomy and XEN® stent implant. Graefes Arch Clin Exp Ophthalmol. 2019;257(5):1005–1011. doi: 10.1007/s00417-019-04272-8. [DOI] [PubMed] [Google Scholar]
- 43.Marcos Parra M.T., Salinas López J.A., López Grau N.S., Ceausescu A.M., Pérez Santonja J.J. XEN implant device versus trabeculectomy, either alone or in combination with phacoemulsification, in open-angle glaucoma patients. Graefes Arch Clin Exp Ophthalmol. 2019;257(8):1741–1750. doi: 10.1007/s00417-019-04341-y. [DOI] [PubMed] [Google Scholar]