Highlights
-
•
Hydatid disease is endemic in North Africa countries such as Tunisia.
-
•
Retroperitoneal location is scarce.
-
•
Parietal complications are rarely described even in endemic geographic locations.
-
•
Management of parietal complications of hydatid cysts is not consensual.
-
•
Surgical drainage remains the gold standard.
Keywords: Cystic echinococcosis, Hydatid disease, Retroperitoneal cyst, Parietal complication
Abstract
Introduction
Hydatid disease is a global zoonosis. Any organ of the human body can be involved. Single or multiple locations are reported. However, retroperitoneal hydatid cysts are uncommon. Furthermore, parietal complications are rarely reported in literature. Therefore, the management of hydatid cysts ruptured in the abdominal wall remains challenging.
Presentation of case
In this case report, we aim to describe our experience in treating a primary retroperitoneal hydatid cyst with rupture into abdominal wall in an 87-year-old woman who presented with a 15-centimeter mass of the right flank. Hydatid serology test was positive. An abdominal CT scan showed a 20-centimeter cystic mass of retroperitoneum extended to the abdominal wall with several septa within and enhanced thick wall. The patient underwent a surgical elective drainage with perioperative antiparasitic chemotherapy. Follow-up showed no recurrence.
Discussion
Primary retroperitoneal hydatid cyst with parietal complications is scarce and barely described in literature. We performed a review of the recent relevant literature that deals with this subject. None of the hydatid cysts reported in 55 cases was located in retroperitoneum. The top seven countries of origin are located in Mediterranean region except for India. Imaging is compulsory for the diagnosis along with patient’s history, physical examination and hydatid serology. The treatment is surgical and must be must be covered by antiparasitic chemotherapy.
Conclusion
Primary retroperitoneal hydatid cyst extended to the abdominal wall remains a rare and challenging diagnosis that must be considered in endemic countries.
1. Introduction
Hydatid cyst is a worldwide zoonosis caused by Echinococcus granulosus. It could affect any organ and cause several complications [1,2]. The most frequently involved organs are the liver and lungs [3]. The retroperitoneal location is very rare and seldomly described in literature [4]. Hydatid cyst rupture is a common complication, especially its rupture into the peritoneal cavity or into the biliary tract. However, its rupture in a subcutaneous area is exceptional [4]. Those rare locations and complications may pose diagnostic and therapeutic dilemmas.
We hereby report a rare and unusually located hydatid cyst with a subcutaneous rupture, while detailing the diagnostic and therapeutic issues.
The case report has been reported in line with the SCARE criteria [5].
2. Case report
An 87-year-old female living in a rural area, with no past medical, surgical or drug history, was referred by family physician to our department, for an isolated right flank mass evolving progressively for 3 months. On physical examination, the patient had a superficial and well-defined 15 cm-cystic-mass of the right flank (Fig. 1). No inflammatory signs were present. The physical examination found a painlessly palpable, firm and fluctuant mass, measuring 15 cm. The remainder of the physical examination was normal. The patient’s Blood Tests revealed a biological inflammatory syndrome with a hyperleukocytosis and a high C-reactive protein. In addition, eosinophilia of 15% was noticed in the complete blood cell count. Her Hydatid serology test result was positive.
Fig. 1.
Mass of the right flank.
Abdominal ultrasound showed a cystic mass, with a diameter of 15 cm, protruding in the subcutaneous area. These results were highly suggestive of hydatid disease.
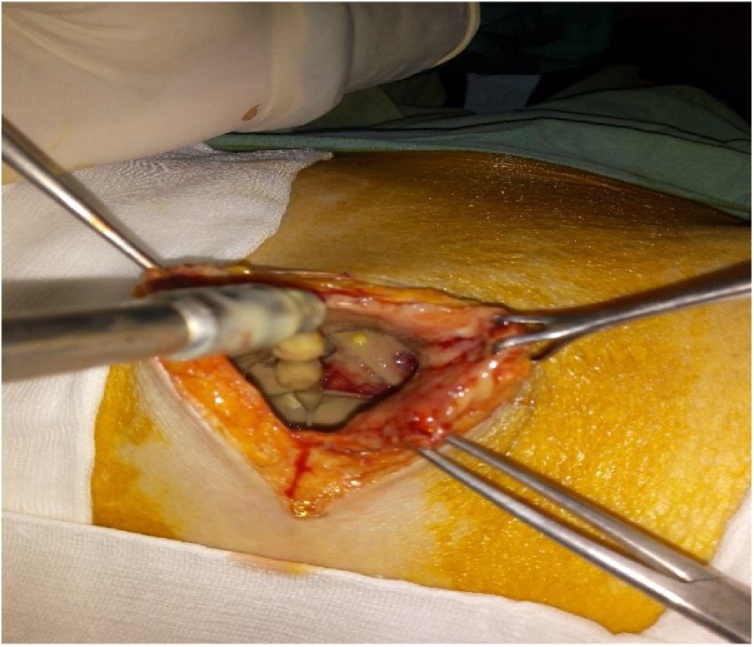
An abdominal computed tomography was performed to determine the mass’ location and its intra or extra peritoneal extension. The CT revealed (Fig. 2) a 20 × 15 cm cystic mass with an enhanced thick wall, containing several septa within, extending to the subcutaneous tissues of the right side of the abdominal wall. The mass was independent from any intra-peritoneal organ. However, the voluminous cyst caused a significant mass effect on adjacent organs especially the right kidney. The diagnosis of a retroperitoneal hydatid cyst ruptured into the abdominal wall was established. The patient received a preoperative antiparasitic chemotherapy based on Albendazole 400 mg twice daily for one month. Then, she underwent a surgical treatment (Fig. 3) three days after admission. Surgical drainage by an elective right flank incision was performed by an associate professor in general surgery, under general anesthesia with the patient in the left lateral decubitus position. The punction of the cyst resulted in the aspiration of approximately 1500 mL of purulent material including daughter vesicles. The cyst was then completely emptied of its content. No other surgical procedure was performed due to the advanced age of the patient. Drainage of the residual cavity was performed. The post-operative course was uneventful. The patient was discharged 8 days after hospitalization and was followed at the outpatient clinic. She received an adjuvant Albendazole treatment for 6 months. The clinical and radiological follow-up for 12 months showed no evidence of recurrence and the patient was satisfied with the result.
Fig. 2.
CT scan of the ruptured Retroperitoneal cyst.
Fig. 3.
Preoperative view.
3. Discussion
Hydatid disease is a significant public health problem in North Africa [6]. It is an endemic zoonotic disorder in Tunisia, which is mainly caused by Echinococcus granulosus. It could affect any organ and cause several complications [7]. Other organs are less frequently involved by the hydatid disease such as the spleen, the kidneys and the pancreas. Hydatid disease involving the retroperitoneum, as observed in our case, is extremely rare [4,6]. A significant proportion of cases may remain asymptomatic for years. Symptoms differ depending on the location, number and size of the hydatid cysts [4]. In addition, signs depend on whether the disease is complicated or not. The most common complications of hydatid disease are rupture, secondary infections and compression [7]. Because of cyst enlargement and compression, hydatid cysts can rupture into physiologic tracts, into the peritoneal cavity, or even in adjacent organs. Parietal complications are extremely scarce and its clinical presentation can be derailing. To our knowledge, our case report is the only well-documented primary retroperitoneal hydatid cyst ruptured into the abdominal wall. It aims to add to our understanding of this disease and possible treatments. A review of literature [8] concerning hydatid cysts extended to the abdominal wall with or without cutaneous fistula was recently published. It covers 52 previous publications (English, French, Spanish, Italian, German and Russian) with a total of 55 reported cases. In none of these cases was the hydatid cyst located in the retroperitoneum. Factors responsible for subcutaneous rupture of hydatid cyst are inflammation and infection [9]. The cyst content was purulent in our case. The parietal complications of the hydatid cyst are generally classified into 3 stages based on the depth of invasion of the lesions in the abdominal wall [10]. Stage 1 includes protruding hydatid lesions in the wall muscle layer. When these lesions exceed the muscular layer to invade the subcutaneous layer, the hydatid cyst is classified as stage 2, as it was the case for our patient. Finally, stage 3 corresponds to a hydatid disease fistulized to the skin.
The diagnosis of parietal complications is based mainly on clinical data and patient’s history. Indeed, our patient presented with a cystic mass of the right flank but had no medical or surgical history. Serological tests are useful for establishing the diagnosis and excluding the differential diagnoses particularly in endemic areas like Tunisia. It was positive in our patient’s case. The contribution of medical imaging is undeniable. The most commonly used radiological tools to both diagnose the parietal complications of the hydatid disease and determine the location of lesions are the abdominal ultrasound and CT scan. It is certain that sonography is sufficient for the diagnosis of the hydatid disease [11]. However, the necessity of determining the exact number, size, location, complications and intra-abdominal relationships of the cysts drove us to lean on the CT scan which is, actually, the recommended abdominal imaging before any surgical or medical treatment for a complicated hydatid disease [12]. In the case of our patient, the imaging was outstanding. It revealed a retroperitoneal hydatid cyst ruptured in the abdominal wall: a cystic mass with an enhanced thick wall and many septa, extending to the subcutaneous tissues of the right side of the abdominal wall. The mass was independent from any intra-peritoneal organ. Its management is nonconsensual and depends on the surgeon’s experience and the patient's condition. Surgery remains the best option [6]. The appropriate treatment for a hydatid cyst depends on its localization, size, and complications. The general principles in treating hydatid disease can be used in these cases [8]. We could perform a radical surgery with pericystectomy and eventual en-bloc resection of involved organs. However, in light of imaging findings in our patient and her general condition, elective conservative surgery was the most suitable alternative. Surgery must be covered by an Albendazole-based treatment in order to minimize the risk of recurrence [13], particularly after conservative surgery.
4. Conclusion
Parietal complications of the hydatid disease are rare. Adequate knowledge of diagnostic imaging clues of this type of complications is crucial to guide the clinical, radiological, and therapeutic management. Its management is nonconsensual and depends on the surgeon’s experience and the patient's condition. Subcutaneous rupture of hydatid disease should be considered as a differential diagnosis for patients presenting a subcutaneous mass, especially in endemic regions. In order to avoid such complications, more preventive measures and public health education are mandatory.
Declaration of Competing Interest
None.
Funding
None.
Ethical approval
Given the nature of the article, a case report, no ethical approval was required.
Consent
Written informed consent was obtained from the patient for publication of this case and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Author contribution
Houcine Maghrebi: Writing – original draft.
Ahmed Ben Mahmoud: Writing – original draft.
Amin Sebei: Writing – original draft.
Anis Haddad: Study concept and design.
Youssef Chaker: Project administration.
Wael Rebei: Supervision.
Sarra Cheikhrouhou: Writing – original draft; Data interpretation of the pathological findings.
Seif Boukriba: Data interpretation of the radiological findings.
Bedis Jeribi: Methodology.
Montasser Kacem: Supervision.
Registration of research studies
Not applicable.
Guarantor
Ahmed Ben Mahmoud.
Provenance and peer review
Not commissioned, externally peer-reviewed.
Acknowledgements
Not applicable.
Contributor Information
Houcine Maghrebi, Email: houcine.maghrebi@fmt.utm.tn.
Ahmed Ben Mahmoud, Email: ahmed.benmahmoud92@gmail.com.
Anis Haddad, Email: haddad.anis2013@gmail.com.
Sarra Cheikhrouhou, Email: sarra.cheikhrouhou@fmt.utm.tn.
Amine Sebei, Email: aminesebei@gmail.com.
Youssef Chaker, Email: youssef.chaker2@gmail.com.
Seif Boukriba, Email: seif.boukriba@fmt.utm.tn.
Bedis Jeribi, Email: bedisjeribii@yahoo.com.
Wael Rebai, Email: rebaiwael@gmail.com.
Montasser Jameleddine Kacem, Email: kacem_montasser@yahoo.fr.
References
- 1.Garcea G., Rajesh A., Dennison A.R. Surgical management of cystic lesions in the liver. ANZ J. Surg. 2013;83:3–20. doi: 10.1111/j.1445-2197.2012.06096.x. [DOI] [PubMed] [Google Scholar]
- 2.Hamamci E.O., Besim H., Korkmaz A. Unusual locations of hydatid disease and surgical approach. ANZ J. Surg. 2004;74:356–360. doi: 10.1111/j.1445-1433.2004.02981.x. [DOI] [PubMed] [Google Scholar]
- 3.Makni A., Jouini M., Kacem M., Ben Safta Z. Extra-hepatic intra-abdominal hydatid cyst: Which characteristic, compared to the hepatic location? Updates Surg. 2013;65:25–33. doi: 10.1007/s13304-012-0188-6. [DOI] [PubMed] [Google Scholar]
- 4.Yang G., Wang X., Mao Y., Liu W. Case report of primary retroperitoneal hydatid cyst. Parasitol. Int. 2011;60:333–334. doi: 10.1016/j.parint.2011.04.002. [DOI] [PubMed] [Google Scholar]
- 5.Agha R.A., Borrelli M.R., Farwana R., Koshy K., Fowler A., Dennis P. The SCARE 2018 Statement: Updating Consensus Surgical case report (SCARE) Guidelines. Int. J. Surg. 2018;60:132–136. doi: 10.1016/j.ijsu.2018.10.028. [DOI] [PubMed] [Google Scholar]
- 6.Jayant K., Agrawal S., Agarwal R., Dayama K.G. Spontaneous external fistula: the rarest presentation of hydatid cyst. BMJ Case Rep. 2014;2014 doi: 10.1136/bcr-2014-203784. bcr2014203784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Baraket O., Moussa M., Ayed K., Kort B., Bouchoucha S. Predictive factors of morbidity after surgical treatment of hydatid cyst of the liver. Arab J. Gastroenterol. 2014;15:119–122. doi: 10.1016/j.ajg.2014.05.004. [DOI] [PubMed] [Google Scholar]
- 8.Akbulut S. Parietal complication of the hydatid disease comprehensive literature review. Medicine (United States) 2018;97 doi: 10.1097/MD.0000000000010671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mandolkar S., R. B, A. PL, S. GT Cystocutaneous fistula of the left lobe of liver: an extremely rare presentation of hydatid liver cyst. Int. Surg. J. 2015;2:109. doi: 10.5455/2349-2902.isj20150224. [DOI] [Google Scholar]
- 10.Kjossev K., Teodosiev I. Cutaneous fistula of liver echinococcal cyst previously misdiagnosed as fistulizated rib osteomyelitis. Trop. Parasitol. 2013;3:161. doi: 10.4103/2229-5070.122150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gharbi H.A., Hassine W., Brauner M.W., Dupuch K. Ultrasound examination of the hydatic liver. Radiology. 1981;139:459–463. doi: 10.1148/radiology.139.2.7220891. [DOI] [PubMed] [Google Scholar]
- 12.Salerno S., Cracolici E., Lo Casto A. Subcutaneous rupture of hepatic hydatid cyst: CT findings. Dig. Liver Dis. 2006;38:619–620. doi: 10.1016/j.dld.2006.02.018. [DOI] [PubMed] [Google Scholar]
- 13.Bedioui H., Ayari H., Bouslama K., Maghrebi H., Hsairi H., Jouini M., Kacem J.M., Ben Safta Z. Les facteurs prédictifs de récidive du kyste hydatique du foie : L’expérience tunisienne. Bull. La Soc. Pathol. Exot. 2012;105:265–269. doi: 10.1007/s13149-012-0243-z. [DOI] [PubMed] [Google Scholar]