Abstract
Background:
Candida species are a group of coexistent microorganisms in the oral cavity that opportunistically cause disease in vulnerable people, including addicts. This study is aimed at identifying and determining the frequency of Candida species in the oral cavity of the addicts to inform the epidemiological panel and to warn to prevent the resistance of the species.
Materials and Methods:
In this study, sampling was done from the oral cavity of 83 addicts who referred to Addiction Treatment Centers in Isfahan, Iran, using moist sterile swab. The presence of yeast on the direct microscope slides of 58 samples was confirmed. To carry out culture and the primary identification, Sabouraud dextrose agar medium with chloramphenicol as well as HiCrome Candida agar medium was used. Isolates were identified by polymerase chain reaction (PCR) restriction fragment length polymorphism (using specific primers ITS1-ITS4 and MSP I enzyme) and Duplex PCR test (using specific primers CDU1-CDU2/CAL1-CAL2).
Results:
Out of 93 Candida isolates which had been isolated from 58 culture-positive samples of the oral cavity, Candida albicans (41.93%) were the most prevalent species, followed by Candida dubliniensis (24.73%), Candida glabrata (21.50%), Candida kefyr (8.60%), Candida tropicalis (2.15%), and Candida parapsilosis (1.07%), respectively. In 33 cases (56.90%), the presence of more than one Candida species was observed.
Conclusion:
Compared to the studies conducted on the oral cavity of healthy controls, smoking certain drugs can have a significant effect on the presence and frequency of Candida species, particularly C. dubliniensis and C. glabrata.
Keywords: Addiction, Candida, oral cavity, polymerase chain reaction, restriction fragment length polymorphism
Introduction
The human oral cavity is naturally the habitat of microorganisms such as yeast-like Candida, which in natural conditions without developing diseases, coexists with other microorganisms present in the flora of this region. Generally, about 25%–75% of people have oral Candida flora.[1,2,3] The genus Candida contains 150 species, among which there are >20 important medical species.[4] The most yeasts which are commonly separated from the oral cavity are Candida albicans (47%–75%), Candida tropicalis (7%), Candida glabrata (7%), and Candida parapsilosis, Candida krusei, and Candida guilliermondii, each <5%.[5]
Candida species, like other opportunistic fungi, are capable of causing infection due to the initial physiological and immunologic host weakness or genetic and underlying factors.[6] Among the underlying factors which cause these opportunistic diseases are: diabetes, immunodeficiency syndrome, soft tissue injury, loss of natural defensive barriers, dryness and lack of saliva, artificial teeth, smoking cigarettes, and addiction. The infection resulting from Candida is called candidiasis, which is one of the most common opportunistic infections of the oral cavity and has several types.[7,8] One of the important underlying factors which lead to candidiasis is addiction.[9,10] Addiction to drugs is defined as the condition in which the drug abusers restrict their goals to searching for the drugs, its abuse and enjoying it, as well as continuing all these, although their undesirable and troublesome side effects. Indeed, addiction is a chronic, progressive, reversible, and destructive disease that creates many structural and functional changes in the brain and affects all aspects of the drug abusers', their families, and relatives' lives.[11,12]
Addiction is the result of a series of interactions that arise from drug abuse and its reciprocal internal and external effects on an individual. In this case, drug abuse turns to be an impetus in the individual's life.[13] Addictive drugs are classified in a variety of ways; one of the most widely-used methods categorizes the drugs into seven groups: drugs, stimulants, hallucinogenic drugs, cannabis or cannabinoids, sedative-hypnotic medications, alcohol family and ultimately inhalable family such as ether and gasoline. Instances of narcotics include opium, sap, burned opium, heroin, heroin crystals, and morphine. Cocaine, crack cocaine, amphetamines, and methamphetamine can also be mentioned as instances of stimulants.[14] Addictive drugs can be used orally as well as through smoking, inhalation, and injection. Smoking is mostly common for narcotics, stimulants, and cannabinoids family.[15] Today, addiction is considered as an increasing problem for health and public hygiene due to the prevalence of various complications and infections.[16,17] The previous studies depicted that oral lesions were more prevalent in drug users compared to the general public.[10] There is a long and recognized relationship between addiction and an increase in the level of infection, including fungal infections.[18,19] Concerning the current claims, with weakening the immune system, addiction provides conditions for the development of chronic infections such as oral thrush or candidiasis.[20,21] A plethora of previous studies indicates that oral candidiasis is one of the most common oral infections, particularly in individuals with weakened immune systems, including addicts, and in some cases, as it becomes resistant to treatment, it creates certain problems.[20,22] The application of certain substances lead to changes such as Candidiasis, frictional hyperkeratosis, gingivostomatitis, aphthous stomatitis, and herpes simplex, which are normally found in the oral mucosa.[23]
C. albicans is one of the most prevalent Candida species in the oral cavity of healthy and sick individuals and is generally known as a dominant pathogenic species in sensitive hosts.[22,24] Recently, it has been noted that dissemination of Candida through the mouth is one of the reasons for the development of Candida disseminated infections in immunocompromised patients.[25,26] For example, esophageal candidiasis, a common symptom in addicts, especially crack abusers who are infected with AIDS, usually occurs following the dissemination of oral lesions. In Nature et al.'s study, the prevalence amount of esophagus' Candidiasis in HIV-positive patients who also used crack cocaine was reported to be 11.6%, whereas such prevalence amount was 1.2% in HIV-positive patients who had not abused crack cocaine. The findings of this study revealed that this prevalence degree of was reported 3% among the patients who had already had crack cocaine abuse.[27] The results of Freire-Garabal et al.'s experimental studies, which explored the impacts of amphetamine on the advancement of oral candidiasis in rats, indicated a remarkable increase in the number of C. albicans, the percentage of developed lesions on the surfaces of the tongue, the percentage of unnatural papillae as well as the presence of mycelium threads in tissue sections of the tongue. While Freire-Garabal et al.'s previous studies showed that amphetamine had no statistically significant effects on the latter two.[28]
Nowadays, the occurrence of systemic candidiasis is considerably increasing and it is recognized that many of these infections are caused by non-albicans Candida species, which play an important role, particularly in the development of candidemia and invasive candidiasis.[29] Non-albicans candida agents, in comparison to C. albicans ones, are more resistant to common fungal drugs. For example, according to certain studies, C. glabrata has intrinsic resistance to the azoles combinations, whereas Candida dubliniensis has relative resistance to such combinations.[30,31] The uncontrolled and unconventional use of antifungal drugs makes the species resistant and increases drug resistance, causing a lot of problems.
Considering the above, since addiction can be considered as a predisposing factor for the development of candidiasis and given the fact that simple and systemic Candida infections are caused by commensal species, and many of the species have a variable susceptibility pattern to certain common antifungal drugs.[32,33] The aim of this study was to determine the frequency of Candida species isolated from the oral cavity of drug smokers regarding the type of drug abusing.
Materials and Methods
The present study was an epidemiological descriptive-inferential study that examined 83 narcotic and stimulant drug abusers in Isfahan, Iran. Sampling was done beside the flame by two moist sterile cotton swabs that were simultaneously rotated on the internal surfaces of the whole oral cavity, above and under the tongue. After sampling, one of the swabs was immediately cultured through the sweep-plate method on a Sabouraud dextrose agar medium with chloramphenicol (Merck-Germany), and another swab was used to prepare direct microscope slides stained with Giemsa. The without-yeast samples on direct microscope slides were excluded from the study. Plates were kept at a temperature of 30°C for 48 h, and their growth rate and form of the colonies were examined.
Differentiation of Candida species by phenotypic method
After purification, for the initial detection and isolation of the mixed species, the colonies were cultured on HiCrome Candida agar (HiMedia, Mumbai, India). The isolates were identified based on the colors introduced in the manufacturer catalog [Figure 1]. Some of the mixed species were purified again in HiCrome Candida agar medium due to color mixing.
Figure 1.

Appearance color of Candida colonies, isolated from the mouth of drug smoker addicts on CHROMagar Candida medium No. 1 shows Candida tropicalis, no. 2, 4, 6, 7, 9, 10 and 11 indicate albicans/dubliniensis complex, no. 3, 5 and 8 demonstrate Candida glabrata and no. 12 shows a non-albicans Candida species
Identification of Candida species using polymerase chain reaction-restriction fragment length polymorphism method
As the CHROMagar culture medium was not specialized for all Candida species, molecular methods were used to confirm the initial detections and to identify the species more accurately.
DNA extraction
In the current research, considering the previous studies, extraction of DNA was carried out via boiling method,[34] through which a loop of the fresh colony was transferred into 1.5 mL microtubes containing 100 μl sterile distilled water. After it was mixed, it was heated at 90°C for 20 min in a bain-marie. Subsequently, the microtubues were centrifuged at 10,000 rpm for 10 min and the supernatant containing crude DNA was transferred to 0.2 mL microtubes to be used in molecular tests.
Selection of primers and the target DNA
Replication of the gene responsible for coding ribosomal RNA (rDNA) located in the ITS1-5.8S-ITS2 region was also used in this study. Primers ITS1 and ITS4, with the following sequence, were selected as forward (ITS1) and reverse (ITS4) primers.[35]
ITS1 5´ TCCGTAGGTGAACCTGCGG 3´
ITS4 TCCTCCGCTTATTGATATGC 3´
Polymerase chain reaction process
To carry out the PCR reaction for each sample, a mixture of 12.5 μl of ready-to-use Master Mix (AMPLIQON, Denmark), 3 μL of DNA template, 0.5 μl of both primers (concentrated at 10 pmol), and 8.5 μl of sterile double distilled water were prepared to obtain 25 μL final volume per reaction.
The PCR process during the temperature cycle consists of: an initial denaturation cycle at 94°C for 5 min, followed by 34 consecutive cycles composed of 30 s denaturation at 94°C, annealing at 55°C for 45 s, and extension at 72°C for 1 min. These cycles were followed by a cycle at 72°C for 7 min as the final extension.
The amplicon, which resulted from PCR was loaded in 1.5% Agarose gel and electrophoresis was run on it at 80 volts for 45–60 min. The gel was placed in a special position in the ultraviolet (UV) doc, and the image of the bands was checked on the monitor and recorded [Figure 2a].
Figure 2.
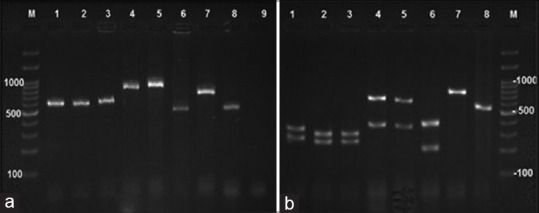
Electrophoresis of polymerase chain reaction and polymerase chain reaction-restriction fragment length polymorphism products of some isolates of this study left (a) Electrophoresis of polymerase chain reaction products of Candida isolates using primers ITS 1 and ITS 4 right (b) Electrophoresis of polymerase chain reaction products of Candida isolates after endonuclease digestion with MSPI No. 1-3 show Candida albicans, 4 and 5 Candida glabrata, 6: Candida tropicalis, 7: Candida kefyr, 8: Candida parapsilosis. 9: indicates the negative control and M denotes 100 bp fragments
Restriction fragment length polymorphism process
At this stage, the MSPI enzyme was used to cut PCR products. For each 15 μl reaction, 10 μl of PCR product, 3 μl of water, 1.5 μl of buffer and 0.5 μl of the MSPI enzyme were mixed. The microtubes containing the prepared ingredients were incubated at 37°C for 1 h. Finally, the products were loaded in 2% agarose gel.
To run electrophoresis, the bands which had been formed were observed under UV light of the UV doc and were interpreted for each sample considering the scale of the applied marker and the existing standards [Table 1 and Figure 2b].
Table 1.
Results of the polymerase chain reaction-restriction fragment length polymorphismprocess for all oral isolates of this study
| Candida species | Amplicon molecular weight | Molecular weight(s) of restriction product(s) | n |
|---|---|---|---|
| Candida albicans | 535 | 238-279 | 53 |
| Candida glabrata | 871 | 314-557 | 20 |
| Candida kefyr | 721 | 721 | 8 |
| Candida tropicalis | 524 | 184-340 | 2 |
| Candida parapsilosis | 520 | 520 | 1 |
Duplex-polymerase chain reaction
Concerning the inability of the MspI enzyme to differentiate C. albicans from C. dubliniensis, the differentiation of these two species was done by duplex PCR (dPCR) using specific primers CDU1-CDU2/CAL1-CAL2, and the results were previously reported.[25]
Data analysis
After conducting all the aforementioned research processes, the data were entered in the SPSS software (SPSS, Inc., Chicago, IL, USA, version 23), and the data were analyzed through descriptive and inferential statistics.
Results
Through the investigation of the colored microscope slides in this study, among 83 samples, the presence of yeast was confirmed on direct microscope slides of 58 samples. The number of colonies from the cultivation of these 58 positive clinical samples varied from 20 to 52,800 on each plate.
Phenotypic investigations
All isolates had the potential to grow in the CHROMagar Candida culture medium, and altogether 84 yeast isolates were isolated in this medium, of which 53 isolates were shown with green and were reported as “albicans/dubliniensis complex,” 20 isolates were shown with purple and were reported as “C. glabrata,” and two isolates were shown with blue and light violet margin and were reported as “C. tropicalis.” Moreover, nine samples were recorded as non-albicans Candida species and were shown with nonspecific colors in white-to-cream spectrum as well as light pink [Figure 1].
Molecular investigations
The results of the PCR-RFLP experiments confirmed the Candida species' identities recognized through phenotypic investigations; furthermore, non-albicans Candida samples were divided into eight Candida kefyr isolates and one C. parapsilosis isolate [Figure 2].
The dPCR assay performed on the samples identified as C. albicans proved the presence of 39 C. albicans and 23 C. dubliniensis isolates.
The frequency and mean of different Candida isolates separated from the mouth of drug smokers, and the type of drugs showed in Table 2.
Table 2.
Frequency of Candida species isolated from the oral cavity of drug smokers regarding the type of drug
| Type of drug | Candida species | Total, n (%) | Mean of colony | |||||
|---|---|---|---|---|---|---|---|---|
| Candida albicans, n (%) | Candida dubliniensis, n (%) | Candida glabrata, n (%) | Candida kefyr, n (%) | Candida tropicalis, n (%) | Candida parpsilosis, n (%) | |||
| Resin | 4 (66.7) | - | - | 2 (33.3) | - | - | 6 (100) | 3367 |
| Opium | 4 (33.3) | 4 (33.3) | 3 (25) | 1 (8.3) | - | - | 12 (100) | 1271 |
| Heroin | 8 (42.1) | 6 (31.6) | 3 (15.8) | 1 (5.3) | 1 (5.3) | - | 19 (100) | 400 |
| Crack cocaine | 3 (30) | 5 (50) | 2 (20) | - | - | - | 10 (100) | 10824 |
| Methamphetamine | 6 (37.5) | 3 (18.7) | 4 (25) | 2 (12.5) | - | 1 (6.25) | 16 (100) | 2095 |
| Opium and methamphetamine | 2 (40) | 1 (20) | 2 (40) | - | - | - | 5 (100) | 395 |
| Heroin and methamphetamine | 9 (53) | 2 (11.8) | 5 (29.4) | - | 1 (5.9) | - | 17 (100) | 4274 |
| Crack cocaine and methamphetamine | 4 (50) | 1 (12.5) | 1 (12.5) | 2 (25) | - | -- | 8 (100) | 1352 |
Discussion
Due to the weak and ineffective immune system, addicts are an important group of vulnerable people against opportunistic infections. With the increasing prevalence of addiction in recent years, we have been witnessing the spread of Candida infections, especially oral candidiasis, among addicts.[36,37] Although oral C. albicans, particularly in the mouth, still remain at the forefront of Candida reports, in recent years, non-albicans species have attracted lots of attention due to an increase in emergence, epidemiological changes, and more resistance.[38] In this study, out of 93 isolates which were identified, 39 isolates (41.93%) were C. albicans, 23 isolates (24.73%) were C. dubliniensis, 20 isolates (21.50%) were C. glabrata, eight isolates (8.60%) were C. kefyr, two isolates (2.15%) were C. tropicalis and only one isolate (1.07%) was C. parapsilosis. In 33 samples (56.96%) of 58 clinical samples taken, more than one Candida species was observed. Considering the remarkable presence of non-albicans species, especially the high degree of C. dubliniensis, which is a rare species, these quantities seem to be a bit thought-provoking. However, the findings of the current study are in line with Hadzic et al.'s study which investigated the frequency of Candida species in the mouth of addicts hospitalized in addiction treatment centers in Bosnia and Herzegovina; they reported the frequency of Candida species as follows: C. albicans (43%), C. dubliniensis (23%), and other Candida species (34%).[39] In the aforementioned study, which is the only study found to be very similar to the present study, after differentiating the results in terms of type of drug abuse; in the 19-member group who abused opioids, C. albicans (47.4%), C. krusei (26.3%), C. dubliniensis (15.8%), C. tropicalis (5.3%) and C. glabrata (5.3%) were observed. Whereas in the 16-member group of alcohol users, C. glabrata (19%) had the highest frequency after C. albicans (37.5%), followed by C. tropicalis and C. krusei, each 6.2% as more frequent species. In this group, the frequency of C. dubliniensis was reported to be 3.25%. Considering that alcohol abuse in Iran is among the top drug dependence[40] and most of the participants in this study also had the background of alcohol abuse, the compound results of both groups are expected. The absence of C. krusei in the present study and the absence of C. kefyr in the study whose findings were compared can be due to differences in the type of drug abused or the regional epidemiological characteristics.
In the study conducted in Suadi Arabia in 2019, Mokeem et al. explored the Candida flora in the oral cavity of smokers as well as users of waterpipe and electronic cigarettes. While separating the C. albicans, C. tropicalis, and C. parapsilosis species, they reported C. albicans as the most prevalent species in all three groups. Although a greater variety of species was reported in the current study probably due to the various used substances and users' hygiene poverty, the presence of all three identified species in both studies can be regarded as a parallel finding in these two studies. Climate conditions and sample size can be among the other effective factors in differences.[41]
Javaheri et al., conducted a study to identify Candida species in smokers' saliva. They reported C. albicans (42.10%) as the most prevalent species followed by C. kefyr and C. krusei. Unlike the current study, they found no isolates of C. paraposilosis, C. glabrata, and C. dubliniensis.[42] Although this study has been carried out on cigarette smokers, the differences in the type of smoking, geographic climate, and method may explain the inconsistencies.
In a research conducted by Heidarian et al., to identify the Candida species isolated from oral lesions of HIV-positive people in Isfahan, C. albicans had the highest frequency (44%) followed by C. glabrata (26.8%), C. dubliniensis (17.1%), C. kefyr (4.8%), and C. Trocopicalis (4.8%).[43] The results of this study are relatively consistent with the findings of the present study. Differences in values seem reasonable due to the differences in the community and immunological disorder. Probably, narcotic and sexual behavior are one of the factors influencing the variety of frequency distribution of Candida species.
Studying a variety of samples of 124 patients with immunodeficiency virus in India, the most frequent of which was oral samples (82 patients), Maheshwari et al., (2016) isolated seven Candida species, including C. albicans and C. dubliniensis and reported C. albicans as the most prevalent species.[44] These results are also relatively consistent with the findings of this study. Studies have shown that, like the results of the present study regarding the simultaneous presence of species, there is a high incidence of mixed infections in people infected with HIV. In a study carried out by Dronda et al. on oral lesions of 12 HIV-infected patients, 7 cases of the simultaneous presence of C. albicans and C. krusei, 4 cases of the simultaneous presence of C. albicans and C. glabrata, and one case of the simultaneous presence of C. albicans and C. Tropicalis were reported.[45] The differences in the species reported in Dronda et al.'s study and those reported in the present study may result from differences in the population under study and time difference because time, as well as medical and pharmaceutical progress, are considered as the key elements in the presence and identification of non-albicans species. In addition, it is worth noting that Dronda et al.'s study, contrary to the present study, was carried out on individuals with oral lesions, which can be an important reason for differences in species.
The similarity of the results of this study, which was conducted on oral samples of addicts, to the studies conducted on people infected with the HIV virus, can be due to the physiological and immunological similarities of these two groups of people as well as the probability of co-occurrence of AIDS and addiction. Studies have denoted that drugs have a very destructive effect on the immune system and generally there is a direct relationship among the interaction of addiction, ineffectiveness of the immune system, increased pathogen acquisition, creation of different patterns in the development of diseases and chronic infections.[19,46,47,48,49] The HIV and drug use both significantly affect cellular immunity and especially T lymphocytes so that they interfere with the ratio of CD4+/CD8+ cells while decreasing CD4+ cells.[21,50,51] It seems that geographical climate, time, underlying factors, population and type of the sample under study as well as the method used can probably contribute to the presence of various species of Candida in communities and the reason for the differences between the results of the present study and the findings of the inconsistent studies.
Conclusion
This study clearly showed the noticeable presence of C. albicans and non-albicans species such as resistant C. glabrata and C. dubliniensis in oral samples of drug smokers, which could be a warning for the presence of resistant species in the abusers who smoke drugs.
Financial support and sponsorship
The following study was performed with a Grant (No. 394770) from Research Deputy of Isfahan University of Medical Sciences.
Conflicts of interest
There are no conflicts of interest
Acknowledgments
We express our thanks to all participants, as well as the staff and authorities of the Addiction Treatment Centers, collaborating with this project. We would also like to express our sincere appreciation to Dr. Hooman Manshaei, the head of the Scientific Community of Addiction Therapists of Isfahan, Iran, for his notable assistance in coordinating for sampling.
References
- 1.Anaissie E, McGinnis M, Pfaller M. Clinical Mycology. Churchill Livingstone: London, UK: Elsevier Health Sciences; 2009. [Google Scholar]
- 2.Ranjan K, Poças-Fonseca MJ. Microbial Diversity in Ecosystem Sustainability and Biotechnological Applications. Singapore: Springer; 2019. Genetic diversity of pathogenic yeasts; pp. 593–615. [Google Scholar]
- 3.AL-Janabi AA, Al-Mosawe HA, Karrar AM. Yeasts: One member of the normal flora of the oral cavity. Int J Med Sci Curr Res. 2019;2:345. [Google Scholar]
- 4.Theill L, Dudiuk C, Morano S, Gamarra S, Nardin ME, Méndez E, et al. Prevalence and antifungal susceptibility of Candida albicans and its related species Candida dubliniensis and Candida africana isolated from vulvovaginal samples in a hospital of Argentina. Rev Argent Microbiol. 2016;48:43–9. doi: 10.1016/j.ram.2015.10.003. [DOI] [PubMed] [Google Scholar]
- 5.Vázquez-González D, Perusquía-Ortiz AM, Hundeiker M, Bonifaz A. Opportunistic yeast infections: Candidiasis, cryptococcosis, trichosporonosis and geotrichosis. J Dtsch Dermatol Ges. 2013;11:381–93. doi: 10.1111/ddg.12097. [DOI] [PubMed] [Google Scholar]
- 6.Polvi EJ, Li X, O'Meara TR, Leach MD, Cowen LE. Opportunistic yeast pathogens: Reservoirs, virulence mechanisms, and therapeutic strategies. Cell Mol Life Sci. 2015;72:2261–87. doi: 10.1007/s00018-015-1860-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mobeen N. Oral candidiasis – A short review. Int J Curr Res Rev. 2014;6:89. [Google Scholar]
- 8.Vila T, Sultan AS, Montelongo-Jauregui D, Jabra-Rizk MA. Oral candidiasis: A disease of opportunity. J Fungi (Basel) 2020;6(1):15. doi: 10.3390/jof6010015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Leen CL, Brettle RP. Fungal infections in drug users. J Antimicrob Chemother. 1991;28(Suppl A):83–96. doi: 10.1093/jac/28.suppl_a.83. [DOI] [PubMed] [Google Scholar]
- 10.Valadas LAR, Fernandes ML, Silva MI, Citó C, Maia IC, de Carvalho MR, et al. Oral manifestations of drug abuse: A review of literature. J Young Pharm. 2020;12:483. [Google Scholar]
- 11.Hser YI, Hoffman V, Grella CE, Anglin MD. A 33-year follow-up of narcotics addicts. Arch Gen Psychiatry. 2001;58:503–8. doi: 10.1001/archpsyc.58.5.503. [DOI] [PubMed] [Google Scholar]
- 12.MacLeod CM. The stroop task: The gold standard of attentional measures. J Exp Psychol Gen. 1992;121:12–4. [Google Scholar]
- 13.Shelby CL. Addiction and Meaning Addiction Palgrave Macmillan. London: Springer; 2016. pp. 101–21. [Google Scholar]
- 14.Association American Psychiatric. Diagnostic and Statistical Manual of Mental Disorders (DSM-5®) Washington, DC, USA: American Psychiatric Publishing; 2013. [Google Scholar]
- 15.Brown SA, Myers MG, Lippke L, Tapert SF, Stewart DG, Vik PW. Psychometric evaluation of the customary drinking and drug use record (CDDR): A measure of adolescent alcohol and drug involvement. J Stud Alcohol. 1998;59:427–38. doi: 10.15288/jsa.1998.59.427. [DOI] [PubMed] [Google Scholar]
- 16.Hussey HH, Katz S. Infections resulting from narcotic addiction; report of 102 cases. Am J Med. 1950;9:186–93. doi: 10.1016/0002-9343(50)90021-0. [DOI] [PubMed] [Google Scholar]
- 17.Lo TW, Yeung JW, Tam CH. Substance abuse and public health: A multilevel perspective and multiple responses. Int J Environ Res Public Health. 2020;17:2610. doi: 10.3390/ijerph17072610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sapira JD. The narcotic addict as a medical patient. Am J Med. 1968;45:555–88. doi: 10.1016/0002-9343(68)90172-1. [DOI] [PubMed] [Google Scholar]
- 19.Friedman H, Pross S, Klein TW. Addictive drugs and their relationship with infectious diseases. FEMS Immunol Med Microbiol. 2006;47:330–42. doi: 10.1111/j.1574-695X.2006.00097.x. [DOI] [PubMed] [Google Scholar]
- 20.Nucci M, Marr KA. Emerging fungal diseases. Clin Infect Dis. 2005;41:521–6. doi: 10.1086/432060. [DOI] [PubMed] [Google Scholar]
- 21.Moyano J, Aguirre L. Opioids in the immune system: From experimental studies to clinical practice. Rev Assoc Mé Bras. 2019;65:262–9. doi: 10.1590/1806-9282.65.2.262. [DOI] [PubMed] [Google Scholar]
- 22.Farah CS, Lynch N, McCullough MJ. Oral fungal infections: An update for the general practitioner. Aust Dent J. 2010;55(Suppl 1):48–54. doi: 10.1111/j.1834-7819.2010.01198.x. [DOI] [PubMed] [Google Scholar]
- 23.Goel D, Patthi B, Singla A, Malhi R, Chaudhary PK, Khan A. Assessment of knowledge and attitude regarding management of patients with substance usage in dental clinics in Modinagar – A cross-sectional study. J Family Med Prim Care. 2019;8:3683–8. doi: 10.4103/jfmpc.jfmpc_733_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Keboa MT, Enriquez N, Martel M, Nicolau B, Macdonald ME. Oral health implications of cannabis smoking: A rapid evidence review. J Can Dent Assoc. 2020;86:k2. [PubMed] [Google Scholar]
- 25.Abharian PH, Dehghan P, Abharian PH, Tolouei S. Molecular characterization of Candida dubliniensis and Candida albicans in the oral cavity of drug abusers using duplex polymerase chain reaction. Curr Med Mycol. 2018;4:12–7. doi: 10.18502/cmm.4.1.29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Li X, Kolltveit KM, Tronstad L, Olsen I. Systemic diseases caused by oral infection. Clin Microbiol Rev. 2000;13:547–58. doi: 10.1128/cmr.13.4.547-558.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Nacher M, Adenis A, Hanf M, Adriouch L, Vantilcke V, El Guedj M, et al. Crack cocaine use increases the incidence of AIDS-defining events in French Guiana. AIDS. 2009;23:2223–6. doi: 10.1097/QAD.0b013e32833147c2. [DOI] [PubMed] [Google Scholar]
- 28.Freire-Garabal M, Núñez MJ, Balboa J, Rodríguez-Cobo A, López-Paz JM, Rey-Méndez M, et al. Effects of amphetamine on development of oral candidiasis in rats. Clin Diagn Lab Immunol. 1999;6:530–3. doi: 10.1128/cdli.6.4.530-533.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Maheronnaghsh M, Tolouei S, Dehghan P, Chadeganipour M, Yazdi M. Identification of Candida species in patients with oral lesion undergoing chemotherapy along with minimum inhibitory concentration to fluconazole. Adv Biomed Res. 2016;5:132. doi: 10.4103/2277-9175.187394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Fidel PL, Vazquez JA, Sobel JD. Candida glabrata: Review of epidemiology, pathogenesis, and clinical disease with comparison to C. albicans. Clin Microbiol Rev. 1999;12:80–96. doi: 10.1128/cmr.12.1.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Golirad N, Fozouni L, Pordeli H. Evaluation of susceptibility to fluconazole and voriconazole in oral Candida glabrata isolates from drug addicts. Int J High Risk Behav Addict. 2019;8(4):e92807. [Google Scholar]
- 32.Ramani R, Chaturvedi V. Flow cytometry antifungal susceptibility testing of pathogenic yeasts other than Candida albicans and comparison with the NCCLS broth microdilution test. Antimicrob Agents Chemother. 2000;44:2752–8. doi: 10.1128/aac.44.10.2752-2758.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Yang YL, Li SY, Cheng HH, Lo HJ TSARY Hospitals. The trend of susceptibilities to amphotericin B and fluconazole of Candida species from 1999 to 2002 in Taiwan. BMC Infect Dis. 2005;5:99. doi: 10.1186/1471-2334-5-99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Silva GA, Bernardi TL, Schaker PD, Menegotto M, Valente P. Rapid yeast DNA extraction by boiling and freeze-thawing without using chemical reagents and DNA purification. Braz Arch Biol Technol. 2012;55:319–27. [Google Scholar]
- 35.Mirhendi H, Makimura K, Khoramizadeh M, Yamaguchi H. A one-enzyme PCR-RFLP assay for identification of six medically important Candida species. Nihon Ishinkin Gakkai Zasshi. 2006;47:225–9. doi: 10.3314/jjmm.47.225. [DOI] [PubMed] [Google Scholar]
- 36.Majima T, Ito-Kuwa S, Nagatomi R, Nakamura K. Study of the oral carriage of Candida sp in dental students and staff – Identification of Candida sp and background survey. Oral Sci Int. 2014;11:30–4. [Google Scholar]
- 37.Mohammadi R, Mirhendi H, Rezaei-Matehkolaei A, Ghahri M, Shidfar MR, Jalalizand N, et al. Molecular identification and distribution profile of Candida species isolated from Iranian patients. Med Mycol. 2013;51:657–63. doi: 10.3109/13693786.2013.770603. [DOI] [PubMed] [Google Scholar]
- 38.Gutiérrez J, Morales P, González MA, Quindós G. Candida dubliniensis, a new fungal pathogen. J Basic Microbiol. 2002;42:207–27. doi: 10.1002/1521-4028(200206)42:3<207::AID-JOBM207>3.0.CO;2-C. [DOI] [PubMed] [Google Scholar]
- 39.Hadzic S, Dedic A, Gojkov-Vukelic M, Mehic-Basara N, Hukic M, Babic M, et al. The effect of psychoactive substances (drugs) on the presence and frequency of oral Candida species and Candida dubliniensis. Mater Sociomed. 2013;25:223–5. doi: 10.5455/msm.2013.25.223-225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Mokri A. Brief overview of the status of drug abuse in Iran. Arch Iranian Med. 2002;5:184–90. [Google Scholar]
- 41.Mokeem SA, Abduljabbar T, Al-Kheraif AA, Alasqah MN, Michelogiannakis D, Samaranayake LP, et al. Oral Candida carriage among cigarette- and waterpipe-smokers, and electronic cigarette users. Oral Dis. 2019;25:319–26. doi: 10.1111/odi.12902. [DOI] [PubMed] [Google Scholar]
- 42.Javaheri M, Mohammadi F, Chadeganipour M, Nekoian S, Dehghan P. Identification of Candida species in oral cavity of smokers and nonsmokers. J Isfahan Med School. 2015;33:2105–10. [Google Scholar]
- 43.Heidarian A, Dehghan P, Chadeganipour M, Tayeri K. Frequency of Candida species isolated from the oral cavity of HIV-infected patients referring to behavioral disease counseling center of Isfahan in 2017-2018. SJKU. 2019;24:30–41. [Google Scholar]
- 44.Maheshwari M, Kaur R, Chadha S. Candida species prevalence profile in HIV seropositive patients from a major tertiary care hospital in New Delhi, India. J Pathog. 2016;2016:1–8. doi: 10.1155/2016/6204804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Dronda F, Alonso-Sanz M, Laguna F, Chaves F, Martínez-Suárez JV, Rodríguez-Tudela JL, et al. Mixed oropharyngeal candidiasis due to Candida albicans and non-albicans Candida strains in HIV-infected patients. Eur J Clin Microbiol Infect Dis. 1996;15:446–52. doi: 10.1007/BF01691310. [DOI] [PubMed] [Google Scholar]
- 46.Friedman H, Newton C, Klein TW. Microbial infections, immunomodulation, and drugs of abuse. Clin Microbiol Rev. 2003;16:209–19. doi: 10.1128/CMR.16.2.209-219.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Yu Q, Zhang D, Walston M, Zhang J, Liu Y, Watson RR. Chronic methamphetamine exposure alters immune function in normal and retrovirus-infected mice. Int Immunopharmacol. 2002;2:951–62. doi: 10.1016/s1567-5769(02)00047-4. [DOI] [PubMed] [Google Scholar]
- 48.Anwar KP, Malik A, Subhan KH. Profile of candidiasis in HIV infected patients. Iran J Microbiol. 2012;4:204–9. [PMC free article] [PubMed] [Google Scholar]
- 49.Irwin MR, Olmos L, Wang M, Valladares EM, Motivala SJ, Fong T, et al. Cocaine dependence and acute cocaine induce decreases of monocyte proinflammatory cytokine expression across the diurnal period: Autonomic mechanisms. J Pharmacol Exp Ther. 2007;320:507–15. doi: 10.1124/jpet.106.112797. [DOI] [PubMed] [Google Scholar]
- 50.Katiraee F, Khosravi AR, Khalaj V, Hajiabdolbaghi M, Khaksar AA, Rasoulinejad M, et al. Oral candidiasis in human immunodeficiency virus (HIV) infected individuals in Iran. Tehran Univ Med J. 2010;68:37–44. [Google Scholar]
- 51.Vivancos-Gallego MJ, Okhai H, Perez-Elías MJ, Gomez-Ayerbe C, Moreno-Zamora A, Casado JL, et al. CD4+:CD8+ T-cell ratio changes in people with HIV receiving antiretroviral treatment. Antivir Ther. 2020 doi: 10.3851/IMP3354. 103851/IMP3354 [published online ahead of print, 2020 Apr 27] [DOI] [PubMed] [Google Scholar]


