Abstract
Background
The COVID-19 pandemic and related social distancing public health recommendations will have indirect consequences for individuals with current and remitted substance use disorder (SUD). Not only will stressors increase risk for symptom exacerbation and/or relapse, but individuals will also have limited service access during this critical time. Individuals with SUD are using free, online digital recovery support services (D-RSS) that leverage peer-to-peer connection (i.e., social-online D-RSS) which simultaneously help these individuals to access support and adhere to public health guidelines. Barriers to SUD treatment and recovery support service access, however, are not unique to the COVID-19 epoch. The pandemic creates an opportunity to highlight problems that will persist beyond its immediate effects, and to offer potential solutions that might help address these long-standing, systemic issues. To help providers and other key stakeholders effectively support those interested in, or who might benefit from, participation in free, social-online D-RSS, this review outlines the following: 1) theories of expected therapeutic benefits from, and potential drawbacks of social-online D-RSS participation; 2) a typology that can be used to describe and classify D-RSS; 3) a D-RSS “case study” to illustrate how to apply the theory and typology; 4) what is known empirically about social-online D-RSS; and 5) whether and how to engage individuals with these online resources.
Method
Narrative review combining research and theory on both in-person recovery supports and social-online D-RSS.
Results
Studies examining in-person recovery support services, such as AA and other mutual-help organizations, combined with theory about how social-online D-RSS might confer benefit, suggest these digital supports may engage individuals with SUD and mobilize salutary change in similar ways. While people may use in-person and digital supports simultaneously, when comparing the two modalities, communication science and telemedicine group therapy data suggest that D-RSS may not provide the same magnitude of benefit as in-person services. D-RSS can be classified based on the a) type of service, b) type of platform, c) points of access, and d) organizations responsible for their delivery. Research has not yet rigorously tested the effectiveness of social-online D-RSS specifically, though existing data suggest that those who use these services generally find their participation to be helpful. Content analyses suggest that these services are likely to facilitate social support and unlikely to expose individuals to harmful situations.
Conclusions
When in-person treatment and recovery support services are limited, as is the case during the COVID-19 pandemic, expected therapeutic benefits and emerging data, taken together, suggest providers, mentors, and other community leaders may wish to refer individuals with current and remitted SUD to free, social-online D-RSS. Given the array of available services in the absence of best practice guidelines, we recommend that when making D-RSS referrals, stakeholders familiarize themselves with theorized benefits and drawbacks of participation, use a typology to describe and classify services, and integrate current empirical knowledge, while relying on trusted federal, academic, and national practice organization resource lists.
Keywords: Mutual-help organizations, Digital recovery support services, Telemedicine, COVID-19
1. Introduction
The COVID-19 pandemic, caused by a novel coronavirus, SARS-CoV-2, will have many indirect consequences for individuals with current or remitted alcohol and other drug use disorders (i.e., substance use disorder; SUD) in the United States. These indirect consequences are in addition to direct risks of contracting the infection. In response to the pandemic, the United States' public health policy of “social distancing” (Centers for Disease Control and Prevention [CDC], 2020) has introduced new challenges for those with SUD, including, but not limited to, reduced access to SUD treatment and recovery support services. Thus, the disruption of SUD service provision further magnifies increased risk for exacerbation or recurrence of SUD symptoms due to stress and other negative affective states (Marlatt, 1996; Ramo & Brown, 2008) that the pandemic causes.
Issues with limited access to services during high stress times are not unique to the COVID-19 epoch, however; the pandemic offers an opportunity to highlight and address problems, and potential solutions, that will persist beyond this public health crisis. More specifically, telemedicine and online, digital recovery support services (D-RSS) have taken center stage as potential solutions for individuals who are increasingly unable to access SUD treatment and recovery support services in person. Given the expansive reach of D-RSS, greater understanding of whether, and for whom, they are helpful may enhance the field's public health response to SUD more broadly.
At any given time, many millions of Americans with substance use problems depend on recovery support services that leverage peer-to-peer connection. Attendance at mutual-help organizations (MHOs), such as Alcoholics Anonymous (AA) and SMART Recovery, is the most common form of help-seeking for all professional and nonprofessional services among individuals with current SUD as well as those who have resolved a substance use problem (Grant et al., 2015; Grant et al., 2016; Kelly et al., 2017). Other more comprehensive recovery support services that may link to, but are not synonymous with, MHOs, such as recovery community centers (Kelly, Fallah-Sohy, et al., 2020; Kelly, Stout, et al., 2020) and educational recovery services like collegiate recovery programs (Laudet et al., 2014; Laudet et al., 2015) also rely on peer-to-peer recovery support and will be negatively impacted by social distancing. Thus, for millions of people in the US, as well as millions internationally, the COVID-19 pandemic and its related public health response have increased stress and constrained access to SUD services and recovery-related social support, thereby amplifying the risk for negative health outcomes.
Free, online D-RSS that leverage peer-to-peer connection (i.e., social-online D-RSS)—including online video recovery support meetings, discussion boards and chat rooms, and social network sites—may be critical resources in helping to address these unintended consequences. By complementing in-person services on which many individuals with SUD have come to rely, social-online D-RSS can provide access to services that are both free (to the end-user) and may help to prevent SUD exacerbation or relapse while adhering to public health guidelines during this global pandemic.
To aid treatment providers, administrators, policy-makers, mentors, and other community leaders in most effectively supporting individuals with SUD during this critical time, this primer has the following objectives: to outline the theorized therapeutic benefits one might expect from participation, as well as drawbacks or disadvantages relative to in-person services (Section 2); to propose a typology that can describe an array of social-online D-RSS (Section 3); to present a D-RSS case study outlining how theorized therapeutic benefits may apply, and its classification within the proposed typology (Section 4); to review what is known empirically about D-RSS participation (Section 5); and to recommend whether and how to engage individuals with these digital resources (Section 6).
2. Theorized therapeutic benefits and drawbacks
2.1. Potential benefits
Individuals with alcohol and stimulant use disorder, as well as opioid use disorder in tandem with buprenorphine, benefit from in-person, 12-step MHO attendance and active involvement (Crits-Christoph et al., 1999; Kelly, Humphreys & Ferri, 2020; Rawson et al., 2004; Weiss et al., 2005; Weiss et al., 2019). Emerging research suggests that secular MHOs, too, such as SMART Recovery, may be as effective as 12-step MHOs for those who choose to attend after adjusting for a greater likelihood of nonabstinence goals among secular group attendees (Zemore et al., 2018).
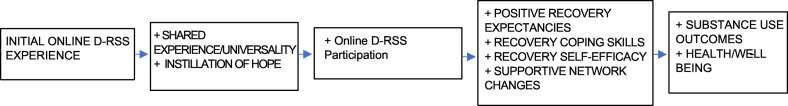
We hypothesize that social-online D-RSS participation will offer clinical and public health benefits based on the potential for these digital supports to engage individuals through similar, salutary group theory processes as in-person MHOs (Labbe et al., 2014) and to mobilize the same helpful therapeutic mechanisms that explain how in-person MHOs promote better SUD outcomes (Kelly, 2017; Kelly et al., 2009; Laudet et al., 2004; Moos, 2008; Tonigan & Rice, 2010). Fig. 1 provides a conceptual model of these potential benefits. It is important to note that this model has not yet been tested for D-RSS, but it does provide a testable scientific framework informed by what is known empirically about in-person recovery supports.
Fig. 1.
Conceptual model theorizing how social-online D-RSS enhance initial engagement and confer benefits. The “+” symbolizes a theorized increase or enhancement of the construct (e.g., + online D-RSS participation = increased engagement with online D-RSS).
We posit that, upon first engaging with social-online D-RSS, participation will engender a sense of shared experience and universality based on identification with other participants, and these other participants will instill hope that change is possible. Consistent with stress and coping theory, online D-RSS participation may enhance coping skills, through new information and vicarious learning, and enhance recovery self-efficacy, through access to 24/7 social support. Consistent with both social learning and social control theories, digital recovery supports may also offer opportunities to meet recovery-supportive individuals who could, over time, become go-to friends and mentors who reinforce prosocial behavior, promote strong social bonds, and help to provide monitoring and accountability. Finally, consistent with social learning theory, ongoing interactions with these recovery mentors and role models in online contexts may enhance individuals' positive SUD recovery expectancies.
We may expect individuals who are ambivalent about change, or who are committed to reducing rather than quitting substances, to benefit therapeutically given the cross-applicability of these hypothesized mechanisms to strategies that address both abstinence and harm reduction goals (e.g., coping with urges to drink or use other drugs). For those ambivalent about changing their substance use, D-RSS may enhance general strategies to cope with life demands and enhance psychological well-being. At the same time, exposure to a recovery social norm may help to shift attitudes in the direction of greater health behavior change. Also, social-online D-RSS may afford greater anonymity than possible with in-person services. This way, the potential for individuals with harm reduction goals to participate without identification, if they choose, may help to mitigate reasonable anxiety about seeking support from individuals whose goal is abstinence.
2.2. Potential drawbacks
Online and in-person services are not mutually exclusive. For example, among individuals who used online D-RSS in a nationally representative sample of US adults who resolved a substance use problem (Kelly et al., 2017), 48% also engaged with in-person recovery support services, 26% attended psychosocial treatment, and 27% were prescribed SUD medications, such as buprenorphine (Bergman et al., 2018). That said, to understand how individuals might fare if only participating in D-RSS, or how D-RSS participation might provide incremental benefit as an adjunct to in-person services, a discussion of its potential drawbacks provides important context. These drawbacks include missing out on in-person activities and behaviors, obstacles to social and emotional connection in digital spaces, and issues with the technology itself.
First, D-RSS may not facilitate active recovery involvement as well as in-person groups. This active involvement generally produces greater substance use benefits compared to attendance alone (Kelly et al., 2013; Montgomery et al., 1995; Weiss et al., 2005). For example, spending time with other recovering individuals (Kelly et al., 2013), obtaining a sponsor (Tonigan & Rice, 2010), and joining a home group (Zemore et al., 2013) may be more challenging in D-RSS relative to in-person MHOs. In addition, regular engagement with in-person services may improve outcomes, in part, through a desire to adhere to in-group norms of abstinence and/or health and well-being (Best et al., 2016). This accountability may not be present if participating in D-RSS. Finally, on average, more time in recovery, as well as participation in recovery support services, are each uniquely associated with greater comfort disclosing one's status as a person in recovery (Earnshaw et al., 2019). It is unclear whether this comfort, and any potential mental health benefits (i.e., decreased shame) might also increase over time in association with D-RSS participation. Of note, these missing elements could be especially problematic for those committed to SUD recovery, but early in the process. As such, it may ultimately prove helpful to contextualize the therapeutic benefits of D-RSS within a developmental recovery framework. For example, D-RSS may be more useful for individuals with previous service engagement and existing recovery support ties (e.g., individuals with a 12-step MHO home group). For those with less or no experience, however, active involvement may be more challenging without professional D-RSS facilitation via linkages and outreach. While we offer these possibilities for consideration, future research should examine the utility of a developmental recovery framework in the study of D-RSS.
Second, the benefit of recovery support service participation is explained to a large extent by peer-to-peer social connection (Kelly, 2017; Kelly et al., 2012; Kelly, Stout, et al., 2020). Whether and how digital platforms can engender this social connection are critical empirical questions. Professional telemedicine for individuals with psychiatric disorders may be instructive. A review of this literature (Simpson & Reid, 2014) suggests that the therapeutic alliance between therapist and patient is generally as good for telemedicine when compared to in-person therapy. Importantly, however, for group therapy, the group alliance may be lower when delivered via telemedicine relative to in person. This group format may better approximate social-online D-RSS, where individuals often interact with multiple peers at once, and manage competing cognitive and social demands. While the reasons for such a decrement in alliance for group telemedicine are unclear, communication science provides some clues. For example, digital spaces may not allow for the implicit perception of non-verbal cues that people use to guide their behavior and decision-making in social interaction (Argyle, 1971; Reinhard & Sporer, 2008). At the same time, the closeness and eye gaze of faces on a computer screen (i.e., increased immediacy) may enhance arousal and negative affect (Jarick & Bencic, 2019; Patterson, 1976). Taken together, individuals may need more cognitive and emotional resources in digital spaces to achieve the same level of social interaction that they would achieve with fewer resources in person, thereby decreasing connection, satisfaction, and ultimately engagement. If decreased social connection results in reduced social identification with other D-RSS participants, individuals may be less able to leverage vicarious learning (Bandura, 1971, Bandura, 2004), and forced to rely more on increased coping primarily through new information.
Third, the technology itself may introduce challenges. For example, there may be added privacy risks when participating in D-RSS. These risks include little control over who views another participant's screen. Online platforms themselves may also collect or share data from participants. In addition, D-RSS participation necessitates some level of comfort with technology, both for participants and any moderators or facilitators who may be well trained on the substantive issues at hand—those having to do with SUD recovery—but not as well trained on how to troubleshoot technological issues or navigate digital spaces. It is also crticial to mention that (Pew Research Center, 2019a) one in four US adults do not have household access to broadband internet, which is necessary to engage with some D-RSS. Consistent with other resource disparities among individuals living in the US, Black and Latino individuals, and those in lower socioeconomic strata, are disproporationately represented among those lacking household broadband internet access and, perahps in parallel, access to D-RSS as well.
3. Proposed typology to describe and classify social-online D-RSS
There is an array of free, social-online D-RSS, which constitute only one type of D-RSS (see Ashford et al., 2019 for an in-depth narrative review of all D-RSS). We propose the following typology to help describe and classify these different services, which, in turn, may help to enhance communication and aid referral. Each social-online D-RSS is available on different online platforms, enabled through different points of access, and under the auspices of different types of organizations (Table 1 ).
Table 1.
Proposed typology to describe and classify social-online D-RSS.
| a) Type of service | The recovery support service or activity with which someone engages (e.g., online recovery support meeting). Can be synchronous – real-time interaction – or asynchronous – interaction without time constraints |
| b) Type of platform | How the recovery support service is delivered (e.g., remote video conferencing, discussion boards, recovery-specific social network sites, etc.) |
| c) Points of access | Communication technology through which individuals access the online D-RSS platform (e.g., website, smartphone application, telephone, etc.) |
| d) Organization/individuals responsible | Organization and/or individuals that developed, maintains, monitors, and oversees the D-RSS (e.g., mutual-help organization, private company, peer volunteer monitors, etc.) |
Note: D-RSS = digital recovery support service.
3.1. Services
D-RSS may be synchronous, occurring in real-time; or asynchronous, where interactions occur over time. Common examples of social-online D-RSS include online video recovery support meetings. These online analogs of in-person MHO meetings often often include more well-known AA/NA and SMART Recovery formats. They also include All Recovery meetings, which are popular in recovery community centers and educational recovery settings, and cater to individuals who might be engaging one or more of a variety of recovery pathways (e.g., 12-step, secular, medication-assisted, etc.). Importantly, individuals need not disclose their identities to participate in online video recovery support meetings as they may observe without a webcam or having toggled off their webcam. Other service examples include recovery-focused discussion boards, where individuals can post or comment within topic threads. Discussion boards may have a naturally occurring community ethos and include policies and standards for participation. In chat groups, individuals engage in text-based conversation in real time. Individuals may also participate in social network activities focused on SUD recovery, where they are posting news stories, original text, and image-based content such as pictures, GIFs, and “memes”, consuming and reacting to (e.g., “liking”) these posts, and socializing with other participants using these posts as a backdrop. D-RSS may be framed within different goals, including, for example, psychoeducation versus social support, or a combination of the two.
3.2. Platforms
Individuals may access these services on several types of platforms. The platforms rely on different combinations of communication technologies, including text, audio, and video. Individuals may or, in some cases, must use specific commmunication technologies to engage with the D-RSS and, when relevant, interact with other members. Common examples include remote conferencing services (e.g., “Zoom”), which are very popular platforms for hosting online video recovery support meetings typically accessible by anyone with the relevant meeting room web address. These D-RSS may also be accessed through online community spaces affiliated with an MHO, including 12-step MHOs such AA and secular MHOs such as SMART Recovery. Services may also be delivered through social network sites, popular online communities where individuals create a profile, interact with streams of user-generated or shared content, and navigate the connections between and among other users (Ellison & boyd, 2013). These could be general-interest social network sites such as Facebook and Reddit, for example, or recovery-specific, which function like general-interest sites but cater to individuals in, seeking, or who want to learn more about SUD recovery. They often contain several different types of recovery-related resources, including, but not limited to, online video recovery support meetings, discussion boards and chat groups, and general social network activities, in addition to nonsocial resources such as locators for in-person meetings.
3.3. Points of access
Individuals can access these platforms, in turn, through one or more digital communication tools. Common points of access include websites and smartphone or computer applications. As mentioned above, while the “digital divide” is narrowing, those in lower socioeconomic strata, as well as Black and Latino individuals, are less likely than those in higher strata and White individuals, respectively, to have household broadband internet access (Pew Research Center, 2019a). Thus, the telephone remains an important point of access for many—some online recovery support meetings can also be accessed via telephone—and research has shown it to be a critical SUD continuing care point of access (McKay, 2009).
3.4. Organizations responsible for development, delivery, and oversight
Some services are entirely participant-led and monitored, often with volunteer monitors. In most cases, organizations are commonly responsible for social-online D-RSS, including MHOs, recovery community organizations (White et al., 2012)—nonprofit community-based groups that promote recovery-supportive advocacy, events, and policies, and may offer services within recovery community centers—and industry or private companies. Included in this element of the typology is the culture of the organization, such that some platforms may be better than others at engaging individuals who are accessing the D-RSS for the first time.
4. Theorized therapeutic benefits and proposed typology in action with an example: Intherooms.com
Intherooms.com is a free, recovery-specific social network site with more than 450,000 registered users, and 30,000 monthly visitors. It functions like other social network sites, such as Facebook or Instagram, but caters to individuals in, seeking, or who want to learn more about SUD recovery (Bergman et al., 2017). In addition to standard social network site offerings, including the opportunity to establish a network of “friends”, post or engage with newsfeed content (e.g., likes, comments, etc.), and discussion boards, Intherooms.com also offers live, online recovery support meetings, an archive of 12-step MHO recordings of individuals sharing their recovery stories (i.e., “speaker tapes”), and a database to find in-person meetings. We review what is known empirically about Intherooms.com participation here (Section 5), though we use the site to describe theorized benefits with an illustrated example and to demonstrate classification within the proposed typology (Table 1).
Initial exposure to Intherooms.com offers opportunities via social network site activities, discussion boards, and live online video meetings to interact with individuals in SUD recovery—both with individuals early in their SUD recovery process and those with more recovery experience. If a new user is in early recovery (or not in recovery at all), they might identify with shared experiences in other members, and feel a greater sense of hope that recovery-related change is also possible for them. Theory (Yalom & Leszcz, 2005) suggests this process of initial engagement will result in greater Intherooms.com participation—more time spent on the site, interactions with other users, and more activities in which they engage. More active involvement might, in turn, mobilize mechanisms of behavior change known to be activated by in-person recovery support services like 12-step MHOs (Kelly et al., 2012). For example, ongoing support from individuals with more recovery experience may increase an individual's sense that recovery efforts will yield real-life benefits (positive recovery expectancies). Also, the 24/7 access to recovery-supportive individuals and resources—not only through live online meetings but also by reading and learning from discussion boards—can provide opportunities for recovery coping and, in turn, enhanced confidence to handle challenging situations (e.g., recovery self-efficacy). Finally, as with 12-step MHOs, Intherooms.com offers a network of individuals in recovery with whom participants can form new social ties or transform latent ties into manifest ties (Steinfield et al., 2008). Taken together, these opportunities for recovery-supportive change could provide the foundation to reduce or quit substance use, and potentially enhance well-being more generally.
Applying the typology that we proposed to describe and classify social-online D-RSS, Intherooms.com is a recovery-specific social network site; a platform offering several services, some synchronous and some asynchronous, including social network site activities, discussion boards, and live online video meetings. Its points of access include both website and smartphone application. A for-profit company is responsible for development, delivery, and oversight. While the company running Intherooms.com earns money primarily through advertising from treatment and recovery support services, which enables individuals to use the site for free, the company does not use individuals' data to personalize the advertising, as is the case for ubiquitous general-interest sites such as Facebook.
5. What is known empirically about social-online D-RSS
5.1. Online video recovery support meetings
In the National Recovery Study, a representative sample of U.S. adults who resolved a substance use problem, 4.1%, or 900,000 individuals, reported lifetime participation in one or more online recovery support meetings (Bergman et al., 2018). In a randomized controlled trial testing SMART Recovery meeting attendance against a web-based cognitive behavioral intervention, Hester and colleagues (Campbell et al., 2016; Hester et al., 2013) found that among the entire sample, online SMART meeting attendance was related to improved percent days abstinent from baseline to 3-month follow-up. Online SMART attendance, however, was unrelated to changes in other drinking outcomes during this time, and unrelated to changes in drinking outcomes between 3-month and 6-month follow-ups. There are no studies to date that specifically examine participation in, or effectiveness of, online 12-step MHO meeting attendance.
5.2. Discussion boards and chat groups
Reddit-based discussion boards, some of which host many thousands of Redditors, are among the best studied social-online D-RSS (D'Agostino et al., 2017; Sowles et al., 2017; Wombacher et al., 2019). Two studies, one examining an opioid recovery group and one a cannabis recovery group, showed group comments on the 100 “hottest” posts, determined by a Reddit algorithm, typically mapped onto Yalom's (Yalom & Leszcz, 2005) curative group therapy factors (D'Agostino et al., 2017) or comprised generally helpful advice such as lifestyle changes and cognitive reframing (Sowles et al., 2017). The authors determined that only very few comments were potentially harmful (D'Agostino et al., 2017; Sowles et al., 2017). In addition to these recovery-focused discussion boards, those catering to discussions broadly about substance use facilitate support primarily related to harm reduction (e.g., advice on dosages and safety), and to a lesser extent general emotional/social support as well (Wombacher et al., 2019).
“SHE RECOVERS” is a hybrid online/in-person recovery organization for women in, or seeking, recovery from any number of behavioral health difficulties including but not limited to SUD (Curtis et al., 2019). In a survey of SHE RECOVERS participants (N = 729), individuals had 6 years in recovery, on average, and 85% identified as being in recovery from SUD (majority were alcohol primary) and 55% from a behavioral health disorder (majority were depression or anxiety primary). Eight in 10 participants said that they either had connected, or would like to connect, with another SHE RECOVERS member outside of services or events, and all members had made at least one digital friendship. These data suggest this gender-specific recovery community may help to mobilize social network changes.
Studies have leveraged recovery-focused discussion boards to elucidate recovery processes (Bliuc et al., 2019) and to pre-emptively identify signs of recurrence of substance use using natural language processing and machine learning (Kornfield, Sarma, et al., 2018; Kornfield, Toma, et al., 2018). These critical and innovative areas of ongoing investigation are outside the scope of this review, however.
5.3. Recovery-specific social network sites
Studies of free, recovery-specific social network sites have focused on the most active users within Intherooms.com, available via website and smartphone application, and Sober Grid, available via smartphone application only (Ashford et al., 2020; Bergman et al., 2017). Individuals who participate on these sites may have substance use and psychiatric disorder histories, with the majority having attended formal treatment as well as MHOs such as AA. Also, duration of recovery and degree of community engagement may be site dependent. For example, the average Sober Grid participant had less than 1 year of continuous abstinence and logged on for 12.5 sessions (Ashford et al., 2020), whereas the average Intherooms.com participant had 7 years of continuous abstinence and logged on several times per week for 30 min per session, on average (Bergman et al., 2017). Intherooms.com data, however, were based on participant report, while Sober Grid data were based on objectively derived site analytics. Intherooms.com participants generally found their participation helped to increase recovery motivation and self-efficacy, irrespective of whether they were in recovery for less than 1 year (or not in recovery) versus 1 or more years. Interestingly, older Sober Grid participants demonstrated greater site engagement (e.g., posts, comments, and likes) and the self-selected group of Intherooms.com survey participants was 51 years old on average. Thus, while younger individuals in the general population are disproportionately represented on social network sites (Pew Research Center, 2019b), older individuals, who tend to have longer recovery durations, may be more engaged on recovery-specific sites.
Recovery-specific sites that operate on monthly fee-for-use models are outside the scope of this review. Though given the paucity of data on benefits of recovery-specific social network site participation, it is worth mentioning that longitudinal research has shown that greater engagement on Daybreak (formerly Hello Sunday Morning), including more posts and comments, is associated with better drinking outcomes over time (Kirkman et al., 2018; Tait et al., 2019).
6. Recommendations on whether and how to engage individuals with free, social-online D-RSS
Studies that examine in-person recovery support services, such as AA and other MHOs, combined with theory about how social-online D-RSS might confer benefit, suggest that these digital supports may engage individuals with SUD and mobilize salutary change in ways similar to AA (Kelly, 2017; Kelly et al., 2009; Moos, 2008). As such, these free, online recovery supports may provide key scaffolding to individuals with current and remitted SUD while adhering to COVID-19 social distancing recommendations. The potential drawbacks of D-RSS notwithstanding, studies that do examine social-online D-RSS suggest participants perceive benefit and existing services may help to facilitate social support. Thus, given that the COVID-19 pandemic will disrupt the lives of many individuals with SUD, these free digital resources may enable individuals to maintain physical distance while also engaging with ongoing recovery-related social support and connection. The expected therapeutic benefits and emerging data on social-online D-RSS, taken together, particularly during a public health crisis, suggest providers, mentors, and other community leaders may wish to refer individuals to social-online D-RSS. Such referrals, however, should also include a discussion of the potential drawbacks of digital versus in-person recovery support services and risks of participating on digital platforms.
Several organizations have compiled lists of free, social-online D-RSS with relevant links to access the services in question. These organizations include, but are not limited to, the Grayken Center for Addiction at the Boston Medical Center (https://www.bmc.org/addiction/covid-19-recovery-resources), the American Society of Addiction Medicine (https://www.asam.org/Quality-Science/covid-19-coronavirus/support-group), the National Institute on Drug Abuse (https://www.drugabuse.gov/related-topics/covid-19-resources), Google's Recover Together (https://recovertogether.withgoogle.com/), and our group at the Recovery Research Institute (https://www.recoveryanswers.org/media/digital-recovery-support-online-and-mobile-resources/).
The COVID-19 pandemic highlights barriers to SUD treatment and recovery support service access that predate and are likely to persist well beyond the COVID-19 epoch. Research on whether and how D-RSS may help to address these barriers is ongoing. In the absence of best practice guidlines for social-online D-RSS, we recommend that providers, policy-makers, and other community leaders familiarize themselves with potential benefits and drawbacks of participation, use a typology to describe and classify services, integrate current empirical knowledge, and rely on trusted sources when referring individuals to these free, digital recovery supports.
Funding/support
Dr. Bergman is supported by an early career development award from the NIH (National Institute on Alcohol Abuse and Alcoholism [NIAAA]; K23AA025707) and Dr. Kelly is supported by a midcareer investigator award from the NIH (NIAAA; K24AA022136).
Declaration of competing interest
Dr. Bergman is a member of the board of directors for Unity Recovery, a nonprofit recovery community organization that partners with other recovery community organizations and the technology startup company WEConnect to offer free, online recovery support meetings and other digital recovery support services. Dr. Bergman receives no compensation from, nor has any financial stake in, Unity Recovery or any of its partners.
References
- Argyle M. In: Non-verbal communication. Hinde R., editor. Cambridge University Press; Cambridge, UK: 1971. Non-verbal communication in human social interaction. [Google Scholar]
- Ashford R.D., Bergman B.G., Kelly J.F., Curtis B. Systematic review: Digital recovery support services used to support substance use disorder recovery. Human Behavior and Emerging Technologies. 2019 doi: 10.1002/hbe2.148. [DOI] [Google Scholar]
- Ashford R.D., Giorgi S., Mann B., Pesce C., Sherritt L., Ungar L., Curtis B. Digital recovery networks: Characterizing user participation, engagement, and outcomes of a novel recovery social network smartphone application. Journal of Substance Abuse Treatment. 2020;109:50–55. doi: 10.1016/j.jsat.2019.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bandura A. In: The nature of reinforcement. Glaser R., editor. Academic Press; New York: 1971. Vicarious and self-reinforcement processes; pp. 228–278. [Google Scholar]
- Bandura A. Health promotion by social cognitive means. Health Education & Behavior. 2004;31(2):143–164. doi: 10.1177/1090198104263660. [DOI] [PubMed] [Google Scholar]
- Bergman B.G., Claire Greene M., Hoeppner B.B., Kelly J.F. Expanding the reach of alcohol and other drug services: Prevalence and correlates of US adult engagement with online technology to address substance problems. Addictive Behaviors. 2018;87:74–81. doi: 10.1016/j.addbeh.2018.06.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bergman B.G., Kelly N.W., Hoeppner B.B., Vilsaint C.L., Kelly J.F. Digital recovery management: Characterizing recovery-specific social network site participation and perceived benefit. Psychology of Addictive Behaviors. 2017;31(4):506–512. doi: 10.1037/adb0000255. [DOI] [PubMed] [Google Scholar]
- Best D., Beckwith M., Haslam C., Haslem S.A., Jetten J., Mawson E., Lubman D.I. Overcoming alcohol and other drug addiction as a process of social identity transition: The social identity model of recovery (SIMOR) Addiction Research & Theory. 2016;24(2):111–123. doi: 10.3109/16066359.2015.1075980. [DOI] [Google Scholar]
- Bliuc A.-M., Doan T.-N., Best D. Sober social networks: The role of online support groups in recovery from alcohol addiction. Journal of Community & Applied Social Psychology. 2019;29(2):121–132. doi: 10.1002/casp.2388. [DOI] [Google Scholar]
- Campbell W., Hester R.K., Lenberg K.L., Delaney H.D. Overcoming Addictions, a web-based application, and SMART Recovery, an online and in-person mutual help group for problem drinkers, part 2: Six-month outcomes of a randomized controlled trial and qualitative feedback from participants. Journal of Medical Internet Research. 2016;18(10) doi: 10.2196/jmir.5508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (CDC) Implementation of mitigation strategies for communities with local COVID-19 transmission. 2020. https://www.cdc.gov/coronavirus/2019-ncov/downloads/community-mitigation-strategy.pdf Retrieved from.
- Crits-Christoph P., Siqueland L., Blaine J., Frank A., Luborsky L., Onken L.S.…Beck A.T. Psychosocial treatments for cocaine dependence: National Institute on Drug Abuse Collaborative Cocaine Treatment Study. Archives of General Psychiatry. 1999;56(6):493–502. doi: 10.1001/archpsyc.56.6.493. [DOI] [PubMed] [Google Scholar]
- Curtis B., Bergman B., Brown A., McDaniel J., Harper K., Eisenhart E.…Ashford R. Characterizing participation and perceived engagement benefits in an integrated digital behavioral health recovery community for women: A cross-sectional survey. JMIR Mental Health. 2019;6(8) doi: 10.2196/13352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- D’Agostino A.R., Optican A.R., Sowles S.J., Krauss M.J., Escobar Lee K., Cavazos-Rehg P.A. Social networking online to recover from opioid use disorder: A study of community interactions. Drug and Alcohol Dependence. 2017;181:5–10. doi: 10.1016/j.drugalcdep.2017.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Earnshaw V.A., Bergman B.G., Kelly J.F. Whether, when, and to whom? An investigation of comfort with disclosing alcohol and other drug histories in a nationally representative sample of recovering persons. Journal of Substance Abuse Treatment. 2019;101:29–37. doi: 10.1016/j.jsat.2019.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ellison N.B., boyd d. In: The Oxford handbook of internet studies. Dutton W.H., editor. Oxford University Press; Oxford: 2013. Sociality through social network sites; pp. 151–172. [Google Scholar]
- Grant B.F., Goldstein R.B., Saha T.D., Chou S.P., Jung J., Zhang H.…Hasin D.S. Epidemiology of DSM-5 alcohol use disorder: Results from the National Epidemiologic Survey on Alcohol and Related Conditions III. JAMA Psychiatry. 2015 doi: 10.1001/jamapsychiatry.2015.0584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant B.F., Saha T.D., Ruan W.J., Goldstein R.B., Chou S.P., Jung J.…Hasin D.S. Epidemiology of DSM-5 drug use disorder: Results from the National Epidemiologic Survey on Alcohol and Related Conditions-III. JAMA Psychiatry. 2016;73(1):39–47. doi: 10.1001/jamapsychiatry.2015.2132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hester R.K., Lenberg K.L., Campbell W., Delaney H.D. Overcoming Addictions, a web-based application, and SMART Recovery, an online and in-person mutual help group for problem drinkers, part 1: Three-month outcomes of a randomized controlled trial. Journal of Medical Internet Research. 2013;15(7) doi: 10.2196/jmir.2565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jarick M., Bencic R. Eye contact is a two-way street: Arousal is elicited by the sending and receiving of eye gaze information. Frontiers in Psychology. 2019;10:1–14. doi: 10.3389/fpsyg.2019.01262. 1262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly J.F. Is alcoholics anonymous religious, spiritual, neither? Findings from 25 years of mechanisms of behavior change research. Addiction. 2017 doi: 10.1111/add.13590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly J.F., Bergman B.G., Hoeppner B.B., Vilsaint C.L., White W.L. Prevalence and pathways of recovery from drug and alcohol problems in the United States population: Implications for practice, research, and policy. Drug and Alcohol Dependence. 2017;181(Supplement C):162–169. doi: 10.1016/j.drugalcdep.2017.09.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly J.F., Fallah-Sohy N., Vilsaint C., Hoffman L.A., Jason L.A., Stout R.L.…Hoeppner B.B. New kid on the block: An investigation of the physical, operational, personnel, and service characteristics of recovery community centers in the United States. Journal of Substance Abuse Treatment. 2020;111:1–10. doi: 10.1016/j.jsat.2019.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly J.F., Hoeppner B., Stout R.L., Pagano M. Determining the relative importance of the mechanisms of behavior change within alcoholics anonymous: A multiple mediator analysis. Addiction. 2012;107(2):289–299. doi: 10.1111/j.1360-0443.2011.03593.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly J.F., Humphreys K., Ferri M. Alcoholics anonymous and other 12-step programs for alcohol use disorder. Cochrane Database of Systematic Reviews. 2020;3 doi: 10.1002/14651858.CD012880.pub. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly J.F., Magill M., Stout R.L. How do people recover from alcohol dependence? A systematic review of the research on mechanisms of behavior change in alcoholics anonymous. Addiction Research & Theory. 2009;17(3):236–259. doi: 10.1080/16066350902770458. [DOI] [Google Scholar]
- Kelly J.F., Stout R.L., Jason L.A., Fallah-Sohy N., Hoffman L.A., Hoeppner B.B. One-stop shopping for recovery: An investigation of participant characteristics and benefits derived from U.S. recovery community centers. Alcoholism: Clinical and Experimental Research. 2020;44(3):711–721. doi: 10.1111/acer.14281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly J.F., Stout R.L., Slaymaker V. Emerging adults’ treatment outcomes in relation to 12-step mutual-help attendance and involvement. Drug and Alcohol Dependence. 2013;129(1–2):151–157. doi: 10.1016/j.drugalcdep.2012.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirkman L.J.J., Leo B., Moore C.J. Alcohol consumption reduction among a web-based supportive community using the hello Sunday morning blog platform: Observational study. Journal of Medical Internet Research. 2018;20(5) doi: 10.2196/jmir.9605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kornfield R., Sarma K.P., Shah V.D., McTavish F., Landucci G., Pe-Romashko K., Gustafson H.D. Detecting recovery problems just in time: Application of automated linguistic analysis and supervised machine learning to an online substance abuse forum. Journal of Medical Internet Research. 2018;20(6) doi: 10.2196/10136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kornfield R., Toma C.L., Shah D.V., Moon T.J., Gustafson D.H. What do you say before you relapse? How language use in a peer-to-peer online discussion forum predicts risky drinking among those in recovery. Health Communication. 2018;33(9):1184–1193. doi: 10.1080/10410236.2017.1350906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Labbe A.K., Slaymaker V., Kelly J.F. Toward enhancing 12-step facilitation among young people: A systematic qualitative investigation of young adults’ 12-step experiences. Substance Abuse. 2014;35(4):399–407. doi: 10.1080/08897077.2014.950001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laudet A., Harris K., Kimball T., Winters K.C., Moberg D.P. Collegiate recovery communities programs: What do we know and what do we need to know? Journal of Social Work Practice in the Addictions. 2014;14(1):84–100. doi: 10.1080/1533256x.2014.872015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laudet A.B., Cleland C.M., Magura S., Vogel H.S., Knight E.L. Social support mediates the effects of dual-focus mutual aid groups on abstinence from substance use. American Journal of Community Psychology. 2004;34(3–4):175–185. doi: 10.1007/s10464-004-7413-5. http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=15663205 Retrieved from. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laudet A.B., Harris K., Kimball T., Winters K.C., Moberg D.P. Characteristics of students participating in collegiate recovery programs: A national survey. Journal of Substance Abuse Treatment. 2015;51:38–46. doi: 10.1016/j.jsat.2014.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marlatt G.A. Taxonomy of high-risk situations for alcohol relapse: Evolution and development of a cognitive-behavioral model. Addiction. 1996;91:S37–S49. http://ezp-prod1.hul.harvard.edu/login?url=http://search.ebscohost.com/login.aspx?direct=true&db=aph&AN=9702072771&site=ehost-live&scope=site Retrieved from. [PubMed] [Google Scholar]
- McKay J.R. Continuing care research: What we’ve learned and where we’re going. Journal of Substance Abuse Treatment. 2009;36(2):131–145. doi: 10.1016/j.jsat.2008.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Montgomery H.A., Miller W.R., Tonigan J.S. Does alcoholics anonymous involvement predict treatment outcome. Journal of Substance Abuse Treatment. 1995;12(4):241–246. doi: 10.1016/0740-5472(95)00018-z. [DOI] [PubMed] [Google Scholar]
- Moos R.H. Active ingredients of substance use-focused self-help groups. Addiction. 2008;103:387–396. doi: 10.1111/j.1360-0443.2007.02111.x. [DOI] [PubMed] [Google Scholar]
- Patterson M.L. An arousal model of interpersonal intimacy. Psychological Review. 1976;83(3):235–245. doi: 10.1037/0033-295X.83.3.235. [DOI] [Google Scholar]
- Pew Research Center . 2019. Internet/broadband fact sheet.http://www.pewinternet.org/fact-sheet/internet-broadband/ Retrieved from. [Google Scholar]
- Pew Research Center Social media fact sheet. 2019. http://www.pewinternet.org/fact-sheet/social-media/ Retrieved from.
- Ramo D.E., Brown S.A. Classes of substance abuse relapse situations: A comparison of adolescents and adults. Psychology of Addictive Behaviors: Journal of the Society of Psychologists in Addictive Behaviors. 2008;22(3):372–379. doi: 10.1037/0893-164X.22.3.372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rawson R.A., Marinelli-Casey P., Anglin M.D., Dickow A., Frazier Y., Gallagher C.…Methamphetamine Treatment Project Corporate, A A multi-site comparison of psychosocial approaches for the treatment of methamphetamine dependence. Addiction. 2004;99(6):708–717. doi: 10.1111/j.1360-0443.2004.00707.x. [DOI] [PubMed] [Google Scholar]
- Reinhard M.-A., Sporer S.L. Verbal and nonverbal behaviour as a basis for credibility attribution: The impact of task involvement and cognitive capacity. Journal of Experimental Social Psychology. 2008;44(3):477–488. doi: 10.1016/j.jesp.2007.07.012. [DOI] [Google Scholar]
- Simpson S., Reid C. Therapeutic alliance in videoconferencing psychotherapy: A review. Australian Journal of Rural Health. 2014;22:280–299. doi: 10.1111/ajr.12149. [DOI] [PubMed] [Google Scholar]
- Sowles S.J., Krauss M.J., Gebremedhn L., Cavazos-Rehg P.A. “I feel like I’ve hit the bottom and have no idea what to do”: Supportive social networking on Reddit for individuals with a desire to quit cannabis use. Substance Abuse. 2017;38(4):477–482. doi: 10.1080/08897077.2017.1354956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steinfield C., Ellison N.B., Lampe C. Social capital, self-esteem, and use of online social network sites: A longitudinal analysis. Journal of Applied Developmental Psychology. 2008;29:434–445. doi: 10.1016/j.appdev.2008.07.002. [DOI] [Google Scholar]
- Tait R.J., Paz Castro R., Kirkman J.J.L., Moore J.C., Schaub M.P. A digital intervention addressing alcohol use problems (the “daybreak” program): Quasi-experimental randomized controlled trial. Journal of Medical Internet Research. 2019;21(9) doi: 10.2196/14967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tonigan J.S., Rice S.L. Is it beneficial to have an alcoholics anonymous sponsor? Psychology of Addictive Behaviors. 2010;24(3):397–403. doi: 10.1037/a0019013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss R.D., Griffin M.L., Gallop R.J., Najavits L.M., Frank A., Crits-Christoph P.…Luborsky L. The effect of 12-step self-help group attendance and participation on drug use outcomes among cocaine-dependent patients. Drug and Alcohol Dependence. 2005;77:177–184. doi: 10.1016/j.drugalcdep.2004.08.012. [DOI] [PubMed] [Google Scholar]
- Weiss R.D., Griffin M.L., Marcovitz D.E., Hilton B.T., Fitzmaurice G.M., McHugh R.K., Carroll K.M. Correlates of opioid abstinence in a 42-month posttreatment naturalistic follow-up study of prescription opioid dependence. Journal of Clinical Psychiatry. 2019;80(2) doi: 10.4088/JCP.18m12292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- White W.L., Kelly J.F., Roth J.D. New addiction-recovery support institutions: Mobilizing support beyond professional addiction treatment and recovery mutual aid. Journal of Groups in Addiction & Recovery. 2012;7(2–4):297–317. [Google Scholar]
- Wombacher K., Sheff S.E., Itrich N. Social support for active substance users: A content analysis of r/drugs. Health Communication. 2019:1–10. doi: 10.1080/10410236.2019.1587691. [DOI] [PubMed] [Google Scholar]
- Yalom I.D., Leszcz M. 5th ed. Basic Books; New York, NY US: 2005. The theory and practice of group psychotherapy. [Google Scholar]
- Zemore S.E., Lui C., Mericle A., Hemberg J., Kaskutas L.A. A longitudinal study of the comparative efficacy of Women for Sobriety, LifeRing, SMART Recovery, and 12-step groups for those with AUD. Journal of Substance Abuse Treatment. 2018;88:18–26. doi: 10.1016/j.jsat.2018.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zemore S.E., Subbaraman M., Tonigan J.S. Involvement in 12-step activities and treatment outcomes. Substance Abuse. 2013;34(1):60–69. doi: 10.1080/08897077.2012.691452. [DOI] [PMC free article] [PubMed] [Google Scholar]