Abstract
Background
Several studies have identified fatigue as one of the major symptoms experienced during and after cancer treatment. However, there are limited options to manage cancer related fatigue (CRF) with pharmacological interventions. Several acupuncture studies suggested that acupuncture has a positive impact on CRF. This review aims to assess the evidence of acupuncture for the treatment of CRF.
Method
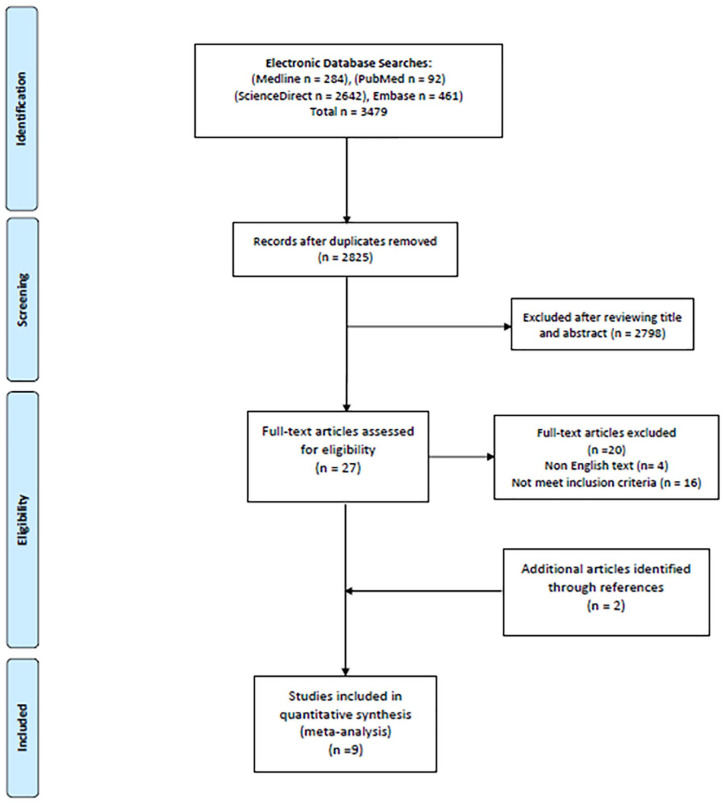
Electronic database searches were conducted on 4 English databases (Medline, PubMed, Embase, and ScienceDirect). Search keywords were; “acupuncture” and “cancer,” or “cancer related fatigue.” Studies published as full text randomized controlled trials (RCTs) in English were included. Estimates of change in fatigue cores were pooled using a random effects meta-analysis where randomized comparisons were available for true acupuncture versus sham acupuncture and true acupuncture versus usual care. The quality of original papers were assessed using the Cochrane Collaboration’s tool for assessing risk of bias (ROB).
Results
Nine RCTs were selected for review with a total of 809 participants and a range of 13 to 302 participants within the studies. Six RCTs reported significant improvement of CRF for the acupuncture intervention compared to the control groups. Pooled estimates suggest Brief Fatigue Inventory scores are 0.93 points lower 95% CI (−1.65, −0.20) in true acupuncture versus sham acupuncture and 2.12 points lower 95% C (−3.21, −1.04) in true acupuncture versus usual care. Six studies had low risk of bias (ROB) and 3 studies had a moderate ROB predominantly in blinding of participants, blinding of assessors and incomplete data outcomes. Among the 9 RCTs, 2 studies have reported the occurrence of minor adverse effects (spot bleeding and bruising) related to acupuncture treatment. No serious adverse reactions related to acupuncture were reported.
Conclusion
The current literature review suggests that acupuncture has therapeutic potential in management of CRF for cancer survivors. Promotion of acupuncture in cancer care to manage CRF may improve the quality of life of cancer survivors.
Keywords: acupuncture, cancer, fatigue, cancer related fatigue
Introduction
Cancer-related Fatigue (CRF) is one of the most prevalent symptoms of cancer. It has been reported that up to 40% of individuals with cancer experience CRF at diagnosis, as do 90% of those treated with radiation and 80% of those who undergo chemotherapy.1 Unlike normal fatigue, CRF is disproportionate to exertion level and is not relieved by rest or sleep.2 The National Comprehensive Cancer Network (NCCN) defined CRF as “distressing, persistent or cognitive tiredness or exhaustion related to cancer or cancer treatment that is not proportional to activity, interferes with usual functioning, and is not relieved by rest.”3 CRF impacts on patients’ quality of life and functional status, thus affecting not only the individual but also the family.4,5 CRF is associated with various comorbidities such as pain, insomnia, dyspnea, loss of appetite, depression, and anxiety.1,6 CRF is also associated with shorter recurrence-free and overall survival in patients with cancer.7 Fatigue is a complex symptom that relates to multiple factors including physical, mental, and emotional aspects.8 Hence, there are limited treatment options to manage CRF with currently available pharmacological interventions although attempts have been made to manage CRF with psycho-stimulants, erythropoietin, and antidepressants.3,9,10
As a result, there has been an increase in interest in non-pharmacological approaches to managing CRF11 with exercise,12 education counselling or sleep therapy.13 Recently, there has been a growing body of evidence supporting complementary and alternative medicine (CAM) for CRF.10 Among the various CAM therapies, acupuncture has gained significant attention as a tool to manage CRF.14 A number of recent acupuncture studies suggest that it has the potential to benefit patients who suffer from CRF and improve their quality of life (QoL).15 Further, a recent network meta-analysis suggested that acupuncture ranked the best for the management of CRF among nonpharmacological interventions.16 This review is therefore conducted to assess the current evidence for acupuncture in the management of CRF.
Methods
The systematic review and meta-analysis was conducted following the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-analyses) 2018 guideline for systematic review and meta-analysis. Electronic database searches were conducted on 4 English databases (Medline, PubMed, Embase, and ScienceDirect) from inception through May 2019. Searches were performed using the following keywords; “acupuncture” and “cancer,” or “cancer related fatigue.” Eligibility criteria were; full text studies published in English, and RCTs with the primary outcome of CRF. Two reviewers (AJ and BO) screened the titles and abstracts and reviewed for eligibility after reading the full text. Additionally, further potential studies were searched for by screening references in the identified studies as well as relevant studies to the topic.
Data Analysis
Outcomes at the first post-treatment assessment were summarized and compared by treatment arms. Estimates of treatments effects on fatigue scores were extracted and compared for randomized arms (true acupuncture, sham, usual care). Random effects meta-analysis was used to compute pooled estimates allowing for variation. One study only reported the outcomes as change from baseline estimates but was included in the meta-analysis (it is still a reasonable estimate of the treatment effect, albeit with a lower variance). Two studies15,17 reported different fatigue outcomes (general fatigue, mental fatigue, physical fatigue) and these were pooled separately to evaluate consistency. The meta-analysis was performed using R version 3.5.3 statistical software and the “metafor” package (version 2.1).
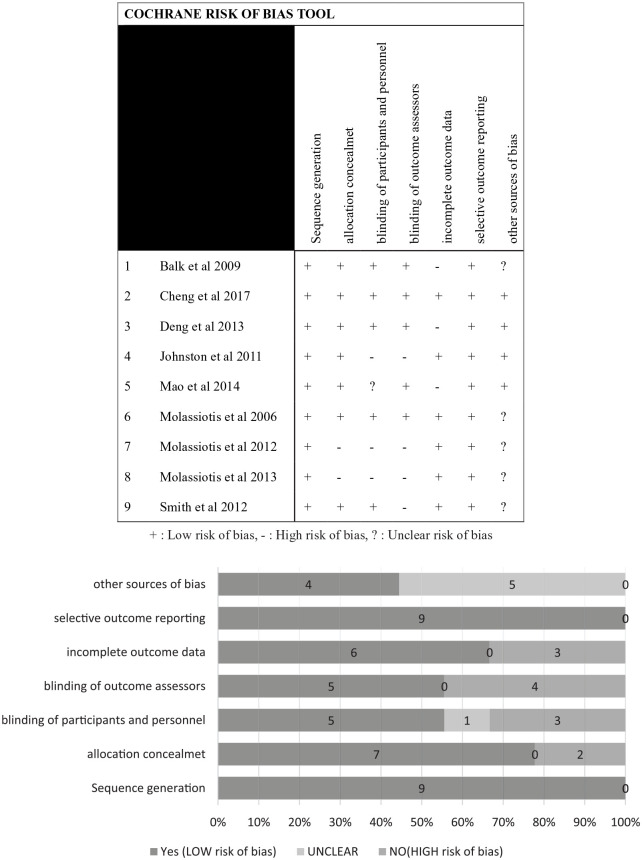
Quality Assessment of Original Papers
Risk of Bias (ROB) Assessment: To adequately assess ROB of the included RCTs in the review, 2 reviewers independently assessed the ROB using the Cochrane Collaboration’s tool for assessing ROB. The Cochrane Collaboration tool consists of 7 domains: “adequate sequence generation, allocation concealment, blinding of participants and personnel, blinding outcome assessment, incomplete outcome data, selective reporting and other ROB.”18 Any disagreement between the 2 reviewers was resolved via discussion.
Results
A total of 3479 studies were initially identified and screened in this literature search. After an in-depth evaluation of screening titles and abstracts, 27 articles remained to be further assessed for eligibility to be included in the study. Nine studies were included in the review (Figure 1).
Figure 1.
Flow chart.
Characteristics of Clinical Studies and Quality of Evidence
In the 9 RCTs, there were a total of 809 participants with a range of 13 to 302 participants within the studies, of which 421 were in the acupuncture (intervention) group and 271 in the control group (Table 1). Total dropouts were 145 in the studies. Studies were conducted with breast cancer patients (n = 6),15,17,19-22 non-small cell lung cancer (n = 1),23 and various types of malignancy (n = 2).6,24 Three studies15,17,20 reported stages I-III of cancer. Studies were conducted in USA (n = 4),19,20,22,24 UK (n = 3)6,15,17 and one each were from Australia21 and China.23 The earliest RCT was published in 2009.22 Five15,19,22-24 of the 9 studies had 2-arm trials and 4 studies6,17,20,21 had 3-arm trials. All 9 trials had acupuncture treatment as their intervention and 2 studies20,22 included electro stimulation to the needles. Four trials6,22-24 incorporated Sham/placebo needling as their main control and 5 studies15,17,19-21 used usual care as their control. Total acupuncture treatment sessions were 10 sessions (n = 2),17,20 9 sessions (n = 1),21 8 sessions (n = 2),19,23 6 sessions (n = 3),6,15,24 and 1 study22 was unable to determine the exact number of total sessions. Acupuncture intervention periods were 10 weeks (n = 1),17 8 weeks (n = 2),19,20 6 weeks (n = 3),15,21,24 4 weeks (n = 1),23 2 weeks (n = 1),6 and 2 to 4 weeks (n = 1).22 The number of treatments per week varied and included 3 treatments (n = 1),6 2 treatments (n = 1),23 and 1 treatment (n = 4),15,17,19,24 as well as mixed number of treatments per week (n = 3).20-22 Needle retention times were 45 minutes (n = 1),23 30 minutes (n = 3),19,20,22 and 20 minutes (n = 5).6,15,17,21,24 The primary outcome of CRF was measured with the Brief Fatigue Inventory (BFI) (n = 5),19-21,23,24 Multidimensional Fatigue Inventory (MFI) (n = 3),6,15,17 and Functional Assessment of Chronic Illness Therapy-Fatigue subscale (FACIT-F) (n = 1).22
Table 1.
Summary of Findings.
| Author | Study design | Population | Sample size | Intervention/control | Outcome measurement tools | Adverse effects | Results/conclusions |
|---|---|---|---|---|---|---|---|
| Cheng et al23
China |
RCT 2 arms |
Non-small cell lung cancer (NSCLC) | Total N = 28 TA: N = 14 SA: N = 14 |
Both groups received 8 × 45 min sessions for 4 weeks (2 per week) Acupuncture points (LI4, REN6, ST36, KI3, and SP6) Park sham needles used for placebo group |
BFI-C and FACT-LCS | Measured with the CTCAE version 3.0 - 1-2 grade pain 28.6% (n = 3) - 1-2 grade dizziness 14.3% (n = 2) - 1-2 grade bleeding 7.1% (n = 1) |
A significant reduction in the BFI-C score was observed at 2 weeks in the 14 participants who received active acupuncture compared with those receiving the placebo (P < .01). At week 6, symptoms further improved according to the BFI-C (P < .001) and the FACT-LCS (P = .002). Fatigue is a common symptom experienced by lung cancer patients. Acupuncture may be a safe and feasible optional method for adjunctive treatment in cancer palliative care. |
| Balk et al22
USA |
RCT 2 arms |
Women with localized cancer | Total N = 27 TA: N = 16 SA: N = 11 |
Both groups received 2 × 30 min treatment for 4-6 weeks Acupuncture points (SP6, LI4, REN6, SI3, and ST36) TA: electro-acupuncture on KI3 and ST36, heat lamp on REN 6) SA: Park sham needles (electro-acupuncture not turned on KI3 and ST36, heat lamp on low setting) |
Primary outcome: FACIT-F Secondary outcome: SF-36 and CRFDS |
No subjects reported adverse reaction | Both true and sham acupuncture groups had improved fatigue, fatigue distress, quality of life, and depression from baseline to 10 weeks, but the differences between the groups were not statistically significant. The true acupuncture group improved 5.50 (SE, ±1.48) points on the Functional Assessment of Chronic Illness Therapy-Fatigue Subscale (FACIT-F), whereas the sham acupuncture group improved by 3.73 (SE ±1.92) points. This study was underpowered to find a statistically significant difference. To demonstrate a statistically significant improvement between true and sham acupuncture would require 75 subjects per group in a future study |
| Deng et al24
USA |
RCT 2 arms |
Diagnosed with a malignancy | Total N = 97 TA: N = 47 SA: N = 50 |
Both groups received 1 × 20 min treatment for 6 weeks Acupuncture points (REN6, REN4, KI3, ST36, SP6, LI11, HT6, auricular point: anti-depression) SA: Streitberger placebo needle |
Primary outcome: BFI, HADS, FACT-G | Measured with the CTCAE version 3.0; bronchospasm (1), low blood counts (1), renal failure (2), secondary malignancy (1), nausea (1), vomiting (2), small bowel obstruction (1), dyspnea (1), and back pain (1). | BFI scores fell by about one point between baseline and follow-up in both groups with no statistically significant difference between groups. HADS and FACT-G scores also improved in both groups, but there was no significant difference between groups. True acupuncture as provided in this study did not reduce post-chemotherapy chronic fatigue more than did sham acupuncture. The study is limited by the number of patients lost to follow-up. We also cannot exclude the possibility that a more intensive treatment regimen may be more effective. |
| Johnston et al19
USA |
RCT 2 arms |
Finished primary treatment for BCa | Total N = 13 TA: N = 5 UC: N = 7 |
Both groups received 30 min education for 4 weeks for UC Intervention group received 1 × 30 min treatment for 8 weeks Acupuncture points (LI4, SP6, ST36, KI3) other points were used according to patients signs and symptoms |
Primary outcome: BFI Secondary outcome: FACT-COG |
With a standardized checklist to assess for adverse events after each treatment, including bruising at needling site, panic, severe disorientation, fainting, infection, or puncture of an internal organ. | Compared to usual care control, the intervention was associated with a 2.38-point decline in fatigue as measured by the BFI (90% Confidence Interval from 0.586 to 5.014; P < .10). Patient education integrated with acupuncture had a very promising effect that warrants conducting a larger RCT to confirm findings. An effective recruitment strategy will be essential for the successful execution of a larger-scale trial. |
| Mao et al20
USA |
RCT 3 arm |
Women with a history of early stage of cancer (stages I-III) | Total N = 67 TA: N = 22 SA: N = 22 WL: N = 23 |
Interventions twice weekly for 2 weeks, then weekly for 6 more weeks, for a total of 10 treatments over 8 weeks. TA: Electro acupuncture (EA) SA: Streitberger placebo needle |
Primary outcome: BPI and BFI Secondary outcome: PSQI, HADS |
Not reported | Compared with the WL condition, EA produced significant improvements in fatigue (P = .0095), anxiety (P = .044), and depression (P = .015) and a nonsignificant improvement in sleep disturbance (P = .058) during the 12-week intervention and follow-up period. In contrast, SA did not produce significant reductions in fatigue or anxiety symptoms but did produce a significant improvement in depression compared with the WL condition (P = .0088). Compared with usual care, EA produced significant improvements in fatigue, anxiety, and depression; whereas SA improved only depression in women experiencing AI-related arthralgia. |
| Molassiotis et al6
UK |
RCT 3 arm |
Patients with cancer who have completed chemotherapy | Total N = 47 TA: N = 15 AP: N = 16 SAP: N = 16 |
TA: had a 20-min acupuncture session needling 3 points (LI4, SP6, and ST36) bilaterally 3 times a week for 2 weeks AP: patients were taught to apply pressure to the same points for 1 min each, daily for 2 weeks. SAP: was taught to apply pressure in 3 points (LI12, GB33, and BL61) in the same way as in the acupressure group. |
Primary outcome: MFI | Bleeding n = 2 Bruise n = 1 Discomfort in acupuncture point n = 1 Nausea n = 1 Nervous n = 1 |
Significant improvements were found with regards to general fatigue (P < .001), physical fatigue (P = .016), activity (P = .004) and motivation (P = .024). At the end of the intervention, there was a 36% improvement in fatigue levels in the TA group, while the acupressure group improved by 19% and the sham acupressure by 0.6%. Improvements were observed even 2 weeks after treatments, although they were lower (22%, 15%, 7%, respectively). Acupuncture was a more effective method than acupressure or sham acupressure. Subjects needed a longer treatment period to have more sustained results. The trial was methodologically feasible |
| Molassiotis et al15
UK |
Pragmatic RCT 2 arm |
BCs stage I, II, or IIIA | Total N = 302 TA: N = 227 UC: N = 75 |
All trial patients received UC TA: 20 min weekly treatment over 6 weeks. (LI4, SP6, and ST36) |
Primary outcome: MFI Secondary outcome: HADS, FACT-B |
Not reported | The difference in the mean General Fatigue score, between those who received the intervention and those who did not, was 3.11 (95% CI, 3.97-2.25; P < .001). The intervention also improved all other fatigue aspects measured by MFI Acupuncture is an effective intervention for managing the symptom of CRF and improving patients’ quality of life. |
| Molassiotis et al17
UK |
Phase 3, unblinded pragmatic RCT. 3 arm |
BCa diagnosed stage I, II, or IIIa | Total N = 198 TA: N = 65 SF: N = 67 UC: N = 65 |
All patients received 6 week 1 per week × 20 min acupuncture treatment, total of 6 treatments. (LI4, SP6, and ST36) and then all 198 patients were rerandomized into 3 groups of - Acupuncture: another 4 weeks of treatment - Self-acupuncture: 4 weeks of self acupuncture on points SP6 and ST36 - UC |
Primary outcome: MFI (GF) Secondary outcome: HADS, FACT-G |
Spot bleeding on acupuncture points | Primary outcome scores were equivalent between the therapist delivered acupuncture and self-acupuncture (P > .05). A non-significant trend in improving fatigue was observed at the end of 4 weeks in the combined acupuncture arms (P = .07). There was no impact on mood or quality of life of the further acupuncture sessions at 18 weeks beyond the improvement observed in initial trial. Self-acupuncture is an acceptable, feasible, and safe maintenance treatment for patients with CRF. However, overall, maintenance acupuncture did not yield important improvements beyond those observed after an initial clinic-based course of acupuncture. |
| Smith et al21
Australia |
A mixed method RCT 3 arm |
Women diagnosed with BCa | Total N = 30 TA: N = 10 SA: N = 10 WL: N = 10 |
Both acupuncture groups received 3 week 2× per week 20 min acupuncture treatment and another 3 week 1× per week 20 min Acupuncture points (KI3, Ki27, ST36, SP6, CV4, CV6, and addition of 3 points accordingly) SA: Park sham needles |
Primary outcome: BFI Secondary outcome: W-BQ12, MYCaW |
Not reported | There was a significant reduction in fatigue for women receiving acupuncture compared with control after 2 weeks mean difference (MD) 5.3, 95% CI 4.5 to 6.2, P = .05, and a significant improvement in well-being at 6 weeks for acupuncture compared with the sham and wait list control, MD 2.7, 95% CI 2.1 to 3.2, P = .006 Fatigue is a common symptom experienced by people recovering from treatment, and an appropriately powered trial to evaluate the effect of acupuncture is needed. |
Abbreviations: AP, acupressure; SAP, sham acupressure; BCa, breast cancer; BFI, Brief Fatigue Inventory; CTCAE, Common Terminology Criteria for Adverse Events; CRFDS, cancer related fatigue distress scale; FACIT-F, Functional Assessment of Chronic Illness Therapy; SA, sham acupuncture; SF, self-acupuncture; SF-36, quality of life short form; TA, true acupuncture; UC, usual care; WL: wait list; EA, electro acupuncture; PSQI, Pittsburgh Sleep Quality Index; HADS, Hospital Anxiety and Depression Scale; W-BQ12, Well-being Questionnaire; MYCaW, Measure Yourself Concerns and Wellbeing; NSCLC, non-small-cell lung carcinoma.
Outcomes of Acupuncture on CRF
Six individual studies6,15,17,19,21,23 reported a significant improvement in fatigue with acupuncture compared to control groups whereas 3 studies20,22,24 reported no significant difference between true acupuncture and control groups. However, all studies showed some improvement in fatigue when comparing pre and post intervention scores.
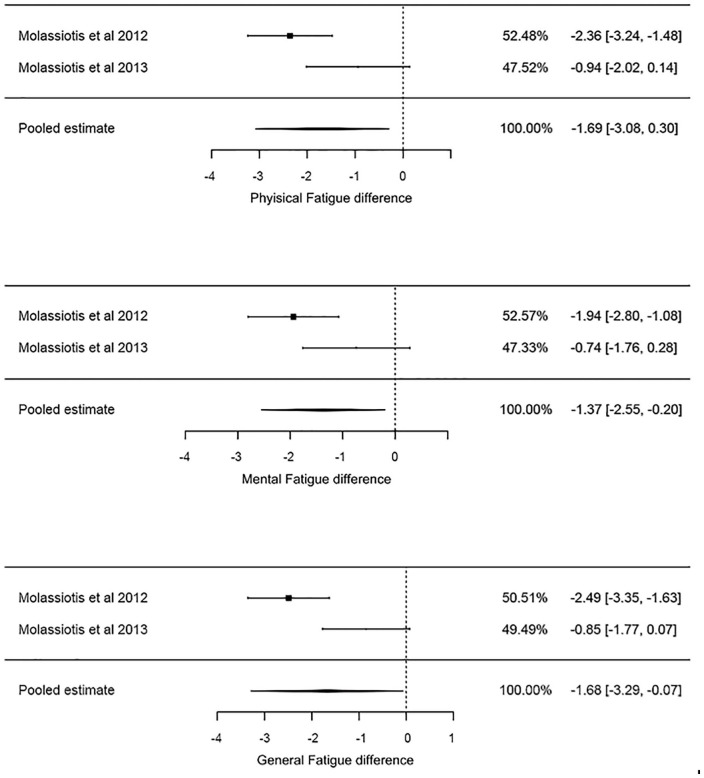
Pooled estimates suggest that the true acupuncture group’s BFI scores were 0.93 points lower with a 95% CI (−1.65, −0.20) compared to sham acupuncture. In the comparison of true acupuncture and usual care groups, the true acupuncture group had an estimated BFI score 2.12 points lower with a 95% CI (−3.21, −1.04) (Figures 2 and 3). Two studies (Figure 4) reported a general reduction across the other fatigue scales (general fatigue, mental fatigue, physical fatigue).
Figure 2.
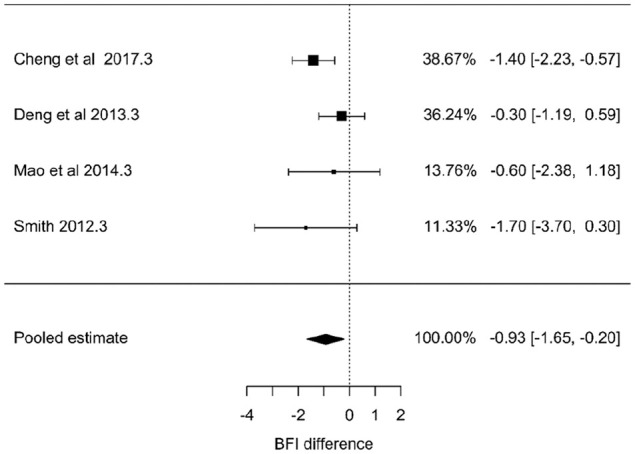
Forest plot of the estimated of true acupuncture and sham acupuncture with cancer related fatigue.
Figure 3.
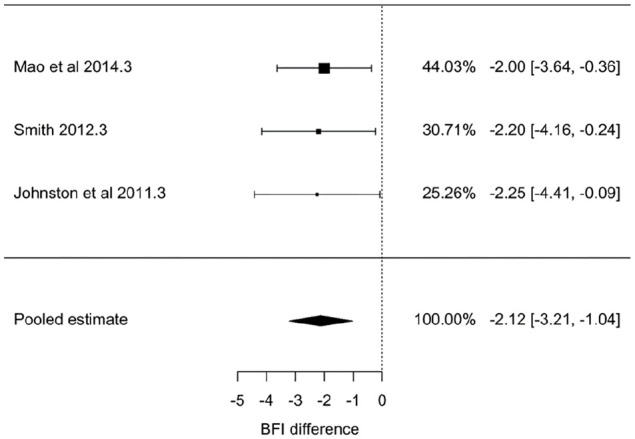
Forest plot of the subgroup analyses of true acupuncture versus usual care.
Figure 4.
Other fatigue estimates.
Safety of Acupuncture and Overall Risk of Bias
Overall, no serious adverse reactions were reported in relation to acupuncture although some studies6,17,19,22-24 have reported the occurrence of minor events directly related to acupuncture treatment (spot bleeding [n = 3], bruising [n = 1], local discomfort [n = 4], nausea and dizziness [n = 4]). Three studies15,20,21 did not collect data relating to adverse effects from participants. The risk of bias (ROB) was detected in respect to blinding participants, blinding assessors, incomplete data outcome reporting, and allocation concealment. Six RCTs6,19-21,23,24 had low ROB and 3 RCTs15,17,22 had a moderate ROB, predominantly in 3 domains (blinding of participants, blinding of assessors, and incomplete data outcome). Individual scores for ROB are presented in Figure 5.
Figure 5.
Risk of bias.
Discussion
This systematic review included 9 RCTs comprising 809 cancer patients with fatigue and suggests that true acupuncture is significantly associated with reducing CRF compared with control groups both with sham acupuncture and usual care. The results of the current study are similar to previous systematic reviews and meta-analyses.11,25,26 However, most individual acupuncture studies reported that the effects of true acupuncture were not significant when compared to sham acupuncture whereas a significant reduction in CRF was found when true acupuncture was compared to usual care.25 Consequently, most previous reviews attempted to demonstrate the effects of true acupuncture compared to combined control groups which included both sham acupuncture and usual care, and did not report the results of comparison between true acupuncture and sham acupuncture that controlled for placebo effects. Hence, previous studies conducted without controlling for the placebo effects of acupuncture provided weaker and less informative evidence in regards to acupuncture in the management of CRF despite attempting to evaluate the efficacy of acupuncture on CRF. Recently a systematic review and meta-analysis27 reported that true acupuncture is associated with reducing CRF compared with sham acupuncture as well as usual care in parallel to the results of the present study.
In recognition of the complexity of designing a sham control group capable of adequately controlling placebo effects in acupuncture RCTs, a number of clinical research guidelines were developed. Their use was recommended in order to facilitate high quality research comparable with RCTs in the last 3 decades that focused on pharmacological or other medical interventions.28
Nonetheless, debate continues to surround the issue of robust RCT design in acupuncture research. Most biomedically trained researchers consider the double-blind RCT to be the most powerful and high quality design available for both pharmacological and non-pharmacological trials despite concerns relating to sham control interventions in non-pharmacological drug trials.29 For acupuncture research, sham acupuncture (non-skin penetrating) devices were developed and utilized in recent several acupuncture RCTs to control for placebo effects and blinding of participants. While some studies reported validation of this method of blinding of participants, several researchers have argued that the application of sham acupuncture (Streitberger placebo needle and Park sham acupuncture) as a control group to control for placebo effects is insufficient.30 Acupuncture-trained researchers have found that Sham acupuncture devices are inducers of a certain magnitude of true acupuncture effect, thus they are not adequate to apply as a control group intervention. With increasing awareness of the shortcomings of sham acupuncture, current acupuncture consensus guidelines recommend robust RCT design with 3 arms (true acupuncture vs sham acupuncture vs usual care).31 Thus, the present review assessed the efficacy of true acupuncture compared to sham acupuncture on CRF following the current acupuncture research guidelines. The current review finds that the positive results from sham controlled RCTs provide plausible evidence for the clinical application of acupuncture in the management of CRF. Although the current review suggests positive outcomes for acupuncture in the management of CRF, it has several limitations. Firstly, of the 9 RCTs, 4 RCTs were conducted with insufficient sample sizes (≤30), which meant there was a potential risk of overestimating positive outcomes. Furthermore, interpretation of these studies, performed with inadequate power and without control of variables such as age, gender, belief, cancer diagnosis, and stage of cancer or specific clinical characteristics, needs to be approached with caution. Next, despite 6 papers6,19-21,23,24 having a low ROB, blinding of participants in individual acupuncture RCTs was the main criterion associated with high risk of bias in individual studies. In addition, 3 RCTs were conducted with a comparison to usual care without a sham acupuncture control, which in turn meant that it was impossible to definitively attribute the improved CRF in the acupuncture group solely to acupuncture itself. Henceforth, the reliability of the evidence presented here is limited. Furthermore, substantial heterogeneity was observed in the RCTs which may downgrade the level of evidence from high to moderate. Sensitivity analyses were completed through subgroup analyses, which showed reduced heterogeneity (Figures 2 and 3) for true versus sham acupuncture and true versus usual care. in addition to inconsistency in control groups (sham and usual care), there were several variations in the parameters of the acupuncture intervention (acupuncture point selection, needle retention time, intervention period, total acupuncture treatment sessions, and study populations) in each study. Hence, it is difficult to draw conclusions about the formulation of a standard acupuncture protocol to manage CRF for cancer survivors.
Future trials of acupuncture for CRF should consider the limitations of current studies and design robust RCTs following the CONSORT and STRICT (Standards for Reporting Interventions in Clinical Trials of Acupuncture) guidelines as recommended by the acupuncture research consensus guidelines.31 Moreover, all studies included in this review were measured fatigue with patient reported outcomes (PRO) including BFI, MFI, and FACIT-F. It would be beneficial if future studies included fatigue related biomarkers such as inflammatory cytokines,32 salivary protein,33 and oxidative stress34 to investigate the physiological mechanisms underlying the effects of acupuncture on fatigue response.
Conclusion
Given that CRF is a debilitating symptom among cancer survivors that has proven complex to manage, it is important to explore a wide range of treatment options. The findings of this systematic review and meta-analysis suggest that acupuncture has clinical applications in the management of CRF in conjunction with standard care. Investigating the physiological mechanisms underlying the effects of acupuncture on CRF with biomarkers including cytokines will provide important insights into future clinical applications. Acupuncture for cancer survivors with fatigue, particularly those receiving chemotherapy and radiation therapy that induce fatigue, can have a beneficial effect on fatigue and overall quality of life, when used as an adjunctive intervention to conventional cancer care. Therefore, it is recommended that acupuncture be incorporated into guidelines for the management of CRF in order to improve patient care.
Footnotes
Author Contributions: Reviewer (AJ, CB, and BO) had full access to the study data and take responsibility for the integrity and accuracy of data analysis. Concept and design: All authors. Acquisition, analysis, or interpretation of data: AJ, CB, IM, and BO. Draft of the manuscript: AJ, CB, IM, and BO. Critical revision of the manuscript for important intellectual content: All authors. Statistical analysis: CB.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorships, and/or publication of this article.
ORCID iD: Byeongsang Oh  https://orcid.org/0000-0002-7204-6716
https://orcid.org/0000-0002-7204-6716
References
- 1. Brown LF, Kroenke K. Cancer-related fatigue and its associations with depression and anxiety: a systematic review. Psychosomatics. 2009;50:440-447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Glaus A, Crow R, Hammond S. A qualitative study to explore the concept of fatigue/tiredness in cancer patients and in healthy individuals. Eur J Cancer Care. 1996;5:8-23. [DOI] [PubMed] [Google Scholar]
- 3. Richardson PG, Laubach JP, Schlossman RL, Mitsiades C, Anderson K. Complications of multiple myeloma therapy, part 1: risk reduction and management of peripheral neuropathy and asthenia. [Erratum appears in J Natl Compr Canc Ne 2010 Mar;8(3):xlv Note: Dosage error in article text]. J Natl Compr Canc Ne. 2010;8:S4-S12. [DOI] [PubMed] [Google Scholar]
- 4. Saligan LN, Kim HS. A systematic review of the association between immunogenomic markers and cancer-related fatigue. Brain Behav Immun. 2012;26:830-848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Vickers AJ, Cronin AM, Maschino AC, et al. Acupuncture for chronic pain: individual patient data meta-analysis. Arch intern Med. 2012;172:1444-1453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Molassiotis A, Sylt P, Diggins H. The management of cancer-related fatigue after chemotherapy with acupuncture and acupressure: a randomised controlled trial. Complement Ther Med. 2007;15:228-237. [DOI] [PubMed] [Google Scholar]
- 7. Groenvold M, Petersen MA, Idler E, Bjorner JB, Fayers PM, Mouridsen HT. Psychological distress and fatigue predicted recurrence and survival in primary breast cancer patients. Breast Cancer Res Treat. 2007;105:209-219. [DOI] [PubMed] [Google Scholar]
- 8. Escalante CP, Manzullo EF. Cancer-related fatigue: the approach and treatment. J Gen Intern Med. 2009;24:S412-S416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Minton O, Richardson A, Sharpe M, Hotopf M, Stone P. Drug therapy for the management of cancer-related fatigue. Cochrane Database of Syst Rev. 2010;7:CD006704. [DOI] [PubMed] [Google Scholar]
- 10. Finnegan-John J, Molassiotis A, Richardson A, Ream E. A systematic review of complementary and alternative medicine interventions for the management of cancer-related fatigue. Integr Cancer Ther. 2013;12:276-290. [DOI] [PubMed] [Google Scholar]
- 11. Posadzki P, Moon T-W, Choi T-Y, Park T-Y, Lee MS, Ernst E. Acupuncture for cancer-related fatigue: a systematic review of randomized clinical trials. Support Care Cancer. 2013;21:2067-2073. [DOI] [PubMed] [Google Scholar]
- 12. Kuchinski AM, Reading M, Lash AA. Treatment-related fatigue and exercise in patients with cancer: a systematic review. Medsurg Nurs. 2009;18:174-180. [PubMed] [Google Scholar]
- 13. Wanchai A, Armer JM, Stewart BR. Nonpharmacologic supportive strategies to promote quality of life in patients experiencing cancer-related fatigue: a systematic review. Clin J Oncol Nurs. 2011;15:203-214. [DOI] [PubMed] [Google Scholar]
- 14. Vickers AJ, Straus DJ, Fearon B, Cassileth BR. Acupuncture for postchemotherapy fatigue: a phase II study. J Clin Oncol. 2004;22:1731-1735. [DOI] [PubMed] [Google Scholar]
- 15. Molassiotis A, Bardy J, Finnegan-John J, et al. Acupuncture for cancer-related fatigue in patients with breast cancer: a pragmatic randomized controlled trial. J Clin Oncol. 2012;30:4470-4476. [DOI] [PubMed] [Google Scholar]
- 16. Wu C, Zheng Y, Duan Y, et al. Nonpharmacological interventions for cancer-related fatigue: a systematic review and Bayesian network meta-analysis. Worldviews Evid Based Nurs. 2019;16:102-110. [DOI] [PubMed] [Google Scholar]
- 17. Molassiotis A, Bardy J, Finnegan-John J, et al. A randomized, controlled trial of acupuncture self-needling as maintenance therapy for cancer-related fatigue after therapist-delivered acupuncture. Ann Oncol. 2013;24:1645-1652. [DOI] [PubMed] [Google Scholar]
- 18. Higgins JPT, Altman DG, Gøtzsche PC, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Johnston MF, Hays RD, Subramanian SK, et al. Patient education integrated with acupuncture for relief of cancer-related fatigue randomized controlled feasibility study. BMC Complement Altern Med. 2011;11:49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Mao JJ, Farrar JT, Bruner D, et al. Electroacupuncture for fatigue, sleep, and psychological distress in breast cancer patients with aromatase inhibitor-related arthralgia: a randomized trial. Cancer. 2014;120:3744-3751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Smith C, Carmady B, Thornton C, Perz J, Ussher JM. The effect of acupuncture on post-cancer fatigue and well-being for women recovering from breast cancer: a pilot randomised controlled trial. Acupunct Med. 2013;31:9-15. [DOI] [PubMed] [Google Scholar]
- 22. Balk J, Day R, Rosenzweig M, Beriwal S. Pilot, randomized, modified, double-blind, placebo-controlled trial of acupuncture for cancer-related fatigue. J Soc Integr Oncol. 2009;7:4-11. [PubMed] [Google Scholar]
- 23. Cheng CS, Chen LY, Ning ZY, et al. Acupuncture for cancer-related fatigue in lung cancer patients: a randomized, double blind, placebo-controlled pilot trial. Support Care Cancer. 2017;25:3807-3814. [DOI] [PubMed] [Google Scholar]
- 24. Deng G, Chan Y, Sjoberg D, et al. Acupuncture for the treatment of post-chemotherapy chronic fatigue: a randomized, blinded, sham-controlled trial. Support Care Cancer. 2013;21:1735-1741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Ling WM, Lui LY, So WK, Chan K. Effects of acupuncture and acupressure on cancer-related fatigue: a systematic review. Oncol Nurs Forum. 2014;41:581-592. [DOI] [PubMed] [Google Scholar]
- 26. Zhang Y, Lin L, Li H, Hu Y, Tian L. Effects of acupuncture on cancer-related fatigue: a meta-analysis. Support Care Cancer. 2018;26:415-425. [DOI] [PubMed] [Google Scholar]
- 27. Zeng Y, Luo T, Finnegan-John J, Cheng ASK. Meta-analysis of randomized controlled trials of acupuncture for cancer-related fatigue. Integr Cancer Ther. 2014;13:193-200. [DOI] [PubMed] [Google Scholar]
- 28. World Health Organization. Regional Office for the Western P. Guidelines for Clinical Research on Acupuncture. Manila: WHO Regional Office for the Western Pacific; 1995. [Google Scholar]
- 29. Edmond SN, Turk DC, Williams DA, Kerns RD. Considerations of trial design and conduct in behavioral interventions for the management of chronic pain in adults. Pain Rep. 2019;4:e655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Lundeberg T, Lund I, Sing A, Näslund J. Is placebo acupuncture what it is intended to be? Evid Based Complement Alternat Med. 2011;2011:932407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Witt CM, Aickin M, Baca T, et al. Effectiveness guidance document (EGD) for acupuncture research—a consensus document for conducting trials. BMC Complement Altern Med. 2012;12:148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Prell T, Witte OW, Grosskreutz J. Biomarkers for dementia, fatigue, and depression in Parkinson’s disease. Front Neurol. 2019;10:195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Xu YL, Gong YN, Xiao D, et al. Discovery and identification of fatigue-related biomarkers in human saliva. Eur Rev Med Pharmacol Sci. 2018;22:8519-8536. [DOI] [PubMed] [Google Scholar]
- 34. Fukuda S, Nojima J, Motoki Y, et al. A potential biomarker for fatigue: oxidative stress and anti-oxidative activity. Biol Psychol. 2016;118:88-93. [DOI] [PubMed] [Google Scholar]