FIGURE 1.
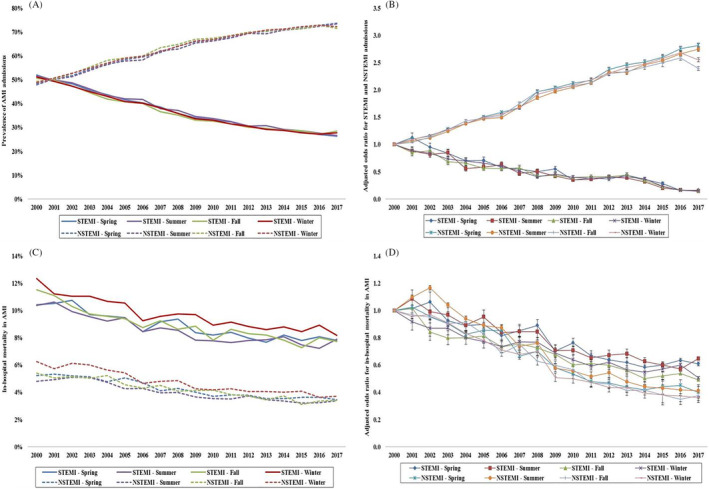
Trends in the prevalence and in‐hospital mortality in AMI admissions stratified by type of AMI. A, Unadjusted temporal trends of the proportion of AMI admissions stratified by type of AMI during spring, summer, fall, and winter (P < .001 for trend over time). B, Adjusted odds ratio for STEMI and NSTEMI weekend admissions by year (with 2000 as the referent); adjusted for age, sex, race, comorbidity, primary payer, socioeconomic status, STEMI location, hospital region, hospital location and teaching status, and hospital bed‐size (P < .001 for trend over time). C, Unadjusted in‐hospital mortality in AMI admissions stratified by type of AMI during spring, summer, fall, and winter (P < .001 for trend over time). D, Adjusted odds ratio for in‐hospital mortality by year (with 2000 as the referent) in AMI admissions stratified by type of AMI and weekend vs weekday admission; adjusted for age, sex, race, comorbidity, primary payer, hospital region, hospital location and teaching status, hospital bed‐size, weekend admission, multiorgan failure, cardiogenic shock, cardiac arrest, coronary angiography, PCI, pulmonary artery catheterization, mechanical circulatory support, invasive mechanical ventilation, and acute hemodialysis (P < .001 for trend over time). AMI, acute myocardial infarction; NSTEMI, non‐ST‐segment elevation myocardial infarction; STEMI, ST‐segment elevation myocardial infarction
