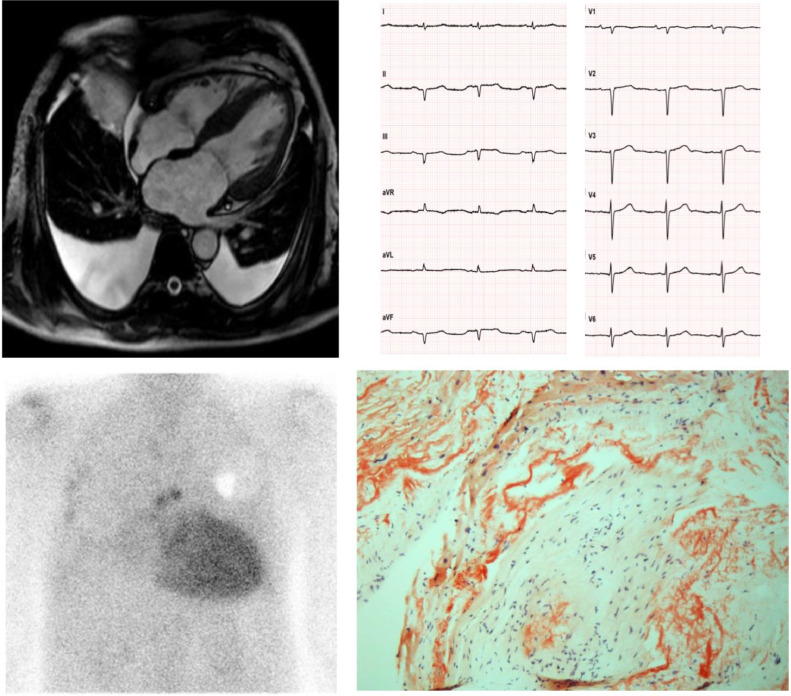
Fig. 3.
A 62-year-old man diagnosed with hypertrophic cardiomyopathy. The patient underwent a cardiological evaluation due to palpitations and a family history of sudden death (father died at 78). An ECG revealed low-voltage QRS in the peripheral leads, Q waves in the inferior leads and poor R wave progression in the precordial leads (‘pseudonecrosis’). A Holter ECG revealed paroxysmal AF and 3 consecutive ectopic ventricular beats >120 bpm. The echocardiogram and CMR showed LV hypertrophy (interventricular septum > 15 mm), left atrial dilatation and pericardial and bilateral pleural effusion. A diagnosis of hypertrophic cardiomyopathy was made, and the patient was implanted with an ICD for primary prevention of SCD. After 2 years, he was referred to our Cardiovascular Department for unexplained syncopal episodes. No arrhythmias were detected by the ICD. The patient complained of a one-year history of symptomatic bilateral carpal tunnel syndrome and discontinued anti-hypertensive drugs due to poor tolerability. An endomyocardial biopsy revealed diffuse amyloid fibrils upon Congo red staining (courtesy of Professor Rossana Bussani, MD, Institute of Pathological Anatomy and Histology, University of Trieste, Italy). Scintigraphy revealed high-grade (Perugini 3) cardiac accumulation of bone tracers, and after excluding a monoclonal component a diagnosis of ATTR-CA was made. Genetic testing revealed wild type transthyretin, and the patient was started on Tafamidis. Legend: AF, Atrial Fibrillation; CMR, Cardiac Magnetic Resonance; ECG, Electrocardiogram; ICD, Implantable Cardioverter Defibrillator; SCD, Sudden Cardiac Death.