Abstract
Objective
To quantify how the first public announcement of confirmed coronavirus disease 2019 (COVID‐19) in Italy affected a metropolitan region's emergency medical services (EMS) call volume and how rapid introduction of alternative procedures at the public safety answering point (PSAP) managed system resources.
Methods
PSAP processes were modified over several days including (1) referral of non‐ill callers to public health information call centers; (2) algorithms for detection, isolation, or hospitalization of suspected COVID‐19 patients; and (3) specialized medical teams sent to the PSAP for triage and case management, including ambulance dispatches or alternative dispositions. Call volumes, ambulance dispatches, and response intervals for the 2 weeks after announcement were compared to 2017–2019 data and the week before.
Results
For 2 weeks following outbreak announcement, the primary‐level PSAP (police/fire/EMS) averaged 56% more daily calls compared to prior years and recorded 9281 (106% increase) on Day 4, averaging ∼400/hour. The secondary‐level (EMS) PSAP recorded an analogous 63% increase with 3863 calls (∼161/hour; 264% increase) on Day 3. The COVID‐19 response team processed the more complex cases (n = 5361), averaging 432 ± 110 daily (∼one‐fifth of EMS calls). Although community COVID‐19 cases increased exponentially, ambulance response intervals and dispatches (averaging 1120 ± 46 daily) were successfully contained, particularly compared with the week before (1174 ± 40; P = 0.02).
Conclusion
With sudden escalating EMS call volumes, rapid reorganization of dispatch operations using tailored algorithms and specially assigned personnel can protect EMS system resources by optimizing patient dispositions, controlling ambulance allocations and mitigating hospital impact. Prudent population‐based disaster planning should strongly consider pre‐establishing similar highly coordinated medical taskforce contingencies.
Keywords: ambulances, call centers, COVID‐19 pandemic, disaster planning, emergency medical dispatch, emergency medical services, SARS‐CoV‐2 infection
1. INTRODUCTION
1.1. Background
The first cases of a severe acute respiratory syndrome stemming from the novel coronavirus designated severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2) were reported by China in December 2019. 1 , 2 As the virus quickly spread to other countries, transmission was amplified by a large number of asymptomatic, yet highly contagious, carriers. 1 , 3 Despite early preventive measures to limit spread, the nation of Italy soon was challenged with the largest number of patients in Europe with this new and poorly understood disease, coronavirus disease 2019 (COVID‐19). 4 , 5 , 6 , 7
The first case in Italy was confirmed on February 21, 2020. Following widespread media coverage, an unprecedented increase in telephone calls to “1‐1‐2” (European equivalent to 9‐1‐1, 9‐9‐9, or 0‐0‐0 emergency call systems) began to escalate. Many callers were “worried‐well” persons requesting information and guidance about the new illness. Many other callers were concerned about symptoms they or family members were experiencing. Escalating call volumes soon challenged the capacity of the Azienda Regionale Emergenza Urgenza (AREU), the regional emergency medical services (EMS) system of Milan and surrounding Lombardy. 8
1.2. Importance
Recognizing that call volumes were becoming overwhelming, a strategic plan was implemented immediately to protect ambulance resources and the healthcare system at large.
In contrast to most public safety answering point (PSAP) systems worldwide, on a day‐to‐day basis, the Milan AREU dispatch call center already incorporates expert medical oversight with a rotating team of on‐site physicians and nurses provided by the Niguarda Hospital and the School of Medicine and Surgery at the University of Milano‐Bicocca and University of Milan. Therefore, the medical team members, including their supervising medical director (RF), are quite familiar with the 1‐1‐2 system and its operation and they already provide the medical care protocols for the dispatch center as well as real‐time medical direction and counsel to ambulance crews on‐scene with patients. They can also make disposition decisions related to hospital destinations and coordinate with those hospitals in real time. In that respect and in contrast to most other PSAP operations, they were well positioned and also prospectively authorized to rapidly modify alternative procedures and also to seamlessly assign additional personnel to the AREU PSAP. 9 Also, most of the physician members of the AREU were critical care specialists based at the one of the largest tertiary care facilities in Italy who possessed the most up‐to‐date knowledge about COVID‐19. They also held close affiliations with local public health and infectious disease (ID) specialists who could join in this deployment to the PSAP.
The multidisciplinary team's main task was to attempt identification of possible COVID‐19 patients but also to help determine an appropriate disposition, including directives to remain in isolation, go to the most appropriate hospital, or make other referrals as indicated. The multilevel, interdisciplinary response plan would, it is hoped, enable a more comprehensive interaction between the emergency medical system and regional hospitals as well as public health authorities and the community at large. 10
1.3. Goals of this investigation
Accordingly, the primary study purpose was (1) to quantitate the onset, timing, and magnitude of increased EMS call volumes in the largest metropolitan region in Northern Italy after announcement of the nation's first confirmed case of COVID‐19; and (2) analyze how well rapid reorganization of the EMS dispatching system could control ambulance dispatches, response intervals, and other system resources by introducing tailored COVID‐19 algorithms, increased staffing, and a specialized team of healthcare system‐oriented call‐takers.
2. METHODS
2.1. Setting
AREU, responsible for the metropolitan region of Milan (population 4.2 million), covers a jurisdiction of 1980 square kilometers, one of the largest in Italy. The primary‐level PSAP (PSAP‐1) is the initial recipient of 1‐1‐2 phone calls from citizens seeking police, fire, or medical assistance. PSAP‐1 is staffed by 12 call‐taker technicians (lay dispatchers) at any given time. The PSAP‐1 is tasked with redirecting medically related calls to the medical (secondary‐level) PSAP (PSAP‐2), which manages regional EMS resources. The technicians staffing PSAP‐1 are equivalent to conventional 9‐1‐1 or 9‐9‐9 systems dispatchers utilized in other nations. PSAP‐2 is similarly staffed with 14 equivalent technicians (dispatchers), 7 nurses and 2 physicians (working in teams) who (1) assess and triage medical emergencies; (2) dispatch ambulances (and other healthcare vehicles); and (3) assign the most appropriate hospital destination based on proximity, specific patient needs, bed availability, and operational functioning (Figure 1A). 8 This function includes management of reports from on‐scene ambulance crews. The crews are composed of advanced level emergency medical technicians who routinely receive directives for further care, dispositions, and hospital destinations from these control room doctors and nurses at PSAP‐2.
FIGURE 1.
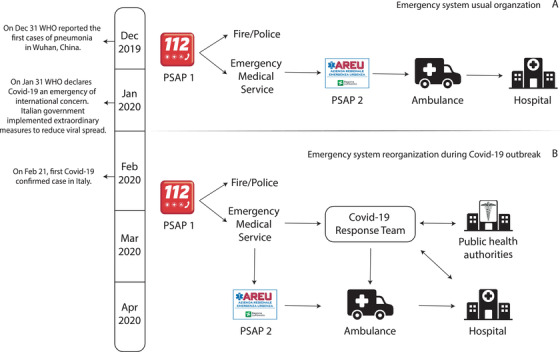
Reorganization of the 1‐1‐2 emergency response system for the metropolitan area of Milan during the early phases of the coronavirus disease 2019 (COVID‐19) outbreak in Italy. PSAP, public safety answering point; WHO, World Health Organization
The Bottom Line
During the COVID19 pandemic the sudden profound escalation of emergency medical services (EMS) call volume can be mitigated by having an EMS physician specialist on‐site at the public safety answering point thereby optimizing EMS system resources by rapidly reorganizing dispatch operations using tailored algorithms, specially assigned personnel, providing real‐time patient dispositions, controlling ambulance allocations, and assigning of hospital destination.
2.2. Main interventions
With escalating call volumes, several actions occurred (Figure 1B). 9 Staffing was adjusted and COVID‐tailored algorithms were provided to both PSAP‐1 and PSAP‐2 staff to help better navigate and manage phone calls.
PSAP‐1 Staffing: Staffing was rapidly augmented from 12 to 30 technicians on duty at any given time using extended work shifts, overtime activity, and recruitment of additional personnel.
PSAP‐1 Call‐Takers Algorithm and Responsibilities: PSAP‐1 technicians applied intake screenings to detect callers with acute medical problems or potential COVID‐19 conditions versus callers simply requesting information about COVID‐19. Those worried‐well callers were given a special counseling service number provided by regional public health authorities. If fever and respiratory symptoms were reported, PSAP‐1 technicians directed those calls to PSAP‐2 for immediate management and dispositions based on symptom severity (Figure 2).
PSAP‐2 Staffing: Similar to PSAP‐1, staffing enhancements emanated from shift modifications, overtime activity, and additional personnel including the specialized COVID‐19 medical response team. Team members were assigned soon after the announcement of the first SARS‐Cov‐2 case (February 21, 2020). Staffing was progressively amplified over the next 3 days. 9 With concomitant suspension of elective surgeries and other hospital activities, additional members of the anesthesia department experienced in EMS and emergency medicine became immediately available to supplement and rotate with the original core group. The team also incorporated public health department physicians and ID specialists for on‐site counsel and additional coordination of patient dispositions. The PSAP‐2 team now included 2 additional technicians (dispatchers), 2 additional nurses, and 8 additional physicians (either ID specialists or physicians from the regional public health department or emergency medical service specialists from Niguarda Hospital), each tasked with complementary responsibilities.
PSAP‐2 Call‐Takers Algorithm and Responsibilities: Taking the transferred call from PSAP‐1, PSAP‐2 call‐takers further assessed medical issues using software‐guided interviews that scored severity according to the degree of consciousness, signs/symptoms of respiratory distress or circulatory failure, and several other predesignated signs/symptoms (Table 1). If cough, dyspnea, and fever were identified, callers were asked about suspected or confirmed COVID‐19 contacts, the caller's residence location (and/or any prolonged stay in COVID‐19 high‐risk zones as indicated by public health authorities) or contact with individuals displaying respiratory symptoms from those hot zones or those with recent travel to/from China (Figure 3). If the previous conditions were excluded, the event was managed as routine EMS activity, including ambulance dispatches. If the caller's information met criteria for suspected COVID‐19 and had a moderate to severe severity score, ambulances were dispatched immediately with preset directives for using strict personal protective equipment (PPE) precautions and vehicle sanitization procedures. 10 With milder severity scores, calls were referred to a member of the specialized AREU COVID‐19 team.
-
Responsibilities of COVID‐19 Team Members:
The public health specialists were responsible for counseling, recording, and isolating suspected or confirmed COVID‐19 cases originally identified by PSAP‐1 call‐takers as being non‐urgent.
The EMS physician specialists on the team were responsible for (1) supervision of PSAP‐2 activities and direct reassessments of COVID‐19 cases classified as urgent; (2) deciding on ambulance dispatch and hospitalization for cases with moderate or severe respiratory symptoms; and (3) continuous interaction with medical authorities and hospitals to facilitate proper continuity of care and bed availability using specifically designed algorithms for identification and management of COVID‐19, attempting to better standardize and guide the difficult decisionmaking process (Figure 3). This role was, in essence, an escalation of their day‐to‐day functions at the PSAP‐2, which are similar to the functions of many traditional centralized regional EMS base stations in the United States and other nations, although these are generally stationed at hospitals. After taking a report from the on‐scene ambulance crews, they routinely provide real‐time medical direction to those who are on scene with the patient including further directives about treatment at the scene or other dispositions. These physicians also coordinate with local hospitals routinely and make destination and triage decisions for the crews based on real‐time feedback and routine communications with area receiving facilities.
Ambulances were promptly dispatched for hospital transport when identifying severe symptoms (eg, fever refractory to antipyretics with productive cough and dyspnea). 11 , 12 , 13
To avoid hospital overload and unnecessary ambulance dispatches, subjects with mild to moderate symptoms were home‐quarantined for 14 days or less if at‐home molecular assay testing for SARS‐Cov‐2 returned negative results. 14 , 15 Quarantined subjects were instructed to contact local health authorities through dedicated numbers but also to call 1‐1‐2 if new symptoms arose or preexisting symptoms worsened significantly. Public health specialists also provided detailed instructions to patients and families on how to limit viral spread at home. 16
A daily report of quarantined COVID‐19 cases (and co‐habitants) was sent to local health authorities by a COVID‐19 response team physician.
FIGURE 2.
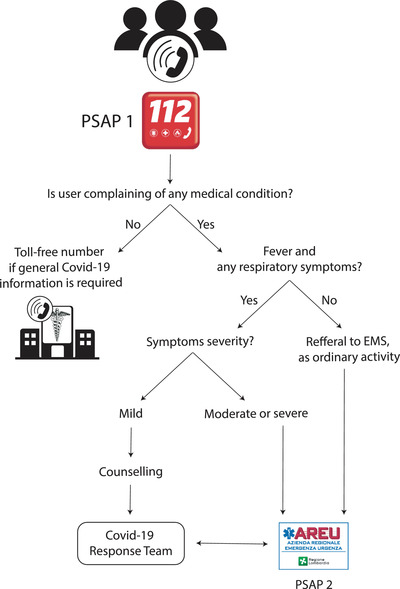 Algorithm to guide the primary public safety answering point (PSAP‐1) call‐takers in detection of coronavirus disease 2019 (COVID‐19) suspected cases. EMS, emergency medical services
Algorithm to guide the primary public safety answering point (PSAP‐1) call‐takers in detection of coronavirus disease 2019 (COVID‐19) suspected cases. EMS, emergency medical servicesFIGURE 3.
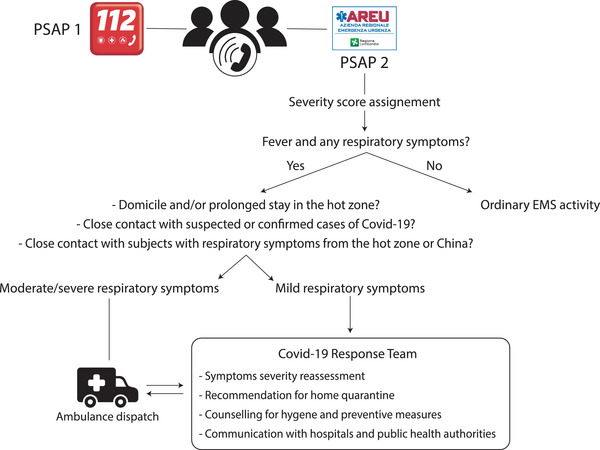 Algorithm to detect suspected coronavirus disease 2019 (COVID‐19) cases, implemented for the secondary (emergency medical services) public safety answering point (PSAP‐2) call‐receivers and the specialized COVID‐19 response team located on‐site at PSAP‐2
Algorithm to detect suspected coronavirus disease 2019 (COVID‐19) cases, implemented for the secondary (emergency medical services) public safety answering point (PSAP‐2) call‐receivers and the specialized COVID‐19 response team located on‐site at PSAP‐2
TABLE 1.
The concurrent World Health Organization criteria for clinical severity provided at the time of study (https://www.who.int/publications/i/item/clinical-management-of-covid-19)
| Severity | Clinical presentation |
|---|---|
| Mild disease | ‐ Symptomatic patients (fever, cough, fatigue, anorexia, myalgia, sore throat, nasal congestion, headache, diarrhea, nausea, anosmia, ageusia) with no evidence of pneumonia or hypoxia. |
| Moderate disease | ‐ Clinical signs of pneumonia (fever, cough, dyspnea, fast breathing, shortness of breath) but no signs of severe pneumonia, including SpO2 ≥ 90% on room air. |
| Severe disease | ‐ Clinical signs of severe pneumonia (fever, cough, respiratory rate > 30 breaths/min, severe respiratory distress, SpO2 < 90% breathing ambient air). |
| ‐ Clinical signs of acute respiratory distress syndrome (ARDS) according to Berlin definition. |
2.3. Data collection and analysis
Data were derived from a regionally developed and commercially available emergency management software version 6.8.5 for computer‐aided dispatch (Emma, Beta80 Group S.P.A., Milan, Italy; http://us.beta80group.com/about/) and exported using SAS Web Report Studio 4.4 M4 (SAS institute Inc., Cary, NC, USA). Sensitive personal data files were stored in access‐restricted cloud‐based storage. Access was restricted to authorized EMS members who were responsible for ensuring data quality, integrity, and confidentiality.
Calls to 1‐1‐2 and resulting ambulance dispatches for February 14 through March 4, 2020 were reported and compared corresponding periods for 2017–2019 using means ± SD. The February 21 to March 4 dates were analyzed to reflect how the resources were managed during the unstable period occurring between the first announcement of the COVID‐19 case and the days leading up to the imposition of a stay‐at‐home policy. For a reasonable contemporary comparison, the prior week's data were also examined, Before and after comparisons of ambulance arrival time at the patient's location after dispatch were reported as medians (with interquartile range) along with previous 3 years’ comparisons. Event classification (medical, traumatic, or others) and severity code (white, green, yellow, or red) were also evaluated for the first 3 months of 2020 and presented as percentage distribution.
Normality of data distribution was assessed with the Shapiro‐Wilk test. For normally distributed variables, data comparisons were made across years using the parametric Student t test. Non‐normally distributed variables are described as medians with interquartile ranges (IQR). Time of ambulance arrival at the patient location after dispatch from February 21 to March 4, 2020 was compared to the corresponding period of the 3 previous years using the Kruskal‐Wallis test followed by Dunn's multiple comparison. P values <0.05 were considered statistically significant. Statistical analysis was conducted using Excel version 16.37 (Microsoft, Redmond, WA, USA) and STATA version 13 (StataCorp, College Station, TX, USA). Graphics were created through Prism 8.0 (GraphPad Software, San Diego, CA).
3. RESULTS
During the immediate 2 weeks following public announcement of the first COVID‐19 case in Italy (February 21), the 1‐1‐2 primary call center (PSAP‐1) recorded a 56% increase in average call volumes for metropolitan Milan compared to the average call volume for the same 2‐week period during the previous 3 years. However, this heightened 2‐week average was largely driven by the early rapid escalation of call volumes over the first few days reaching a 24‐hour peak of 9281 (averaging ∼400/hour) during Day 4 (February 24).
Simultaneously, the EMS PSAP‐2 center recorded an analogous 63% increase in the analogous 2‐week call volume, but that again was driven by a corresponding 24‐hour peak of 3863 calls (∼161 calls/hour) on Day 3 (February 23), a 264% increase from the prior 3 years’ average for that day (Table 2, Figure 4A).
TABLE 2.
Daily emergency medical services (EMS) public safety answering point (PSAP‐2) call‐volumes in 2020 compared to 3 previous years
| Day | 2017 | 2018 | 2019 | 2020 | Mean for 2017‐2018‐2019 | Percentage increase for 2020 versus mean for 2017‐2018‐2019 |
|---|---|---|---|---|---|---|
| Feb 14 | 1221 | 927 | 1337 | 1667 | 1162 ± 211 | 44% |
| Feb 15 | 1334 | 1212 | 1429 | 1597 | 1325 ± 109 | 21% |
| Feb 16 | 1345 | 1260 | 1360 | 1494 | 1322 ± 54 | 13% |
| Feb 17 | 1330 | 1093 | 1364 | 1707 | 1262 ± 148 | 35% |
| Feb 18 | 1222 | 1147 | 1449 | 1578 | 1273 ± 157 | 24% |
| Feb 19 | 1275 | 1204 | 1324 | 1560 | 1268 ± 60 | 23% |
| Feb 20 | 1310 | 1213 | 1326 | 1470 | 1283 ± 61 | 15% |
| Feb 21 | 1235 | 729 | 1330 | 1901 | 1098 ± 323 | 73% |
| Feb 22 | 1263 | 845 | 1347 | 3083 | 1152 ± 269 | 168% |
| Feb 23 | 1203 | 768 | 1213 | 3863 | 1061 ± 254 | 264% |
| Feb 24 | 1209 | 1342 | 1161 | 3446 | 1237 ± 94 | 179% |
| Feb 25 | 1356 | 1121 | 1387 | 2472 | 1288 ± 145 | 92% |
| Feb 26 | 1232 | 1249 | 1318 | 2210 | 1266 ± 46 | 75% |
| Feb 27 | 1260 | 1204 | 1379 | 1913 | 1281 ± 89 | 49% |
| Feb 28 | 1123 | 1223 | 1405 | 1969 | 1250 ± 143 | 57% |
| Feb 29 | N/A | N/A | N/A | 1798 | ||
| Mar 1 | 1225 | 1280 | 1479 | 1735 | 1328 ± 134 | 31% |
| Mar 2 | 1283 | 1244 | 1351 | 1881 | 1293 ± 54 | 46% |
| Mar 3 | 1246 | 1139 | 1222 | 1956 | 1202 ± 56 | 63% |
| Mar 4 | 1135 | 1268 | 1393 | 1881 | 1265 ± 129 | 49% |
FIGURE 4.
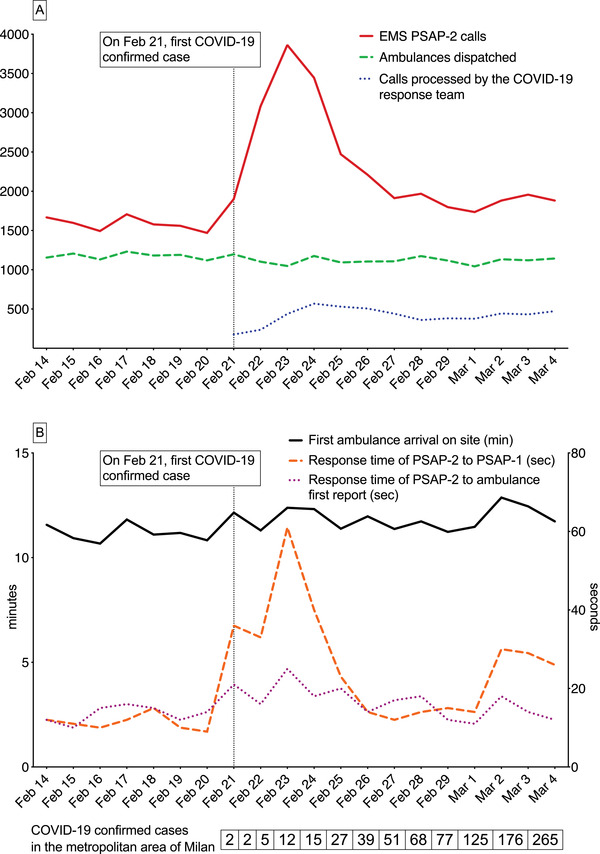
Comparison of the week before, and 2 weeks after, the public announcement of the first confirmed coronavirus disease 2019 (COVID‐19) case in Italy (February 21, 2020). Panel A illustrates the daily number of (1) 1‐1‐2 calls for emergency medical services (EMS) overall, (2) ambulance dispatches, and (3) calls processed by the COVID‐19 medical response team. Panel B illustrates the day‐to‐day time intervals for (1) the time of receipt of the EMS dispatch call to on‐scene arrival time of the ambulances; (2) hold times for the processing and call transfer from the primary public safety answering point (PSAP) to the secondary EMS PSAP (PSAP‐2); and (3) hold time for ambulances waiting to report to the PSAP‐2 medical team for providing their on‐site medical report and receive directives from the medical team
The medical calls processed and triaged by PSAP‐2 staff that did not result in an ambulance dispatch had an average daily volume of 408 ± 61 (26% of total PSAP‐2 calls) the week before the outbreak, but that figure rose to 1580 ± 795 (55% of all PSAP‐2 calls) during the first week of COVID‐19 and still remained high (748 ± 59) during the second week (40% of PSAP‐2 calls). This alleviation of ambulance dispatches was largely because of the effects of the newly implemented COVID‐19 algorithms but was mostly because of the efforts of the COVID‐19 response team embedded at PSAP‐2. Specifically, during that immediate 2‐week period after the COVID‐19 announcement (February 21 to March 4), the PSAP‐2 medical team processed and triaged a total of 5361 phone calls (averaging 432 ± 110 daily) or about one fifth of the total incoming PSAP‐2 calls received during that period. However, on Day 4 (February 24), they processed nearly 600 cases (∼25/hour) of these more complex dispositions. Of note, three quarters (329 + 16) of the 432 + 110 average daily cases managed (and further triaged) by the embedded COVID‐19 specialists team were initially classified as “urgent” by the PSAP‐2 call‐takers.
Accordingly, even though the number of confirmed COVID‐19 cases in the community rose exponentially and formal areawide lockdowns did not occur until March 8, the number of ambulance dispatches remained, on the average, relatively controlled throughout the targeted study period (Figure 4A). Specifically, there was a 9% increase in the average number of daily ambulance dispatches compared to prior 3 years’ average (1120 ± 46 per day vs 1024 ± 29; P < 0.001). However, that postannouncement average was actually lower than that observed during the week before the outbreak (1174 ± 40 per day; P = 0.02). Moreover, the 24‐hour ambulance dispatch numbers remained steady at 1103, 1048 and 1176 per day, respectively, on February 22, 23, and 24 while the 24‐hour incoming calls to PSAP‐2 were dramatically elevated (3083, 3863, and 3446 per day) representing 168%, 264%, and 179% respective increases from the average of those same dates over the prior 3 years.
Despite the significant elevations in calls being processed and the associated time‐intensive processing intervals required in some cases, the median time of arrival at the patient location after dispatch for all PSAP‐2 calls (urgent or non‐urgent) was 13.5 (IQR: 10–20) minutes, only mildly elevated in 2020 compared to prior years: 12.4 (IQR:9‐18) in 2019 (P = 0.03), 11.7 (IQR: 9–17) in 2018 (P < 0.001), and 11.7 (IQR: 9–16) in 2017 (P < 0.001). More important, for urgent cases (ie, the “yellow” and “red codes” in Figure 5), the corresponding response interval in 2020 was 11.7 (IQR: 8–15) minutes versus 10.8 (IQR: 9–14) in 2019 (P = 0.07), 9.8 (IQR: 8–13) in 2018 (P < 0.001) and 10 (IQR: 8–13) in 2017 (P < 0.001).
FIGURE 5.
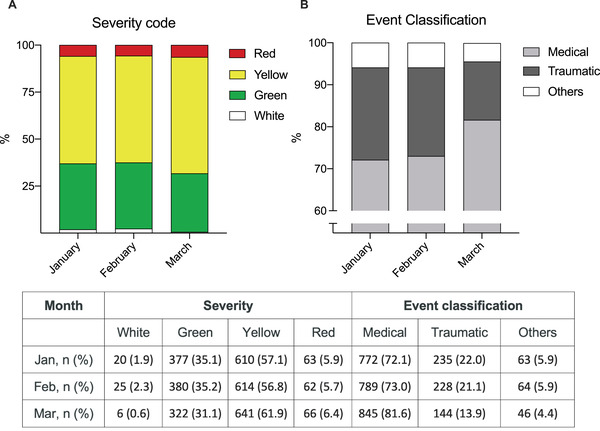
Classification and severity code of emergency medical services (EMS) events
In fact, despite a 4‐fold increase in the call transfer/processing time from PSAP‐1 to PSAP‐2 during the first 3 days (rising from 15 to 60 seconds), that delay was rapidly controlled as staffing increased (Figure 4B). There was an approximate 10‐second delay in the average time elapsing for on‐scene ambulances calling into the control room nurses and doctors at PSAP‐2 (∼10 vs 20 seconds) to provide their routine report and receive disposition directives. However, this increase was not found to be clinically significant in follow‐up quality assurance review, particularly considering the circumstances (Figure 4B).
To better describe the impact of the COVID‐19 outbreak on ordinary EMS activity, the event classifications and severity codes were also analyzed and compared during the first 3 months of 2020 (Figure 5). Compared to prior months, in March, the percentage of more urgent calls rose and the type of call transitioned into more medical cases and fewer trauma calls.
4. LIMITATIONS
Several aspects of this reported reorganization would not be directly applicable to other PSAP systems globally and the study period does not reflect how demands on the healthcare system evolved over ensuing weeks. AREU members were already incorporated into PSAP operations on a day‐to‐day basis and task transition was thus easier with little need for special regulatory approvals, clearances, indemnifications, or recruitment of persons largely unfamiliar with PSAP‐2 operations. Also, there were prior close connections to public health and ID specialists. As more epidemiological information became available, the COVID‐19 response team remained at the PSAP but responsibilities did progressively evolve in response to subsequent characteristics of the outbreak. Nonetheless, other jurisdictions without such turnkey arrangements and relationships should organize such contingencies and the related logistics in advance, including collaborative multidisciplinary training and drills.
Using the control of ambulance dispatches and response intervals as a primary endpoint, though quantifiable, also has potential limitations. The number of ambulance dispatches, particularly for trauma, diminished worldwide following COVID‐19 lockdowns, likely amplified by fears of contracting COVID‐19 by leaving one's home. However, those observations occurred well after shelter‐in‐place directives were issued in the respective jurisdictions and Lombardy did not invoke lockdown until March 8, one of the reasons for the a priori choice for the 2‐week study period ending March 4. Accordingly, the usual EMS call types and severity remained fairly constant throughout February and even into early March (Figure 5).
5. DISCUSSION
COVID‐19 created unprecedented challenges for healthcare systems worldwide with death tolls continuing to rise. In Italy alone, over 34,000 deaths had occurred just within the first 120 days after announcing the nation's first case. Half of those deaths occurred within Lombardy. 17
COVID‐19 was an unexpected, chimeric pandemic with a spectrum of presentations, variable severities, and many asymptomatic carriers. Unanswered questions still remain, not only for the public at large, but knowledgeable scientists as well. Understandably, many non‐ill citizens immediately called 1‐1‐2 seeking guidance following the first confirmed case.
The phenomenon of the “worried‐well” seeking assurance is well known. For example, following the 1989 radiation contamination event in Goiânia, Brazil, 120,000 of 1.2 million residents flooded clinical sites seeking screening examinations whereas <250 may have been exposed. 18 Recognizing that such public reactions are predictable, the current study makes another compelling argument that future disaster planning, be it for another pandemic, a nuclear event, bioterrorism incident, or other similar challenges, should include response strategies such as those implemented in this report. 19 Even in an age of widespread social media, mass media, and the internet, 1‐1‐2 and counterpart systems on other continents remain universal safety nets for the public early on.
The profound escalation in PSAP calls in those early days following February 21 could have created significant compromise to the healthcare and public safety systems. Hospitals may have been overwhelmed had not ambulance dispositions been triaged and controlled by the COVID‐19 medical team. The AREU team's rapid actions not only helped to spare ambulance deployments but also provided more optimal dispositions such as stay‐at‐home quarantine directives. 20 Also, by avoiding lost time taken for hospital transports and lengthier on‐site evaluations by ambulance crews having to use PPE, the algorithms, resources, and processes put into place mitigated worsening response intervals for the true emergencies throughout that early phase.
Although more difficult to quantify, the efforts and processes taken for expert patient assessments, more optimal patient dispositions, and better coordination of the more complex cases with public health officials and hospitals were pivotal functions that also laid the foundations for optimal patient disposition strategies as the disease continued to spread and directly challenged the healthcare system with the truly sick patients. 21 , 22
The specific screening algorithms for PSAP‐1 developed by the team also contributed to more effective management of suspected COVID‐19 cases by allowing PSAP‐2 to better focus on the cases that needed their attention. PSAP‐1 and 2 algorithm referrals to public health authorities added further protection until better public education could evolve through social and mass media. 23 , 24
As exemplified here, demands on the system can suddenly appear overnight, requiring immediate, same‐day implementation. Logistical, regulatory and training barriers to implementation need to be overcome well before the crisis presents itself. The initial overwhelming phase of the public response demonstrated that such contingencies need to be in place ahead of time and that additional qualified personnel should be knowledgeable, prepared, and readily available to constitute specific response teams. In addition, contingency algorithms should be developed with templates that can be easily tailored or updated for the specific event or threat. In terms of communicable diseases, these protocols should be aimed at detecting suspected cases, limiting contagion, assigning the right hospital destination or quarantine dispositions, and avoiding needless ambulance dispatches. As more is learned about any new threat, algorithms must be continuously modified to adapt to evolving epidemiological characteristics and any directives from public health authorities.
In summary, utilizing disease‐tailored algorithms and specially assigned personnel, rapid reorganization of PSAP operations protected the EMS system in Milan by facilitating appropriate disposition of patients, controlling emergency ambulance allocation, and mitigating the potential resulting impact on hospital resources and PPE during the early phases of the COVID‐19 outbreak in Italy. Planning for future population‐based disasters should incorporate and prepare for such specialized team assignments.
CONFLICTS OF INTEREST
None of the authors have any conflicts of interest to declare and the research is derived from the routine quality assurance functions of a public agencies. No human subjects were involved and personal medical information was not involved. There was also no specific funding for the research and no specific grants received from any funding agency in the public, commercial, or not‐for‐profit domains.
AUTHOR CONTRIBUTIONS
Conception and design: Francesco Marrazzo, Stefano Spina, Fabio Sangalli, Paul E. Pepe, Roberto Fumagalli. Data acquisition: Francesco Marrazzo, Stefano Spina, Fabio Sangalli, Alessandra Sforza, Maurizio Migliari, Giuseppe Sechi. Revision of the manuscript: Francesco Marrazzo, Stefano Spina, Fabio Sangalli, Thomas Langer, Paul E. Pepe, Roberto Fumagalli. Final approval: all authors.
ACKNOWLEDGMENTS
The authors are deeply grateful for the professionalism and dedicated, resilient work ethic of the participating public safety answering point (PSAP) technicians, nurses, and physicians serving the AREU 118 emergency medical system network in Lombardy (Italy) as well as fellow PSAP colleagues worldwide.
Biography
Roberto Fumagalli, MD, is anesthetist‐in‐chief, in the Department of Anesthesia and Critical Care at ASST Grande Ospedale Metropolitano Niguarda, Milano, Italy.

Marrazzo F, Spina S, Pepe PE, et al. Rapid reorganization of the Milan metropolitan public safety answering point operations during the initial phase of the COVID‐19 outbreak in Italy. JACEP Open. 2020;1:1240–1249. 10.1002/emp2.12245
Funding and support: By JACEP Open policy, all authors are required to disclose any and all commercial, financial, and other relationships in any way related to the subject of this article as per ICMJE conflict of interest guidelines (see www.icmje.org). The authors have stated that no such relationships exist.
Supervising Editor: Juan A. March, MD.
REFERENCES
- 1. Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (covid‐19) outbreak in China. JAMA. 2020;2019:25‐28. 10.1001/jama.2020.2648 [DOI] [PubMed] [Google Scholar]
- 2. Holshue ML, DeBolt C, Lindquist S, et al. First case of 2019 novel coronavirus in the United States. N Engl J Med. 2020;382(10):929‐936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. WHO . Novel coronavirus (2019‐nCoV) situation report 168. World Health Organization, 2020. Accessed July 6, 2020. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200706-covid-19-sitrep-168.pdf?sfvrsn=7fed5c0b_2 [Google Scholar]
- 4. Ministero della salute . Nuovo coronavirus. 2020. Accessed July 6, 2020. http://www.salute.gov.it/nuovocoronavirus
- 5. US Centers for Disease Control and Prevention . Coronavirus disease 2019 (COVID‐19). Cases in the U.S. Accessed July 6, 2020. https://www.cdc.gov/coronavirus/2019-ncov/summary.html
- 6. Onder G, Rezza G, Brusaferro S. Case‐fatality rate and characteristics of patients dying in relation to COVID‐19 in Italy. JAMA. 2020;323(18):1775‐1776. Published online March 23, 2020. 10.1001/jama.2020.4683. [DOI] [PubMed] [Google Scholar]
- 7. Grasselli G, Pesenti A, Cecconi M. Critical care utilization for the COVID‐19 outbreak in Lombardy, Italy: early experience and forecast during an emergency response. JAMA. 2020;323(16):1545‐1546. Published online March 13, 2020. 10.1001/jama.2020.4031. [DOI] [PubMed] [Google Scholar]
- 8. AREU Lombardia. Sale operative regionali . SOREU Metropolitana. Accessed July 6, 2020. https://www.areu.lombardia.it/web/home/soreu-metropolitana
- 9. Spina S, Marrazzo F, Migliari M, Stucchi R, Sforza A, Fumagalli R. The Response of Milan's Emergency Medical System to the COVID‐19 Outbreak in Italy. Lancet. 2020;395(10227):e49‐e50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. US Centers for Disease Control and Prevention . Coronavirus disease 2019 (COVID‐19). Interim recommendations for emergency medical services (EMS) systems and 911 public safety answering points/emergency communication centers (PSAP/ECCs) in the United States during the coronavirus disease (COVID‐19) pandemic. Accessed July 6, 2020. https://www.cdc.gov/coronavirus/2019-ncov/hcp/guidance-for-ems.html
- 11. Wang D, Hu B, Hu C, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus‐infected pneumonia in Wuhan, China. JAMA. 2020;323(11):1061‐1069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Guan W‐J, Ni Z‐Y, Hu Y, et al. Clinical Characteristics of Coronavirus Disease 2019 in China. N Engl J Med. 2020;382:1708‐1720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497‐506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Wilder‐Smith A, Freedman DO. Isolation, quarantine, social distancing and community containment: pivotal role for old‐style public health measures in the novel coronavirus (2019‐nCoV) outbreak. J Travel Med. 2020;27(2):taaa020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. US Centers for Disease Control and Prevention . Coronavirus disease 2019 (COVID‐19). CDC tests for COVID‐19. 2020. Accessed July 6, 2020. https://www.cdc.gov/coronavirus/2019-ncov/about/testing.html
- 16. US Centers for Disease Control and Prevention . Coronavirus disease 2019 (COVID‐19). If You Are Sick or Caring for Someone. Accessed July 6, 2020. https://www.cdc.gov/coronavirus/2019-ncov/hcp/guidance-prevent-spread.html
- 17. Coronavirus (COVID‐19) deaths in Italy as of June 29, 2020, by region. Statista research department; Accessed July 6, 2020. https://www.statista.com/statistics/1099389/coronavirus-deaths-by-region-in-italy/ [Google Scholar]
- 18. Miller DS, Rivera JD. Community disaster recovery and resiliency: exploring global opportunities and challenges. New York: Routledge; 2011. [Google Scholar]
- 19. Challen K, Bentley A, Bright J, Walter D. Clinical review: mass casualty triage ‐ Pandemic influenza and critical care. Crit Care. 2007;11(2):212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Adalja AA, Toner E, Inglesby TV. Priorities for the US health community responding to COVID‐19. JAMA. 2020;323(14):1343‐1344. [DOI] [PubMed] [Google Scholar]
- 21. Hellewell J, Abbott S, Gimma A, et al. Feasibility of controlling 2019‐nCoV outbreaks by isolation of cases and contacts. medRxiv Preprint. 2020. 10.1101/2020.02.08.20021162 [DOI] [PMC free article] [PubMed]
- 22. Wang Y, Wang Y, Chen Y, Qin Q. Unique epidemiological and clinical features of the emerging 2019 novel coronavirus pneumonia (COVID‐19) implicate special control measures. J Med Virol. 2020:92(6):568‐576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Rothe C, Schunk M, Sothmann P, et al. Transmission of 2019‐nCoV infection from an asymptomatic contact in Germany. N Engl J Med. 2020;382(10):970‐971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Backer JA, Klinkenberg D, Wallinga J. Incubation period of 2019 novel coronavirus (2019‐nCoV) infections among travelers from Wuhan, China, 20‐28 January 2020. Euro Surveill. 2020;25(5):2000062. [DOI] [PMC free article] [PubMed] [Google Scholar]


