Abstract
Background and aim
The effect of the COVID‐19 pandemic on alcohol consumption is currently unclear. This study aimed to provide early estimates of how stress and demographics will interact with shifts in harmful alcohol consumption from before the COVID‐19 outbreak to 2 months into social distancing.
Design
Cross‐sectional convenience sample.
Setting
Australia.
Participants
A total of 1684 Australians aged 18–65 years who drink at least monthly.
Measurements
Items from the Alcohol Use Disorders Identification Test (AUDIT) and the stress subscale of the Depression Anxiety and Stress Scale (DASS).
Findings
Overall, harmful drinking decreased during social distancing measures in our sample [2019 score = 8.2, 95% confidence interval (CI) = 7.9–8.4; during the pandemic = 7.3, 95% CI = 7.1–7.6]. Younger drinkers, particularly young women, decreased their consumption the most, but there was a small increase in consumption in middle‐aged women. Drinkers experiencing high levels of stress also reported a relatively higher shift in harmful consumption compared with those with low levels of stress (β = 0.65, P = 0.003), despite reporting a small decrease overall.
Conclusions
The closure of licensed premises and social distancing measures in Australia in response to the COVID‐19 outbreak appear to have reduced harmful alcohol consumption in younger drinkers, particularly young women.
Keywords: Alcohol, AUDIT, COVID‐19, harmful drinking, risky drinking, stress
Introduction
The novel coronavirus (COVID‐19) pandemic has, as of writing, infected an estimated 4.5 million people with more than 300 000 deaths recorded [1], although both these numbers are widely thought to be an underestimate [2]. Public health responses have varied from country to country. Regarding alcohol sales, on‐premise locations such as restaurants and bars have been closed in many countries, along with most businesses that would involve people congregating together.
In most of these countries, stores that sell alcohol for consumption elsewhere (referred hereafter as off‐premise stores) remain open as usual, with a few exceptions such as Greenland, South Africa and Thailand, where they have also been closed [3]. Meanwhile, in India a 70% ‘corona‐tax’ has been placed on alcohol in an attempt to reduce consumption during the pandemic [4]. In countries where such measures have not been put in place there are concerns about consumption in private homes increasing during social distancing [5, 6]. Overall, evidence is lacking with regard to alcohol consumption concerning the effect of social distancing measures, legislation affecting the sale of alcohol and all the other societal upheavals inherent to this pandemic. Early estimates of the impact of the pandemic on consumption are urgently needed to inform health promotion and policy‐based responses.
On 29 March 2020, it was announced that Australians were only allowed to leave their homes for health‐care, exercise, shopping for essentials or essential work/education [7], restrictions that remained in place until 16 May. With all restaurant and bars closed and the population being asked to stay in their homes, consumption in licensed premises will decrease markedly. This may be matched by a corresponding increase in consumption in homes. Before the pandemic, almost two‐thirds of alcohol was already consumed at home in Australia, with 55‐year‐old drinkers consuming substantially more of their alcohol at home than younger drinkers (approximately 77% versus approximately 37%, respectively) [7]. One could predict that consumption will decline more for younger drinkers who are no longer able to drink in places where they usually drink, notably other people's homes and licensed venues [8].
However, there is also reason to be concerned that harmful consumption may increase. In times of economic crisis, risky drinking in men is thought to increase as a response to stress, while overall consumption falls in response to financial constraints [9]. Indeed, a study on health‐risk behaviours during the COVID‐19 pandemic in men who sleep with men found that more people had increased, than decreased, consumption since social distancing was implemented [10]. Social distancing and/or lockdown‐type measures have led to increased stress [11], which is directly associated with alcohol use [12], and alcohol‐related harms typically correlate with drinking to cope [13, 14, 15]. The stress of the pandemic, particularly among those who work and have caring commitments, has led to increases in stress, particularly in women [11]. This prior work on stress and consumption suggests that we will see an increase in consumption; however, this will presumably be somewhat counterbalanced by the closure of licensed premises and restricted social gatherings and face‐to‐face interactions. How much people will replace in‐person social drinking occasions with virtual ones is unknown, but this presumably will not be consistent by age. Overall, little is known about what changes we might see in alcohol consumption among different demographic groups.
Therefore, predicting the effect of the COVID‐19 pandemic on alcohol consumption is difficult. Timely and applicable research is required to inform health‐care professionals and policymakers working to limit the impact of potential harms. Internet‐based convenience samples are an expedient way of collecting exploratory data during this crisis when traditional methods are either not possible, due to distancing restrictions and high cost and/or time demands [6]. The results presented here aim to provide early indicators of changes in consumption and harms among drinkers during social distancing. The first hypothesis is that young people will disproportionately reduce their harmful drinking compared to older drinkers. The second hypothesis is that men will increase their harmful drinking relative to women. The third hypothesis is that those who experience high levels of stress will increase their harmful drinking more than other drinkers.
Method
Sample
To assess alcohol consumption before and during social distancing and levels of stress, a national cross‐sectional survey design was implemented. A convenience sample of adults aged between 18 and 65 were recruited through Facebook and Instagram advertisements. Data were collected between 16 April 2020 and 11 May 2020. To participate in the study, potential participants were redirected to the survey. After providing voluntary consent, participants were first screened using three inclusion criteria and then asked to complete the survey.
Online surveys were administered through http://www.qualtrics.com, which took approximately 10–15 minutes to complete. At the end of the survey, respondents were invited to enter a prize draw of 10 grocery vouchers worth 50$AU. The study protocol was approved by the Ethics Committee at La Trobe University (HEC20052).
In total, 2630 people clicked on the Facebook or Instagram advertisements and agreed to participate. Of those, 695 (26.4%) did not meet the inclusion criteria (i.e. being Australian, aged 18–65 and consume alcohol once a month) and a further 251 participants (12.7%) did not complete the survey.
Within the sample of 1684 participants 64.6% were female, 31.2% male, 3.6% preferred to self‐describe as non‐binary, gender‐fluid, agender or an option not listed and 0.7% preferred not to reply. Please note that all respondents are included in the results in Table 1; however, the combination of small sample size and the use of interactions in the model meant that only those who self‐identified as men or women could be included in the analyses presented in Table 2. The sample has a mean age of 48.9 [standard deviation (SD) = 13.3], with 79% completing a diploma or bachelor's degree. Comparisons between this sample and that of a nationally representative survey are shown in Table 1.
Table 1.
Comparison of mean (95% CI) AUDIT scores before and during the pandemic and commensurate scores from the representative sample in the NDSHS.
| Item | Before SD | During SD | % decrease | % increase | NDSHS |
|---|---|---|---|---|---|
| % Female | 64.5 (62.2, 68.8) | 47.6 (46.7, 48.7) | |||
| Age | 48.9 (48.3, 49.5) | 40.5 (40.2, 40.8) | |||
| 1. How often do you have a drink containing alcohol? | 3.02 (2.98, 3.06) | 3.08 (3.03, 3.13)** | 14.6 (12.9, 16.4) | 21.8 (19.9, 23.9) | 2.48 (2.46, 2.50) |
| 2. How many standard drinks do you have on a typical day when you are drinking? | 1.01 (0.96, 1.07) | 0.97 (0.91, 1.02)* | 14.6 (12.9, 16.4) | 14.0 (12.4, 15.8) | 1.01 (0.98, 1.04) |
| 3. How often do you have six or more standard drinks in one occasion? | 1.59 (1.53, 1.65) | 1.27 (1.20, 1.34)*** | 33.4 (31.1, 35.7) | 8.9 (7.6, 10.4) | 1.39 (1.36, 1.42) |
| Consumption subscale (AUDIT‐C) | 5.62 (5.49, 5.75) | 5.32 (5.18, 5.46) *** | 35.8 (33.5, 38.1) | 24.9 (22.8, 27.0) | 4.89 (4.82, 4.95) |
| 4. How often during the last year have you found that you were not able to stop drinking once you had started? | 0.79 (0.73, 0.85) | 0.61 (0.55, 0.66)*** | 20.2 (18.3, 22.3) | 6.2 (5.1, 7.5) | 0.33 (0.31, 0.34) |
| 5. How often during the last year have you failed to do what was normally expected of you because of your drinking? | 0.37 (0.33, 0.41) | 0.30 (0.26, 0.33)*** | 12.8 (11.2, 14.5) | 5.8 (4.7, 7.0) | 0.26 (0.25, 0.28) |
| 6. How often during the last year have you needed a first drink in the morning to get yourself going after a heavy drinking session? | 0.10 (0.08, 0.13) | 0.11 (0.08, 0.14) | 1.4 (0.9, 2.1) | 2.1 (1.5, 2.9) | 0.06 (0.05, 0.07) |
| Dependence subscale (AUDIT‐D) | 1.26 (1.16, 1.36) | 1.01 (0.91, 1.11) *** | 22.1 (20.1, 24.2) | 10.2 (8.8, 11.7) | 0.65 (0.62, 0.68) |
| 7. How often during the last year have you had a feeling of guilt or remorse after drinking? | 0.75 (0.71, 0.80) | 0.64 (0.59, 0.70)*** | 26.3 (24.2, 28.5) | 8.9 (7.6, 10.4) | 0.39 (0.37, 0.40) |
| 8. How often during the last year have you been unable to remember what happened the night before because you had been drinking? | 0.52 (0.48, 0.56) | 0.36 (0.32, 0.40)*** | 18.2 (16.4, 20.2) | 4.5 (3.6, 5.7) | 0.42 (0.40, 0.44) |
| Total (eight items) | 8.16 (7.90, 8.42) | 7.33 (7.05, 7.62) *** | 48.2 (45.8, 50.6) | 23.5 (21.4, 25.6) | 6.35 (6.25, 6.45) |
| 1684 | 1684 | 13 739 |
CI = confidence interval; n = 1684; NDSHS = National Drug Strategy Household Survey; AUDIT = Alcohol Use Disorders Identification Test.
P < 0.05;
P < 0.01;
P < 0.001.
Bold type indicates differences in score before and during social distancing as per a paired t‐test. SD = social distancing.
Table 2.
Multiple linear regression predicting the difference in AUDIT scores during and before the COVID‐19 pandemic.
| Frequency | Quantity | Risky | Consumption | Dependence | Total | ||
|---|---|---|---|---|---|---|---|
| Gender | Female | 0 (Ref.) | 0 (Ref.) | 0 (Ref.) | 0 (Ref.) | 0 (Ref.) | 0 (Ref.) |
| Male | 0.09 | 0.41** | 0.42** | 0.92** | 0.44 | 1.52* | |
| Age (years) | 18–25 | 0 (Ref.) | 0 (Ref.) | 0 (Ref.) | 0 (Ref.) | 0 (Ref.) | 0 (Ref.) |
| 26–35 | 0.19 | 0.56*** | 0.51*** | 1.26*** | 0.33* | 1.91*** | |
| 36–50 | 0.33*** | 0.87*** | 0.81*** | 2.00*** | 0.45** | 3.26*** | |
| 51–65 | 0.22** | 0.83*** | 0.87*** | 1.93*** | 0.65*** | 3.51*** | |
| Female × 18–25 | 0 (Ref.) | 0 (Ref.) | 0 (Ref.) | 0 (Ref.) | 0 (Ref.) | 0 (Ref.) | |
| Male × 26–35 | −0.02 | −0.17 | −0.14 | −0.33 | −0.34 | −1.13 | |
| Male × 36–50 | −0.29 | −0.52** | −0.43* | −1.23** | −0.45 | −1.82* | |
| Male × 51–65 | −0.25 | −0.46** | −0.55** | −1.26*** | −0.60* | −2.01** | |
| Education | < High school | 0 (Ref.) | 0 (Ref.) | 0 (Ref.) | 0 (Ref.) | 0 (Ref.) | 0 (Ref.) |
| > High school | 0.09 | 0.14** | −0.01 | 0.22* | −0.08 | 0.33 | |
| Stress | Low | 0 (Ref.) | 0 (Ref.) | 0 (Ref.) | 0 (Ref.) | 0 (Ref.) | 0 (Ref.) |
| Medium | 0.10* | 0.04 | 0.15** | 0.29** | −0.01 | 0.32 | |
| High | 0.11* | 0.08 | 0.15** | 0.33** | 0.12 | 0.65** |
n = 1612. Coefficients are unstandardized regression coefficients.
P < 0.05;
P < 0.01;
P < 0.001. AUDIT = Alcohol Use Disorders Identification Test.
Measures
Online survey
The survey consisted of selected questions from the Alcohol Use Disorders Identification Test (AUDIT), the stress subscale from the Depression Anxiety and Stress Scale (DASS) and some demographic items.
Demographics
Participants’ age, gender and highest level of academic qualification were requested.
Alcohol use and dependence
Eight items from the 10‐item AUDIT were used to assess alcohol use and dependence. The AUDIT is a screening tool that aims to identify hazardous and harmful alcohol consumption [16]. The first three questions focus on alcohol consumption and the next three make up a dependence subscale. Finally, in the full 10‐item AUDIT there are four questions that address negative consequences of drinking. However, as two of these items have response options that differentiate between harms that have happened in the past year and those that have happened in their life‐time, these items were deemed inappropriate for comparison between two time‐points that are less than a year apart. Therefore, while the first two items of this subscale are included in the eight‐item AUDIT, the negative consequences subscale has not been calculated. The total of the eight AUDIT items has been included as an overall measure of harmful or hazardous drinking, with the caveat that it is not the full scale that was designed for this purpose.
To identify differences before and during social distancing, the AUDIT was administered twice. In the first iteration of the survey the following was included as a precursor: ‘You are going to be asked similar questions twice. This is to help capture changes that we have all undergone due to coronavirus. In this section we are interested in your alcohol consumption over the past year before social distancing/isolation restrictions’. All questions then started with the words: ‘Before social distancing/isolation restrictions...’.
The second set of questions started with the precursor: ‘Now, here is the same set of questions relating to drinking since there have been social distancing/isolation restrictions. Usually we would ask people to think about what they would normally do but we are very aware that normal has taken on a new meaning in these difficult times. So, can you please answer the questions on this page about your time since there have been social distancing/isolation restrictions?’. All questions then started with the words: ‘Since social distancing/isolation’. The item wording of each question after the introductory text is shown in Table 1.
Response option scores from each question range from 0 to 4, meaning that subscale scores range from 0 to 12 and the eight‐item total from 0 to 32. Full item wording and response options can be found in the scale's original publication [17].
Levels of stress
The stress subscale from the short form DASS‐21 [18] was used to assess stress in the week preceding completion of the survey. The DASS‐21 is a 21‐item self‐report instrument designed to measure depression, anxiety and stress with robust reliability [19]. Response categories ranged from 0 (did not apply to me at all) to 3 (applied to me very much or most of the time) with scores ranging from 0 to 21. The stress scale has a excellent internal reliability (Cronbach's αstress = 0.93) [19]. In order to facilitate examination of non‐linear relationships and graphical representation of the findings, respondents were grouped into approximately equal low [7, 8, 9, 10], medium [11, 12, 13, 14] and high (15+) stress groups.
National Drug Strategy Household Survey
Data from the 2016 National Drug Strategy Household Survey (NDSHS [20]) were used to assess differences in demographics and survey responses between a sample representative of the Australian population and those obtained in the convenience sample used in the current study. The NDSHS is collected every 3 years via drop‐and‐collect paper forms, computer‐assisted telephone interview and on‐line surveys using multi‐stage, stratified random sampling [20]. The 2016 NDSHS had a 51.1% response rate. A total of 13 739 respondents (males = 6319, females = 7420) aged between 18 and 65 years who consumed alcohol at least monthly were used for the comparison analysis.
Respondents who had consumed any alcohol in the past 12 months completed the AUDIT. In the NDSHS, the AUDIT items are not asked together in one single section. Items one to three of the AUDIT vary slightly in the NDSHS, with slightly different wording and response options. The responses given in the NDSHS were recoded to reflect the responses available in the AUDIT (please see [21] for more details).
Analysis
Given the importance of quickly collecting data during an unprecedented time, these analyses were not pre‐registered and results should be considered exploratory. As noted above, 251 respondents were removed for not completing the survey. No other missing data were recorded. Mean scores on all items, subscale totals and total AUDIT scores were calculated for before and during social distancing measures following the pandemic. Paired t‐tests were used to identify significant shifts in AUDIT scores. In order to provide some insight into the differences between our sample and a sample more representative of the Australian population, corresponding results from the NDSHS were also generated.
Next, in order to ascertain which demographic groups experienced shifts in consumption, regression models predicting shifts in consumption during the first month of social distancing in Australia were conducted. The difference in scores between times 1 and 2 were calculated so that a positive number indicated an increase in score and was used as the outcome variable in regression models. Stress, education, age and gender and an interaction between age and gender were used as predictor variables. The interaction was included to allow for shifts between age and gender that were not uniform. Estimated marginal means in the shift in AUDIT scores by the age and gender interaction were graphed for ease of interpretation of results. Outcome variables included the total score, the two subscales with complete items and the three questions on consumption. These were selected because (a) these three items account for the majority of AUDIT scores and correlate highly with the total and (b) the three items in this subscale did not shift in unison.
Results
The scores on the AUDIT before and during the pandemic, along with the NDSHS comparisons, are shown in Table 1. The sample recruited for this study was older, more often female and had higher AUDIT scores in 2019 than those in the national representative sample. As can be seen, there was a reduction in total AUDIT score in our sample during the pandemic. Similar reductions were found in the two complete subscales, the AUDIT‐C and the AUDIT‐D. At the item level, reductions were consistently found in all items and subtotals except for item one, addressing frequency of consumption. This was also the only item in which more people reported a higher score during the pandemic. Please note that all figures in this paper represent scores on the AUDIT items, rather than a specific number of drinks or drinking days. On all other items, except for those on quantity per occasion and drinking first thing in the morning, more people reported a lower score during the pandemic. Overall, almost half of respondents had a decrease in total AUDIT score of one point or more and nearly a quarter increased.
Table 2 displays models predicting shifts in AUDIT scores during the pandemic. Given the importance of consumption in the study of harmful drinking, the three items in the consumption subscale are included as outcome variables here, as well as consumption and dependence subscale totals and the eight‐item total. In order to facilitate interpretation of results, the estimated marginal means of these shifts in scores are shown by age and sex in Fig. 1. The mean shift in score of each demographic group with 95% confidence intervals (CIs) can be seen in all the figures. An estimated marginal mean of one indicates an increase of score by 1 point during the pandemic.
Figure 1.
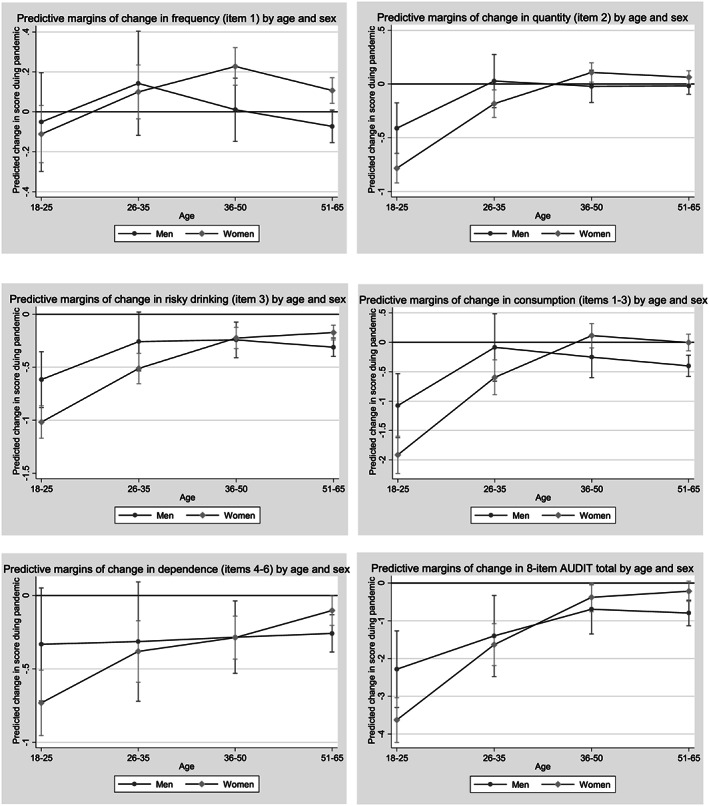
Predictive margins of change in score with 95% confidence intervals during the pandemic by age and gender.Reference line = 0 (or no change in score) in each graph
As Fig. 1 demonstrates, women aged 36–50 increased both their frequency (item one) and quantity (item two) of consumption—for both groups the 95% CIs are clear of the line marking a shift. However, overall decreases in our outcome variables were much more common. In particular, we found that all groups except men aged 26–35 decreased their risky drinking frequency (item three). Consumption subscale scores decreased in respondents age 18–25, women aged 26–35 and men aged 51–65. Dependence subscale scores decreased in all groups except for 18–35‐year‐old men. Turning to eight‐item total AUDIT scores, the first hypothesis was supported, as decreases in harmful drinking are larger in the younger age groups – only women aged 35 and older did not significantly decrease their harmful drinking. The second hypothesis was partially supported, as decreases in total score and other outcome variables appear to be driven by younger women; however, it was only older women who did not decrease their harmful consumption significantly during the pandemic.
The third hypothesis was partially supported, as those experiencing high levels of stress had relatively higher shifts in scores than those who reported low levels of stress. However, the estimated marginal means for those in the high stress group (−0.77, 95% CI = −1.06, −0.49) were still significantly below zero, indicating that this group also decreased their harmful drinking overall. In the other models, those in the high and medium stress groups reported relatively higher shifts than those in the low stress group for items one and three and the consumption subscale.
Discussion
This study aimed to identify groups that might have increased or decreased harmful consumption in Australia during the COVID‐19 pandemic. In our convenience sample, we found a small downward shift in most alcohol indicators during the early stages of the pandemic. The first hypothesis was supported, as younger drinkers decreased their harmful consumption more than older drinkers. We found partial support for the second hypothesis: men's consumption did not increase, although it decreased less compared to women in younger age groups. The third hypothesis was supported, as higher levels of stress were positively associated with shifts in total AUDIT score.
Decreases in harmful drinking in our sample were primarily driven by drinkers aged 18–25, particularly women. These relatively large downward shifts in harmful drinking masked a plateau or even a small increase in consumption in older drinkers. Conversely, drinkers aged 36–50 increased AUDIT scores during the pandemic; again, this is being driven more by women, as they showed increased scores in the consumption subscale and overall AUDIT score. Previous research has demonstrated that women but not men increase their alcohol consumption when confronted with conflicting work and family duties [22], which may have become more prevalent or pronounced during social distancing; a worthwhile avenue of future research. Our finding that men also decreased their alcohol consumption during the pandemic is in contrast to the finding of Sanchez and colleagues [10], who found a sample of men who had sex with men reported increases in consumption. It is possible that this is due to our study's broader target population, or it may reflect respondents being asked to assess their shift in consumption themselves—these respondents may be referring to the same increase in frequency of consumption that we found in the current study, rather than an increase in overall consumption or harm.
The finding that more stress was linked with relatively higher harmful consumption during the pandemic is consistent with previous non‐pandemic specific work on harmful drinking and stress within individuals [9]. Overall, however, scores have decreased in what can be considered a stressful time. Therefore, it appears that the reduction of opportunities for drinking with people outside an individual's household has outweighed increases attributable to stress, particularly in young people, and at least in the first month of social distancing. It appears that the decrease of availability of on‐premise drinking locations remains an important strategy to prevent young adults’ harmful drinking. This is in line with work on availability and alcohol‐related harm both in Australia and internationally [23].
Overall, the shifts in AUDIT scores that we found were quite small. Scores on most of the scores in most demographic groups have not significantly shifted. Early studies such as this are less likely to detect shifts in consumption than those that are administered later in the pandemic—future work assessing this is recommended. However, of potential concern here is that there is a subgroup of individuals who have increased their alcohol consumption during this stressful time, and that this could continue even after social distancing measures are eased. We recommend that health‐care professionals working with people dealing with increased stress during the pandemic ask about alcohol consumption. Further, particular attention could be paid to middle‐aged women in this regard.
The most important limitation of the current study is the sampling strategy. A convenience sample has been recruited via advertising on Facebook and Instagram and, as indicated by the differences in demographics between our sample and the NDSHS, is not representative of the Australian population. Instead, the sample is two‐thirds female, significantly older and drink more heavily than the average Australian population (aged 18–65) recruited for the NDSHS. This study can provide important early indications of how alcohol consumption might be changing as a result of this pandemic. Furthermore, the analyses that account for demographic differences provide insight into how different groups of Australians might be reacting to the pandemic with respect to their alcohol consumption. In addition, respondents were asked to estimate their monthly consumption since social distancing and also for the previous year—which may be susceptible to a difference in recall bias [24] and would presumably be less accurate than a study in which respondents could provide their consumption at the two time‐points [24]. Finally, questions on the economic and labour‐related disruptions subsequent to the pandemic were not included in this study. Future work on these factors and their impact on consumption are recommended.
To conclude, we found early indications from a large convenience sample that, overall, from before to during the COVID‐19 pandemic Australians may have decreased harmful drinking, particularly among young adults. This is despite a slight increase in quantity of consumption. As would be expected, the closure of licensed premises has resulted in a decrease in harmful alcohol consumption in young adults in particular, but there is no reason to assume that these decreases will not reverse when licensed premises re‐open. Based on these early estimates, reductions in short‐term harms from alcohol in Australia during social distancing should be expected. A potential issue to be aware of is that respondents may become accustomed to more frequent drinking in the home. Given that home drinking is thought to be habitual [25], higher levels of consumption might be difficult to reverse when coronavirus restrictions begin to ease, leading to more drinking opportunities which are associated with more risky drinking. Research monitoring how consumption patterns shift when licensed premises re‐open is recommended.
Declaration of interests
None.
Author contributions
Sarah Callinan: Conceptualization; data curation; formal analysis; funding acquisition; investigation; methodology; project administration; supervision. Koen Smit: Conceptualization; investigation; methodology; project administration; supervision. Yvette Mojica‐Perez: Formal analysis; methodology; project administration; validation. Simon D'Aquino: Data curation; investigation; project administration. David Moore: Data curation; investigation; project administration. Emmanuel Kuntsche: Conceptualization; formal analysis; funding acquisition; investigation.
Acknowledgements
S.C. is funded by an Australian Research Council Discovery Early Career Researcher Award (DE180100016). The Centre for Alcohol Policy Research is co‐funded by the Foundation for Alcohol Research and Education, an independent, charitable organization working to prevent the harmful use of alcohol in Australia (http://www.fare.org.au). The Australian Institute of Health and Welfare manage the data collection and dissemination of the National Drug Strategy Household Survey and we are grateful to them for facilitating access to the data via the Australian Data Archive.
Callinan, S. , Smit, K. , Mojica‐Perez, Y. , D'Aquino, S. , Moore, D. , and Kuntsche, E. (2021) Shifts in alcohol consumption during the COVID‐19 pandemic: early indications from Australia. Addiction, 116: 1381–1388. 10.1111/add.15275.
References
- 1. World Health Organization (WHO) . Situation report—118. In: WHO, editor. Coronavirus Disease (COVID‐2019); 2020. Available at: https://www.who.int/docs/default‐source/coronaviruse/situation‐reports/20200517‐covid‐20200519‐sitrep‐20200118.pdf?sfvrsn=20200521c20200510dafe_20200516 (accessed 17 May 2020).
- 2. Buonanno P., Galletta S., Puca M. Estimating the severity of COVID‐19: evidence from the Italian epicenter SSRN 2020. Available at: 10.2139/ssrn.3567093 (accessed 2 April 2020). [DOI] [PMC free article] [PubMed]
- 3. Green E. Some countries are banning alcohol sales in their lockdowns—leading shoppers to panic‐buy, the world: PRX. 2020. Available at: https://www.pri.org/stories/2020‐2004‐2009/some‐countries‐are‐banning‐alcohol‐sales‐their‐lockdowns‐leading‐shoppers‐panic (accessed 5 May 2020).
- 4. ABC News . Delhi imposes 70 per cent coronavirus tax on alcohol to curb India's post‐lockdown thirst: ABC online. 2020. Available at: https://www.abc.net.au/news/2020‐2005‐2006/india‐hikes‐alcohol‐prices‐through‐coronavirus‐tax/12218582 (accessed 6 May 2020).
- 5. Paradis C. Open versus closed: the risks associated with retail liquor stores during COVID‐19. Canadian Centre on Substance Use and Addiction. 2020. Available at: https://www.ccsa.ca/open‐versus‐closed‐risks‐associated‐retail‐liquor‐stores‐during‐covid‐19 (accessed 5 May 2020).
- 6. Marsden J., Darke S., Hall W., Hickman M., Holmes J., Humphreys K. et al. Mitigating and learning from the impact of COVID‐19 infection on addictive disorders. Addiction 2020; 115: 1007–1010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Callinan S., Livingston M., Room R., Dietze P. Drinking contexts and alcohol consumption: how much alcohol is consumed in different Australian locations? J Stud Alcohol Drugs 2016; 77: 612–619. [DOI] [PubMed] [Google Scholar]
- 8. Kuntsche E., Gmel G. Alcohol consumption in late adolescence and early adulthood—where is the problem? Swiss Medical Week 2013; 143: 13826. [DOI] [PubMed] [Google Scholar]
- 9. de Goeij M. C. M., Suhrcke M., Toffolutti V., van de Mheen D., Schoenmakers T. M., Kunst A. E. How economic crises affect alcohol consumption and alcohol‐related health problems: a realist systematic review. Soc Sci Med 2015; 131: 131–146. [DOI] [PubMed] [Google Scholar]
- 10. Sanchez T., Zlotorzynska M., Rai M., Baral S. Characterizing the impact of COVID‐19 on men who have sex with men across the United States in April, 2020. AIDS Behav 2020; 24: 2024–2032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Wang C., Pan R., Wan X., Tan Y., Xu L., Ho C. S. et al. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID‐19) epidemic among the general population in China. Int J Environ Res Public Health 2020; 17: 1729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Keyes K., Hatzenbuehler M., Grant B., Hasin D. Stress and alcohol: epidemiologic evidence. Alcohol Res 2012; 34: 391. [PMC free article] [PubMed] [Google Scholar]
- 13. Blevins C., Abrantes A., Stephens R. Motivational pathways from antecedents of alcohol use to consequences: a structural model of using alcohol to cope with negative affect. Am J Drug Alcohol Abuse 2016; 42: 395–403. [DOI] [PubMed] [Google Scholar]
- 14. Grant V., Stewart S., Mohr C. Coping‐anxiety and coping‐depression motives predict different daily mood–drinking relationships. Psychol Addict Behav 2009; 23: 226–237. [DOI] [PubMed] [Google Scholar]
- 15. Young C., Dibello A., Traylor Z., Zvolensky M., Neighbors C. A longitudinal examination of the associations between shyness, drinking motives, alcohol use, and alcohol‐related problems. Alcohol Clin Exp Res 2015; 39: 1749–1755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Saunders J., Aasland O., Babor T., de la Fuente J., Grant M. Development of the alcohol use disorders identification test (AUDIT): WHO collaborative project on early detection of people with harmful alcohol consumption—II. Addiction 1993; 88: 791–804. [DOI] [PubMed] [Google Scholar]
- 17. Babor T., Higgins‐Biddle J., Saunders J., Monteiro M. The Alcohol Use Disorders Identification Test: Guidelines for Use in Primary Care. Geneva: World Health Organization; 2001. [Google Scholar]
- 18. Lovibond P., Lovibond S. The structure of negative emotional states: comparison of the depression anxiety stress scales (DASS) with the Beck depression and anxiety inventories. Behav Res Ther 1995; 33: 335–343. [DOI] [PubMed] [Google Scholar]
- 19. Henry J., Crawford J. The short‐form version of the depression anxiety stress scales (DASS‐21): construct validity and normative data in a large non‐clinical sample. Br J Clin Psychol 2005; 44: 227–239. [DOI] [PubMed] [Google Scholar]
- 20. Australian Institute of Health and Welfare National Drug Strategy Household Survey 2016. Canberra: Australian Institute of Health and Welfare; 2016. [Google Scholar]
- 21. Callinan S., Livingston M., Murtaza G., Cowlishaw S., Grittner U., Dietze P. et al. Identification of age differences in the Alcohol Use Disorders Identification Test using item response theory. Utrecht, the Netherlands: Kettil Bruun Society for Social and Epidemiological Research on Alcohol Annual Conference; 2019. [Google Scholar]
- 22. Kuntsche S., Kuntsche E. When the burden gets overwhelming: testing an inverse U‐shaped relation between work‐family conflicts and alcohol use. Eur Addict Res 2020; 10.1159/000507665 [DOI] [PubMed] [Google Scholar]
- 23. Babor T., Caetano R., Casswell S., Edwards G., Giesbrecht N., Graham K. et al. Alcohol: No Ordinary Commodity—Research and Public Policy. Oxford: Oxford University Press; 2010. [Google Scholar]
- 24. Ekholm O. Influence of the recall period on self‐reported alcohol intake. Eur J Clin Nutr 2004; 58: 60–63. [DOI] [PubMed] [Google Scholar]
- 25. Brierley‐Jones L., Ling J., McCabe K., Wilson G., Crosland A., Kaner E. et al. Habitus of home and traditional drinking: a qualitative analysis of reported middle‐class alcohol use. Sociol Health Illn 2014; 36: 1054–1076. [DOI] [PubMed] [Google Scholar]


